Abstract
Purpose
This study aimed to investigate stress shielding of anatomical tibial components (ATCs) in comparison to conventional symmetric tibial components (STCs) in Korean patients which may be related to medial tibial bone loss.
Method
78 knees in 59 patients with ATCs (Persona™) and 74 knees in 58 patients with STCs (NexGen LPS-Flex™) were retrospectively reviewed. Radiographic parameters and clinical outcomes in both groups were compared. Logistic regression analysis was performed to identify risk factors for medial tibial bone loss.
Results
Medial tibial bone loss was significantly greater in the ATC group (1.6 ± 1.3 mm) than in the STC group (0.4 ± 0.8 mm) (p < 0.001). The ATC group showed a shorter distance between the distal metal tip and anteromedial cortex and higher invading into the sclerotic bone lesion (ISBL) than the STC group (p = 0.034 and p = 0.044, respectively). Multiple logistic regression analysis suggested ATC, a shorter distance to the anteromedial cortex, and the presence of ISBL as risk factors for medial tibial bone loss. The odds ratios of medial tibial bone loss according to type of prosthesis, distance to anteromedial cortex, and presence of ISBL were 6.25 (range 2.86–13.63, p < 0.001), 0.69 (range 0.51–0.93, p = 0.015), and 3.79 (range 1.56–9.21, p = 0.003), respectively. Notwithstanding, there was no difference in clinical outcomes between the two groups.
Conclusion
In Korean patients, ATCs potentially causes greater medial tibial bone loss due to stress shielding than STCs. The design, however, does not yet appear to affect clinical outcomes at mid-term follow-up.
Level of evidence
Retrospective cohort study, level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) shows excellent results in the treatment of end-stage knee osteoarthritis (OA). With increases in the average human life span, the demand and indications for TKA are concomitantly increasing. To meet this demand, prostheses with various materials and designs have been developed, the characteristics of which can affect long-term clinical outcomes [17].
Medial tibial bone loss due to the phenomenon of stress shielding is a well-known complication of TKA that can cause loosening or migration of an implant. The incidence of medial tibial bone loss varies depending on the characteristics of the tibial component of an implant. Martin et al. reported that a tibial component composed of cobalt chrome (CoCr) alloy, which is a material with high elastic modulus, caused more bone loss than titanium (Ti) alloy or all-polyethylene components [12]. In another study, they reported that bone loss was greater with the use of thicker baseplates for the same CoCr alloy tibial components [13]. Predisposing patient factors, such as the degree of correction of the hip–knee–ankle angle (HKA) [8] and the alignment of an implant [15], interact in a complex manner with the characteristics of a prosthesis.
A base plate designed with an anatomical tibial component (ATC) is similar to the tibial section of the human body, allowing for optimal rotational alignment and maximum tibial surface coverage [4]. Its medialized keel allows for better alignment between the tibial component and tibial shaft. This anatomical design is expected to provide good clinical outcomes and longevity of the prosthesis [7]. However, to our knowledge, there has been no report on the occurrence of stress shielding in association with ATC, especially in Asian patients.
Significant varus and increased proximal tibial vara are common in Korean knee osteoarthritic patients [10, 11]. Thus, the stem of the tibial component would tend to be placed in a medialized position when aiming for mechanical alignment [19]. In addition, as the location of the canal in regards to the tibial plateau for Asian patients is in an anterolateral position, contrary to Caucasian patients, it is more likely that the stem would be biased to the medial position when using ATCs with a medially offset stem [18, 20]. Thus, we hypothesized that ATC with medially offset stem would not be effective for stress transfer in Korean patients or in those with similar anatomical structures, so it could induce stress shielding which may be related to medial tibial bone loss.
Therefore, this study aimed to investigate differences in radiographic characteristics and clinical outcomes of ATCs and conventional symmetric tibial components (STCs) in Korean patients.
Material and methods
Patient selection
With approval from Institutional Review Board (3-2019-0155) of the author’s institution (Gangnam Severance Hospital), 234 knees in 184 Korean adult patients who consecutively received primary TKA with designated prostheses for degenerative OA from July 2013 to June 2016 were enrolled. A STC (NexGen LPS-Flex™) and an ATC prosthesis (Persona™) from a single manufacturer (Zimmer, Warsaw, IN, USA) were used. Prior to May 2015, STC was used, and ATC was used afterwards. All perioperative protocols, except for implant type, were the same. The exclusion criteria were as follows: (1) patients who were not followed for more than 2 years; (2) patients who did not undergo an image study for evaluation; (3) patients with a history of previous infection, trauma, rheumatoid arthritis and osteonecrosis; and (4) patients with severe bone defects using bone grafts, metal blocks, or long stems. Finally, 152 knees in 117 patients were included in this study. There were 78 knees (59 patients) in the ATC group and 74 knees (58 patients) in the STC group. Demographic data, radiographic parameters, and clinical outcome scores of the two groups are shown in Table 1.
