Abstract
Purpose
The purpose of this study was to evaluate the radiographic and clinical outcomes of patients with hallux valgus (HV) with concomitant metatarsus adductus (MA) treated with distal chevron metatarsal osteotomy (DCMO), without any procedure for the second or third metatarsal.
Methods
A multicentre retrospective study involving four hospitals was conducted. A total of 45 feet from 38 patients who had received DCMO for HV with MA with at least one year post-operative follow-up were analysed. HV angle (HVâ), inter-metatarsal angle (IMâ), MA angle (MAâ), and the lateral sesamoid grade were measured. Foot function index (FFI) and visual analogue scale (VAS) were recorded. Patients were divided into mild (18° ≤ MAâ < 20°) and moderate (20° ≤ MAâ) MA groups, and results were compared.
Results
The mean HVâ and IMâ improved significantly from 35.1° and 14.4° pre-operatively to 10.6° and 7.1° one year post-operatively (p < 0.001). There were no differences in pre-operative HVâ, IMâ, or the sesamoid grade, and also no difference in post-operative HVâ or the sesamoid grade between mild and moderate MA groups. Only the mean post-operative IMâ showed a difference between the two groups (8.3° vs. 6.3°; p = 0.019). All clauses of FFI and VAS improved significantly (p < 0.001). When the extent of improvement was compared between the two groups, there were no significant differences in any category (p > 0.05). The total rate of recurrence (HVâ ≥ 20°) was 11.1% (5/45), and although the moderate group (4/29, 13.8%) had a higher proportion than the mild group (1/16, 6.3%), this was not statistically significant (p = 0.641).
Conclusion
DCMO for patients with HV with MA had satisfactory radiographic and clinical outcomes with minimal recurrence. Except in cases of severe combined deformity, we recommend performing DCMO alone without any additional procedure or manipulation of the other metatarsals as a viable treatment option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metatarsus adductus (MA) is a transverse plane deformity of the forefoot with the metatarsus in adduction. It is associated with hallux valgus (HV) and is a risk factor for recurrence after corrective surgery for HV [1, 2].
Since MA can cause the gap between the first and second metatarsals to narrow, it can present a challenge for patients requiring correction of the first metatarsal. Various methods have been used for surgical correction of HV with MA, including scarf osteotomy, proximal first metatarsal osteotomy, first tarsometatarsal joint arthrodesis, and additional osteotomies for the second and third metatarsals [3,4,5,6,7,8]. However, the published literature on this topic is limited, and there are no clear guidelines for the surgical method to be employed depending on the severity of the MA deformity.
Distal chevron metatarsal osteotomy (DCMO) has traditionally been recommended for correction of mild HV deformity [9]. However, it has become a popular procedure even for moderate to severe deformities when combined with soft tissue procedures and Akin osteotomy [10,11,12]. Stable osteotomy and rapid bone healing are possible after DCMO so that full weight-bearing ambulation immediately after surgery is permissible [13,14,15].
DCMO is an operative technique for osteotomy of the first metatarsal laterally displacing the distal part of the osteotomy site. Since it does not entail any procedure for the second metatarsal, it is not a method for correcting the MA angle (MAâ). Also, it is a pure translation technique, with the amount of translation being limited by the width of the metatarsal bone and the remaining contact surface [16]. There are currently no available data regarding radiographic changes, clinical outcomes, or recurrence rates after DCMO surgery for correction of HV with MA.
The aims of this multicentre study were to investigate the results of DCMO for HV with MA by evaluating the radiographic results and clinical outcomes after DCMO for HV with MA. Furthermore, we divided subjects into mild and moderate groups depending on the severity of MA and compared the results after DCMO.
Materials and methods
This multicentre retrospective study was conducted after approval by the institutional review board. Data were collected from four hospitals for patients with HV with MA who had undergone DCMO from 2010 to 2018. Patients aged above 19 years with available weight-bearing radiographs pre-operatively, three months post-operatively, and one year post-operatively were included. Patients who received DCMO with concurrent Akin osteotomy were included, but those who received any other form of surgical procedure for the second or third metatarsal were excluded. Other exclusion criteria were patients with a follow-up period < one year, missing radiographs three month or one year post-operatively, unavailable clinical outcome scores, presence of rheumatoid arthritis, and a history of ipsilateral foot and ankle surgery.
