Abstract
Background
This retrospective study compares tibial component rotations and radiological and functional outcomes in patients who underwent Oxford medial unicompartmental knee arthroplasty (UKA), using the antero-posterior (AP) tibia axis or anterior superior iliac spine (ASIS) as the landmarks for the direction of the vertical cut.
Methods
A total of 86 patients, who underwent Oxford medial UKA were divided into 2 groups, each consisting of 43 patients, according to the use of AP axis (group I) or ASIS (group II) as landmarks for the rotation of vertical tibial cut and compared for the radiological and functional outcomes. Tibial component rotations (α-angle), involvement of the posterior cruciate ligament (PCL) fossa, and instant bearing position (IBP) were measured on computed tomography (CT) images. Functional outcomes were evaluated using Oxford knee score (OKS) and Knee Society score (KSS).
Result
The median α‑angle was significantly smaller in group I than group II (2.5°, range −4–5.5° vs. −6°, range −13–0.5°, p < 0.001). The rates of PCL fossa involvements were 14 (32.6%) and 17 (39.5%, p = 0.7). The median flexion angle of the femoral component (7° vs. 10.5°) and posterior tibial slope (6° vs. 8°) were significantly lower in group I than group II (p = 0.001). All other radiological parameters, preoperative and final OKS and KSS were statistically similar in both groups.
Conclusion
Taking the AP tibial axis as a landmark for vertical tibial cut rotation provides more neutral tibial component rotation in Oxford medial UKA compared to ASIS; however, this difference may not influence the clinical outcomes.
Zusammenfassung
Hintergrund
Diese retrospektive Studie vergleicht die Rotation der Tibiakomponente sowie die radiologischen und funktionellen Ergebnisse bei Patienten, die eine mediale unikondyläre Knieendoprothese (Oxford-Schlittenprothese) am Kniegelenk erhalten hatten, wobei die anteroposteriore Tibiaachse oder die Spina iliaca anterior superior (SIAS) als Orientierungspunkt für die Richtung des vertikalen Schnitts verwendet wurde.
Methoden
Insgesamt 86 Patienten, die eine mediale unikondyläre Schlittenprothese erhalten hatten, wurden in 2 Gruppen mit jeweils 43 Patienten unterteilt, je nachdem, ob die a.-p.-Achse (Gruppe I) oder die SIAS (Gruppe II) als Orientierungspunkt für die Rotation des vertikalen Tibiaschnitts verwendet wurde, und hinsichtlich der radiologischen und funktionellen Ergebnisse verglichen. Die Rotation der Tibiakomponente (α-Winkel), die Beteiligung der Fossa des hinteren Kreuzbands (HKB) und die sofortige Lagerposition („instant bearing position“ [IBP]) wurden auf CT-Bildern gemessen. Die funktionellen Ergebnisse wurden mit dem Oxford Knie Score (OKS) und dem Knee Society Score (KSS) bewertet.
Ergebnis
Der mediane α‑Winkel war in Gruppe I signifikant kleiner als in Gruppe II (2,5°, Range: −4 bis 5,5° vs. −6°, Range: −13 bis 0,5°; p < 0,001). Die Raten der HKB-Fossa-Beteiligung betrugen 14 (32,6 %) und 17 (39,5 %; p = 0,7). Der mediane Flexionswinkel der femoralen Komponente (7 vs. 10,5) und die posteriore tibiale Neigung (6 vs. 8) waren in Gruppe I signifikant geringer als in Gruppe II (p = 0,001). Alle anderen radiologischen Parameter sowie der präoperative und endgültige OKS und KSS waren in beiden Gruppen statistisch ähnlich.
