Abstract
Purpose
Increase in breast cancer survivorship, advancements in diagnostic imaging and standardization of contralateral breast screening before breast cancer surgery have resulted in increased detection of contralateral breast cancer (CBC). The aim of this study was to assess national trends of synchronous bilateral breast cancer (sBBC) and metachronous bilateral breast cancer (mBBC) incidence in newly diagnosed breast cancer patients.
Methods
The Surveillance, Epidemiology, and End Results (SEER) database (1973–2014) was used to identify 11,177 women diagnosed with CBC. CBC was classified as sBBC when primary breast cancer in both breasts is diagnosed in the same year, or as mBBC, when diagnosed more than one year from primary breast cancer. Temporal trends in sBBC incidence were then evaluated using the Cochran-Armitage test for trend.
Results
Of the 11,177 women diagnosed with CBC, 4228 (38%) had sBBC and 6949 (62%) had mBBC. The incidence of sBBC increased significantly from 1.4% in 1975 to 2.9% in 2014 (p < 0.001). sBBC was more likely to be diagnosed as early stage in recent years (78% in 1975 vs. 90% in 2014 [p < 0.001]), and 69% of patients were treated with mastectomy in 2014.
Conclusion
The number of sBBC has increased, and contralateral tumors are more likely to be detected at an early stage with the first primary breast cancer. Despite the early stage findings, most were treated with mastectomy. Further studies are needed to define the best therapy for patients with contralateral disease and optimal surveillance and detection methods.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
In recent years, more women are living with a breast cancer diagnosis due to increased breast cancer incidence, reduced breast cancer mortality, and improved life expectancy [1]. However, this increase in breast cancer survivorship also means that more women are at risk for developing contralateral breast cancer (CBC). CBC is classified as either synchronous BBC (sBBC), when CBC is diagnosed simultaneously with the first breast cancer, or metachronous BBC (mBBC), when CBC is diagnosed during long-term follow-up after the first breast cancer. Advancements in breast diagnostic imaging and routine use of contralateral breast screening result in increased detection of sBBC; however, there is limited data on the incidence and trends of sBBC or mBBC due to lack of widely accepted or standard definitions [2]. The aim of this study was to examine national trends in sBBC and mBBC incidence for newly diagnosed breast cancer patients in the United States using a large national database.
Materials and methods
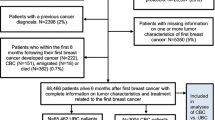
The Surveillance, Epidemiology, and End Results (SEER) database of the National Cancer Institute provides information on cancer incidence and survival in the United States. SEER currently collects and publishes cancer incidence and survival data from population-based cancer registries, which covers approximately 28% of the United States population. Because this study did not meet the definition of human subject research, the protocol was considered exempt from review from the Dana-Farber Cancer Institute Institutional Review Board. Inclusion criteria included female patients aged 20 years or older who were diagnosed with breast cancer between 1973 and 2014 and had surgery. The breast cancer cases and population data were obtained from the SEER 18 Registries Database (SEER 18, November 2016 submission). Since there is no special code in SEER to identify CBC patients, we extracted patients with at least one prior breast cancer and removed ipsilateral breast cancer records, according to laterality, cancer sequence number and multiple primary and histology coding rules in SEER. To evaluate trends in sBBC incidence, we chose patients whose CBCs were diagnosed at every 10 years (1975, 1985, 1995, 2005, and 2014). Although SEER data do not provide the exact date of breast cancer diagnosis, we defined sBBC as breast cancer in both breasts diagnosed in the same year, and defined mBBC as CBC diagnosed at more than 1 year after the first breast cancer. For each case of sBBC in our study, the breast containing the larger tumor was defined as the primary tumor and the contralateral smaller tumor was defined as contralateral tumor of sBBC. We included invasive and in situ cases as breast cancers in our study cohort, according to the TNM classification of AJCC 7th edition [3] which had been used until 2017. Histology and stages were coded in the database according to the International Classification of Diseases for Oncology, Third Edition (ICD-O-3); while stage at diagnosis is coded as in situ, local (localized to the breast), regional (spread to tissues surrounding the breast or to regional lymph nodes), distant (metastatic), or unknown. The crude incidence rates of bilateral breast cancer (BBC) were calculated by dividing the number of BBC patients by the number of newly diagnosed breast cancer cases in the same period. Among 190,871 breast cancer patients diagnosed in these years, we identified 16,567s breast cancers with at least one prior breast cancer record. We excluded 4803 patients with ipsilateral breast tumors and 587 patients who did not undergo breast surgery, resulting in 11,177 CBC patients for analysis (Fig. 1).