To set an adequate criterion for MAâ, the available literature was thoroughly reviewed for reference. The normal range for MAâ has been reported as being between 10 and 21° [17,18,19]. In a study involving newborns, MAâ measured close to 25° but decreased to 15° by adulthood [1, 17, 19]. Depending on the study, the method for measuring MAâ and its normal range showed variability and inconsistency, and there is no widely accepted consensus on determining and classifying the severity of MA. Yu et al. classified metatarsus adductus into three categories using a traditional method, with 15 to 20° as mild, 21 to 25° as moderate, and greater than 25° as severe [20]. This classification system lacks clinical evidence and does not correlate with the disease prognosis. In this multicentre study, a total of 312 DCMO cases for HV performed from 2010 to 2018 across four institutions had both pre-operative and one year post-operative radiographs available. The number of cases with a MAâ of 15° or higher was 142 (45.5%), 18° or higher was 88 (28.2%), and 20° or higher was 61 (19.6%). Reaux et al. reported that in a study of 230 patients with HV, the incidence of associated MA was 35% [1]. Aiyer et al. published a study of 587 patients with HV with a 29.5% incidence of MA, and Loh et al. reported a similar figure in a study of 206 patients with HV with 33% prevalence of MA [5, 8]. Previous studies that had analysed the results of surgery for HV with MA had set the criteria for MA as MAâ of 15° or higher [3] or 20° or higher [5, 7]. Referencing the previously published literature and considering that setting the cutoff at 15° or 20° increased or decreased the proportion of MA too dramatically, criteria for MA were defined as MAâ of 18° or higher for this study. Of the 88 cases with MAâ ≥ 18°, 45 feet from 38 patients were enrolled for the final analysis after applying the aforementioned exclusion criteria. There were two men and 36 women, with a mean age of 57.9 years (range, 19–77 years) and a mean follow-up period of 20.5 months (range, 12–87 months).
Radiographic analysis
Hallux valgus angle (HVâ), first-to-second inter-metatarsal angle (IMâ), and MAâ were measured on weight-bearing foot anteroposterior radiographs. Subluxation of the lateral sesamoid was classified into stages 0–3 [21,22,23].
MAâ was measured using the modified Sgarlato’s method [18]. A line was drawn connecting the most lateral points of the fifth metatarso-cuboid and calcaneo-cuboid joints, and another line was drawn connecting the most medial points of the talo-navicular and medial cuneiform -first metatarsal joints. A third line was made to connect the midpoint of the first two lines. A fourth line, drawn perpendicular to the third, was defined as the longitudinal axis of the lesser tarsus. MAâ was defined as the angle between the longitudinal axis of the lesser tarsus and the longitudinal axis of the second metatarsal (Fig. 1).
Modified Sgarlato’s angle measurement. The line (a) extends between the most lateral point of the fifth metatarso-cuboid and the calcaneo-cuboid joints. The line (b) extends between the most medial point of the talo-navicular and the medial cuneiform-first metatarsal joints. The line (c) extends between midpoints of lines (a) and (b). The line (d) represents the longitudinal axis of the second metatarsal. The line (e) is perpendicular to line (c) and represents the longitudinal axis of the lesser tarsus. Sgarlato’s angle is between the lines (d) and (e). In this case, the angle was 25.5°
Patients with MAâ < 20° were classified as mild, and those with MAâ ≥ 20° were classified as moderate. Of a total of 45 patients, 16 were in the mild group, and 29 were in the moderate group.
Recurrence of HV was defined as HVâ of 20° or higher one year post-operatively [5,6,7].
Clinical analysis
Foot function index (FFI), visual analogue scale (VAS), and subjective patient satisfaction were recorded pre-operatively and one year post-operatively. FFI consists of 23 questionnaires, including subscales for pain (nine elements), disability (nine elements), and activity limitation (five elements) [24]. The 100-mm VAS is a validated self-assessment tool for evaluating pain [25]. Patients were also asked to categorise their current state as ‘very satisfied’, ‘satisfied’, ‘fair’, ‘dissatisfied’, or ‘very dissatisfied’ before surgery and one year after surgery.
