Abstract
Purpose
To analyze the outcome of distal chevron metatarsal osteotomy (DCMO) with lateral release for moderate to severe hallux valgus patients aged 60 years or more.
Methods
Consecutive 77 DCMOs in 54 patients were evaluated. Average age at operation was 65.1 ± 4.3 (range 60~79) years; the mean follow-up period was 20.5 ± 14.2 (range 12~93) months. Hallux valgus angle (HVA), first to second inter-metatarsal angle (IMA), and lateral sesamoid grades were measured. Considering the weak bone quality of the patients, fixation failures such as pin migration, callus formation, delayed union, and first metatarsal bone shortening were reviewed. Osteoarthritis (OA) of the first metatarsophalangeal joint (MTPJ), limitation of 1st MTPJ motion (LOM), and transfer metatarsalgia were also reviewed.
Results
HVA, IMA, and sesamoid grades were improved at three months and final follow-up. The mean HVA was 36.9° ± 7.0° preoperatively and 6.8° ± 7.1° at final follow-up. The mean correction angle of HVA was 31.3° ± 8.5° at three months and 30.1° ± 8.9° at final follow-up. The mean IMA was 16.3° ± 3.0° pre-operatively and 7.7° ± 2.7° at final follow-up. Hallux varus deformity was observed in three feet. Instability of osteotomy site was observed in one foot. Mean metatarsal shortening length was 1.26 ± 2.1 mm at three month follow-up. There were no cases of transfer metatarsalgia after operation. OA was observed in four feet post-operatively. LOM was observed in ten feet (13.0%). There were no instances of re-fracture or avascular necrosis (AVN).
Conclusion
Despite concerns about aggravation of OA and fixation failure, distal chevron osteotomy with lateral release was safe on patients aged 60 years and over.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previously, distal chevron metatarsal osteotomy (DCMO) was considered contraindicated for patients aged more than 50 years in hallux valgus correction [1, 2]. In addition, until 1990s, several experts emphasized that DCMO is likely to fail in elderly patients [3]. However, DCMO became one of the most popular procedures ever performed even for moderate to severe deformities when combined with soft tissue procedures and Akin proximal phalangeal osteotomy [4,5,6]. Despite prior concerns about poor outcome of DCMO in elderly, satisfactory outcomes and infrequent avascular necrosis (AVN) occurrence were later reported [7, 8].
However, according to our literature review, there was a lack of technical points on DCMO performed in elderly. Moreover, no study focused on outcome of DCMO in elderly has been found. We assume that previous concerns about performing DCMO in elderly were mechanical failures (e.g., fixation failure, instability, non-union, delayed union, re-fracture, recurrence, and hallux varus deformity), presumably due to local porotic bone quality.
It is now commonly known that stable osteotomy and rapid bone healing is possible after DCMO, so that full weight-bearing ambulation immediately after surgery and simultaneous bilateral procedures are even possible [9, 10].Therefore, for more than a decade, we have been making efforts to safely correct elderly bones with DCMO with soft tissue procedures. In this study, we report outcome of DCMO for moderate to severe hallux valgus patients aged 60 years and over.
Patients and methods
We retrospectively reviewed consecutive 77 DCMOs in 54 patients aged 60 years or more performed by a senior foot surgeon between June 2010 and July 2018. Cases with short-term follow-up period less than 12 months, mild hallux valgus deformity with less than 25° of hallux valgus angle (HVA), rheumatoid foot, previous hallux operation, and concomitant operation of the other toe performed were excluded. Finally, 77 feet of 54 patients (5 men, 49 women) were enrolled in the analysis. Average age at the time of surgery was 65.1 ± 4.3 (range 60~79) years. Twenty-three patients of symptomatic bilateral hallux valgus underwent bilateral simultaneous operation (Table 1). The mean follow-up period was 20.5 ± 14.2 (range 12~93) months. Patients who underwent concomitant operation of the other ipsilateral toe, including 2nd toe Weil operation and hammer toe operation, were excluded to analyze metatarsal shortening lengths, callosities, and 2nd transfer lesions more precisely.