Baseline characteristics were compared using the Chi-squared test for categorical variables and Student’s T test for continuous variables. To determine temporal trends of the incidence of sBBC, we used the Cochran-Armitage test for trends. All p values were two-sided, with a threshold of 0.05 used to indicate statistical significance. Statistical analyses were performed using JMP (SAS Institute Inc., Cary, NC, USA).
Results
Trends of CBC incidence
The absolute number of CBC cases significantly increased over time, from 2.6% of all breast cancers in 1975 to 7.5% in 2014 (p < 0.001) (Fig. 2). The increase was also statistically significant in sBBC, from 1.4% in 1975 to 2.9% in 2014 (p < 0.001) and in mBBC, from 1.2% in 1975 to 4.6% in 2014 (p < 0.001).
Characteristics of bilateral breast cancers (Table 1)
Of the 11,177 women diagnosed with CBC, 4228 (37.8%) had sBBC and 6949 (62.2%) had mBBC (Table 1). Of all 22,354 cancers diagnosed in 11,177 BBC patients, 25.2% (N = 5623) were diagnosed at an in situ stage and 52.2% (N = 11,679) were diagnosed at a localized stage. With respect with histology, 14.9% (N = 3326) of all 11,177(× 2) cancers among the BBC were diagnosed with invasive lobular carcinoma or invasive lobular carcinoma mixed with other types of carcinoma, especially women with sBBC (18.1% vs. 12.9% in mBBC [p < 0.01]). Of the 4228 sBBC patients, 40.4% of contralateral tumors were diagnosed as in situ carcinoma compared to 26.0% of contralateral tumors of mBBC being diagnosed as in situ carcinoma (p < 0.01). In addition, contralateral tumors of sBBC were more likely to be treated with mastectomy than contralateral tumors of mBBC (67.5% vs. 53.5% [p < 0.01]).
Trends in characteristics of contralateral tumors of sBBC
The proportion of contralateral tumors of sBBC diagnosed at an early stage (in situ and localized disease) increased from 77.5% in 1975 to 89.6% in 2014 (Table 2). Contralateral tumors of sBBC were more likely to be diagnosed as in situ carcinoma than in earlier years (36.8% in 1975 and 44.3% in 2014 [p < 0.001]). Despite the early stage at diagnosis in most contralateral tumors in sBBC—83.5% in 1995, 84.1% in 2005 and 89.6% in 2014—mastectomy rates remained relatively high from 69.8% in 1995, 66.7% in 2005 and 69.0% in 2014.
Discussion
Our study demonstrated an increase in the number and proportion of sBBC in newly diagnosed breast cancer patients. In addition, we report findings that suggest contralateral cancers diagnosed in more recent years are more likely to be diagnosed at an earlier stage and treated with mastectomy as sBBC when compared to CBC treated in previous years. It is interesting to note that despite the fact that 90% of contralateral tumors of sBBC were detected at an early stage, nearly 70% of them were treated with mastectomy in 2014.
One of the main factors contributing to the increase of sBBC is early detection of contralateral tumors brought about by advances in breast diagnostic imaging and routine use of contralateral breast screening in patients with newly diagnosed breast cancer. Early detection of breast cancer has been conducted with a gradual shift to full-field digital mammography (FFDM) from screen film mammography [4]. As FFDM replaced analog mammography, some reports revealed that breast cancer associated with microcalcifications often associated with DCIS was more likely to be identified by FFDM [5]. As a result, the incidence of DCIS has markedly increased from 5.83/100,000 women in 1975 to 37.02/100,000 in 2009 based on November 2016 SEER data [6]. Contralateral breast screening has been conducted with mammography since the 1990s; compared with clinical breast examination alone, mammography resulted in a 2.4 increase in the number of breast cancers detected [7, 8]. In addition, the use of breast magnetic resonance imaging (MRI) might contribute to the increase in sBBC incidence. Currently in the United States, MRI is frequently used for estimating extent of disease even in those without an inherited predisposition to breast cancer. MRI technology has a high sensitivity for detecting breast cancer [9]. Advances in MRI equipment have enabled simultaneous screening of the contralateral breast as well as the ipsilateral site. It has been reported that MRI can detect mammographically and clinically occult contralateral breast cancer in 3.1% of women with unilateral breast cancer [10]. Although the details of these changes in imaging modalities were not coded in the SEER database, these advancements in mammography and MRI likely have had a substantial impact on the early detection of CBC.