Operative technique
Data was collected from four hospitals, and all surgeries were performed according to a standardised protocol, as described below, by orthopaedic surgeons with a foot and ankle fellowship.
The patient was placed in the supine position. For all cases, initial lateral release of the first metatarsal was performed via a lateral incision. After adductor tenotomy and metatarso-sesamoid capsular release for lateral soft tissue release, gentle varus brisement was performed. To evaluate the appropriate amount of lateral release, the varus stress test of the first metatarsophalangeal joint (MTPJ) was performed, with approximately 20° of varus shift deemed optimal. With the medial approach, a T-shaped incision was made at the medial capsule, and depending on the severity of the deformity, a 5–8-mm-wide vertical limb of the capsule was removed. Bunionectomy was performed using an oscillating microsaw, cutting parallel to the medial aspect of the first metatarsal shaft. For the 60° chevron osteotomy, the apex was placed approximately 5–7 mm from the articular surface at the centre of the first metatarsal head, and following the osteotomy, the metatarsal head was translated laterally by 5–9 mm. For patients with a large distal metatarsal articular angle (DMAâ), simultaneous correction of DMAâ was attempted by rotating the distal fragment medially [26]. To fix the displaced distal fragment, two 1.1-mm Kirschner wires were inserted from a point 2 cm proximal to the osteotomy site, and any remaining prominent bone was excised. If there was a cancellous bone defect around the osteotomy site, or a bone cyst, or a low density of cancellous bone, autologous bone graft was applied using the bunionectomied bone or the removed fragments of the proximal bony prominence. Capsulorrhaphy was performed with the pronated toe in supination. If residual deformity persisted after DCMO and accompanying soft tissue procedures, Akin phalangeal osteotomy was performed, according to the judgment of the surgeon. Osteotomy was performed 7 mm distal to the proximal phalangeal base, and for patients with no residual hallux pronation, 1–3-mm medial closing wedge osteotomy was indicated with an attempt to greenstick the lateral cortex. For patients with residual toe pronation, complete osteotomy was performed, followed by derotation. Fixation was done using two 1.1-mm Kirschner wires. The Akin procedure was skipped in five feet (11.1%).
Post-operative rehabilitation
For six weeks following surgery, a 1.5-cm gauze spacer was placed in the first web space. Immediate full weight-bearing and ambulation with hard-soled shoes were allowed. At two weeks post-operatively, MTPJ motion exercise was provided to achieve the full range of motion. At six weeks post-operatively, ordinary shoes were permitted. The Kirschner wires were removed eight to 12 weeks post-operatively. Return to normal sports activity was allowed two months post-operatively.
Statistical analysis
Student’s t-test was used to compare radiographic outcomes before surgery, three months post-operatively, and one year post-operatively. When the difference between the samples’ means could not be assumed to be normally distributed, Wilcoxon signed-rank test was used. For comparison of clinical outcomes before surgery and one year after surgery, Wilcoxon signed-rank test was used. To evaluate differences between mild and moderate groups before surgery and one year after surgery, Wilcoxon rank-sum test was applied. Fisher’s exact test was used to examine the recurrence rate in both groups. In all instances, p-value < 0.05 was considered to be statistically significant. All analyses were performed using SAS version 9.4 (SAS Institute, Inc., Cary, NC USA and R statistical software, version 3.6.3).