Surgical techniques
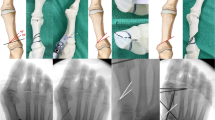
Initially, lateral release was performed with lateral incision. Adductor tenotomy and metatarso-sesamoid capsular release were performed as lateral soft tissue procedures, followed by gentle varus brisement. With varus stress test of 1st metatarsophalangeal joint (MTPJ), we assessed appropriate lateral release; we generally thought 20 degrees of varus shift was optimal. DCMO was performed through a medial approach. A T-shaped incision was then made at the medial capsule, and 5–8-mm-wide vertical limb of capsule was removed depending on the degree of deformity. Using an oscillating microsaw, a bunionectomy was performed parallel to the medial aspect of the first metatarsal shaft. Then, 60°-angled chevron osteotomy was performed at the centre of the first metatarsal head with the apex located at 5–7 mm distance from the articular surface, which is unconventionally more distal. A 5–8-mm lateral translation of the metatarsal head was performed. Distal metatarsal articular angle (DMAA) correction was simultaneously attempted by rotating the distal fragment medially for large DMAA cases. Two 1.1-mm Kirschner wires were inserted to fix the displaced fragment 2 cm proximal to the osteotomy site, and the remaining prominent bone was excised. Autologous bone graft was performed on 71 feet (92.2%) using bunionectomy bony fragment into the medullary bone. A capsulorrhaphy was performed while supinating the pronated toe.
The Akin phalangeal osteotomy was performed 7 mm distal to the proximal phalangeal base if residual deformity was present after DCMO and soft tissue procedure. This procedure was skipped in nine feet (11.7%). If there is no residual hallux pronation, a 1–3-mm medial closing wedge osteotomy was performed, with an attempt to greenstick the lateral cortex. For the residual pronated toe, de-rotation was performed after complete osteotomy. Fixation was performed using two 1.1-mm Kirschner wires.
Post-operative rehabilitations
A 1.5-cm gauze spacer was placed in the first web space for 6 weeks. Patients were allowed immediate full weight-bearing with hard-soled shoes. MTPJ motion exercise was provided at two weeks post-operatively to achieve full range of motion. Ordinary shoes were allowed approximately six weeks post-operatively. The Kirschner wires were removed eight to ten weeks post-operatively. Active sports activity was allowed two months post-operatively (Fig. 1).
Radiographic analysis
HVA and first-to-second inter-metatarsal angle (IMA) were measured pre-operatively, at two weeks, six weeks and three months post-operatively, and at the final follow-up with weight-bearing foot posteroanterior (PA) plain radiographs as described by Shima et al. [11] Subluxation of the lateral sesamoid was graded from 0 to 3 [12,13,14].
We measured the first metatarsal bone shortening (mm) by comparing length with that of the second metatarsal bone using Morton’s method [15, 16]. Due to concerns about local weak bone quality of the elderly, occurrence of imperfections, such as malunion, non-union, delayed union, bony callus formation, significant shortening, hardware failure, and re-fracture at the osteotomy site, were counted during the entire post-operative follow-up period, particularly until three months post-operatively.
Delayed union was defined as “no sufficient evidence of bone union after three months post-operatively.” Hardware failure, such as pin migration, pin breakage, cut through, and subsidence of pins, was defined as “any atraumatic mechanical instability.”
Osteoarthritis of 1st MTPJ and its change were evaluated throughout the follow-up radiographs as described by Coughlin et al. [17, 18].
Two orthopaedic surgeons measured all the radiographic parameters and reviewed radiographs twice at an interval of two weeks. The average of the four measurements was used for analysis.
Clinical analysis
We reviewed the range of motion (ROM) of 1st MTPJ including dorsiflexion and plantar flexion. We defined limitation of 1st MTPJ motion as “dorsiflexion of 50° or less” according to the descriptions by Gatt et al. and Laird et al. [19, 20].
Complications, such as AVN of the metatarsal head, recurrence of valgus deformity, iatrogenic hallux varus deformity, deep wound infection, and newly developed post-operative transfer lesion of the second or third metatarsal head, were also reviewed.
