Abstract
Introduction: Continuous bedside brain tissue oxygenation (pbrO2) monitoring using the Licox system is an established method for detecting secondary ischemia in comatose patients with acute brain injury. The purpose of the current study was to compare the newly introduced Raumedic pbrO2 probe with the established standard.
Methods: Eighteen patients with acute traumatic brain injury or aneurysmal subarachnoid hemorrhage had pbrO2 probes of both types implanted side by side in the same vascular territory at risk of ischemia. Data were analyzed by the Bland–Altman method as well as random effect regression models to correct for multiple measurements per individual.
Results: Both types of probes were able to display spontaneous fluctuations of pbrO2 as well as reactions to therapy. Mean measurement difference between the Licox and Raumedic probes was −2.3 mmHg, with corresponding 95% limits of agreement of −32.3 to 27.5 mmHg. Regarding an ischemia threshold of 15 mmHg, both probes were in agreement in 78% and showed disparate results in 22%.
Conclusions: Our data suggest that the pbrO2 measurements of the two systems cannot be interchanged. Although we were unable to determine which system delivers more valid data, we do think that more rigorous testing is necessary before implementing the new probe in clinical routine.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Continuous bedside brain tissue oxygenation (pbrO2) monitoring with the Licox system (Integra Neuroscience) is an established method of detecting secondary ischemia in comatose patients with acute brain injury. In patients after traumatic brain injury and subarachnoid hemorrhage, a relationship between pbrO2 monitoring and outcome has recently been established [1–3]. Owing to its stability and the lack of competition, the Licox pbrO2 sensor became the de facto gold standard.
Recently, a new pbrO2 probe by a different manufacturer (Neurovent PTO, Raumedic) was introduced. This new probe facilitates concurrent measurement of intracranial pressure (ICP), brain temperature, and pbrO2. Therefore, its use would reduce the invasiveness of multimodal neuromonitoring. However, before new technology is introduced, its performance and compatibility with the existing standards need to be established. The ICP component of the new probe has shown favorable performance in bench testing and multicenter evaluation [4, 5]. The purpose of the present study was to investigate the level of agreement of pbrO2 values from the Licox and Raumedic probes in routine clinical use.
Materials and Methods
In 23 comatose patients requiring mechanical ventilation after aneurysmal subarachnoid hemorrhage or traumatic brain injury, a Licox CC1.SB pbrO2 probe (Integra Neuroscience, Saint Priest, France) and a Neurovent PTO probe (Raumedic, Münchberg, Germany) were implanted side by side in the same vascular territory at risk of ischemia (Fig. 1). Placement target was the frontal white matter, either the side of the more severely injured hemisphere after traumatic brain injury or the tissue supplied by the aneurysm-harboring vessel after subarachnoid hemorrhage. The indication for implementation of advanced neuromonitoring using parenchymal ICP and pbrO2 probes was based solely on clinical grounds at the discretion of the neurosurgeon in charge.
Patients were treated during 2008 in the Department of Neurosurgery, Klinikum Bogenhausen, Technical University of Munich, Germany and from June 2009 until April 2010 in the Department of Neurosurgery at Campus Virchow, Charité University Berlin, Germany. Thirteen of the patients in Berlin were included in a prospective study investigating the pbrO2 reactivity of the two probes. Their next of kin gave informed consent, as required by the local ethics committee. For anonymous review of the data from the other patients, the need for informed consent was waived.
Multimodal neuromonitoring data were stored online with dedicated software (ICUpilot, CMA Microdialyis, Solna, Sweden, in Munich, and ICMplus, University of Cambridge, UK, in Berlin, respectively) and averaged once per minute. Only pbrO2 values within the clinical relevant range between 1 and 50 mmHg were investigated. Measurements outside this range were discarded to reduce distortion of the numerical analysis by outlying values.
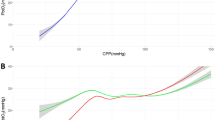
Data were analyzed graphically by plotting the difference against the corresponding mean of single measurements from both probes, as proposed by Bland and Altman [6]. A second plot was performed with the differences expressed as percentage of the means. In Bland–Altman analysis, the mean of all differences defines the bias of measurements and the borders of the 95% confidence interval of mean differences are traditionally termed as the limits of agreement.
