Abstract
Autism spectrum disorder (ASD) is becoming an increasingly prevalent chronic health condition in childhood. Therefore, the quality of health care among children with ASD has gained increased importance for health-care providers and policymakers. As this chapter demonstrates, health-care experiences, quality, and outcomes for children with ASD are poorer than for children with other types of health conditions, likely in part due to the complex nature of ASD and its all-encompassing effect on children and their families. Fewer than one in four children with ASD meet standards of a defined minimum quality of care index, and less than half receive care that meets all or all but one of the core outcomes performance standards defined by the Maternal and Child Health Bureau’s System of Care for Children with Special Health Care Needs. Improvements to ASD care are greatly needed so that children with ASD can attain their full health and developmental potentials.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Health-Care Quality Measurement and Improvement Efforts for Children with Autism Spectrum Disorder in the United States
Recent population estimates suggest that approximately 1 in every 88 US children has an autism spectrum disorder (ASD), and the prevalence of this disorder is increasing (Centers for Disease Control and Prevention [CDC] 2012; Kogan et al. 2009). Given the number of children who are affected by ASD and the impact of the condition on their families and communities, measuring health-care quality for children with ASD has gained increased importance (Baron-Cohen et al. 2009; Boyle et al. 2011; Shieve et al. 2012). Recent health-care legislation has emphasized the importance of quality measurement for children with autism specifically (e.g., the Combating Autism Reauthorization Act of 2011) and also as part of the larger population of children with special health-care needs (CSHCN) (e.g., the Children’s Health Insurance Program Reauthorization Act of 2009 and the Patient Protection and Affordable Care Act of 2010). Based on the federal Maternal and Child Health Bureau (MCHB) definition of children with special health-care needs (CSHCN) (McPherson et al. 1998), here, CSHCN are those who experience any type of chronic physical, developmental, behavioral, or emotional condition (having lasted or expected to last at least 12 months) for which they require health and related services of a type or amount above those required by children generally.
When children with ASD receive high-quality care, both they and their families may have improved health outcomes and functional status (Kogan et al. 2008; Perrin 2012). For example, findings from a study conducted by Kogan et al. (2008) demonstrated that children with ASD who received care within a medical home had family members who were less likely to experience financial and employment impacts compared to children with ASD who lacked a medical home. Others have found that the receipt of care within a medical home may also enhance patient experiences of care as well as shared decision-making between providers and families of children with ASD (Brachlow et al. 2007; Golnik et al. 2012; Hyman and Johnson 2012; Kogan et al. 2008; Sheldrick and Perrin 2010).
Lifetime costs, including those related to health care, have been found to exceed one million dollars for children with ASD (Leslie and Martin 2007). Despite this, children with ASD unfortunately receive some of the lowest quality of care of all CSHCN. For instance, a recent study revealed that only 22.8 % of children with ASD met a minimum quality of care index indicating that they had (1) adequate health insurance, (2) at least 1 preventive medical care visit in the past year, and (3) received care meeting baseline criteria for being a medical home (Bethell et al. 2011). This was the lowest rate of any of the 22 health conditions examined in the study. To elucidate why children with ASD may experience poor health-care quality, previous research has examined health-care quality for children with ASD and its associations with the sociodemographic characteristics of children and their families (Begeer et al. 2009; Liptak et al. 2008; Mandell et al. 2009; Montes and Halterman 2011); condition severity (Bethell et al. 2011); complexity of health-care needs (Ahmedani and Hock 2012; Bethell et al. 2011); risk and protective factors interconnected with the home, school, and neighborhood environments (Kalkbrenner et al. 2011); and programs and policies in the state or county of residence (Mandell et al. 2012; Thomas et al. 2012). Still, a comprehensive report on the health and quality of care among children with ASD compared to other CSHCN and compared to the general US pediatric population has not yet been established from which systemic improvements may be monitored over time.
Thus, this chapter takes a comprehensive approach to profiling health-care quality related to the health-care needs of children with ASD and reviews actual health-care quality experienced by children with ASD who have qualified as CSHCN on the Children with Special Health Care Needs Screener (referred to herein as CSHCN + ASD) in two national surveys. The CSHCN Screener is a five-item parent-completed tool that identifies children who currently experience one or more of five common health consequences due to a physical, mental, behavioral, or other type of health condition that has lasted or is expected to last at least 12 months (Bethell et al. 2002; Bramlett et al. 2009). Unsurprisingly, nearly all children whose parents report that they currently have ASD qualify as CSHCN, because of the condition’s impact on their functioning and health-care needs for specialized services (Ahmedani and Hock 2012; Bethell et al. 2011; Boulet et al. 2009; Bryson et al. 2008; Gurney et al. 2006; Joshi et al. 2010; Kogan et al. 2009; Narendorf et al. 2011). Analyses in this chapter compare CSHCN + ASD to other CSHCN (referred to herein as CSHCN-ASD) and children without special health-care needs (referred to herein as non-CSHCN). Data were gathered from the 2009–2010 National Survey of Children with Special Health Care Needs (NS-CSHCN) and the 2007 National Survey of Children’s Health (NSCH). The NS-CSHCN and NSCH provide population-based national- and state-level estimates on a wide range of child health, quality of care, and family and community factors imperative to shaping programs and policies (Kogan et al. 2012). Detailed survey methodology is provided in the technical methods appendix and may also be accessed online at www.childhealthdata.org. A synopsis of the analytic strategy employed is provided in Text Box A.
