Abstract
Purpose
The aim of this study was to investigate the difference in clinical and radiographic outcomes between conventional open lateral soft tissue release (OLSTR) and transarticular lateral soft tissue release (TLSTR) in patients undergoing distal chevron metatarsal osteotomy (DCMO) for hallux valgus (HV) correction.
Methods
This study included weight-bearing anteroposterior radiographs of 138 patients (185 feet) with HV that underwent DCMO and Akin phalangeal osteotomy at a mean age of 51.7 years (21–74) with a mean 26 months of follow-up between June 2004 and June 2010. Patients were classified into two groups: OLSTR as group 1 (84 feet) and TLSTR as group 2 (101 feet). We evaluated clinical and radiographic outcomes between the two groups using the American Orthopaedic Foot and Ankle Society hallux score, visual analogue scale pain score, hallux valgus angle, intermetatarsal angle and complications, pre- and post-operatively.
Results
There were no significant differences between the two groups except for post-operative complications such as first metatarsophalangeal joint (MTPJ) stiffness (group 1) and post-operative hallux varus (group 2).
Conclusions
Clinical and radiographic outcomes between OLSTR and TLSTR in HV correction using DCMO were not significantly different except for post-operative limitation of motion of the first MTPJ and hallux varus tendency. Different precautions should be taken into account when choosing the type of lateral soft tissue release due to possible complications associated with each technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Open lateral soft tissue releases (OLSTR) are performed in patients undergoing distal chevron metatarsal osteotomy (DCMO) to compensate for insufficient correction in hallux valgus (HV) deformities [1–7]. However, an OLSTR is less cosmetically desirable due to the scar caused by the extra incision between the dorsum of the first web space [4, 6, 8, 9]. In addition, there may be a risk of an avascular necrosis (AVN) at the metatarsal head due to possible combination of excessive OLSTR and DCMO although AVN is rare in clinical practice [10–13]. Schneider et al. [14] have revealed that the single dorsomedial approach for lateral soft tissue release was safe without risk of AVN in DCMO. Lee and Kim [3] reported the usefulness of proximal chevron metatarsal osteotomy (PCMO) through a medial incision without AVN of the first metatarsal head.
Less invasive techniques that focus on maximising function and cosmesis have been proposed [15–20], including a lateral soft tissue release without a dorsal incision, also known as the transarticular lateral soft tissue release (TLSTR) [19–21]. However, there are no published studies comparing OLSTR and TLSTR. Therefore, the aim of this study was to investigate the difference in clinical and radiographic outcomes between conventional and TLSTR in patients undergoing DCMO for HV correction.
Materials and methods
In 138 patients with HV who underwent DCMO with Akin phalangeal osteotomy between June 2004 and June 2010, 185 feet that underwent DCMO were classified into two groups according to the type of lateral soft tissue release: OLSTR as group 1 (84 feet) and TLSTR as group 2 (101 feet). The mean HV angle (HVA) was 30.5 ± 5.4° (range 20–60°). None of the patients had an HVA less than 20°. The details of the two groups are summarised in Table 1. Cases of HV due to fracture complication, rheumatoid arthritis and hallux rigidus were excluded. Between June 2004 and September 2009, the transarticular adductor tenotomy was combined with a DCMO. Between October 2009 and June 2010 the OLSTR (adductor tenotomy and metatarsosesamoid ligament resection) was done with the DCMO by the same orthopaedic surgeon (HS Lee). The average patient age was 51.7 years (range 21–74 years), and the average follow-up was 26 months (range 18–36 months).
Radiographic evaluation
The HVA and intermetatarsal angle (IMA) were measured preoperatively and at the final follow-up with weight-bearing foot anteroposterior (AP) plain radiographs. Preoperatively, the longitudinal axis of the first and second metatarsals was used to measure HVA and IMA. Post-operatively, a connecting line between the centre of the displaced distal metatarsal head and the centre of the metatarsal base was used as the longitudinal axis to measure HVA and IMA as described by Shima et al. [22]. This method has high intraobserver and interobserver reliability [22]. Two orthopaedic surgeons measured the HVA and IMA twice at an interval of two weeks. The averages of the four measurements were used for analysis. Subluxation of the lateral sesamoid was graded from 0 to 3 according to the lateral cortical border of the first metatarsal head on the weight-bearing foot AP plain radiographs at preoperative assessment, three-month post-operative follow-up and last follow-up by modification of the Agrawal method for severity grading on the basis of position of the lateral sesamoid due to crudeness of criteria (Table 2) [23, 24].