Statistical analysis
To evaluate whether the improvement of radiographic parameters is maintained after sufficient period, we conducted Wilcoxon signed rank-sum test for comparisons between pre-operative and each follow-up period. To avoid false positive results due to inflated type I error multiple testing, we applied Bonferroni correction, and p value less than 0.0167 (= 0.05/3) was considered statistically significant.
Results
The mean HVA improved significantly from 36.9° ± 7.0° (range 25~58°) pre-operatively to 3.1° ± 6.0° (range − 8~19°, p < 0.01) at 2 weeks, 4.9° ± 5.8° (range − 7~17°, p < 0.01) at six weeks, 5.5° ± 5.3° (range − 8~17°, p < 0.01) at three months post-operatively, and 6.8° ± 7.1° (range − 10~26°, p < 0.01) at final follow-up. The mean IMA improved as well from 16.3° ± 3.0° (range 8~23°) to 6.7° ± 2.4° (range 2~19°, p < 0.01), 7.7° ± 2.2° (range 3~15°, p < 0.01), 7.6° ± 2.7° (range 1~16°, p < 0.01), and 7.7° ± 2.7° (range 2~18°, p < 0.01). Sesamoid position also improved significantly (p < 0.05; Table 2). Mean correction angles of HVA were 31.3° ± 8.5° (range 14~56°) at 3 months and 30.1° ± 8.9° (range 7~54°) at final follow-up.
Recurrence of hallux valgus deformity defined as “correction loss more than 10°” was observed in seven feet (9.1%). Among them, final HVA > 20° was observed only in three feet. Their pre-operative HVA were 58°, 40°, and 50° each and improved to 25°, 21°, and 26°, respectively, with bunion pain remission. Therefore, no revisional operation was required.
Post-operative hallux varus deformity was observed in three feet of three patients. The final varus angle was 10° or less (6°, 9°, and 10° each). No corrective operation was required for hallux varus deformities.
The mean first metatarsal bone shortening (mm) values after DCMO measured using Morton’s method were 1.02 ± 2.13 mm at 2 weeks, 1.07 ± 2.29 mm at six weeks, and 1.26 ± 2.05 mm at 3 months. The differences between measurements at follow-up periods were not statistically significant (p > 0.05). Final first metatarsal bone shortening > 5 mm was observed in four feet (5.2%; measurements 8.8 mm (Fig. 2), 5.9 mm, 5.7 mm, and 5.2 mm). In addition, there was no newly presented second toe transfer lesion in these patients, and there was no delayed union or non-union either. One foot had early post-operative instability in osteotomized site with significant metatarsal shortening with callus formation and pin migration (Fig. 2).
Case 2, 64-year-old female hallux valgus patient with left hemi-paresthesia and unhealed chronic foot ulcer. (2-a) 1 cm × 2 cm sized superficial chronic ulcer on the plantar aspect of the medial sesamoid bone of 1st toe unhealed due to ipsilateral hemi-paresthesia consequently after spinal cord surgery. (2-b (I, II)) (I) Pre-operative standing posteroanterior (PA) radiograph, (II) immediate post-operative PA radiograph. (2-c (I, II)) Post-operative two weeks PA (I) and lateral (II) standing radiographs. Pin migration, metatarsal shortening, and dorsiflexion of distal osteotomized fragment were observed. We applied short leg cast for four weeks without re-fixation. (2-d) Final post-operative 38 months PA standing radiograph; despite the shortening of 1st metatarsal bone by approximately 9 mm as measured using Morton’s measurement method, asymptomatic full ROM of 1st MTPJ was obtained without occurrence of a second toe transfer lesion or callosity. Patient was very satisfied with complete ulcer healing
Pre-operative callosities under second to fifth metatarsal head were observed in 35 feet (45.5%), 34 of which resolved during follow-up, and although one foot had a residual painless callosity, there was no aggravation or symptom. There was no new post-operative transfer lesion or symptomatic callosity in any enrolled patient.