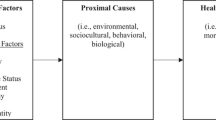
This chapter’s key findings profile US CSHCN + ASD with respect to their (1) sociodemographic characteristics and health-care needs, (2) ASD health and related impacts at both the child and family level, (3) health services needs and utilization, (4) child and family risk and protective factors for healthy development, and (5) access to and quality of health care received, using the federal MCHB System of Care for CSHCN framework that includes six age-relevant core outcomes (Fig. 1).
US Children with Autism Spectrum Disorder and Special Health-Care Needs
ASD Prevalence and Severity
According to 2007 NSCH findings previously reported by Kogan et al. (2009), the overall prevalence of ASD among US children aged 3–17 years is 1.1 %, or an estimated 673,000 children nationwide. More recent findings from the 2009–2010 NS-CSHCN reveal that an estimated 820,000 US CSHCN age 3–17 years have ASD. Though the difference between the 2007 NSCH and 2009–2010 NS-CSHCN ASD prevalence rates among US CSHCN may in part be attributed to the methodological differences that exist between the NS-CSHCN and NSCH (Bethell et al. 2008); prevalence may have actually increased due to ongoing ASD diagnostic criteria modifications and screening processes (Johnson and Myers 2007; Hertz-Picciotto and Delwiche 2009), changing exposure to an array of risk factors (Kinney et al. 2010; Shelton et al. 2010), and other temporal and environmental factors (Ratajczak 2011; Rice 2011). Slightly over half of CSHCN + ASD were reported to have moderate or severe ASD by their parents according to findings from both the 2009–2010 NS-CSHCN (50.5 %) and 2007 NSCH (53.5 %); this is likely an underestimate since parents tend to conservatively report the severity of conditions that their children experience (Simon et al. 2008).
Sociodemographic Characteristics
The sociodemographic characteristics of US CSHCN + ASD relative to CSHCN-ASD age 3–17 years are presented in Table 1; sociodemographic findings for children with ASD relative to all US children aged 3–17 years have been previously reported (Kogan et al. 2009). To summarize, CSHCN + ASD were significantly more likely than CSHCN-ASD to be male (80.4 %; P < .001), live in a household with two biological or adoptive parents (61.9 %; P = .001), have at least one parent who achieved more than a high school education (76.3 %; P < .001), and reside in the northeastern or western regions of the United States (45.7 %; P < .001). CSHCN + ASD were also significantly less likely to have private health insurance (45.8 %) than CSHCN-ASD (54.2 %; P < .001).
Special Health-Care Needs and Multiple Conditions
In general, CSHCN + ASD were more medically complex than CSHCN-ASD (Table 1). While some CSHCN experienced conditions that are largely managed by prescription medications, nearly all (97.4 %) CSHCN + ASD required additional services to manage their health conditions, such as specialized therapy or mental health counseling. CSHCN + ASD were also more likely than other CSHCN to have multiple conditions: 56.2 % of CSHCN + ASD had four or more conditions, from a list of 20 specific health conditions asked about in the NS-CSHCN, compared to 13.3 % of CSHCN-ASD (AOR 10.77, [9.25–12.54]; P < .001). These findings align with previous research demonstrating that children with ASD have greater health-care needs (Boulet et al. 2009; Narendorf et al. 2011) in addition to a higher likelihood of experiencing multiple conditions, particularly psychiatric conditions, relative to other children (Joshi et al. 2010; Kogan et al. 2009; Kohane et al. 2012; Levy et al. 2008; Simonoff et al. 2008).
Quality of Care Relevant Health Impact of ASD on Children and their Families
The functional status and daily activities of CSHCN + ASD are important health outcomes that are potentially impacted by the health-care quality they receive. Here, five measures of child functioning along with three measures of financial and employment impacts on families from the 2009–2010 NS-CSHCN were evaluated for CSHCN + ASD, including discrepancies among various subgroups. Key findings are displayed in Fig. 2.