Schlussfolgerung
Bei der medialen unikondylären Oxford-Schlittenprothese führt die Verwendung der a.-p.-Tibiaachse als Orientierungspunkt für die vertikale Rotation des Tibiaschnitts zu einer neutraleren Rotation der Tibiakomponente im Vergleich zur SIAS; dieser Unterschied hat jedoch möglicherweise keinen Einfluss auf das klinische Outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In the treatment of isolated medial compartment osteoarthritis, medial unicondylar knee arthroplasty (UKA) has been used successfully with around 95% of 10-year implant survival rate, which is similar to that of total knee arthroplasty (TKA) [5, 18, 20, 22, 23, 28, 30]. Besides its advantages in terms of morbidity, mortality, rehabilitation, and functional outcomes [12, 13, 31], mobile-bearing systems have a greater risk of complications in less experienced hands, some of which are directly related to incorrect surgical technique, mostly in the tibial cutting stage [11, 12, 21, 24, 27]. Therefore, tibial component malpositioning in the coronal, sagittal, or axial plane may cause various complications, such as insert dislocation [14], medial tibial plateau fracture [4, 26], impingement [3, 29], and loosening [2].
Tibial plateau resection for the Oxford partial knee system is performed through a saw guide, which determines varus/valgus and cut depth in the coronal plane, and posterior tibial slope, but does not provide guidance for the vertical cut in the sagittal plane, which determines the rotation of the tibial component. The designers suggest pointing the tip of the blade toward the anterior superior iliac spine (ASIS) or using the flexion plane while making the vertical cut; however, ASIS may not be a good bony landmark because it is far from the surgical field, difficult to palpate for the surgeon and draped. The current literature shows a wide variability among the series in the results of tibial component rotation based on computed tomography (CT) images obtained after UKA [2, 6, 8, 15, 25].
The anteroposterior (AP) axis of the tibia is on the flexion plane of the knee. Because the tibial saw guide is placed parallel to the tibial crest on the flexion plane of the knee, the AP axis of the tibia, which is easy to palpate, observe, and correct intraoperatively, is an appropriate landmark for the vertical cut. We hypothesized that a more accurate vertical tibial cut could be made by placing the saw blade on the flexion plane of the knee, which is created by the tibial crest and saw guide. This study compared tibial component rotation, and radiological and functional results, in patients who underwent Oxford UKA performed using the ASIS or AP axis as the landmark to determine the direction of the vertical cut.
Material and methods
The study was conducted according to the Declaration of Helsinki and a priori institutional review board approval was obtained. Prospectively collected data of 86 consecutive patients who underwent Oxford medial UKA between March 2013 and August 2014, with a diagnosis of anteromedial osteoarthritis and an at least 5‑year postoperative follow-up, were analyzed retrospectively. All patients were operated on by two high volume arthroplasty surgeons who have expertise in Oxford UKA and prefer to use either AP axis (group I) or ASIS (group II) as landmarks for the vertical cut.
Surgical technique
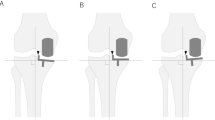
All patients were operated on under a tourniquet, through a mini-medial parapatellar approach using a thigh support and the Oxford microplasty instrumentation system. The surgeons routinely placed the tibial saw guide parallel to the tibial crest in both planes. To place the cutting guide on the AP axis, its distal end was positioned anterior to the midpoint of the bimalleolar line and the tibial crest, while its proximal end was placed just medial to the patellar tendon so that the tibial crest and guide created the flexion plane of the knee. For the vertical tibial cut, the surgeon placed the saw blade parallel to the AP axis of the tibia, just medial to the apex of the medial tibial spine (group I; Fig. 1a–c). In group II, a senior resident palpated the ASIS and placed his fingers on it to show its position to the surgeon, who in turn placed the saw blade just medial to the tip of the medial tibial eminence and pointed it towards the resident’s hand while making the vertical tibial cut (Fig. 2). The medial tibial plateau resection was completed with a transverse cut through the guide. Femoral resection, gap balancing in flexion and extension, and tibial baseplate sizing were performed. Appropriately sized cementless femoral and tibial components were implanted in all patients.
All patients were allowed full weight-bearing as tolerated on the day of or day after surgery and were discharged on the first or second postoperative day. They were followed up at 2 weeks, 6 weeks, and 6 months, and annually thereafter.