It has also been postulated that one of the causes of the increasing sBBC rates in the United States is the growing number of occult cancers diagnosed after a contralateral prophylactic mastectomy (CPM). The proportion of unilateral breast cancer patients who undergo CPM have increased from 3.9% in 2002 to 12.7% in 2012 [11], and the incidence rate of occult breast cancer diagnosed after CPM ranges between 1.3 and 11.3% [12,13,14,15,16]. Detecting occult cancer in CPM specimens is likely to be an additional reason for the increase of contralateral tumors of sBBC.
It is noteworthy and not surprising that many sBBC patients chose mastectomy for their contralateral breast tumors despite its early detection. Although sBBC is not an absolute contraindication for breast-conserving surgery [17] and even after 1991 when a National Institutes of Health consensus statement recommended breast-conserving surgery plus radiation as an appropriate alternative primary therapy to mastectomy for the majority of women with early stage breast cancer [18], our result showed that about 70% of contralateral tumors of sBBC were treated with mastectomy in 1995, 2005, and 2014, despite 83–90% of contralateral tumors being diagnosed at an early stage (Table 2). Importantly, our analyses excluded data from 1975 to 1985, as the majority of breast surgery was mastectomy in this era; thus, these results reflect trends in the breast conservation era from 1995 to 2014. Explanations surrounding why women diagnosed with CBC are choosing mastectomy over breast-conserving surgery are complex and unclear. Several studies suggest that BBC is one of the related clinical factors that increases the probability of BRCA mutations [19, 20] and remains one of the criteria for recommendation of genetic testing [17]. In the absence of a genetic predisposition, the presence of the second breast cancer may also motivate patients to choose a more aggressive surgical approach that will reduce their overall breast cancer risk in the future.
In addition to these explanations, one could also posit that surgeons would have been more apt to recommend bilateral mastectomy for BBC patients, particularly for lobular cancers. It is well known that invasive lobular carcinomas have a higher frequency of bilaterality and multicentricity than invasive ductal carcinomas [21]. Patients with invasive lobular carcinoma or invasive lobular carcinoma mixed with other types of carcinoma were significantly more likely to undergo mastectomy than invasive ductal carcinoma not otherwise specified in both sBBC and mBBC (Table 3). Although invasive lobular carcinoma represents 10–15% of invasive breast tumors [22], our study showed that 20.0% of invasive BBC cases were invasive lobular carcinoma and infiltrating lobular carcinoma mixed with other types of carcinoma. In addition, of the sBBC patients, 21.3% of the primary tumors were diagnosed with invasive lobular carcinoma compared to 14.8% of the contralateral tumors (Table 1). Although there are possibilities that the patients diagnosed with invasive lobular carcinoma had more aggressive imaging, diagnostic intervention and prophylactic treatment for the contralateral breast, we could not assess the details in SEER data.
sBBC incidence can be approximated according to how many patients with CBC are treated simultaneously among the total number of patients with primary breast cancer during the same period. Similar estimates of mBBC incidence in this study were approximated by calculating how many patients had a previous CBC among the number of patients with primary breast cancer during the same periods. On the other hand, the incidence of mBBC generally expresses the future risk of CBC for unilateral breast cancer patients and is estimated by how often CBC occurs during follow-up for a unilateral breast cancer. In previous reports using a large database, the overall trend of mBBC was found to be declining, possibly because of the widespread usage of adjuvant hormonal therapies [23, 24]. As shown in this study, although the chance of finding mBBC may have increased due to the number of patients treated with unilateral breast cancer and advances in diagnostic imaging, the risk of CBC is also expectedly reduced by appropriate systemic treatment.