Impact of ASD on children and families from the 2009–2010 National Survey of Children with Special Health Care Needs. (Measures were computed for CSHCN age 3–17 years, unless otherwise indicated. Raw n in parantheses. All odds ratios reported were adjusted for child’s age, sex, race/ethnicity, household income, primary household language, and US geographic region using logistic regression analysis unless otherwise specified. For all AORs, the referent group was CSHCN who were never told they have ASD.) This figure depicts the weighted prevalence and adjusted odds ratios of CSHCN+ASD relative to CSHCN–ASD who were impacted by their conditions in their daily activities in addition to those who experienced family-level impacts related to employment and finances based on 2009–2010 NS-CSHCN data
Impact on Child Functioning and Activities
Overall, CSHCN + ASD experienced greater impacts on functioning and daily activities than did CSHCN-ASD: CSHCN + ASD had 8.23 times higher adjusted odds of having conditions that consistently affected their activities often or a great deal in comparison to CSHCN-ASD (95 % CI, 7.12–9.51). Strikingly, CSHCN + ASD also had 18.21 greater adjusted odds of experiencing four or more functional difficulties from a list of 14 specific difficulties (e.g., difficulty with self-care activities, behavior problems, and hearing difficulties even when using hearing aids) relative to CSHCN-ASD (95 % CI, 14.87–22.31). ASD was also found to interfere with children’s participation in extracurricular activities (AOR: 6.00, [5.15–6.99]) and school attendance (AOR: 1.79, [1.46–2.19]).
Quality of care for CSHCN + ASD impacted functioning: CSHCN + ASD who did not receive care within a medical home had 1.65 greater adjusted odds of being consistently affected in their daily activities due to their conditions compared to those CSHCN + ASD who received care within a medical home (95 % CI, 1.23–2.21). Health insurance adequacy was also associated with functioning for CSHCN + ASD: CSHCN + ASD with inadequate insurance were more likely than CSHCN-ASD to have missed 11 or more school days (AOR 1.79, [1.22–2.63]).
Impact on Family
Previous research suggests that parental stress, health, and well-being may also be associated with child health status and development (Krakowiak et al. 2012; Victorino and Gauthier 2009). Results from the 2007 NSCH show that having a child with ASD is associated with poorer parental health: compared to children who do not qualify as CSHCN (non-CSHCN), CSHCN + ASD had lower adjusted odds of having fathers with excellent or very good physical and mental health (AOR 0.56, [0.38–0.83]) or having mothers with excellent or very good physical and mental health (AOR 0.37, [0.26–0.51]). As demonstrated by previous research (Schieve et al. 2011) and confirmed here, CSHCN + ASD (53.9 %) were also more likely to have parents who often experienced stress from parenting compared to non-CSHCN (8.1 %; AOR: 16.47, [11.40–23.81]).
Families of CSHCN + ASD are more likely to experience difficulties with employment and finances (Cidav et al. 2012; Kogan et al. 2008). Analyses here show that compared to CSHCN-ASD, CSHCN + ASD had higher adjusted odds of having a family member who cut back and/or stopped working due to the child’s condition(s) (AOR: 5.32, [4.61–6.13]), having a family member who avoided changing jobs because of concerns about maintaining the child’s health insurance (AOR: 2.29, [1.97–2.66]), and having a family member who experienced financial problems due to the child’s health-care needs (AOR: 3.36, [2.90–3.89]). When CSHCN + ASD were adequately insured, impacts were lessened: CSHCN + ASD whose insurance coverage was inadequate had higher adjusted odds of having family members who cut back and/or stopped working (AOR: 1.87, [1.40–2.49]) and who experienced financial problems (AOR: 3.23, [2.41–4.33]) compared to CSHCN + ASD whose insurance was adequate. The quality of a child’s health care also impacted family finances and employment: among CSHCN + ASD, those who did not receive care within a medical home had 2.21 greater adjusted odds of having families who experienced financial problems due to the child’s condition(s) (95 % CI, 1.57–3.13) and 1.47 greater adjusted odds of having family members who cut back and/or stopped working because of the child’s condition(s) (95 % CI, 1.10–1.97) relative to CSHCN + ASD who received care within a medical home.
Quality of Care Relevant Risk and Protective Factors for Children with ASD
Risk and protective factors in early childhood influence a child’s long-term developmental trajectory and are essential to address in the context of high-quality health care (Fine and Kotelchuck 2010; Forrest and Riley 2004; Halfon and Hochstein 2002). Essential factors influencing health are contextual and time sensitive in nature, exerting the greatest influence on the health of children in their homes, schools, and neighborhoods during certain developmental periods. At a population level, the systemic effects of such factors may determine disparities or equity in health and quality of care. For this reason, select risk and protective factors with special relevance for health-care quality among CSHCN + ASD were examined using three previously reported on indices of home, school, and neighborhood environmental factors (Table 2; Text Box B). Two age-relevant indices of protective home environment and neighborhood safety and support contextual factors were constructed from the 2007 NSCH (Text Box B), as previously documented and reported on for all US CSHCN and non-CSHCN (US Department of Health and Human Services, Health Resources and Services Administration [HRSA], MCHB, 2011). A third index of factors promoting school success was used (Text Box B), previously constructed and reported on for all US CSHCN and non-CSHCN (Bethell et al. 2012). However, data from these indices have not been reported on specifically among CSHCN + ASD relative to CSHCN-ASD and non-CSHCN.