Surgical procedure
All surgeries were performed with a posterior stabilized type TKA using a midvastus approach by a single experienced surgeon. A tourniquet was inflated just before making the skin incision and was deflated after skin closure. All operations were performed with mechanically aligned TKA to ensure that the tibia was cut at 90° to the axis using an extramedullary guide. If a sclerotic bone was present on the medial tibial plateau after tibial cutting, a small drill was used to puncture the sclerotic bone area at 3 mm intervals to improve intrusion of the cement. All surgical procedures and perioperative protocols were the same except for the type of prosthesis.
Data collection
All radiographs taken at the hospital and at outpatient clinics were true anterior–posterior radiographic images with the patella as the center. The bone loss extent in coronal radiographs and distance to the cortex in computed tomography (CT) images were measured with calibration based on the actual size of the implant.
All patients underwent preoperative and postoperative lower extremity scanograms with measurements of the HKA, correction angle and medial proximal tibial angle (MPTA). A postoperative fluoroscopic radiograph was obtained to measure the deviation of the keel and tibial component alignment to tibia axis. Deviation from the coronal radiograph was calculated by measuring the distance from the distal tip of the keel to the medial and lateral cortex in a horizontal direction on the base plate of the implant (deviation = distance to lateral cortex/distance to medial cortex; Fig. 1a). The presence of overhang and underhang was also confirmed by postoperative fluoroscopic radiographs. Overhang was defined as the absence of tibia bone below the base plate on immediate postoperative radiographs, and underhang was defined as exposure of the tibial cut surface.
Medial tibial bone loss was measured in a coronal radiograph with a minimum follow up of 2 years. Medial tibial bone loss was defined as the distance between the edge of the medial tibial plateau at the inferior tibial baseplate in the immediate postoperative radiograph and that of last follow-up radiograph (Fig. 2). Joint line orientation angle (JLOA) was measured on standing true anterior–posterior radiographs at the last follow up.
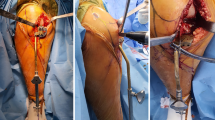
Our institution routinely performs postoperative low-dose axial CTs for rotational evaluation within 1 week after TKA. When implanting the tibial component, the phenomenon in which the keel went beyond the sclerotic bone area of the tibial cut surface was defined as invading into the sclerotic bone lesion (ISBL). This was confirmed by traces of drilling and cement intrusion in the postoperative CT axial plane (Fig. 3). The closest position of the distal tip of the keel to the cortex and the distance to the cortex were also measured in the postoperative CT axial plane (Fig. 1b).
Clinical outcome
Clinical outcomes were assessed using Visual analogue scale (VAS), Knee society score (KSS), Western Ontario and McMaster Universities Arthritis Index (WOMAC), and UCLA activity scores.
Statistical analysis
Student's t-test was used to compare the means of demographic factors, radiographic parameters, and clinical outcome scores between the two groups. Logistic regression analysis was performed to determine risk factors for medial tibial bone loss. Statistical analysis was performed using SPSS software for Windows (version 25.0, SPSS, Chicago, IL). The statistical software G*Power (version 3.1.9.4; Heinrich Heine Universität Düsseldorf, DE) was used for sample size calculation [5]. An odds ratio for sample size calculation was obtained from the result of a logistic regression analysis in a pilot study that included 40 subjects. A total of 147 subjects were required to perform logistic regression analysis using power of 0.95 and alpha error of 0.05, and hence the sample size of the present study satisfied it. All P values < 0.05 were considered statistically significant. The intra- and inter-observer reliabilities of measurements were assessed using intra-class correlation coefficients.