Radiological evaluation
A senior resident, who did not participate in the surgeries and was blinded to the groups made all measurements on the PACS system and repeated 2 weeks later for intraobserver reliability, therefore the average values were used in the statistical analysis.
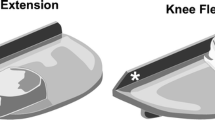
Tibial component rotation was measured on axial CT images (16-MDCT Aquilion 16 system; Toshiba Medical Systems, Japan) obtained at the 2nd week, postoperatively. For CT, the patient was positioned with the lower extremity in full extension and the hips in neutral rotation, with the patella pointing upward. Tibial component rotation (α-angle) was defined as the angle between the line passing through the lateral wall of the tibial component and Akagi’s line, i.e. the line between the center of the tibial attachment site of the posterior cruciate ligament and medial edge of the patellar tendon insertion (Fig. 3; [1]). Based on the reference line, the α‑angle was defined as positive (+) if the tibial component was placed in external rotation (ER) and negative (−) if it was in internal rotation (IR). The instant bearing position (IBP) was evaluated by measuring the angle between the line passing through the lateral wall of the tibial component and a line drawn perpendicular to the radiopaque linear line placed in the anterior part of the bearing (Fig. 4; [15]). Similarly, insert ER relative to the lateral side of the tibial component was considered (+), while IR was considered (−). Posterior overhang of the tibial component into posterior cruciate ligament (PCL) fossa was also assessed on axial CT scans.
Tibial component rotation (α-angle) was measured on axial CT images as the angle between the line passing through the lateral wall of the tibial component (blue line) and Akagi’s line (orange line), i.e. the line between the center of the tibial attachment site of the posterior cruciate ligament and medial edge of the patellar tendon insertion
The varus (−)/valgus (+) angulation of the tibial and femoral components, posterior tibial slope, and femoral component flexion angle were measured on AP and lateral full-length radiographs (Figs. 5 and 6). Posterior tibial slope was considered as (+) and reverse tibial slope as (−). Flexion of the femoral component was considered as (+) and extension as (−).
Functional evaluation
Patients were evaluated using the Oxford knee score (OKS) and Knee Society score (KSS), preoperatively and at the last follow-up. Complications, reoperations, and revisions during follow-up were also recorded.
Outcome parameters
The primary outcome of this study was the α‑angle. Secondary outcomes were varus or valgus of the femoral and tibial components in the coronal plane, posterior tibial slope, flexion of the femoral component in the sagittal plane, rate of posterior overhang of the tibial component into the PCL fossa, and position of the mobile bearing relative to the tibial component (instant bearing position, IBP) in the axial plane [15]. Functional outcomes, i.e. the OKS, KSS and complications, were also analyzed.
Statistical analyses
The statistical analyses were performed using SPSS, version 22 (IBM SPSS Statistics for Windows, Armonk, NY, USA; IBM Corp., Released 2013). In order to find the difference of between the two groups statistically significant in terms of rotational angle, the minimum number of subjects required in each group was determined to be 43 [15] (power of 80% and significance level at 0.05). The statistical significance level was set to p < 0.05.
Kolmogorov-Smirnov test was used to determine if the data were normally distributed. Nonparametric tests of Mann-Whitney U, Wilcoxon signed ranks and Kruskal-Wallis were used to compare continuous variables across the groups. The χ2-test and Fisher’s exact test were used to compare categorical variables between two groups. The median (Q1 (1st quartile)-Q3 (3rd quartile)), mean ± standard deviation, frequency and percentage were reported as descriptive statistics. Intraobserver reliability of the measurements were assessed using the intraclass correlation coefficient and the 95% confidence interval (CI).
Results
Each group consisted of 43 patients with a similar gender distribution. The mean ages of the patients were 65.1 ± 7.2 years in group I and 63.6 ± 8.7 years in group II. Table 1 summarizes the demographic data.