Both plots showed a dependency of the mean differences in magnitude and variance on the mean pbrO2. As this and the repeated measurement nature of the data with multiple values per individual are limitations of the classic Bland–Altman analysis [7], random effects modeling was performed for appropriate statistical analysis [8]. To facilitate comparability with other published work, the classical limits of agreement, without consideration of the aforementioned violations of the Bland–Altman approach, were also calculated.
Results
Data from 18 of the 23 patients were analyzable. In three patients, one of the two probes was located in infarcted tissue on CT following implantation. One patient required craniectomy for refractory ICP due to brain swelling a few hours after probe placement and both probes had to be removed. In another patient, the pbrO2 part of the Raumedic probe was malfunctioning after implantation. Consequently, data from these patients were excluded. Additionally, the pbrO2 part of five Raumedic probes ceased to function prematurely and data after this time were removed.
Mean analyzed measurement time per patient was 6.7 days. In total, 172,585 min of pbrO2 data were evaluated. When all data were pooled, mean pbrO2 values were 25.7 (SD 11.5) mmHg using Licox probes and 28.0 (SD 14.9) mmHg with Raumedic probes, giving a mean bias of −2.3 mmHg or −8.8%. Bias was widely scattered between patients (−22.1 to 19.5 mmHg).
Both types of probes were able to display spontaneous fluctuations of pbrO2 as well as reactions to therapy. Analysis of single patients revealed no discernible pattern in the relationship between measurement values of the two probes (Fig. 2). Regarding an ischemia threshold of 15 mmHg, as suggested for the Licox system, both probes were in agreement in 78% and showed disparate results in 22% of single measurement points.
Measurement time series of the Raumedic and the Licox pbrO2 probe (same patient as in Fig. 1). Although both seem to capture short-term trends and fluctuations accurately, there is no constant, recognizable pattern for a transfer function
The 95% limits of agreement according to a classic Bland–Altman analysis were −32.3 to 27.5 mmHg or −118% to 112% (Fig. 3). Further investigation with a random effects model to consider repeated measurements, non-constant mean difference, and changing variance over the measurement range gave a more appropriate characterization of the data (bold dashed lines in Fig. 3). Bias and 95% limits of agreement were significantly related to the mean pbrO2 in each instance of different random effects models with the mean difference expressed either absolute or as a percentage (all: p < 0.001). Licox probes showed a tendency toward higher values at low pbtO2, while the values from the Raumedic probes were higher at high pbrO2.
Discussion
The main finding of our study was that pbrO2 measurements of the Licox and the Raumedic systems show a large discrepancy, although both probes were implanted side by side in the same vascular territory. We were unable to find a reliable transfer algorithm for conversion of measurement data from one system to the other. However, we want to emphasize that our study design did not allow us to determine which system delivers more valid data.
Classic Bland–Altman analysis is known to underestimate the limits of agreement in the case of repeated measurements in the same individual [7]. Random effects modeling allows a more adequate statistical assessment, but is of course not able to remove the scatter present in the raw data. However, judgment on the exchangeability of measurements from the two devices is a clinical decision that depends on the required accuracy and not on statistical significance. A maximum difference of 30% was proposed to rate two different methods of measurement as equal [9]. This failed with either type of statistical description.
So far, published data on the comparison of both probes are inconclusive [10–12]. In laboratory bench testing using calibrated oxygenated fluids, both probes were accurate in detecting different oxygen tensions and did not deviate over longer recording times [10]. Differences were found in response time to changes in oxygen tension, favoring the Raumedic system. A swine model showed a similar baseline measurement of the two probes, but revealed significantly different profiles during hyperoxygenation and a faster response time for the Raumedic probe [11]. In their conclusion, the authors questioned whether the existing knowledge on the hypoxic threshold established for the Licox probe might be directly transferred to the new system. A clinical comparison study with a similar design to ours showed limits of agreement of the same magnitude (95% CI: −25.1 to 22.6 mmHg) [12]. Nevertheless, the authors suggested that both probes might be used interchangeably, but cautioned with regard to their interpretation owing to several limitations of their study. Of further concern in this and in our study is a high rate of mechanical failure of the pbrO2 part of the Raumedic probe.