Results
Radiographic outcomes
Medial tibial bone loss was occurred in 71.8% (56/78) of the ATC group and 25.7% (19/74) of the STC group (p < 0.001). The extent of bone loss was significantly greater in the ATC group (1.6 ± 1.3 mm) than in the STC group (0.4 ± 0.8 mm) (p < 0.001). In the ATC group, 5.1% (4/78) of the subjects had underhang, and 5.1% (4/78) had overhang. In the STC group, 58.1% (43/74) of the subjects had underhang, and no cases of overhang were detected. The medial deviation of the ATC group was greater than that of the STC group (p < 0.001). There were no significant differences in tibial component alignment, HKA, correction angle, MPTA, JLOA and tourniquet time between the two groups. In 89.7% (70/78) of the ATC group and 58.1% (43/74) of the STC group, the shortest distance of the distal tip of the keel to the cortex was located in the anteromedial area in CT axial images. The distal metal tip in the ATC group was closer to the anteromedial cortex, compared to the STC group (3.4 ± 1.3 mm and 3.9 ± 1.5 mm, p = 0.034) in CT images. The ATC group showed greater ISBL than the STC group (34.6% and 18.9%, p = 0.044).
Multiple logistic regression analysis suggested that ATC, a shorter distance to the anteromedial cortex, and the presence of ISBL are risk factors for medial tibial bone loss (Table 2). When comparing the presence of bone loss between the ATC and STC groups, the odds ratio was 6.25 (range 2.86–13.63, p < 0.001). In addition, the odds ratios of medial tibial bone loss according to the distance to the anteromedial cortex and the presence of ISBL were 0.69 (range 0.51–0.93, p = 0.015), and 3.79 (range 1.56–9.21, p = 0.003), respectively.
The intra- and inter-observer reliabilities for the radiographic parameters were as follows: 0.867 and 0.844 for extent of bone loss, 0.898 and 0.852 for tibial component alignment, 0.946–0.985 and 0.947–0.973 for HKAs, 0.946 and 0.874 for MPTA, 0.883 and 0.865 for JLOA, and 0.904 and 0.882 for the distance to the anteromedial cortex at the 95% confidence interval, respectively.
Clinical outcomes
The differences in clinical outcomes (VAS, KSS, WOMAC, and UCLA scores) were not significant between the groups (Table 1). There was also no difference in clinical outcome in relation to the presence of bone loss (Table 3). The findings of this study indicated that there is no need for revision surgery during the follow-up period, even if bone loss occurs.
Discussion
The most important finding of the present study was that ATC (Persona™) caused more medial tibial bone loss than STC (NexGen LPS-Flex™) due to stress shielding in Korean patients. However, during the mid-term follow-up period, there were no differences in clinical scores between the two groups. Furthermore, the presence of bone loss did not affect clinical scores. As there were no differences between the two groups except for the type of implant, the radiographic differences likely resulted from the anatomical tibial component design.
The baseplate of Persona™ is asymmetric and similar to the tibial section of the human body. The size of the tibial component is more diverse than previous designs, allowing for optimal rotational alignment and maximum coverage of the tibial cut surface. Moreover, depending on size, the keel is medialized to 1–4 mm, allowing for more precise alignment with the diaphyseal axis in Caucasian patients. Despite such improvements from previous models, greater medial tibial bone loss was observed in the present study.
The tibial components of both the Persona™ and NexGen LPS-Flex™ prostheses used in present study are made of Ti alloy, with baseplate thicknesses of 3.68 mm and 4.18 mm, respectively. According to Martin et al. [12, 13], ATCs should have less stress shielding; however, this study revealed the opposite. Several studies have also reported that a longer stem of the tibial component induces more stress shielding on the proximal bone [14, 16]. This is also in contrast with the results of this study, where there was more bone loss with the Persona™ prosthesis, which has a shorter keel length compared to NexGen LPS-Flex™ across all sizes. In addition, Gu et al. reported that the presence of underhang increases bone resorption [6]. However, in this study, more bone loss was observed in patients with Persona™, which had much less underhang. Therefore, it can be concluded that stress shielding in the cohort of the present study could be caused by factors different from those in previous studies, such as the material, thickness of the baseplate, length of stem, and the presence of underhang. This difference can be explained by different hypotheses.