Home, School, and Neighborhood Contextual Factors
Across the three indices reflective of factors influencing child and family health in the home, school, and neighborhood environments, 2007 NSCH results reveal that CSHCN + ASD are less likely than non-CSHCN to meet all age-relevant criteria (Table 2).
Specifically, CSHCN + ASD (15.4 %) were significantly less likely to meet the minimum criteria used to indicate a protective home environment compared to both CSHCN-ASD (22.1 %, P = .05) and non-CSHCN (27 %, P < .01). After adjusting for sociodemographic characteristics, the difference between CSHCN + ASD and non-CSHCN remained (AOR 0.48, [0.30–0.76]). CSHCN + ASD who were Black and non-Hispanic (AOR: 0.07, [0.01–0.61]) or who had public health insurance (AOR: 0.26, [0.10–0.67]) had lower adjusted odds of meeting all age-relevant protective home environment index criteria when compared to those who were White and non-Hispanic (NH) or who had private sector health insurance.
Approximately one in three school-age CSHCN + ASD (34.7 %) experienced each of the three factors included in the promoting school success index, representing a lower adjusted odds compared to non-CSHCN (AOR 0.28, [0.17–0.44]). CSHCN + ASD (34.7 %) were also significantly less likely to meet the factors promoting school success criteria relative to CSHCN-ASD (52.5 %, P <.01). Health insurance adequacy was associated with whether or not CSHCN + ASD met the factors for promoting school success criteria such that CSHCN + ASD with inadequate insurance were less likely to meet these criteria than those with adequate health insurance (AOR: 0.38, [0.19–0.76]), perhaps indicative of the important role health-care services can play to improve school attendance and success.
Likewise, relative to non-CSHCN, CSHCN + ASD had lower adjusted odds of meeting neighborhood safety and support criteria (AOR 0.67, [0.47–0.96]). Among CSHCN + ASD, those who did not meet neighborhood safety and support index criteria were more likely to lack care within a medical home than those who met neighborhood safety and support criteria (AOR: 2.46, [1.36–4.44]). A similar pattern of results was recently found among the broader population of US children by Aysola et al. (2011), reinforcing that pediatric health-care quality improvement may yield the furthest reaching benefits when synergistically and holistically driven throughout the health-care system including from the community level upward.
Health Services Needs and Utilization of Health-Care and Related Services
In addition to the substantial and potentially modifiable impact of ASD on children and their families, CSHCN + ASD generally experienced greater need and unmet need both for specific health services and equipment as well as family support services (Ahmedani and Hock 2012; Bitsko et al. 2009, Brachlow et al. 2007; Brown et al. 2011; Kogan et al. 2008; Mandell 2008; McGrath et al. 2009; Ming et al. 2011; Montes et al. 2009; Pringle et al. 2012; Shattuck et al. 2011). Table 3 summarizes the prevalence of specific health service needs, unmet needs, and utilization among CSHCN + ASD compared to CSHCN-ASD based on 2009–2010 NS-CSHCN results.
Specific Health Services Needs, Unmet Needs, and Utilization
The 2009–2010 NS-CSHCN primarily assesses child health service needs, unmet needs, and utilization related to 14 specific services and equipment (e.g., mental health care or counseling, home health-care services) as well as need and unmet need for three family support services (e.g., respite care, family mental health care, or counseling). Utilization of educational services is also included. Overall, CSHCN + ASD experienced greater need for specific health services, being more likely to need five or more of the specific services asked about (AOR: 2.73, [2.35–3.17]). Three in four (75.4 %) CSHCN + ASD needed physical, occupational, or speech therapy compared to only 20.3 % of CSHCN-ASD (AOR: 12.00, [10.34–13.93]). In comparison to CSHCN-ASD, those with ASD were also significantly more likely to need communication aids or devices (AOR: 9.97, [7.73–12.85]), home health-care services (AOR: 3.97, [2.93–5.37]), and mental health-care or counseling services (AOR: 3.42, [2.96–3.94]). Though so many CSHCN + ASD required specific health and support services, nearly 2 in 5 (38.2 %) had unmet needs for at least one of the 14 types of services assessed, representing a 2.41 greater adjusted odds when compared to CSHCN-ASD (95 % CI, 2.06–2.81).
Differences in service use and unmet need also extend to the families of CSHCN + ASD: approximately one-quarter (25.4 %) of CSHCN + ASD had families who needed respite care compared to 4.6 % of CSHCN-ASD (AOR: 7.02, [5.79–8.52]). Findings from recent research have demonstrated that children with ASD whose families receive needed respite care services may be less likely to utilize inpatient health care as a result of hospitalizations (Mandell et al. 2012). Similarly, CSHCN + ASD had 3.11 greater adjusted odds of having families who needed mental health or counseling services compared to CSHCN-ASD (95 % CI, 2.64–3.68). Despite this heightened level of need, CSHCN + ASD had 5.5 greater adjusted odds of experiencing unmet need for one or more of three specific family support services asked about in the 2009–2010 NS-CSHCN compared to CSHCN-ASD (95 % CI, 4.53–6.69).
