Abstract
The current clinical practice of tissue handling and sample preparation is multifaceted and lacks strict standardisation: this scenario leads to significant variability in the quality of clinical samples. Poor tissue preservation has a detrimental effect thus leading to morphological artefacts, hampering the reproducibility of immunocytochemical and molecular diagnostic results (protein expression, DNA gene mutations, RNA gene expression) and affecting the research outcomes with irreproducible gene expression and post-transcriptional data. Altogether, this limits the opportunity to share and pool national databases into European common databases. At the European level, standardization of pre-analytical steps is just at the beginning and issues regarding bio-specimen collection and management are still debated. A joint (public–private) project entitled on standardization of tissue handling in pre-analytical procedures has been recently funded in Italy with the aim of proposing novel approaches to the neglected issue of pre-analytical procedures. In this chapter, we will show how investing in pre-analytics may impact both public health problems and practical innovation in solid tumour processing.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Why New Projects in Pre-analytical Phases of Surgical Pathology
The current clinical practice of tissue handling and sample preparation is multifaceted and lacks strict standardisation: this scenario leads to significant variability in the quality of clinical samples. Technological innovations that pursue standardisation of pre-analytical processes in surgical pathology represent fundamental tools to assure correct diagnosis, which in turn will enhance treatment decisions. Standardisation of bioptic and surgical specimens is not only a need of patients but also of researchers. The detrimental effect of poor tissue preservation (i) leads to morphological artefacts; (ii) hampers the reproducibility of immunocytochemical and molecular diagnostic results (protein expression, DNA gene mutations, RNA gene expression) and (iii) affects the research outcomes with irreproducible gene expression and post-transcriptional data, thus limiting the opportunity to share and pool national databases into European common databases.
Moreover, fostering an upgrade in surgical pathology is not easier than in other healthcare fields, due to the escalating costs, long product development cycles and protracted regulatory approval. It is well known that the difficulties in economics in Europe involve also the healthcare public system thus inhibiting the innovation process. Finally, pathologists are not keen to change their habits. Procedures for preservation and processing of human tissue obtained from biopsies and surgical specimens date back to Rudolf Virchow in the nineteenth century, anachronistically known as the ‘father of modern pathology’.
On one hand, pathologists should start thinking about the possibilities to apply for funding in order to create a network open to different stakeholders. On the other hand, institutions should be better informed of our work and thus understand that our everyday diagnosis may be not scientifically sexy, but needs to be as precise, reliable and up to date as possible for the patient care.
A recent ‘viewpoint’ article [1] calls on pathologists to consider that as genomic testing becomes part of routine care and patients become increasingly informed, the workflow of pathology lab will have to adapt to meet the demands of the ‘next generation of patients’.
Pathologists are also expected to facilitate procurement, preservation and distribution of tissues to qualified biomedical researchers. Dr. Compton, Director of the National Cancer Inst. Office of Biorepositories and Biospecimen Research, said that billions of dollars have been wasted in the past because researchers developing biomarkers supposed to be predictive of cancer and response to therapies relied on tissue samples that were utterly useless; tissues had been subjected to careless handling, in addition storage and sampling procedures were missing, so that results were not reproducible.
Changing practices within both the pathology and oncology communities is not a trivial task but it is bound to happen, since the field has no better choice.
2 Examples of Funding Opportunities and Projects Financed in Pre-analytics
In the USA, the Cancer Diagnosis Program of the National Cancer Institute (NCI) has recently invited applications for cooperative agreement awards for the NCI-supported Collaborative (currently “Cooperative”) Human Tissue Network (CHTN) (http://www.chtn.nci.nih.gov/).
The goal for CHTN is to collect and distribute high-quality human tissue specimens to facilitate basic and early translational cancer research. The CHTN is designed as a unique biospecimen resource as it is based on prospective collection and distribution of samples upon specific investigators’ requests.