Radiological results
The median α‑angle was significantly smaller in group I than in group II (2.5°, range: −4–5.5° vs. −6 range: −13–0.5), indicating that the tibial component rotation was closer to the neutral in group I (p < 0.001). The median flexion angles of the femoral components (7 vs. 10.5) and posterior tibial slopes (6 vs. 8) were significantly lower in group I than group II (p = 0.001). All other radiological parameters were similar in both groups (Table 2). Radiological parameters did not differ by tibial component size (Table 3). While PCL fossa involvement rate was 32.6% in group, in group 2, this ratio was 39.5%. The rates of PCL fossa involvement were 14 (32.6%) and 17 (39.5) (p = 0.7). The median α‑angle was significantly greater in patients with versus without PCL fossa involvement (−5, range: −13–2 vs. 0.5, range: −5–5.5; p = 0.02).
Functional outcomes
The preoperative and final OKS and KSS were similar in both groups (Table 4). Both groups had significant functional improvements (p < 0.001).
Complications
In group I, two complications were observed and all required reoperation without revision TKA. In group II, there were three complications, with one reoperation and two conversions to TKA.
Discussion
The designers of the Oxford partial knee recommend using the ASIS or flexion plane of the knee as landmarks to ensure an accurate vertical tibial cut for the appropriate tibial baseplate rotation; however, the literature does not clearly demonstrate that one of these two techniques is superior to another. In addition, there are limited data about the effect of tibial component rotation on the functional outcomes and complications. This study found that the tibial AP axis is a better landmark than the ASIS because it enables more accurate tibial component rotation; however, this difference did not influence the clinical outcome, and good and excellent results were obtained using both methods. Different studies have used the ASIS [8, 15], femoral head, medial wall of the intercondylar notch [10], medial femoral condyle, medial intercondylar ridge [29], and tibia AP line [6, 29] as landmarks. Strengths of our study include its comparative design, CT measurements, and evaluation of the effect of the methods on the mid-term clinical outcome. In addition, all measurements were made by a blinded observer.
Making a vertical tibial cut with near-neutral rotation is important. Excessive ER of the tibial component reduces bone support, increases polyethylene wear, and adversely affects the clinical outcome [6,7,8, 16]. Kamenaga et al. showed that the mobile insert hits the lateral wall of the tibial component and tends to escape posteriorly after 60° of knee flexion if it is placed in ER [9]. Excessive IR increases the space available for the baseplate in the mediolateral direction, but this may cause PCL damage [7]. Compared to the ASIS, the AP axis allowed us to achieve significantly more neutral tibial baseplate rotation. This could be due to its location and proximity to the surgeon, which promotes easy palpation and visibility. Although the mean α‑angle was within 6° with both methods, and the Oxford mobile bearing may tolerate this difference, excessive IR or ER was seen in some patients. If up to 10° of malrotation is considered normal, 18 knees in group II had excessive baseplate rotation versus only 3 patients in group I. This shows that the AP axis provides a more reliable landmark and less variation in component rotation than the ASIS. In a magnetic resonance study of healthy knees, Kawahara et al. stated that the medial wall of the intercondylar notch is almost parallel to Akagi’s line [10]; however, its reliability is questionable in cases with osteophytes and advanced degeneration. Comparing the tibial AP line with the medial intercondylar ridge line as a guide, Tsukamoto et al. demonstrated that rotation of the vertical cut is closer to neutral, where neutral rotation provides more surface area for the baseplate when the tibial AP line is used [29]. Theoretically, using the AP axis may help prevent plateau tibia fractures and medial overhang of the baseplate by providing a larger medial tibial surface area.
The mean posterior tibial slope and flexion of the femoral component were higher in group II, which is considered to be unrelated to the method; however, the difference was small and did not affect the OKS or KSS in our series. As we show here, excessive baseplate IR increases the possibility of overhang into the PCL fossa [15]. The designers recommend less than 2 mm of posterior overhang, but we could not demonstrate the clinical importance of this threshold.