Results
Radiographic outcomes
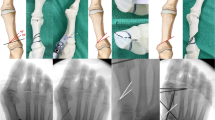
The mean HVâ improved significantly from 35.1° (range, 11.5–58.5°) pre-operatively to 11.0° (range, − 4.0–34.6°, p < 0.001) three months post-operatively, and 10.6° (range, − 2.0–29.0°, p < 0.001) one year post-operatively. The mean IMâ improved from 14.4° (range, 7.1–23.0°) pre-operatively to 7.8° (range, 1.0–26.9°, p < 0.001) three months post-operatively and 7.1° (range, 2.0–12.0°, p < 0.001) one year post-operatively. Lateral sesamoid position also showed a statistically significant improvement (p < 0.001). Meanwhile, the average MMA was recorded as 21.5° (range, 18.1–38.8°) pre-operatively, 21.5° (range, 17.1–38.2°, p = 0.767) three months post-operatively, and 21.2° (range, 16.0–37.9°, p = 0.218) at the final follow-up, showing no statistically significant change (Table 1) (Fig. 2).
(a) Pre-operative, (b) 2 weeks post-operative, and (c) 1 year post-operative weight-bearing radiographs of the 60-year-old female patient with a hallux valgus deformity and concomitant metatarsus adductus. Pre-operatively, the patient had a hallux valgus angle (HVâ) of 48.0°, an intermetatarsal angle (IMâ) of 16.1°, and a metatarsus adductus angle (MAâ) of 25.0°. Post-operatively, the patient had a HVâ of 10.0°, an IMâ of 4.0°, and a MMA of 23.5°
There were no statistically significant differences in the pre-operative mean HVâ, IMâ, or the sesamoid grade between mild and moderate MA groups (p = 0.126, 0.924, and 0.689, respectively). At one year post-operatively, there were still no significant differences in the mean HVâ or sesamoid grade between the two groups (p = 0.713 and 0.403, respectively), but the mean IMâ differed between mild (8.3°, range, 5.0–12.0°) and moderate MA (6.3°, range 2.0–11.0°) groups (p = 0.019). When changes in radiographic parameters from the pre-operative period to one year post-operatively were examined, only IMâ was significantly different between the mild and moderate MA groups (median, − 5.50° vs. − 7.40°; p = 0.036), while changes in HVâ, MAâ, and the sesamoid position were statistically insignificant (p = 0.056, 0.361, and 0.225, respectively; Table 2).
Clinical outcomes
All clauses of FFI and VAS improved significantly one year post-operatively compared to pre-operatively (all p < 0.001; Table 3). Subjective patient satisfaction, which was ‘very dissatisfied’ for 21 patients and ‘dissatisfied’ for 24 patients before surgery, improved to ‘very satisfied’ for 24 patients, ‘satisfied’ for 16 patients, and ‘fair’ for five patients post-operatively. When mild and moderate MA groups were divided separately and the analysis performed for each group, results also showed a significant improvement in all outcomes one year post-operatively. When the extent of improvement was compared between the two groups, there were no significant differences in any category (all p > 0.05; Table 4).
Recurrence rates
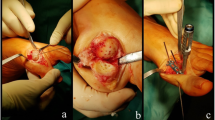
Recurrence was defined as a measured HVâ ≥ 20° one year post-operatively, and five cases (11.1%) were identified. The pre-operative HVâ for each case was 43.4°, 34°, 58°, 57°, and 58.5°, which improved to 20.5°, 21°, 21°, 29°, and 21.5°, respectively. None of the five patients with recurrence complained of bunion pain one year after surgery, and none required revision surgery (Fig. 3).
Recurrence of hallux valgus deformity in a 72-year-old female patient. (a) Pre-operatively, the patient had a hallux valgus angle (HVâ) of 58.5° and a metatarsus adductus angle (MAâ) of 38.8°. (b) One year post-operatively, the patient had a HVâ of 21.5° and a MMA of 37.9°. Although this case was classified as a recurrence due to a measured HVâ ≥ 20° 1 year post-operatively, she did not complain of any symptoms and rated subjective patient satisfaction to be ‘very satisfied’, so revision surgery was unnecessary
Although there were nearly double the proportion of recurred cases in the moderate MA group (13.8%, 4/26 feet) compared to the mild MA group (6.3%, 1/19 feet), this difference was not statistically significant (p = 0.641).
Discussion
This was a multicentre retrospective study conducted with data collected from four hospitals, focusing on outcomes of patients with HV and MA who received DCMO surgery and had a minimum one year post-operative follow-up. Corrective surgery was performed only for the first metatarsal, with no additional procedures or manipulation of the second metatarsal, and results showed significant radiographic and clinical improvements.