Clinical evaluation
The American Orthopaedic Foot and Ankle Society (AOFAS) hallux score and visual analogue scale (VAS) pain score were recorded preoperatively and at final follow-up. Limitation of motion (LOM) was defined when the first metatarsophalangeal joint (MTPJ) range of motion (ROM) was less than 40° of dorsiflexion or 20° of plantarflexion. Patients were post-operatively assessed for AVN, nonunion, hallux varus deformity and infection.
Open lateral soft tissue release
A two centimetre dorsal incision was made between the first and second metatarsals and a blunt dissection was undertaken. The conjoined tendon of the adductor hallucis was cut and detached at the lateral sesamoid. The metatarsosesamoid ligament was also released. No attempt was made to release the transverse metatarsal ligament or the lateral head of the flexor hallucis brevis (FHB). In some cases with a tight first MTPJ lateral capsule, capsule perforation was performed using several stab incisions with care to avoid a complete release. If capsular over-release did occur, it was repaired to prevent post-operative varus of the first MTPJ.
Common medial bony procedure after both kinds of lateral soft tissue releases
A bunionectomy was performed through a T-shaped incision of the medial capsule. The 60° angled chevron osteotomy was made at the centre of the first metatarsal head with the apex located distally. A five to seven millimetre lateral translation was applied using the distal fragment of the metatarsal head. At the same time, a distal metatarsal articular angle (DMAA) correction was attempted by impaction on the medial side of the distal fragment. Two 1.1-mm Kirschner wires were inserted to fix the displaced fragment two centimetres proximal to the osteotomy site. The medial prominent proximal fragment was excised after displacement of the distal fragment laterally. A capsulorrhaphy was performed with PDS 2-0 (Ethicon®, Johnson & Johnson).
Transarticular lateral soft tissue release
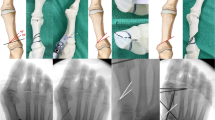
As per the medial bony procedure, a medial incision and T-shaped capsular flap incision were made. The first toe was distracted distally and a no.15 blade was inserted blind through the first MTPJ (medial to lateral) to release the adductor tendon (Fig. 1). As the approach was blind, one strategy to control the extent of lateral soft tissue tension was to hold the blade stationary and move the hallux medially, allowing the lateral structures to contact the blade. This resulted in a lateral capsulotomy and adductor tenotomy without a metatarsosesamoid ligament release.
Akin phalangeal osteotomy
The osteotomy was performed seven millimetres distal from the proximal phalangeal base. In cases of a pronated hallux, de-rotation was performed as required. Those with no hallux pronation received a one to three millimetre medial closing wedge osteotomy parallel to the MTPJ with an attempt to greenstick the lateral cortex. Fixation was performed using two 1.1-mm Kirschner wires.
Post-operative care
Two-ply 4 × 3 gauze rolled into a thickness of approximately 1.5 cm was placed between the first and second toe for six weeks. After surgery patients were allowed immediate full weight-bearing with hard-soled shoes. Passive forceful manipulations were provided at two weeks post-operatively. Depending on the patient, ordinary shoes were allowed six weeks post-operatively. The Kirschner wires were removed eight to ten weeks post-operatively under local anaesthesia. Active sports were allowed after removal of the K-wires.
Statistical analysis
Statistical comparisons between the two groups with regard to demographic variables and outcomes were assessed with the independent t test. The comparison between preoperative and last follow-up outcomes for each group was performed with a paired t test and Mann-Whitney U test (sesamoid subluxation). Among follow-up periods, comparison of sesamoid subluxation for each group was performed with the Friedman test. A post hoc test was done by Wilcoxon signed-rank test and Bonferroni correction. The incidence of post-operative complications in each group was compared using the chi-square test. The level of significance was set at p < 0.05.