First, it is possible that the medialized keel showed a behavior different from that expected by the manufacture in Korean patients. The medially offset stem was originally developed to mimic anatomical features, but it could be inappropriate for Asian people since the design is based on studies on Caucasian subjects whose medullary canal of the tibia is biased toward the anteromedial side. Tang et al. performed an MRI-based study on 100 Chinese patients, wherein they found that the tibial medullary canal was biased toward the anterolateral direction from the center of the tibial plateau [18], in contrast to Caucasians patients. Since Korean patients have anatomical characteristics similar to those of Chinese patients, it is reasonable that a medially offset stem is not the most suitable design, due to contact with the medial tibial cortex [20]. This study also confirms that the distal metal tip of the ATC is more likely to be biased toward the anteromedial side on coronal radiographs and CTs. Taken together, it seems that a medialized keel designed for better alignment in Caucasian patients can lead to excessive medial deviation in Asian patients. It is observed that the distal metal tip was closer to the anteromedial cortex, where stress is concentrated, which may cause stress shielding of the medial proximal tibia. Multiple logistic regression analysis indicated that a shorter distance between the distal metal tip and the anteromedial cortex is a risk factor of medial tibial bone loss, which supports our hypothesis.
Second, regardless of the effect of the distal portion, the medialized keel’s proximal portion may also affect stress shielding. Sclerotic changes are common in the medial tibial plateau in end-stage OA patients. After tibia cutting, many sclerotic bone areas remain on the proximal tibial medial side. When the keel is medialized, it is more likely to be in contact with a larger sclerotic bone area, compared to symmetric designs. An increase in contact with hard sclerotic bone consequently increases the stress concentration in that focal area, and the overall stress transfer does not occur efficiently. It seems that this inefficient stress concentration contributes to stress shielding. In the present study, ISBL of the prosthesis due to a medialized keel was significantly higher in the ATC group than in the STC group, and was a risk factor of medial tibial bone loss in logistic regression analysis.
Third, focal underhang is difficult to identify in coronal radiographs. In this study, the incidence of medial underhang in coronal radiographs was higher in the STC group. Persona™ has an anatomical design and varies in implant sizes; therefore, it seems to be easier to approximate the correct mediolateral size. According to Jin et al., who performed a CT-based study on 100 Korean patients, the anatomically-designed Persona™ prosthesis was able to achieve an optimal fit in medioposterior and mediolateral dimensions, compared to NexGen LPS-Flex™ [9]. However, although they did not directly compare Persona™ and NexGen LPS-Flex™ prostheses, a CT-based study of 14791 subjects by Clary et al. showed different results for the anteromedial area. The subjects using Persona™ had a greater degree of cutting bone exposure in the anteromedial cortex than subjects using a symmetric design (PFC Sigma®, Attune®) and asymmetric design (Genesis II®) [3]. Therefore, although ATC prostheses provide optimal overall coverage, compared to other designs, coverage of the anteromedial area is rather poor, resulting in focal underhang, which is difficult to identify in coronal radiographs. This may be the cause of stress shielding [6].
Notwithstanding the above, there were no differences in clinical outcomes between the two groups, even when the groups were divided according to the presence of bone loss. In addition, the follow-up period was longer than that in similar studies in the literature [12, 13], the amount of bone loss was smaller, and there were no complications leading to revision surgeries. However, a longer follow up is necessary due to the possibility that the anatomical design characteristics mentioned above may continue to cause stress shielding.
This study has several limitations. First, since the subjects were selected non-randomly and in a retrospective manner, selection bias could not be completely eliminated even if there were no differences in demographic factors between the two groups. Second, there is no clear evidence that chosen follow-up period is optimal. In previous studies, it was reported that stress shielding of total hip arthroplasty appeared most commonly 1 year after surgery and rarely after 2 years [1, 2]. Therefore, it can be considered that the optimal time should be about 2 years after which a balance between bone resorption and bone remodeling is achieved. Due to this reason, patients who were followed up for more than 2 years were included. However, there is no definite consensus about the duration of remodeling in TKA; further research is needed in this area. Third, because this was not an experimental study, there were many limitations in independently analyzing factors affecting stress shielding. An extended comparison of the anatomical differences between Asian and Caucasian cohorts or a finite element model study may be useful for elucidating the causal factors leading to stress shielding. Nevertheless, this study is significant in that it is the first to show how an ATC design induces more medial tibial bone loss than conventional designs in Asian patients.
Conclusion
In this study of a Korean cohort, medial tibial bone loss due to stress shielding was more common in patients treated with an anatomical tibial component (Persona™) than in patients treated with a symmetric tibial component (NexGen LPS-Flex™). The anatomical design and medialized keel, which are advantages of ATCs, seemed to have caused this phenomenon. Although there was no clinical difference at mid-term follow-up, a longer follow-up may be necessary to exclude the possibility of stress shielding progression. These results can help surgeons with optimal implant selection and also help manufacturers to improve future implant designs, especially for Asian patients.