This Funding Opportunity Announcement (FOA—Funding Opportunity: RFA-CA-13-007) solicits applications for CHTN awards from institutions/teams capable of contributing to the mission of CHTN by: (1) providing prospective investigator-defined procurement of high-quality malignant, benign, diseased and uninvolved (normal adjacent) tissues and fluids from patients throughout North America and elsewhere; (2) assisting individual investigators with regard to specific specimen needs of their research; (3) assisting in developing and disseminating knowledge on high-quality practices for successfully operating a biospecimen repository and (4) educating the community about the importance of the availability of high-quality human tissue specimens for medical research.
At the European level, standardisation of pre-analytical steps is just at the beginning and issues regarding bio-specimen collection and management are still debated.
Of note, in the last 7th Framework Programme (7FP) the EU funded some programs that pertain to pre-analytic issues and biobanking. As an example, SPIDIA (http://www.spidia.eu/) is a 4.5 year project, funded by the European Union FP7 programme to the value of 9 million Euros, which brings together a consortium of 16 leading academic institutions, international organisations and life sciences companies. The project is coordinated by QIAGEN-GmbH. It aims at tackling the standardisation and improvement of pre-analytical procedures for in vitro diagnostics. The proposed research and standardisation activities cover all steps from creation of evidence-based guidelines to creation of tools for the pre-analytical phase to testing and optimisation of these tools through the development of novel assays and biomarkers.
3 Current Projects and Goals in Italy
In 2012, the Ministry of Health in Italy co-funded together with Milestone srl (Bergamo, Italy—http://www.milestonemedsrl.com/histopathology/index.php) a joint (public–private) project entitled “Standardizing tissue handling in pre-analytical procedures: technological, environmentally-safe innovation in solid tumour processing” (Project Code: RF-2010-2310674). The project proposes novel approaches to the neglected issue of tissue handling in pre-analytical procedures, taking into account both public health problems and practical innovation in solid tumour processing.
The aims of the project were:
-
1.
To standardize and validate the use of Under Vacuum Sealing and Cooling (UVSC) procedure for handling and preserving fresh surgical specimens before fixation.
To overcome the concern related to the use of formalin in the surgery room we have proposed the use of an innovative vacuum biospecimen transfer system (tissueSAFE-Milestone, Italy) [2]. Our aim was to restrict the use of formalin only in pathology labs, where this toxic agent is carefully handled with hoods and gloves in safe environmental conditions. Tissue transfer in UVSC conditions meets the requests of both health authorities and workers by reducing the exposure to formaldehyde; furthermore, the cost related to the UVSC are lower than those related to the traditional transport in formalin immersion.
Standardising the temperature of transport and storage is another important issue. In transplantation pathology it has been shown that a rapid induction of hypothermia at 0–4 °C by perfusion of organ with specific solutions better preserves organ viability [3, 4]. It seems that it is the prompt cooling that principally influences preservation. For instance, Kristensen and colleagues [5] have shown that storage at 4 °C preserved tissues to a higher degree than storage at room temperature, independently of whether the tissue was subjected to vacuum sealing or not. We have proposed the transfer of surgical specimens vacuum-sealed using a chilled plastic box at 4 °C [6]. Our results suggest the avoidance of insulating air around tissues with the UVSC system allows faster cooling at 4 °C. We are working on the rapid reduction of temperature to preserve as much as possible the tissue viability, and the integrity of phosphorylated proteins and of nucleic acids.
The other problem is to monitor the cold ischemia time (which corresponds to the UVSC time) that starts when the specimen is excised and ends with placement in a suitable tissue fixative. When dealing with cell cultures and xenograft implantations researchers may ideally wish to collect the sample for experiments directly in the surgery room in order to keep the cold ischemia time as short as possible. However, any such sampling may lead to problems for pathologists in terms of correct gross evaluation of tumour samples (status of surgical margins, staging etc.). UVSC may therefore represent a valuable strategy to allow tissue sampling for research purposes and proper preservation of tissue specimens for gross evaluation. However, the results of our project show that although UVSC maintains cell viability even after 70 h, the percentage of cell death increases for longer UVSC times [7].