Early Intervention and Special Education Utilization
Given that nearly all children with ASD have greater educational needs than other children, it is generally expected that they will be more likely to receive specialized education services. Furthermore, early intervention and special education services are federally mandated for all children with disabilities under the Individuals with Disabilities Education Act. Despite this, only 46.8 % of CSHCN + ASD received early intervention services prior to age three according to findings from the 2009–2010 NS-CSHCN. Although demand for early intervention services has increased along with the prevalence of ASD among US children, the requisite capacity specifically in terms of workforce may not exist to meet this need (Wise et al. 2010). Findings improve for school-age CSHCN + ASD such that 90.1 % had an Individualized Education Plan (IEP) to guide the provision of special education services. However, consistent with previous research (Pinborough-Zimmerman et al. 2012), only 80.6 % of CSHCN + ASD were reported to actually receive special education services. These findings imply that many CSHCN + ASD are not receiving the special education services they are entitled to.
US Health System Performance and Quality of Care for CSHCN + ASD
In order to place quality of care measurement into a national quality framework, this analysis summarizes the performance of CSHCN + ASD in the context of the MCHB System of Care Core Outcomes for CSHCN (US DHHS, HRSA, MCHB, 2008) (Table 4). These include shared decision-making between families and health-care providers, receipt of care within a medical home, health insurance coverage that was consistent and adequate over the past 12 months, whether or not preventive medical and dental care were received, access and barriers to health care, and health services for youth transition to adulthood. In addition, to provide an overall measure of health-care quality, receipt of care meeting the minimum quality of care index is provided.
MCHB Core Outcomes 1 and 2: Partners in Decision-Making and Medical Home
Relative to CSHCN-ASD, CSHCN + ASD had lower adjusted odds of having families who met criteria indicative of shared decision-making in their children’s health care, including having their child’s doctors discuss a range of health-care options, encourage parents to ask questions or raise concerns, and respect the parent’s treatment choices (AOR: 0.51, [0.44–0.59]).
The receipt of care within a medical home or as indicated by subcomponents comprising the medical home composite measure (e.g., care coordination, family-centered care) has frequently been used to assess pediatric health-care quality, particularly for CSHCN + ASD (Brachlow et al. 2007; Golnik et al. 2012; Kogan et al. 2008; Sheldrick and Perrin 2010). According to the 2009–2010 NS-CSHCN, less than half (45.3 %) of CSHCN-ASD received care within a medical home, and nearly half as many (23.6 %) CSHCN + ASD met criteria for receipt of care within a medical home (AOR: 0.35, [0.30–0.40]). In determining where the receipt of care within a medical home lags the most for CSHCN + ASD compared to those without ASD, it is important to consider the following five medical home subcomponents measured: (1) child has usual source(s) of sick and well care, (2) child has a personal doctor or nurse, (3) child experiences no problems obtaining needed referrals, (4) child receives family-centered care, and (5) child receives effective care coordination services when needed.
In looking at each of these subcomponents, CSHCN + ASD had 1.53 times greater adjusted odds of experiencing problems obtaining needed referrals in comparison to CSHCN-ASD (95 % CI, 1.22–1.92). Moreover, relative to CSHCN-ASD, those with ASD also had lower adjusted odds of receiving family-centered care (AOR: 0.45, [0.39–0.52]) as well as needed care coordination services (AOR: 0.39, [0.34–0.46]). Among CSHCN + ASD, those with inadequate health insurance were less likely than those with adequate insurance to have received family-centered care (AOR: 0.40, [0.31–0.52]) and needed care coordination services (AOR: 0.31, [0.23–0.42]). Together, these findings support previous research documenting the need for systemic improvements that support the delivery of care characteristic of the medical home concept for CSHCN + ASD (Carbone et al. 2009; Golnik et al. 2009).
MCHB Core Outcome 3: Health Insurance Quality
Consistent and adequate health insurance or lack thereof may serve to either help or hinder access to quality care. CSHCN + ASD had lower adjusted odds of being consistently and adequately insured (i.e., health insurance benefits met child’s needs, covered costs to a reasonable extent, and enabled child to visit needed providers) compared to CSHCN-ASD (AOR: 0.60, [0.52–0.69]). Among CSHCN + ASD, those with public health insurance had higher adjusted odds of being consistently and adequately insured relative to those with private insurance (AOR: 1.75, [1.18–2.58]). No significant differences were found to exist between CSHCN + ASD and CSHCN-ASD in terms of health insurance consistency. However, CSHCN + ASD were found to have lower adjusted odds of having adequate health insurance compared to CSHCN-ASD (AOR 0.57, [0.49–0.66]). The breadth and type of health services required by CSHCN + ASD in relationship to systemic shortcomings (e.g., lack of reimbursement, shortages in needed health services) may contribute to the heightened likelihood of health insurance inadequacy among CSHCN + ASD (Ahmedani and Hock 2012; Kauss et al. 2003; Thomas et al. 2012).