References
Bobyn JD, Mortimer ES, Glassman AH, Engh CA, Miller JE, Brooks CE (1992) Producing and avoiding stress shielding. Laboratory and clinical observations of noncemented total hip arthroplasty. Clin Orthop Relat Res 274:79–96
Bugbee WD, Culpepper WJ 2nd, Engh CA Jr, Engh CA Sr (1997) Long-term clinical consequences of stress-shielding after total hip arthroplasty without cement. J Bone Joint Surg Am 79(7):1007–1012
Clary C, Aram L, Deffenbaugh D, Heldreth M (2014) Tibial base design and patient morphology affecting tibial coverage and rotational alignment after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(12):3012–3018
Dai Y, Scuderi GR, Bischoff JE, Bertin K, Tarabichi S, Rajgopal A (2014) Anatomic tibial component design can increase tibial coverage and rotational alignment accuracy: a comparison of six contemporary designs. Knee Surg Sports Traumatol Arthrosc 22(12):2911–2923
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41(4):1149–1160
Gu S, Kuriyama S, Nakamura S, Nishitani K, Ito H, Matsuda S (2019) Underhang of the tibial component increases tibial bone resorption after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27(4):1270–1279
Hartel MJ, Loosli Y, Delfosse D, Diel P, Thali M, Ross S, Kohl S, Eggli S (2014) The influence of tibial morphology on the design of an anatomical tibial baseplate for TKA. Knee 21(2):415–419
Jaroma A, Soininvaara T, Kroger H (2016) Periprosthetic tibial bone mineral density changes after total knee arthroplasty. Acta Orthop 87(3):268–273
Jin C, Song EK, Prakash J, Kim SK, Chan CK, Seon JK (2017) How much does the anatomical tibial component improve the bony coverage in total knee arthroplasty? J Arthroplast 32(6):1829–1833
Kim DK, Seo MC, Song SJ, Kim KI (2015) Are Korean patients different from other ethnic groups in total knee arthroplasty? Knee Surg Relat Res 27(4):199–206
Lasam MP, Lee KJ, Chang CB, Kang YG, Kim TK (2013) Femoral lateral bowing and varus condylar orientation are prevalent and affect axial alignment of TKA in Koreans. Clin Orthop Relat Res 471(5):1472–1483
Martin JR, Watts CD, Levy DL, Kim RH (2017) Medial tibial stress shielding: a limitation of cobalt chromium tibial baseplates. J Arthroplast 32(2):558–562
Martin JR, Watts CD, Levy DL, Miner TM, Springer BD, Kim RH (2017) Tibial tray thickness significantly increases medial tibial bone resorption in cobalt-chromium total knee arthroplasty implants. J Arthroplast 32(1):79–82
Murase K, Crowninshield RD, Pedersen DR, Chang TS (1983) An analysis of tibial component design in total knee arthroplasty. J Biomech 16(1):13–22
Perillo-Marcone A, Barrett DS, Taylor M (2000) The importance of tibial alignment: finite element analysis of tibial malalignment. J Arthroplast 15(8):1020–1027
Reilly D, Walker PS, Ben-Dov M, Ewald FC (1982) Effects of tibial components on load transfer in the upper tibia. Clin Orthop Relat Res 165:273–282
Scott CE, Biant LC (2012) The role of the design of tibial components and stems in knee replacement. J Bone Joint Surg Br 94(8):1009–1015
Tang Q, Zhou Y, Yang D, Xu H, Liu Q (2010) The offset of the tibial shaft from the tibial plateau in Chinese people. J Bone Joint Surg Am 92(10):1981–1987
Thippana RK, Kumar MN (2017) Lateralization of tibial plateau reference point improves accuracy of tibial resection in total knee arthroplasty in patients with proximal tibia vara. Clin Orthop Surg 9(4):458–464
Yoo JH, Kang YG, Chang CB, Seong SC, Kim TK (2008) The relationship of the medially-offset stem of the tibial component to the medial tibial cortex in total knee replacements in Korean patients. J Bone Joint Surg Br 90(1):31–36
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest in association with the present study.
Ethical approval
All procedures were in accordance with the ethical standards of our institutional research committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cho, B.W., Kwon, H.M., Hong, Y.J. et al. Anatomical tibial component is related to more medial tibial stress shielding after total knee arthroplasty in Korean patients. Knee Surg Sports Traumatol Arthrosc 29, 710–717 (2021). https://doi.org/10.1007/s00167-020-05869-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05869-x