Significant 1st MTPJ OA, which was graded 1 or more as described by Coughlin et al. [17, 18], was observed in four feet of three patients (Table 3). A 67-year-old female patient who had a pre-operative subluxated 1st MTPJ OA had satisfactory treatment outcome without transfer metatarsalgia or hallux pain despite minimal aggravation of OA and some limitation of 1st MTPJ motion (LOM) (dorsiflexion 50°, plantar flexion 10°) remaining post-operatively until the final follow-up (Fig. 3). In other patients, aggravation of 1st MTPJ OA was not significant during the entire follow-up period. Patient 3 (Table 3) had bilateral hallux valgus deformities with both sided 1st MTPJ OA; clinical and radiographic outcomes were satisfactory.
Case 3, A 67-year-old female patient with pre-operative 1st MTPJ arthritis with subluxation. Minimal aggravation of 1st MTPJ OA was observed in serial radiographs of post-operative follow-up. (3-a) Moderate HV with 1st MTPJ subluxation and suspicious osteoarthritis was observed in pre-operative PA standing plain radiograph. (3-b) Restoration of 1st MTPJ congruity after DCMO was obtained, but mild osteoarthritic findings could be found on post-operative 3 weeks standing PA plain radiograph. (3-c) Joint space narrowed and osteophyte increased during serial follow-ups. Aggravation of 1st MTPJ OA was suspected on final post-operative 45 months standing PA plain radiograph
Limitation of 1st MTPJ motion was observed in 10 feet (13.0%). However, degree of LOM was not clinically significant in all patients. Non-union, delayed union, re-fracture, AVN, deep wound infection, or any revisional surgery was absent during the entire follow-up period.
Discussion
We analyzed the results of DCMO in patients (age ≥ 60 years) requiring hallux valgus correction. Considering that DCMO was performed on patients over 60 years old, we focused on issues of weak bone quality, osteoarthritis, and susceptibility to mechanical failures. Despite prior concerns about mechanical failures in elderly, there was only one representative case out of the 77 feet that showed instability of osteotomy. The result may advocate the safety and stability of chevron osteotomy even for the elderly with weak bones.
Furthermore, with combination of lateral soft tissue releases and Akin osteotomies, DCMO proved its efficacy even for moderate to severe deformities. In this study, all of the 77 feet had more than 25 of HVA. The biggest correction angle was 54° (HVA in preoperative 54°, final 0° each). We assume that lateral soft tissue release contributed to the good correction power [9, 14]. Deenik et al. reported a recurrence rate of 7% with DCMO, which had comparable result with ours (9%), even though we enrolled older patient group [21].
We performed lateral metatarso-sesamoidal capsule release and adductor hallucis tenotomy following gentle varus brisement until reaching 20° as lateral release procedure while preserving deep transverse metatarsal ligament and plantar capsule to minimize occurrence of AVN of the first metatarsal head and hallux varus deformity [22, 23].
Twenty-three patients underwent bilateral DCMO simultaneously. They also maintained acceptable correction during their follow-up without mechanical failure or the need for revisional operation, even though we allowed the same early weight-bearing ambulation protocol. We think this result supports the inherent stability of DCMO. However, further comparative investigations on “both side correction in same time versus unilateral operation” are necessary. In elderly patients, early post-operative ambulation may have a marked beneficial effect on comorbid medical problems. Thus, we allowed immediate full weight-bearing with hard-soled shoes. Despite allowing early ambulation, we could achieve comparable radiological and clinical outcomes as previous studies [6, 24].
We think the inherent stability of chevron osteotomy has advantage in the porotic bones, and the osteotomy level has greater stability on metatarsal head than on metatarsal shaft. Thus, we located the apex of chevron osteotomy more distally considering the local porotic bone quality. There was no AVN of metatarsal head even with distalized chevron apex. Additional auto-bone packing with resected bone into the medullary space of osteotomy site could support better stability.
Even in weak bone of the elderly, two crossed 1.1-mm Kirschner wires were successfully used for each fixation of chevron osteotomy and Akin osteotomy. We think Kirschner wire osteosynthesis is appropriate for weak bone of the elderly for several reasons. First, several studies showed biomechanically equivalent or superior fixation results of crossed two Kirschner wires to those of screws or staples for chevron osteotomy or Akin osteotomy [25, 26]. Second, pin fixation is easier than screw fixation of the small bone. Third, during inter-fragmentary fixation, position of corrected capital fragment can be maintained more precisely with pins than with screws. Forth, Kirshner wire is inexpensive to use.