MCHB Core Outcome 4: Preventive Health Care to Enable Early and Continuous Screening
The receipt of routine preventive medical and dental care is imperative to enabling early and continuous screening of children for special health-care needs and/or developmental risks or problems. CSHCN + ASD generally had lower adjusted odds of having received recommended preventive medical and dental care compared to CSHCN-ASD (AOR: 0.81, [0.68–0.96]). Among CSHCN + ASD, those with household incomes below the Federal Poverty Level (FPL) (AOR: 0.50, [0.25–0.97]) or 100–199 % of the FPL (AOR: 0.47, [0.29–0.78]) were less likely to have received preventive care compared to CSHCN + ASD with household incomes of 400 % the FPL or higher. CSHCN + ASD also had lower adjusted odds of having received one or more preventive dental care visit during the past 12 months relative to CSHCN-ASD (AOR 0.70, [0.56–0.86]). Child behavior, care costs, and lack of insurance have been found to be barriers to the receipt of dental care services among CSHCN + ASD (Lai et al. 2012).
MCHB Core Outcome 5: Access and Barriers to Health Care
Accessing appropriate care may be difficult for CSHCN + ASD: 55.3 % of CSHCN + ASD experienced difficulties or delays receiving health services compared to 31.9 % of CSHCN-ASD (AOR: 2.79, [2.43–3.21]). CSHCN + ASD were specifically more likely than those without ASD to have experienced delays or difficulties accessing health services for the following reasons: lack of eligibility for services, lack of service availability in their geographic area, problems getting appointments, prohibitive costs, trouble obtaining information about needed services, or other reasons.
In light of their heightened level of unmet need for health-care services, it may be expected that CSHCN + ASD had lower adjusted odds of being able to easily access community-based services compared to CSHCN-ASD (AOR: 0.34, [0.30–0.39]). Among CSHCN + ASD, those with public health insurance (AOR: 0.58, [0.38–0.88]) and inadequate health insurance (AOR: 0.37, [0.27–0.50]) were less likely to easily access community-based services compared to their respective referent groups. Similarly, among CSHCN + ASD, those who lacked care within a medical home had lower adjusted odds of being able to easily access community-based services compared to those with a medical home (AOR: 0.24, [0.17–0.33]).
Further, CSHCN + ASD had 4.03 greater adjusted odds of having parents who experienced frustration getting their children needed health services compared to CSHCN-ASD (95 % CI, 3.34–4.85). Among CSHCN + ASD, those with inadequate health insurance (AOR: 2.35, [1.65–3.36]) or who did not receive care within a medical home (AOR: 5.95, [3.55–9.98]) had higher adjusted odds of having parents who experienced frustration accessing services for their children.
MCHB Core Outcome 6: Health Services for Transition to Adulthood
As CSHCN + ASD transition out of high school into adulthood, they are likely to disengage in health-care services (Shattuck et al. 2011). For this reason, it is especially important that CSHCN + ASD receive health-care services to support this transition. However, in comparison to other youth with special needs, CSHCN + ASD aged 12–17 years had lower adjusted odds of receiving needed health services for their transition to adulthood including anticipatory guidance and encouragement of self-management skills provided by their health-care providers (AOR: 0.35, [0.27–0.44]). While four in five (80.4 %) CSHCN-ASD had doctors who encouraged self-management skills, only 48.1 % of CSHCN + ASD received this type of care (AOR: 0.22, [0.18–0.28]). CSHCN + ASD were also less likely than CSHCN-ASD to have received anticipatory guidance from their health-care providers concerning the transition to adult health-care providers, how health-care needs may change with age, and health insurance coverage in adulthood. Among CSHCN + ASD, those with inadequate health insurance had lower adjusted odds of having received transition to adulthood health services compared to those with adequate insurance (AOR: 0.54, [0.33–0.86]). Additionally, CSHCN + ASD who did not receive care within a medical home had lower adjusted odds of receiving such services compared to those who received care in a medical home (AOR: 0.37, [0.23–0.60]).
Summary of MCHB Core Outcomes and Minimum Quality of Care for CSHCN with ASD
Across each of the MCHB System of Care Core Outcomes for CSHCN, those with ASD generally fared worse than others without ASD (Fig. 3). Using a conservatively defined system of care summary measure (i.e., meeting all or all but one of the age-relevant core outcomes), just over two in five (44.7 %) of CSHCN-ASD met this level of care, in contrast to less than half (22.7 %) of CSHCN + ASD (AOR: 0.32, [0.27–0.37]). In examining differences among subpopulations of CSHCN + ASD according to health insurance type, health insurance adequacy, and receipt of care within a medical home, potential areas for system improvement emerged in relationship to each of the core outcomes and certain outcome subcomponents most germane to the health and well-being of CSHCN + ASD.