Results
The HVA and IMA improved in both groups after surgery: the group 1 HVA improved from 30.7° (range 20–60°) to 6.4° (range 0–18°; p = 0.001) and the group 1 IMA improved from 15.3° (range 8–20°) to 6.0° (range 0–13°; p = 0.001; Fig. 2), whereas the group 2 HVA improved from 30.2° (range 21–46°) to 5.4° (range −13 to 19°) (p = 0.001) and the group 2 IMA improved from 14.6° (range 10–19°) to 6.0° (range 1–13°; p = 0.001; Fig. 3). However, there were no significant differences between the two groups. The AOFAS and VAS pain scores also improved in both groups after surgery: group 1 improved from 50.0 (range 35–83) to 90.3 (range 80–95; p = 0.001) and from 6.3 (range,2–8) to 0.8 (range 0–4; p = 0.001), for AOFAS and VAS scores, respectively, whereas group 2 improved from 49.0 (range 27–60) to 91.5 (range, 77–95) (p = 0.001) and from 6.7 (range,0–8) to 0.6 (range 0–4; p = 0.001), for AOFAS and VAS scores, respectively. There were no significant differences in either AOFAS or VAS scores between the two groups. There were no significant differences in median grade of lateral sesamoid position between the three-month post-operative follow-up and last follow-up in either group (Table 3). In group 1, lateral sesamoid position significantly improved from 2.5 (interquartile range 2–3) at preoperative assessment to 1 (interquartile range 1–2) (p = 0.0001) at the three-month post-operative follow-up and to 1 (interquartile range 1–2) (p = 0.0001) at last follow-up. In group 2, lateral sesamoid position significantly improved from 2 (interquartile range 2–3) at preoperative assessment to 1 (interquartile range 1–2) (p = 0.0001) at the three-month post-operative follow-up and to 1 (interquartile range 1–2) (p = 0.0001) at last follow-up. There were no significant changes of sesamoid subluxation between the three-month post-operative follow-up and last follow-up in both groups.
In group 1, LOM in both dorsi- and plantarflexion was noted in seven cases and LOM in plantarflexion alone was noted in 17 cases. In group 2, LOM in both dorsi- and plantarflexion was noted in four cases and LOM in plantarflexion alone was noted in 12 cases. There were no cases with limitations in dorsiflexion alone in either group. The number of cases with LOM in group 1 was significantly higher than in group 2 (p = 0.048). Seven patients in group 2 had radiographic evidence of acquired post-operative hallux varus (3, 5, 6, 8, 9, 10 and 13°), whereas no patients in group 1 exhibited post-operative hallux varus; this difference was significant (p = 0.048; Fig. 4). The hallux varus patients did, however, exhibit satisfactory ROM of the first MTPJ and were pain free. Correction surgery was thus not performed on any hallux varus patient. There was one case of neuralgia due to lateral dorsal cutaneous nerve injury after TLSTR. The neuralgia recovered after weak steroid injection and application of topical lidocaine jelly. There was no evidence of other significant complications such as AVN, nonunion, extension or flexion malunion, or infection at final follow-up in any patient.
Hallux varus complication. a Preoperative weight-bearing foot AP showing HVA 30° and IMA 14°. b Two-week post-operative weight-bearing foot AP showing DCMO and Akin phalangeal osteotomy with TLSTR. c Twenty-six-month post-operative weight-bearing foot AP at final follow-up showing hallux varus (HVA −13°) and IMA 3°
Discussion
Various anatomical structures are involved in procedures of lateral soft tissue release used in combination with metatarsal osteotomies for HV correction [25, 26]. Due to the HV deformity, the first MTPJ anatomy is distorted with fibrosis and permanent shortening of tissues in the lateral aspect of the joint [26]. Therefore, soft tissue reconstruction has been considered as important as osteotomies used to minimise the vector that maintains the HV deformity [27]. In OLSTR, many different structures can be released with diverse techniques [11, 21, 28]. There has been much debate over whether to use the adductor hallucis release as one of the lateral soft tissue releases in combination with metatarsal osteotomies. Following the techniques of Mann et al. [29], who performed the McBride technique that released the adductor hallucis tendon and the lateral capsule without the fibular sesamoid excision, Resch et al. [30] did not recommend adding a lateral soft tissue release with the chevron metatarsal osteotomy after considering their AVN results in a prospective study of 84 patients. However, it has continued to be used in most lateral soft tissue releases for HV deformity [1, 28, 31]. In our study, the adductor hallucis tendon release was performed in both groups. Although the adductor hallucis tendon transfer after the tenotomy has been used in previous studies [1], we did not perform this transfer as we deemed it to be ineffective compared to the time and effort taken to re-attach the tendon to the metatarsal neck. Other common releases used with DCMOs are the adductor hallucis tendon with the metatarsosesamoid and transverse metatarsal ligament [6, 28]. However, we only included the adductor tendon with the metatarsosesamoid ligament in the OLSTR. The transverse metatarsal ligament was not released due to the possibility of creating instability between the first and second metatarsals and the risk of injuring the nerve. Similarly, Schneider reported that transverse metatarsal ligament release or re-attachment of the adductor hallucis tendon was ineffective in a cadaveric study [32].