Our study has several limitations inherent to large data sets. The SEER database lacks information on the diagnostic imaging techniques utilized, patient family histories or genetic predispositions, HER2 status, systemic therapies administered, and details of the surgical procedures performed; therefore, we could not adjust for these factors to understand the detailed relationship with BBCs. Nonetheless, this large-scale study with over 10,000 CBC with clinicopathologic data of each side which is difficult to extract from other sources provided a unique opportunity to assess temporal trends of sBBC incidence.
In summary, our study reveals that in the United States, the number of sBBC has been increasing and contralateral tumors are more likely to be diagnosed at an early stage and treated with mastectomy. As breast diagnostic imaging becomes more widely and routinely available for contralateral breast screening, the increase in sBBC incidence may be seen in other countries as well. Although most women with CBC chose mastectomy, future studies are needed to demonstrate the clinical significance of early detection of contralateral tumors and optimal screening and surveillance methods.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, Cooper D, Gansler T, Lerro C, Fedewa S, Lin C, Leach C, Cannady RS, Cho H, Scoppa S, Hachey M, Kirch R, Jemal A, Ward E (2012) Cancer treatment and survivorship statistics. CA 62(4):220–241. https://doi.org/10.3322/caac.21149
McCaul KA (2006) Bilateral breast cancer incidence and survival. [PhD thesis]. North Terrace, aDELAIDE SA 5005: University of Adelaide 2006. Available from: university of Adelaide. School of population Health and Clinical Practice, Library E-Reserve
AJCC cancer staging manual (2010). (7th ed). Springer, NY
van Ravesteyn NT, van Lier L, Schechter CB, Ekwueme DU, Royalty J, Miller JW, Near AM, Cronin KA, Heijnsdijk EA, Mandelblatt JS, de Koning HJ (2015) Transition from film to digital mammography: impact for breast cancer screening through the national breast and cervical cancer early detection program. Am J Prev Med 48(5):535–542. https://doi.org/10.1016/j.amepre.2014.11.010
Knox M, O’Brien A, Szabo E, Smith CS, Fenlon HM, McNicholas MM, Flanagan FL (2015) Impact of full field digital mammography on the classification and mammographic characteristics of interval breast cancers. Eur J Radiol 84(6):1056–1061. https://doi.org/10.1016/j.ejrad.2015.03.007
Howlader N NA, Krapcho M, Miller D, Bishop K, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds) SEER Cancer Statistics Review, 1975–2014, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site, April 2017
Morrow M, Schmidt R, Hassett C (1995) Patient selection for breast conservation therapy with magnification mammography. Surgery 118(4):621–626
Morrow M, Strom EA, Bassett LW, Dershaw DD, Fowble B, Giuliano A, Harris JR, O’Malley F, Schnitt SJ, Singletary SE, Winchester DP (2002) Standard for breast conservation therapy in the management of invasive breast carcinoma. CA 52(5):277–300
Tozaki M, Igarashi T, Fukuda K (2006) Positive and negative predictive values of BI-RADS-MRI descriptors for focal breast masses. Magn Reson Med Sci 5(1):7–15
Lehman CD, Gatsonis C, Kuhl CK, Hendrick RE, Pisano ED, Hanna L, Peacock S, Smazal SF, Maki DD, Julian TB, DePeri ER, Bluemke DA, Schnall MD, Group ATI (2007) MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N Engl J Med 356(13):1295–1303
Wong SM, Freedman RA, Sagara Y, Aydogan F, Barry WT, Golshan M (2017) Growing use of contralateral prophylactic mastectomy despite no improvement in long-term survival for invasive breast cancer. Ann Surg 265(3):581–589. https://doi.org/10.1097/SLA.0000000000001698