-
2.
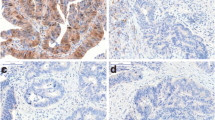
To standardize and validate the use of cold-fixation of tissues for histological diagnosis and long-term preservation of nucleic acids and proteins after paraffin embedding.
Preliminary data using cold-formalin fixation show that this procedure preserves RNA segments up to 660 bp and that both morphological and immunophenotypical features are fully comparable with those obtained with standard fixation [8]. Gene expression profiling analysis showed that RNAs from cold-fixed samples are significantly less fragmented than those from standard Formalin-Fixed Paraffin-Embedded (FFPE) samples: their performance was comparable to that shown by fresh-frozen samples, which are, at present, the sole specimens considered suitable for microarray gene expression analysis.
For the project purposes, the cold-FFPE samples were re-profiled after 24 months to assess the stability of morphology, antigens and nucleic acids. The preliminary results confirmed that cold fixation is a robust procedure to maintain the integrity of these molecules.
4 Conclusion
Pathologists have to move a step forward to face innovation of their procedures taking into account the ethical, legal and social issues. In addition, we need both the support of companies/SMEs for the development of new technologies for tissue preservation and of government to facilitate professionals in rapidly translating the results of new projects into practice.
References
Goetz L, Bethel K, Topol EJ (2013) Rebooting cancer tissue handling in the sequencing era: toward routine use of frozen tumor tissue. JAMA 309(1):37–38. doi:1555140 [pii].10.1001/jama.2012.70832
Di Novi C, Minniti D, Barbaro S, Zampirolo MG, Cimino A, Bussolati G (2010) Vacuum-based preservation of surgical specimens: an environmentally-safe step towards a formalin-free hospital. Sci Total Environ 408(16):3092–3095. doi:10.1016/j.scitotenv.2010.04.022S0048-9697(10)00400-6
Belzer FO, Southard JH (1988) Principles of solid-organ preservation by cold storage. Transplantation 45(4):673–676
D’Alessandro AM, Southard JH (2002) Hypothermic perfusion of the warm ischemic kidney: is 32 degrees C better than 4 degrees C? Am J Transplant 2(7):689,690
Kristensen T, Engvad B, Nielsen O, Pless T, Walter S, Bak M (2011) Vacuum sealing and cooling as methods to preserve surgical specimens. Appl Immunohistochem Mol Morphol 19(5):460–469. doi:10.1097/PAI.0b013e318214e523
Bussolati G, Chiusa L, Cimino A, D’Armento G (2008) Tissue transfer to pathology labs: under vacuum is the safe alternative to formalin. Virchows Arch 452(2):229–231. doi:10.1007/s00428-007-0529-x
Annaratone L, Marchio C, Russo R, Ciardo L, Rondon-Lagos SM, Goia M, Scalzo MS, Bolla S, Castellano I, Verdun di Cantogno L, Bussolati G, Sapino A (2013) A collection of primary tissue cultures of tumors from vacuum packed and cooled surgical specimens: a feasibility study. PLoS ONE 8(9):e75193. doi:10.1371/journal.pone.0075193 PONE-D-13-12418
Bussolati G, Annaratone L, Medico E, D’Armento G, Sapino A (2011) Formalin fixation at low temperature better preserves nucleic acid integrity. PLoS ONE 6(6):e21043. doi:10.1371/journal.pone.0021043 PONE-D-11-03447
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sapino, A., Annaratone, L., Marchiò, C. (2015). Current Projects in Pre-analytics: Where to Go?. In: Dietel, M., Wittekind, C., Bussolati, G., von Winterfeld, M. (eds) Pre-Analytics of Pathological Specimens in Oncology. Recent Results in Cancer Research, vol 199. Springer, Cham. https://doi.org/10.1007/978-3-319-13957-9_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-13957-9_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-13956-2
Online ISBN: 978-3-319-13957-9
eBook Packages: MedicineMedicine (R0)