System of care performance by core outcome among CSHCN+ASD and CSHCN–ASD from the 2009–2010 National Survey of Children with Special Health Care Needs (Measures were computed for CSHCN age 3–17 years, unless otherwise indicated. All odds ratios reported were adjusted for child’s age, sex, race/ethnicity, household income, primary household language, and US geographic region using logistic regression analysis unless otherwise specified. For all AORs, the referent group was CSHCN who were never told they have ASD. Primary household language was not included in the regression model due to sample size limitations)
The minimum quality of care index summarizes the percent of children who received at least one preventive medical visit per year, had adequate health insurance coverage, and received care in a medical home (Bethell et al. 2011). Using new data from the 2009–2010 NS-CSHCN, only 16 % of CSHCN + ASD experienced this minimum quality of care in the United States, approximately half the rate of CSHCN-ASD (31.5 %; AOR 0.39, [0.33–0.46]).
Conclusion
Key Terms
-
Adequate Health insurance. Private and/or public health insurance that usually provides benefits meeting the child’s health-care needs, covers health-care costs to a reasonable extent, and allows the child to visit needed providers.
-
Care coordination. Services encompassing the following components: (1) receipt of help perceived as needed to coordinate the child’s health care, (2) receipt of additional help to coordinate the child’s health care if needed, (3) satisfaction with communication among child’s doctor’s when needed, and (4) satisfaction with doctors’ communication to school or programs when needed.
-
Children with special health-care needs. Children whose ongoing physical, behavioral, or developmental condition(s) necessitate the use of health or related services of a type or amount above those required by children generally.
-
Family-centered care. Care including the following components: (1) doctors/other providers usually spend enough time with the child, (2) listen carefully to the child’s parent(s), (3) are sensitive to family customs and values, (4) provide information specific to the child’s health, and (5) help the family feel like a partner in care.
-
Medical home. Characterized according to the collective presence of the following health-care components: (1) usual source(s) of sick and well care, (2) personal doctor or nurse, (3) no problems obtaining needed referrals, (4) receipt of family-centered care, and (5) receipt of effective care coordination services.
-
Minimum health-care quality. Characterized by the presence of all of the following components: (1) receipt of one or more preventive medical care visit within the past 12 months, (2) adequate health insurance coverage, and (3) receipt of care within a medical home.
-
System of Care for CSHCN. Operationalized by the federal MCHB according to the following six, age-relevant core outcomes: (1) families are partners in decision-making, (2) children receive care within a medical home, (3) children have consistent and adequate health insurance coverage, (4) children are screened early and continuously for special health-care needs, (5) children’s families are able to easily access community-based services, and (6) youth receive health services for their transition to adulthood.
Key Facts
-
An estimated 1.1 % of US children aged 3–17 years have ASD.
-
Nearly all CSHCN + ASD (97.4 %) had complex health-care needs that required multiple types of specialized health-care services.
-
More than two-thirds (68.2 %) of US CSHCN + ASD had health conditions that affected their daily activities often or a great deal.
-
Over half (57.1 %) of US CSHCN + ASD had a family member who cut back and/or stopped working due to the child’s health condition.
-
Parents of CSHCN + ASD were more likely to experience stress from parenting compared to CSHCN-ASD.
-
Less than half of CSHCN + ASD received early intervention services before age 3.
-
Less than half (49.3 %) of CSHCN + ASD had consistent and adequate health insurance coverage.
-
CSHCN + ASD were significantly less likely than CSHCN-ASD to have received care within a medical home, particularly in terms of obtaining referrals, care coordination services, and family-centered care.
-
More than half of CSHCN + ASD did not have care meeting criteria for the MCHB’s 6 System of Care Core Outcomes for CSHCN.
-
Only 16 % of CSHCN + ASD met criteria indicative of minimum health-care quality.
Summary Points
-
CSHCN + ASD generally experience a greater burden of illness than CSHCN-ASD in terms of the complexity of health-care needs they have, multiplicity of conditions and functional difficulties, and effects their condition(s) have on their functional status.
-
Disparities in health-care quality exist between CSHCN + ASD and CSHCN-ASD across an array of measures.
-
Families of CSHCN + ASD are more greatly impacted than CSHCN-ASD with respect to their employment and finances.
-
Receipt of care within a medical home is associated with a reduced likelihood of certain child- and family-level impacts among CSHCN + ASD.
-
Lack of medical home and inadequate health insurance coverage further decrease the likelihood of receipt of quality health care among CSHCN + ASD.
-
Parents of CSHCN + ASD are more likely to experience stress and are less likely to experience excellent or good overall health status compared to CSHCN-ASD.
-
CSHCN + ASD are less likely than those without ASD to meet criteria indicative of protective home environment, factors promoting school success, and neighborhood safety and support.
-
Health-care disparities based on race/ethnicity, age, health insurance type, and household income levels exist among CSHCN + ASD.
-
Continuous monitoring of health care and related improvement efforts for CSHCN + ASD using standardized, population-based measures is imperative to meet federal legislative mandates and ultimately promote health-care equity among this underserved pediatric subpopulation.