The reasons for the wide limits of agreement of pbrO2 measurements of the two probes are unknown. A possible explanation may be the heterogeneity of pbrO2, especially when it is measured in tissue at risk of ischemia. Furthermore, the Licox probe is based on a Clark-type polarographic electrode, while the Raumedic probe uses luminescence quenching [12]. The level of pbrO2 is dependent on the amount of brain edema, cerebral blood flow and metabolism including pH changes induced by hyperventilation. Interactions of biochemical tissue conditions with one or both measurement principles of the pbrO2 probes seem at least conceivable. As the clinical implications of ischemia detection using bedside pbrO2 measurements are great, both theories warrant further investigation.
Conclusion
Our data suggest that the pbrO2 measurements of the two systems cannot be interchanged. We found no reliable transfer algorithm for the conversion of measurement data from one system to the other. Although we want to emphasize that we were unable to determine which system delivers more valid data, we do think that more rigorous testing is necessary before the new probe is implemented in clinical routine. In our opinion, local pbrO2 heterogeneity and the different perception of changes in oxygen tension in biological tissue are possible explanations for the disparate measurements of the two probes and warrant further investigation.
References
Ramakrishna R, Stiefel M, Udoetuk J, Udoteuk J, Spiotta A, Levine JM et al (2008) Brain oxygen tension and outcome in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg 109(6):1075–1082
Narotam PK, Morrison JF, Nathoo N (2009) Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg 111(4):672–682
Spiotta AM, Stiefel MF, Gracias VH, Garuffe AM, Kofke WA, Maloney-Wilensky E et al (2010) Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg 113(3):571–580
Citerio G, Piper I, Cormio M, Galli D, Cazzaniga S, Enblad P et al (2004) Bench test assessment of the new Raumedic Neurovent-P ICP sensor: a technical report by the BrainIT group. Acta Neurochir (Wien) 146(11):1221–1226
Citerio G, Piper I, Chambers IR, Galli D, Enblad P, Kiening K et al (2008) Multicenter clinical assessment of the Raumedic Neurovent-P intracranial pressure sensor: a report by the BrainIT group. Neurosurgery 63(6):1152–1158; discussion 1158
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8(2):135–160
Myles PS, Cui J (2007) Using the Bland-Altman method to measure agreement with repeated measures. Br J Anaesth 99(3):309–311
Critchley LA, Critchley JA (1999) A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput 15(2):85–91
Purins K, Enblad P, Sandhagen B, Lewén A (2010) Brain tissue oxygen monitoring: a study of in vitro accuracy and stability of Neurovent-PTO and Licox sensors. Acta Neurochir (Wien) 152(4):681–688
Orakcioglu B, Sakowitz OW, Neumann JO, Kentar MM, Unterberg A (2010) Evaluation of a novel brain tissue oxygenation probe in an experimental swine model. Neurosurgery 67(6):1716–1722; discussion 1722–1723
Huschak G, Hoell T, Hohaus C, Kern C, Minkus Y, Meisel H (2009) Clinical evaluation of a new multiparameter neuromonitoring device: measurement of brain tissue oxygen, brain temperature, and intracranial pressure. J Neurosurg Anesthesiol 21(2):155–160
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag/Wien
About this chapter
Cite this chapter
Wolf, S., Horn, P., Frenzel, C., Schürer, L., Vajkoczy, P., Dengler, J. (2012). Comparison of a New Brain Tissue Oxygenation Probe with the Established Standard. In: Schuhmann, M., Czosnyka, M. (eds) Intracranial Pressure and Brain Monitoring XIV. Acta Neurochirurgica Supplementum, vol 114. Springer, Vienna. https://doi.org/10.1007/978-3-7091-0956-4_30
Download citation
DOI: https://doi.org/10.1007/978-3-7091-0956-4_30
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-0955-7
Online ISBN: 978-3-7091-0956-4
eBook Packages: MedicineMedicine (R0)