Due to the limited contact surface of DCMO, previous literature has indicated the procedure for cases of HVâ < 30° and IMâ < 15° [27,28,29]. However, in numerous recent articles, DCMO with concurrent lateral soft tissue release and Akin osteotomy has been reported to have favourable outcomes [30,31,32,33]. In our study, we performed lateral release procedures on all patients, and Akin osteotomies in the majority of cases (40/45 feet, 88.9%). Additionally, in a number of cases with a large DMAâ, medial rotation of distal fragment was performed by pulling the lateral side and impacting the medial side of the distal fragment, for the purpose of additional correction [26]. This procedure for DMAâ correction has been attempted in previous studies [26, 27]. We estimate that the combination of lateral release and medial rotation procedures with DCMO contributed considerably to the satisfactory correction results of our study.
Another aim of this study was to divide patients into mild and moderate MA groups and compare the results of DCMO. In the radiographic analysis, all parameters excluding MAâ significantly improved after surgery in both groups. There were no differences in pre-operative HVâ, IMâ, or the sesamoid grade between the two groups, and no differences in post-operative HVâ or the sesamoid grade between the two groups. Only the post-operative IMâ showed a statistically significantly difference, and in fact the average post-operative IMâ was lower and amount of post-operative IMâ correction greater in the moderate MA group. Clinical outcomes improved in both groups after DCMO surgery, but differences between the mild and moderate groups were statistically insignificant. In summary, even when DCMO was administered in a patient group with a relatively more severe MA, results were not inferior radiologically or clinically.
The recurrence rate was higher in the moderate MA group, although it was not statistically significant. Of the total five recurred cases (11.1%), one case (6.3%) occurred in the mild MA group and four cases (13.8%) occurred in the moderate MA group.
Aiyer et al. compared the recurrence rates of patients with HV with and without MA after corrective surgery. The rate was 28.9% for patients with HV with MA and 15.2% for those without MA [34]. This study also defined recurrence as a post-operative HVâ > 20°. However, the authors employed multiple surgical methods, including the Lapidus procedure, proximal first metatarsal osteotomy, and distal first metatarsal osteotomy, and did not specify whether lateral release was performed or not. Shima et al. performed proximal crescentic osteotomy of the first metatarsal and abduction osteotomy of the second and third metatarsals for patients with HV with moderate to severe MA (mean MAâ, 24.6°) and reported a recurrence rate of 19.0% [6]. Conti et al. divided patients with HV who had received the Lapidus procedure into an HV only group and HV with MA group (mean MAâ, 23.8°), and the recurrence rate was 6.6% for the HV only group and 17.1% for the HV with MA group [7].
Numerous studies reported recurrences after DCMO for patients with HV. Deenik et al. noted a recurrence rate of 7% after DCMO [31], and a study by Lee et al. showed a recurrence rate of 9% after DCMO for moderate to severe HV in patients aged over 60 years [13].
In this current study, the recurrence rate was slightly lower than previously published research on patients with HV with MA treated with various surgical methods and slightly higher than other studies focusing on DCMO for patients with HV with or without MA. The mean MAâ was 21.5° when both groups were combined and 22.8° in the moderate MA group, which is a slightly lower mean MAâ than other studies with a higher recurrence rate. Although there were five cases of recurrence, none required re-operation, and subjective patient satisfaction was acceptable, with two patients ‘very satisfied’, two patients ‘satisfied’, and one patient ‘fair’.
For HV with MA, many reports on various surgical methods and their results have been published. Opinions differ on the optimal correction method of the first metatarsal. Aiyer et al. published data in 2014 on surgically treating 173 patients with HV with MA, 35 with the Lapidus procedure, 17 with proximal first metatarsal osteotomy, and 121 with distal first metatarsal osteotomy, but there were no comparisons among surgical methods [5]. In a study by Loh et al., 206 patients treated by scarf osteotomy were divided into MA and control groups [8]. Results were similar for both groups, and the authors concluded that MA did not predispose the patient to poorer functional outcome after scarf osteotomy. In a recent 2021 study, results of the modified Lapidus procedure were compared among patients with HV with and without MA. Despite the MA group showing inferior results, outcomes were more favourable than other reported methods. Therefore, the authors suggested the modified Lapidus procedure as a good option [7].