In this study, the mean 1st metatarsal bone shortening (mm) after DCMO measured using Morton’s method were 1.02 ± 2.13 mm, 1.07 ± 2.29 mm, and 1.26 ± 2.05 mm at post-operative two weeks, six weeks, and three months, respectively. Measurement error could take place due to the crudeness of digital measurement method in PACS (picture archiving communication system). It is difficult to accurately measure length less than 1 mm. Thus, although these figures above showed a seemingly increasing trend, the differences between the follow-up periods were neither statistically (p > 0.05) nor clinically (< 0.5 mm) significant. Additionally, some extreme outliers, such as case 2 (Fig. 2), could exaggerate the mean shortening length in subsequent follow-up visits. There were no post-operative transfer lesions, and there was no notable correlation between first metatarsal bone shortening and transfer lesion. We believe that transfer metatarsalgia after DCMO rarely occurs with the correction of a pronated first toe and functional restoration of the hallux.
In the elderly, pre-operative OA of 1st MTPJ is not relatively rare. Despite the concerns about aggravation of pre-existing OA, 73 feet out of 77 feet had no occurrence of OA until final follow-up. We think DCMO can be indicated for patients with OA of 1st MTPJ in the stage of mild radiographic change with insignificant LOM. OA of 1st MTPJ was radiographically observed in four feet (5.2%) pre-operatively, but all of them were grade 1 pre-operatively according to the grading described by Coughlin et al. In addition, although there was a patient in whom OA of one foot aggravated to radiographically confirmed grade 2, she was still satisfied with the acceptable ROM without pain (Fig. 3). We could not find any radiographic or clinical inferiority in OA patients.
Limitation of 1st MTPJ motion was observed in seven patients (9.1%) at the final follow-up despite our 1st MTPJ ROM exercise education. However, all these cases were of painless stiffness which has more than 30° of dorsiflexion.
In conclusion, despite previous concerns about weak bone and osteoarthritis, distal chevron osteotomy with appropriate lateral soft tissue release could achieve successful correction of moderate to severe hallux valgus in patients aged 60 or more.
References
Corless JR (1976) A modification of the Mitchell procedure (abstract). J Bone Joint Surg B 58:138
Johnson KA, Cofield RH, Morrey BF (1979) Chevron osteotomy for hallux valgus. Clin Orthop Relat Res:44–47. https://doi.org/10.1097/00003086-197907000-00007
Coughlin MJ (1995) Roger A. Mann Award. Juvenile hallux valgus: etiology and treatment. Foot Ankle Int 16:682–697. https://doi.org/10.1177/107110079501601104
Easley ME, Trnka HJ (2007) Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int 28:748–758. https://doi.org/10.3113/FAI.2007.0748
Al-Nammari SS, Christofi T, Clark C (2015) Double first metatarsal and akin osteotomy for severe hallux valgus. Foot Ankle Int 36:1215–1222. https://doi.org/10.1177/1071100715589173
van Groningen B, van der Steen MC, Reijman M, Bos J, Hendriks JG (2016) Outcomes in chevron osteotomy for hallux valgus in a large cohort. Foot (Edinb) 29:18–24. https://doi.org/10.1016/j.foot.2016.09.002
Schneider W, Knahr K (2002) Keller procedure and chevron osteotomy in hallux valgus: five-year results of different surgical philosophies in comparable collectives. Foot Ankle Int 23:321–329. https://doi.org/10.1177/107110070202300406
Schneider W, Aigner N, Pinggera O, Knahr K (2004) Chevron osteotomy in hallux valgus. Ten-year results of 112 cases. J Bone Joint Surg (Br) 86:1016–1020
Choi YR, Lee HS, Jeong JJ et al (2012) Hallux valgus correction using transarticular lateral release with distal chevron osteotomy. Foot Ankle Int 33:838–843. https://doi.org/10.3113/FAI.2012.0838