There are various lateral soft tissue release procedures proposed using a single medial incision, such as the TLSTR used in HV surgery [3, 7, 19, 20, 31]. In contrast to our study, there was a study using a single medial incision to approach the first web space via the dorsal flap to undergo a lateral release with a PCMO [3]. Also, Schneider et al. [14] have shown that the single dorsomedial approach for lateral soft tissue release was safe without risk for the nerve in the DCMO. However, this method relies on exposing and separating the dorsomedial cutaneous nerve, which could increase the risk of nerve injury even though this study showed safe results concerning nerve injury. In addition, skin irritation could occur on the lateral margin of the dorsal flap due to the retraction of the superficial dorsal flap above the extensor hallucis longus and brevis. Compared to this dorsal flap technique, our method of using a TLSTR is safe and simple because there is no need to expose or separate the nerve.
Stamatis et al. reported the use of a more flexible arthroscopic blade in preference to a no. 15 blade [19]. They performed 15 TLSTR procedures on fresh-frozen specimens and demonstrated that the arthroscopic blade could cut continuously on all edges of the blade. The use of an arthroscopic blade for the TLSTR is reported to be reproducible, safe and easy to use with a relatively minimal lateral release of the lateral sesamoid ligament, lateral MTPJ capsule and the adductor tendon insertion. The findings of Stamatis et al. support our view that the TLSTR including an adductor tenotomy and capsulotomy is safe and feasible. Furthermore, Sammarco and Conti [31] showed that a PCMO performed with a single medial incision with an appropriate blade provided good results for HV correction. The authors performed the lateral soft tissue release including the adductor tendon, metatarsosesamoid ligament and capsule with a no. 15 blade. We performed the TLSTR blindly after the first MTPJ capsulotomy, whereas in comparison, Sammarco and Conti depressed the lateral sesamoid using a Penfield elevator and approached the lateral capsule by running the scalpel along the lower margin of the first metatarsal. At this point the lateral capsulotomy was completed by performing a 90° upward rotation at the first MTPJ. Thus, the lateral soft tissue release could have been more excessive than our version of the transarticular tenotomy.
We believe that the single medial incision approach, such as the TLSTR, is a reproducible, safe and simple technique. However, caution should be taken when using this method as overcorrection of the lateral soft tissue tension may lead to post-operative hallux varus. This is partly due to the blind method used and also depends on the surgeon’s subjective judgment in regards to the lateral tension of the first MTPJ. Chen et al. [7] also conducted DCMOs with intra-articular lateral soft tissue releases on 32 patients with moderate to severe HV deformity. Although initial clinical and radiographic results appeared satisfactory, they also reported two cases of post-operative hallux varus. The authors considered that the main cause of post-operative hallux varus was partial division of the lateral head of the FHB when releasing the adductor tendon and recommended great caution when conducting an adductor tenotomy.
We agree that when performing a TLSTR, the overcorrection of the lateral structures in the first MTPJ, such as the division of the FHB at the distal sesamoid, could be the cause of post-operative hallux varus. Transarticular lateral soft tissue release may be cosmetically and functionally superior to OLSTR; however, we believe that the possibility of post-operative hallux varus must be strongly considered when using the TLSTR. In our study, there were no cases of post-operative hallux varus in the OLSTR group. When performing a DCMO with TLSTR, even if the intraoperative deformity correction or the gross appearance of the hallux appears satisfactory, a varus stress test should be conducted at the first MTPJ. If varus laxity is present, a lateral capsule repair through an additional dorsal incision of the first web space, as described and performed by Choi et al. [33], could be helpful to correct the varus instability of the first MTPJ and prevent post-operative hallux varus.
Patients with LOM of first MTPJ had larger preoperative HVA and post-operative varus complication occurred in older age. However, there were no significant differences. A hallux varus complication occurred in an earlier period of this operation. A technical error of transarticular adductor tenotomy could be possible.