Controversy exists on whether or not additional bony procedures are necessary following the first metatarsal osteotomy. Shima et al. reported outcomes of proximal crescentic osteotomy of the first metatarsal and abduction osteotomy of the proximal third of the second and third metatarsals [6]. Sharma advocated a more radical treatment, including first TMT arthrodesis, second and third metatarsal base osteotomies with neck Weil osteotomies, and even calcaneal osteotomy for cases of severe HV with MA [4].
In our study, participating surgeons across four hospitals treated patients with HV with MA with DCMO and lateral release and did not perform any additional bony procedure, except for Akin osteotomy. In some cases with a large DMAâ, translation with medial rotation of the distal fragment after chevron osteotomy was performed additionally. Radiographic and clinical outcomes improved significantly after surgery, and the recurrence rate was relatively lower than previously published literature. When patients were divided into mild and moderate MA groups for further analyses, the moderate MA group did not show inferior results and for some parameters, actually showed more improvement than the mild MA group.
Our study had several limitations. First, it was conducted retrospectively for patients who had received DCMO surgery and, thus, may be predisposed to selection bias. Moreover, the number of enrolled patients was relatively small. Many patients were lost to follow-up or had missing post-operative radiographic or clinical data. However, it was a conjoined effort by four different hospitals to collect data on a comparatively rare disease entity, and we believe the results offer meaningful insight. Second, a number of factors may have contributed to the satisfactory results of the moderate MA group. While all patients received lateral soft tissue release, there is a possibility that severe cases underwent additional tenotomies or more extensive soft tissue release procedures. Also, medial rotation and impaction of the distal fragment after chevron osteotomy were probably performed more often in patients with a larger MAâ. However, these instances were not subdivided and analysed any further, and this may have created a bias when comparing the results of the two groups. If a subsequent investigation was to compare and analyse the effects of a distal fragment medial rotation procedure, it would remedy part of the shortcomings of this study, and contribute further to advancing the DCMO technique for hallux valgus correction. Third, although we presented favourable results for DCMO, similar to other studies, we did not compare outcomes among different surgical methods, failing to provide guidelines for a certain operative procedure being superior to another. Further research, such as a randomised trial, comparing multiple surgical methods may provide valuable insight.
Conclusion
Patients with HV and concomitant MA have been reported to have poor results after surgery and high recurrent rates. Therefore, surgeons face a challenge when deciding on the treatment. This multicentre study showed that performing DCMO for patients with HV with MA had satisfactory radiographic and clinical outcomes with minimal recurrence. Except in cases of severe combined deformity, we recommend DCMO alone without any additional procedure or manipulation of the other metatarsals as a viable treatment option.
Availability of data and material (data transparency)
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Code availability (software application or custom code)
Not applicable.