Lee HJ, Chung JW, Chu IT, Kim YC (2010) Comparison of distal chevron osteotomy with and without lateral soft tissue release for the treatment of hallux valgus. Foot Ankle Int 31:291–295. https://doi.org/10.3113/FAI.2010.0291
Shima H, Okuda R, Yasuda T, Jotoku T, Kitano N, Kinoshita M (2009) Radiographic measurements in patients with hallux valgus before and after proximal crescentic osteotomy. J Bone Joint Surg Am 91:1369–1376. https://doi.org/10.2106/JBJS.H.00483
Panchani S, Reading J, Mehta J (2016) Inter and intra-observer reliability in assessment of the position of the lateral sesamoid in determining the severity of hallux valgus. Foot (Edinb) 27:59–61. https://doi.org/10.1016/j.foot.2015.10.001
Agrawal Y, Desai A, Mehta J (2011) Lateral sesamoid position in hallux valgus: correlation with the conventional radiological assessment. Foot Ankle Surg 17:308–311. https://doi.org/10.1016/j.fas.2011.01.001
Ahn JY, Lee HS, Chun H et al (2013) Comparison of open lateral release and transarticular lateral release in distal chevron metatarsal osteotomy for hallux valgus correction. Int Orthop 37:1781–1787. https://doi.org/10.1007/s00264-013-2023-1
Ahn J, Lee HS, Seo JH, Kim JY (2016) Second metatarsal transfer lesions due to first metatarsal shortening after distal chevron metatarsal osteotomy for hallux valgus. Foot Ankle Int 37:589–595. https://doi.org/10.1177/1071100715627350
Morton DJ (1964, New York) The human foot, its evolution, physiology, and functional disorders. Hafner Pub. Co
Coughlin MJ, Shurnas PS (2003) Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am 85:2072–2088
Coughlin MJ, Shurnas PS (2003) Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int 24:731–743. https://doi.org/10.1177/107110070302401002
Gatt A, Mifsud T, Chockalingam N (2014) Severity of pronation and classification of first metatarsophalangeal joint dorsiflexion increases the validity of the Hubscher Manoeuvre for the diagnosis of functional hallux limitus. Foot (Edinb) 24:62–65. https://doi.org/10.1016/j.foot.2014.03.001
Laird PO (1972) Functional hallux limitus. Illinois Podiatrists 9:4
Deenik A, van Mameren H, de Visser E, de Waal MM, Draijer F, de Bie R (2008) Equivalent correction in scarf and chevron osteotomy in moderate and severe hallux valgus: a randomized controlled trial. Foot Ankle Int 29:1209–1215. https://doi.org/10.3113/FAI.2008.1209
Schneider W (2013) Distal soft tissue procedure in hallux valgus surgery: biomechanical background and technique. Int Orthop 37:1669–1675. https://doi.org/10.1007/s00264-013-1959-5
Schneider W (2012) Influence of different anatomical structures on distal soft tissue procedure in hallux valgus surgery. Foot Ankle Int 33:991–996. https://doi.org/10.3113/FAI.2012.0991
Boychenko AV, Solomin LN, Parfeyev SG, Obukhov IE, Belokrylova MS, Davidov DV (2015) Efficacy of bilateral simultaneous hallux valgus correction compared to unilateral. Foot Ankle Int 36:1339–1343. https://doi.org/10.1177/1071100715589174
Chacon Y, Fallat LM, Dau N, Bir C (2012) Biomechanical comparison of internal fixation techniques for the Akin osteotomy of the proximal phalanx. J Foot Ankle Surg 51:561–565. https://doi.org/10.1053/j.jfas.2012.05.001
Trost M, Bredow J, Boese CK et al (2018) Biomechanical comparison of fixation with a single screw versus two Kirschner wires in distal Chevron osteotomies of the first metatarsal: a cadaver study. J Foot Ankle Surg 57:95–99. https://doi.org/10.1053/j.jfas.2017.08.014
Mann RA (1990) Decision-making in bunion surgery. Instr Course Lect 39:3–13
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence: level 4
Rights and permissions
About this article
Cite this article
Seo, J., Lee, H., Choi, Y. et al. Distal chevron osteotomy with lateral release for moderate to severe hallux valgus patients aged sixty years and over. International Orthopaedics (SICOT) 44, 1099–1105 (2020). https://doi.org/10.1007/s00264-020-04562-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04562-5