Metatarsal osteotomies with TLSTR for HV correction have previously been shown to produce clinically satisfactory results [21]; however, there are no published studies comparing conventional OLSTR and TLSTR. This comparison is important because surgeons who have had success using a single adductor tenotomy with TLSTR may inconveniently resect the metatarsosesamoid ligament with the adductor tenotomy when using an OLSTR, when resecting the adductor tendon alone would have been sufficient. We suggest that complete metatarsosesamoid ligament resection may not be helpful for satisfactory HV correction based on plain radiographs, because when valgus correction is achieved, sesamoid reduction will occur naturally as a consequence of the normal alignment at the first MTPJ.
The complication of LOM of the first MTPJ in OLSTR patients should also be carefully considered as well as post-operative hallux varus originating from medial-lateral soft tissue imbalance at the first MTPJ when using the TLSTR. However, if adequate precautions are taken, the TLSTR can be recommended as it avoids unnecessary scarring in the dorsal aspect of the first web space.
This study has limitations. Firstly, we found that post-operative hallux varus was the most significant problem when using a TLSTR; however, we did not analyse other factors such as generalised laxity. Secondly, the length of the follow-up was relatively short.
Conclusion
Clinical and radiographic outcomes including AOFAS hallux score, VAS pain scale, HVA and IMA were not significantly different between OLSTR and TLSTR for HV correction using DCMO. Consideration should be given to possible complications when choosing the type of lateral soft tissue release: LOM of the first MTPJ associated with OLSTR and overcorrection of the lateral soft tissue tension leading to post-operative hallux varus when using the TLSTR.
References
Granberry WM, Hickey CH (1995) Hallux valgus correction with metatarsal osteotomy: effect of a lateral distal soft tissue procedure. Foot Ankle Int 16:132–138
Lee H-J, Chung J-W, Chu I-T, Kim Y-C (2010) Comparison of distal chevron osteotomy with and without lateral soft tissue release for the treatment of hallux valgus. Foot Ankle Int 31:291–295. doi:10.3113/FAI.2010.0291
Lee W-C, Kim Y-M (2007) Correction of hallux valgus using lateral soft-tissue release and proximal Chevron osteotomy through a medial incision. J Bone Joint Surg Am 89(Suppl 3):82–89. doi:10.2106/JBJS.G.00483
O’Donnell T, Hogan N, Solan M, Stephens MM (2010) Correction of severe hallux valgus using a basal chevron osteotomy and distal soft tissue release. Foot Ankle Surg 16:126–131. doi:10.1016/j.fas.2009.08.002
Coughlin MJ, Grimes S (2005) Proximal metatarsal osteotomy and distal soft tissue reconstruction as treatment for hallux valgus deformity. Keio J Med 54:60–65
Bai LB, Lee KB, Seo CY et al (2010) Distal chevron osteotomy with distal soft tissue procedure for moderate to severe hallux valgus deformity. Foot Ankle Int 31:683–688. doi:10.3113/FAI.2010.0683
Chen YJ, Hsu RW, Shih HN et al (1996) Distal chevron osteotomy with intra-articular lateral soft-tissue release for treatment of moderate to severe hallux valgus deformity. J Formos Med Assoc 95:776–781
Potenza V, Caterini R, Farsetti P et al (2009) Chevron osteotomy with lateral release and adductor tenotomy for hallux valgus. Foot Ankle Int 30:512–516. doi:10.3113/FAI.2009.0512
Panchbhavi VK, Rapley J, Trevino SG (2011) First web space soft tissue release in bunion surgery: functional outcomes of a new technique. Foot Ankle Int 32:257–261. doi:10.3113/FAI.2011.0257
Peterson DA, Zilberfarb JL, Greene MA, Colgrove RC (1994) Avascular necrosis of the first metatarsal head: incidence in distal osteotomy combined with lateral soft tissue release. Foot Ankle Int 15:59–63
Kuhn MA, Lippert FG 3rd, Phipps MJ, Williams C (2005) Blood flow to the metatarsal head after chevron bunionectomy. Foot Ankle Int 26:526–529
Easley ME, Kelly IP (2000) Avascular necrosis of the hallux metatarsal head. Foot Ankle Clin 5:591–608