The relationship between tibial component rotation and pain and function scores is unclear. Kamenaga et al. reported that increased external tibial rotation was related to decreased OKS and KSS [8], while Iriberri et al. found no significant relationship between tibial rotation and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), KSS, or visual analogue scale (VAS) scores, although the groups with good scores tended to have smaller rotation angles [6]. Liow et al. showed that patients with UKA femoral and/or tibial component rotation angles within 3° external rotation to 3° internal rotation of neutral component alignment reported better functional outcomes [17]. They emphasized that surgeons should be cognizant of the high variability noted in UKA component axial rotation and its potential correlation with functional scores. Additionally internal rotational error of the tibial component could be a major cause of pain after TKA [19]. In our study we found no significant association between tibial rotation and the postoperative OKS or KSS; the degree of improvement in the scores also showed no association with tibial rotation.
This study had some limitations, and the results should thus be interpreted cautiously. First, the patients were not randomized into the groups and surgeons. Therefore, results of this study need to be validated by multicenter, randomized, prospective studies. The sample size was relatively small, although we performed an a priori power analysis based on previous studies [15] and used the minimum number of patients to avoid unnecessary radiation exposure. We did not assess the interobserver reliability of the methods and measurements. Another limitation of the study is that the outcomes in patients with a high body mass index, for whom palpation of the ASIS or tibial crest may be difficult have not been studied. Lastly, the study was not powered to detect a relationship between tibial rotation and complications; however, our primary aim was to compare rotation angles between the methods.
In conclusion, the AP tibial axis is a better landmark for accurate rotation of the vertical tibial cut in Oxford medial partial knee replacement compared to the ASIS; however, the clinical outcomes of the two landmarks are comparable.
References
Akagi M, Oh M, Nonaka T, Tsujimoto H, Asano T, Hamanishi C (2004) An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 420:213–219
Barbadoro P, Ensini A, Leardini A et al (2014) Tibial component alignment and risk of loosening in unicompartmental knee arthroplasty: a radiographic and radiostereometric study. Knee Surg Sports Traumatol Arthrosc 22(12):3157–3162
Berger RA, Della Valle CJ (2010) Unicompartmental knee arthroplasty: indications, techniques, and results. Instr Course Lect 59:47–56
Clarius M, Haas D, Aldinger PR, Jaeger S, Jakubowitz E, Seeger JB (2010) Periprosthetic tibial fractures in unicompartmental knee arthroplasty as a function of extended sagittal saw cuts: an experimental study. Knee 17(1):57–60
Emerson RH Jr., Hansborough T, Reitman RD, Rosenfeldt W, Higgins LL (2002) Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin Orthop Relat Res 404:62–70
Iriberri I, Aragon JF (2014) Alignment of the tibial component of the unicompartmental knee arthroplasty, assessed in the axial view by CT scan: does it influence the outcome? Knee 21(6):1269–1274
Kamenaga T, Hiranaka T, Hida Y, Fujishiro T, Okamoto K (2019) Rotational position of the tibial component can decrease bony coverage of the tibial component in Oxford mobile-bearing unicompartmental knee arthroplasty. Knee 26(2):459–465
Kamenaga T, Hiranaka T, Kikuchi K, Hida Y, Fujishiro T, Okamoto K (2018) Influence of tibial component rotation on short-term clinical outcomes in Oxford mobile-bearing unicompartmental knee arthroplasty. Knee 25(6):1222–1230
Kamenaga T, Hiranaka T, Takayama K, Tsubosaka M, Kuroda R, Matsumoto T (2019) Adequate positioning of the tibial component is key to avoiding bearing impingement in oxford unicompartmental knee arthroplasty. J Arthroplasty 34(11):2606–2613
Kawahara S, Matsuda S, Okazaki K, Tashiro Y, Iwamoto Y (2012) Is the medial wall of the intercondylar notch useful for tibial rotational reference in unicompartmental knee arthroplasty? Clin Orthop Relat Res 470(4):1177–1184