References
La Reaux RL, Lee BR (1987) Metatarsus adductus and hallux abducto valgus: their correlation. J Foot Surg 26:304–308
Palestro CJ, Caprioli R, Love C, Richardson HL, Kipper SL, Weiland FL, Tomas MB (2003) Rapid diagnosis of pedal osteomyelitis in diabetics with a technetium-99m-labeled monoclonal antigranulocyte antibody. J Foot Ankle Surg 42:2–8. https://doi.org/10.1053/jfas.2003.50002
Larholt J, Kilmartin TE (2010) Rotational scarf and akin osteotomy for correction of hallux valgus associated with metatarsus adductus. Foot Ankle Int 31:220–228. https://doi.org/10.3113/FAI.2010.0220
Sharma J, Aydogan U (2015) Algorithm for severe hallux valgus associated with metatarsus adductus. Foot Ankle Int 36:1499–1503. https://doi.org/10.1177/1071100715593799
Aiyer AA, Shariff R, Ying L, Shub J, Myerson MS (2014) Prevalence of metatarsus adductus in patients undergoing hallux valgus surgery. Foot Ankle Int 35:1292–1297. https://doi.org/10.1177/1071100714551022
Shima H, Okuda R, Yasuda T, Mori K, Kizawa M, Tsujinaka S, Neo M (2019) Operative treatment for hallux valgus with moderate to severe metatarsus adductus. Foot Ankle Int 40:641–647. https://doi.org/10.1177/1071100719835520
Conti MS, Caolo KC, Ellis SJ, Cody EA (2021) Radiographic and clinical outcomes of hallux valgus and metatarsus adductus treated with a modified lapidus procedure. Foot Ankle Int 42:38–45. https://doi.org/10.1177/1071100720952079
Loh B, Chen JY, Yew AK, Chong HC, Yeo MG, Tao P, Yeo NE, Koo K, Rikhraj Singh I (2015) Prevalence of metatarsus adductus in symptomatic hallux valgus and Its influence on functional outcome. Foot Ankle Int 36:1316–1321. https://doi.org/10.1177/1071100715595618
Johnson KA, Cofield RH, Morrey BF (1979) Chevron osteotomy for hallux valgus. Clin Orthop Relat Res 142:44–47
Al-Nammari SS, Christofi T, Clark C (2015) Double first metatarsal and akin osteotomy for severe hallux valgus. Foot Ankle Int 36:1215–1222. https://doi.org/10.1177/1071100715589173
Easley ME, Trnka HJ (2007) Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int 28:748–758. https://doi.org/10.3113/FAI.2007.0748
van Groningen B, van der Steen MC, Reijman M, Bos J, Hendriks JG (2016) Outcomes in chevron osteotomy for hallux valgus in a large cohort. Foot (Edinb) 29:18–24. https://doi.org/10.1016/j.foot.2016.09.002
Seo JH, Lee HS, Choi YR, Park SH (2020) Distal chevron osteotomy with lateral release for moderate to severe hallux valgus patients aged sixty years and over. Int Orthop 44:1099–1105. https://doi.org/10.1007/s00264-020-04562-5
Choi YR, Lee HS, Jeong JJ, Kim SW, Jeon IH, Lee DH, Lee WC (2012) Hallux valgus correction using transarticular lateral release with distal chevron osteotomy. Foot Ankle Int 33:838–843. https://doi.org/10.3113/FAI.2012.0838
Lee HJ, Chung JW, Chu IT, Kim YC (2010) Comparison of distal chevron osteotomy with and without lateral soft tissue release for the treatment of hallux valgus. Foot Ankle Int 31:291–295. https://doi.org/10.3113/FAI.2010.0291
Badwey TM, Dutkowsky JP, Graves SC, Richardson EG (1997) An anatomical basis for the degree of displacement of the distal chevron osteotomy in the treatment of hallux valgus. Foot Ankle Int 18:213–215. https://doi.org/10.1177/107110079701800405
Bohne W (1987) Metatarsus adductus. Bull N Y Acad Med 63:835–838
Dawoodi AI, Perera A (2012) Radiological assessment of metatarsus adductus. Foot Ankle Surg 18:1–8. https://doi.org/10.1016/j.fas.2011.03.002
Lichtblau S (1975) Section of the abductor hallucis tendon for correction of metatarsus varus deformity. Clin Orthop Relat Res 110:227–232. https://doi.org/10.1097/00003086-197507000-00032
Yu GV, DiNapoli R (1989) Surgical management of hallux abducto valgus with concomitant metatarsus adductus. In: McGlamry ED (ed) Reconstructive surgery of the foot and leg, Update '89. Podiatry Institute Publishing, Tucker, pp 262–268
Panchani S, Reading J, Mehta J (2016) Inter and intra-observer reliability in assessment of the position of the lateral sesamoid in determining the severity of hallux valgus. Foot (Edinb) 27:59–61. https://doi.org/10.1016/j.foot.2015.10.001