Malal JJG, Shaw-Dunn J, Kumar CS (2007) Blood supply to the first metatarsal head and vessels at risk with a chevron osteotomy. J Bone Joint Surg Am 89:2018–2022. doi:10.2106/JBJS.F.01030
Schneider W, Aigner N, Pinggera O, Knahr K (2004) Chevron osteotomy in hallux valgus. Ten-year results of 112 cases. J Bone Joint Surg Br 86:1016–1020
Siclari A, Decantis V (2009) Arthroscopic lateral release and percutaneous distal osteotomy for hallux valgus: a preliminary report. Foot Ankle Int 30:675–679. doi:10.3113/FAI.2009.0675
Lui TH, Chan KB, Chan LK (2010) Endoscopic distal soft-tissue release in the treatment of hallux valgus: a cadaveric study. Arthroscopy 26:1111–1116. doi:10.1016/j.arthro.2009.12.027
Leemrijse T, Valtin B, Besse J-L (2008) Hallux valgus surgery in 2005. Conventional, mini-invasive or percutaneous surgery? Uni- or bilateral? Hospitalisation or one-day surgery? Rev Chir Orthop Reparatrice Appar Mot 94:111–127. doi:10.1016/j.rco.2007.04.006
Oliva F, Longo UG, Maffulli N (2009) Minimally invasive hallux valgus correction. Orthop Clin North Am 40:525–530, x. doi:10.1016/j.ocl.2009.06.005
Stamatis ED, Huber MH, Myerson MS (2004) Transarticular distal soft-tissue release with an arthroscopic blade for hallux valgus correction. Foot Ankle Int 25:13–18
Asunción J, Poggio D (2012) Transmetatarsal lateral release in hallux valgus surgery: technical tip. Foot Ankle Int 33:844–847. doi:10.3113/FAI.2012.0844
Choi YR, Lee HS, Jeong JJ et al (2012) Hallux valgus correction using transarticular lateral release with distal chevron osteotomy. Foot Ankle Int 33:838–843. doi:10.3113/FAI.2012.0838
Shima H, Okuda R, Yasuda T et al (2009) Radiographic measurements in patients with hallux valgus before and after proximal crescentic osteotomy. J Bone Joint Surg Am 91:1369–1376. doi:10.2106/JBJS.H.00483
Mann RA (1990) Decision-making in bunion surgery. Instr Course Lect 39:3–13
Agrawal Y, Desai A, Mehta J (2011) Lateral sesamoid position in hallux valgus: correlation with the conventional radiological assessment. Foot Ankle Surg 17:308–311. doi:10.1016/j.fas.2011.01.001
Lin I, Bonar SK, Anderson RB, Davis WH (1996) Distal soft tissue release using direct and indirect approaches: an anatomic study. Foot Ankle Int 17:458–463
Sammarco VJ (2008) Surgical correction of moderate and severe hallux valgus: proximal metatarsal osteotomy with distal soft-tissue correction and arthrodesis of the metatarsophalangeal joint. Instr Course Lect 57:415–428
Saltzman CL, Aper RL, Brown TD (1997) Anatomic determinants of first metatarsophalangeal flexion moments in hallux valgus. Clin Orthop Relat Res 339:261–269
Pochatko DJ, Schlehr FJ, Murphey MD, Hamilton JJ (1994) Distal chevron osteotomy with lateral release for treatment of hallux valgus deformity. Foot Ankle Int 15:457–461
Mann RA, Rudicel S, Graves SC (1992) Repair of hallux valgus with a distal soft-tissue procedure and proximal metatarsal osteotomy. A long-term follow-up. J Bone Joint Surg Am 74:124–129
Resch S, Stenström A, Reynisson K, Jonsson K (1994) Chevron osteotomy for hallux valgus not improved by additional adductor tenotomy. A prospective, randomized study of 84 patients. Acta Orthop Scand 65:541–544
Sammarco GJ, Conti SF (1993) Proximal Chevron metatarsal osteotomy: single incision technique. Foot Ankle 14:44–47
Schneider W (2012) Influence of different anatomical structures on distal soft tissue procedure in hallux valgus surgery. Foot Ankle Int 33:991–996. doi:10.3113/FAI.2012.0991
Choi KJ, Lee HS, Yoon YS et al (2011) Distal metatarsal osteotomy for hallux varus following surgery for hallux valgus. J Bone Joint Surg Br 93:1079–1083. doi:10.1302/0301-620X.93B8.26430
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahn, J.Y., Lee, H.S., Chun, H. et al. Comparison of open lateral release and transarticular lateral release in distal chevron metatarsal osteotomy for hallux valgus correction. International Orthopaedics (SICOT) 37, 1781–1787 (2013). https://doi.org/10.1007/s00264-013-2023-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-2023-1