Kendrick BJ, Simpson DJ, Kaptein BL et al (2011) Polyethylene wear of mobile-bearing unicompartmental knee replacement at 20 years. J Bone Joint Surg Br 93(4):470–475
Khanna G, Levy BA (2007) Oxford unicompartmental knee replacement: literature review. Orthopedics 30(5):11–14
Kristensen PW, Holm HA, Varnum C (2013) Up to 10-year follow-up of the Oxford medial partial knee arthroplasty—695 cases from a single institution. J Arthroplasty 28(9):195–198
Lee SY, Bae JH, Kim JG et al (2014) The influence of surgical factors on dislocation of the meniscal bearing after Oxford medial unicompartmental knee replacement: a case-control study. Bone Joint J 96(7):914–922
Lee SY, Chay S, Lim HC, Bae JH (2017) Tibial component rotation during the unicompartmental knee arthroplasty: is the anterior superior iliac spine an appropriate landmark? Knee Surg Sports Traumatol Arthrosc 25(12):3723–3732
Lee YS, Yun JY, Lee BK (2014) Tibial component coverage based on bone mineral density of the cut tibial surface during unicompartmental knee arthroplasty: clinical relevance of the prevention of tibial component subsidence. Arch Orthop Trauma Surg 134(1):85–89
Liow MH, Tsai TY, Dimitriou D, Li G, Kwon YM (2016) Does 3‑dimensional in vivo component rotation affect clinical outcomes in unicompartmental knee arthroplasty? J Arthroplasty 31(10):2167–2172
Murray DW, Goodfellow JW, O’Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br 80(6):983–989
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br 92(9):1238–1244
Pandit H, Jenkins C, Gill HS, Barker K, Dodd CA, Murray DW (2011) Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Joint Surg Br 93(2):198–204
Peersman G, Stuyts B, Vandenlangenbergh T, Cartier P, Fennema P (2015) Fixed- versus mobile-bearing UKA: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 23(11):3296–3305
Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW (2001) Rapid recovery after oxford unicompartmental arthroplasty through a short incision. J Arthroplasty 16(8):970–976
Robertsson O, Knutson K, Lewold S, Lidgren L (2001) The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br 83(1):45–49
Scott RD (2010) Mobile- versus fixed-bearing unicompartmental knee arthroplasty. Instr Course Lect 59:57–60
Servien E, Fary C, Lustig S et al (2011) Tibial component rotation assessment using CT scan in medial and lateral unicompartmental knee arthroplasty. Orthop Traumatol Surg Res 97(3):272–275
Sloper PJ, Hing CB, Donell ST, Glasgow MM (2003) Intra-operative tibial plateau fracture during unicompartmental knee replacement: a case report. Knee 10(4):367–369
Smith TO, Hing CB, Davies L, Donell ST (2009) Fixed versus mobile bearing unicompartmental knee replacement: a meta-analysis. Orthop Traumatol Surg Res 95(8):599–605
Svärd UC, Price AJ (2001) Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br 83(2):191–194
Tsukamoto I, Akagi M, Mori S, Inoue S, Asada S, Matsumura F (2017) Anteroposterior rotational references of the tibia for medial unicompartmental knee arthroplasty in Japanese patients. J Arthroplasty 32(10):3169–3175
White SH, Ludkowski PF, Goodfellow JW (1991) Anteromedial osteoarthritis of the knee. J Bone Joint Surg Br 73(4):582–586
Yoshida K, Tada M, Yoshida H, Takei S, Fukuoka S, Nakamura H (2013) Oxford phase 3 unicompartmental knee arthroplasty in Japan—clinical results in greater than one thousand cases over ten years. J Arthroplasty 28(9):168–171
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
O. Aliyev, M. Ağır, A. Aghazada, D.H. Çeşme, D. Kara, A. Toprak, İ. Tuncay, and F. Yıldız declare that they have no competing interests.
Ethical standards.
All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information
Level of evidence
Level III therapeutic

Scan QR code & read article online
Rights and permissions
About this article
Cite this article
Aliyev, O., Ağır, M., Aghazada, A. et al. Antero-posterior axis of the tibia is a better landmark for tibial component rotation in Oxford medial unicompartmental knee arthroplasty. Orthopädie 51, 996–1002 (2022). https://doi.org/10.1007/s00132-022-04308-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-022-04308-8