Agrawal Y, Desai A, Mehta J (2011) Lateral sesamoid position in hallux valgus: correlation with the conventional radiological assessment. Foot Ankle Surg 17:308–311. https://doi.org/10.1016/j.fas.2011.01.001
Ahn JY, Lee HS, Chun H, Kim JS, Seo DK, Choi YR, Kim SW (2013) Comparison of open lateral release and transarticular lateral release in distal chevron metatarsal osteotomy for hallux valgus correction. Int Orthop 37:1781–1787. https://doi.org/10.1007/s00264-013-2023-1
Budiman-Mak E, Conrad KJ, Roach KE (1991) The Foot Function Index: a measure of foot pain and disability. J Clin Epidemiol 44:561–570. https://doi.org/10.1016/0895-4356(91)90220-4
Carlsson AM (1983) Assessment of chronic pain: I. aspects of the reliability and validity of the visual analogue scale. Pain 16:87–101. https://doi.org/10.1016/0304-3959(83)90088-X
Seo JH, Lee HS, Choi YR, Park SH, Lee JH, Chun H (2021) Outcomes of simultaneous bilateral vs unilateral distal chevron metatarsal osteotomy in hallux valgus patients aged ≥ 60 years. Foot Ankle Int 1071100721996707. https://doi.org/10.1177/1071100721996707
Song JH, Kang C, Hwang DS, Lee GS, Lee SB (2019) Comparison of radiographic and clinical results after extended distal chevron osteotomy with distal soft tissue release with moderate versus severe hallux valgus. Foot Ankle Int 40:297–306. https://doi.org/10.1177/1071100718807893
Zettl R, Trnka HJ, Easley M, Salzer M, Ritschl P (2000) Moderate to severe hallux valgus deformity: correction with proximal crescentic osteotomy and distal soft-tissue release. Arch Orthop Trauma Surg 120:397–402. https://doi.org/10.1007/pl00013769
Austin DW, Leventen EO (1981) A new osteotomy for hallux valgus: a horizontally directed “V” displacement osteotomy of the metatarsal head for hallux valgus and primus varus. Clin Orthop Relat Res 157:25–30. https://doi.org/10.1097/00003086-198106000-00007
Bai LB, Lee KB, Seo CY, Song EK, Yoon TR (2010) Distal chevron osteotomy with distal soft tissue procedure for moderate to severe hallux valgus deformity. Foot Ankle Int 31:683–688. https://doi.org/10.3113/FAI.2010.0683
Deenik A, van Mameren H, de Visser E, de Waal MM, Draijer F, de Bie R (2008) Equivalent correction in scarf and chevron osteotomy in moderate and severe hallux valgus: a randomized controlled trial. Foot Ankle Int 29:1209–1215. https://doi.org/10.3113/FAI.2008.1209
Sanhudo JA (2000) Extending the indications for distal chevron osteotomy. Foot Ankle Int 21:522–523. https://doi.org/10.1177/107110070002100614
Park YB, Lee KB, Kim SK, Seon JK, Lee JY (2013) Comparison of distal soft-tissue procedures combined with a distal chevron osteotomy for moderate to severe hallux valgus: first web-space versus transarticular approach. J Bone Joint Surg Am 95:e158. https://doi.org/10.2106/JBJS.L.01017
Aiyer A, Shub J, Shariff R, Ying L, Myerson M (2016) Radiographic recurrence of deformity after hallux valgus surgery in patients with metatarsus adductus. Foot Ankle Int 37:165–171. https://doi.org/10.1177/1071100715608372
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Jae-Jung Jeong, Dong-Kyo Seo, Taehong Kee, and Sangpil So. The first draft of the manuscript was written by Jaehyung Lee and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective study was approved by the institutional review board of Asan Medical Center.
Consent to participate (include appropriate statements)
Informed consent was obtained from patients included in the study.
Consent for publication (include appropriate statements)
Patients signed informed consent regarding publishing their data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, J., Lee, H.S., Jeong, JJ. et al. Distal chevron metatarsal osteotomy is a viable treatment option for hallux valgus with metatarsus adductus—multicentre retrospective study. International Orthopaedics (SICOT) 45, 2261–2270 (2021). https://doi.org/10.1007/s00264-021-05117-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05117-y