Yamauchi H, Okawa M, Yokoyama S, Nakagawa C, Yoshida R, Suzuki K, Nakamura S, Arai M (2018) High rate of occult cancer found in prophylactic mastectomy specimens despite thorough presurgical assessment with MRI and ultrasound: findings from the hereditary breast and ovarian cancer Registration 2016 in Japan. Breast Cancer Res Treat 172(3):679–687. https://doi.org/10.1007/s10549-018-4953-1
McLaughlin SA, Stempel M, Morris EA, Liberman L, King TA (2008) Can magnetic resonance imaging be used to select patients for sentinel lymph node biopsy in prophylactic mastectomy? Cancer 112(6):1214–1221. https://doi.org/10.1002/cncr.23298
van Sprundel TC, Schmidt MK, Rookus MA, Brohet R, van Asperen CJ, Rutgers EJ, Van’t Veer LJ, Tollenaar RA (2005) Risk reduction of contralateral breast cancer and survival after contralateral prophylactic mastectomy in BRCA1 or BRCA2 mutation carriers. Br J Cancer 93(3):287–292. https://doi.org/10.1038/sj.bjc.6602703
Boughey JC, Khakpour N, Meric-Bernstam F, Ross MI, Kuerer HM, Singletary SE, Babiera GV, Arun B, Hunt KK, Bedrosian I (2006) Selective use of sentinel lymph node surgery during prophylactic mastectomy. Cancer 107(7):1440–1447. https://doi.org/10.1002/cncr.22176
Yao K, Liederbach E, Tang R, Lei L, Czechura T, Sisco M, Howard M, Hulick PJ, Weissman S, Winchester DJ, Coopey SB, Smith BL (2015) Nipple-sparing mastectomy in BRCA1/2 mutation carriers: an interim analysis and review of the literature. Ann Surg Oncol 22(2):370–376. https://doi.org/10.1245/s10434-014-3883-3
National Comprehensive Cancer Network. Development and update of the NCCN guidelines. Version 3.2018
NIH consensus conference Treatment of early-stage breast cancer (1991). JAMA 3:391-395
Frank TS, Deffenbaugh AM, Reid JE, Hulick M, Ward BE, Lingenfelter B, Gumpper KL, Scholl T, Tavtigian SV, Pruss DR, Critchfield GC (2002) Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol 20(6):1480–1490. https://doi.org/10.1200/JCO.2002.20.6.1480
Couch FJ, DeShano ML, Blackwood MA, Calzone K, Stopfer J, Campeau L, Ganguly A, Rebbeck T, Weber BL (1997) BRCA1 mutations in women attending clinics that evaluate the risk of breast cancer. N Engl J Med 336(20):1409–1415. https://doi.org/10.1056/NEJM199705153362002
Orvieto E, Maiorano E, Bottiglieri L, Maisonneuve P, Rotmensz N, Galimberti V, Luini A, Brenelli F, Gatti G, Viale G (2008) Clinicopathologic characteristics of invasive lobular carcinoma of the breast: results of an analysis of 530 cases from a single institution. Cancer 113(7):1511–1520. https://doi.org/10.1002/cncr.23811
Li CI, Uribe DJ, Daling JR (2005) Clinical characteristics of different histologic types of breast cancer. Br J Cancer 93(9):1046–1052. https://doi.org/10.1038/sj.bjc.6602787
Mellemkjaer L, Steding-Jessen M, Frederiksen K, Andersson M, Ejlertsen B, Jensen MB et al (2014) Risk of contralateral breast cancer after tamoxifen use among Danish women. Ann Epidemiol 24(11):843–848. https://doi.org/10.1016/j.annepidem.2014.08.003
Nichols HB, Berrington de González A, Lacey JV, Rosenberg PS, Anderson WF (2011) Declining incidence of contralateral breast cancer in the United States from 1975 to 2006. J Clin Oncol 29:1564–1569. https://doi.org/10.1200/JCO.2010.32.7395
Funding
No funding was used in the preparation, design, or writing of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
This study was epidemiological study using de-identified data from the SEER database. Therefore, consent for patient participation and study publication was not required. Because this study did not meet the definition of human subject research, the protocol was considered exempt from review from the Dana-Farber Cancer Institute Institutional Review Board (DFCI Protocol No.: 18-034).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sakai, T., Ozkurt, E., DeSantis, S. et al. National trends of synchronous bilateral breast cancer incidence in the United States. Breast Cancer Res Treat 178, 161–167 (2019). https://doi.org/10.1007/s10549-019-05363-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05363-0