References
Ahmedani BK, Hock RM. Health care access and treatment for children with co-morbid autism and psychiatric conditions. Soc Psychiatry Psychiatr Epidemiol. 2012;47(11):1807–14. doi:10.1007/s00127-012-0482-0.
Aysola J, Orav EJ, Ayanian JZ. Neighborhood characteristics associated with access to patient-centered medical homes for children. Health Aff. 2011;30(11):2080–9.
Baron-Cohen S, Scott FJ, Allison C, Williams J, Bolton P, et al. Prevalence of autism-spectrum conditions: UK school-based population study. Br J Psychiatry. 2009;194:500–9.
Begeer S, Bouk SE, Boussaid W, Terwogt MM, Koot HM. Underdiagnosis and referral bias of autism in ethnic minorities. J Autism Dev Disord. 2009;39:142–8.
Bethell CD, Read D, Stein RE, et al. Identifying children with special health care needs: development and evaluation of a short screening instrument. Ambul Pediatr. 2002;2(1):38–48.
Bethell CD, Read D, Blumberg SJ, Newacheck PW. What is the prevalence of children with special health care needs? Toward an understanding of variations in findings and methods across three national surveys. Matern Child Health J. 2008;12:1–14. doi:10.1007/s10995-007-0220-5.
Bethell CD, Kogan MD, Strickland BB, Schor EL, Robertson J, Newacheck PW. A national and state profile of leading health problems and health care quality for US children: key insurance disparities and across-state variations. Acad Pediatr. 2011;11:S22–33.
Bethell C, Forrest CB, Stumbo S, Gombojav N, Carle A, Irwin CE. Factors promoting or potentially impeding school success: disparities and state variations for children with special health care needs. Matern Child Health J. 2012;16 Suppl 1:S35–43. doi:10.1007/s10995-012-0093-z.
Bitsko RH, Visser SN, Schieve LA, Ross DS, Thurman DJ, Perou R. Unmet health care needs among CSHCN with neurologic conditions. Pediatrics. 2009;124 Suppl 4:S343–51.
Blumberg SJ, Foster EB, Frasier AM, et al. Design and operation of the national survey of children’s health, 2007. Hyattsville: National Center for Health Statistics; 2009.
Boulet SL, Boyle CA, Schieve LA. Health care use and health and functional impact of developmental disabilities among US children. Arch Pediatr Adolesc Med. 2009;163(1):19–26.
Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, Visser S, Kogan MD. Trends in the prevalence of developmental disabilities in US children 1997-2008. Pediatrics. 2011;127(6):1034–42.
Brachlow AE, Ness KK, McPheeters ML, Gurney JG. Comparison of indicators for a primary care medical home between children with autism or asthma and other special health care needs: national survey of children’s health. Arch Pediatr Adolesc Med. 2007;161(4):399–405.
Bramlett MD, Read D, Bethell C, Blumberg SJ. Differentiating subgroups of children with special health care needs by health status and complexity of health care needs. Matern Child Health J. 2009;13(2):151–63.
Brown HK, Ouellette-Kuntz H, Hunter D, Kelley E, Cobigo V, Lam M. Beyond an autism diagnosis: children’s functional independence and parents’ unmet needs. J Autism Dev Disord. 2011;41(10):1291–302.
Bryson SA, Corrigan SK, Mcdonald TP, Holmes C. Characteristics of children with autism spectrum disorders who received services through community mental health services. Autism. 2008;12(1):65–82.
Carbone PS, Behl DD, Azor V, Murphy NA. The medical home for children with autism spectrum disorders: parent and pediatrician perspectives. J Autism Dev Disord. 2009;40(3):317–24.
Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders – autism and developmental disabilities monitoring network, 14 sites, United States, 2008. MMWR Morb Mortal Wkly Rep. 2012;61(2203):1–19.
Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. 2009–2010 National Survey of Children with Special Health Care Needs Frequently Asked Questions. 2011. http://www.cdc.gov/nchs/slaits/cshcn.htm
Children’s Health Insurance Program Reauthorization Act of 2009, Pub L. no. 111-3 (2009). Print.
Cidav Z, Marcus SC, Mandell DS. Implications of childhood autism for parental employment and earnings. Pediatrics. 2012;129:617–23.
Combating Autism Reauthorization Act of 2011, Pub L. no. 112-32 (2011). Print.
Fine A, Kotelchuck M. Rethinking MCH: the life course model as an organizing framework. Prepared for the U.S. Department of Health and Human Services, Health Resources and Services Administration; 2010.
Forrest CV, Riley AW. Childhood origins of adult health: a basis for life-course health policy. Health Aff. 2004;23(5):155–64.
Golnik A, Ireland M, Borowsky IW. Medical homes for children with autism: a physician survey. Pediatrics. 2009;123(3):966–71.
Golnik A, Scal P, Wey A, Gaillard P. Autism-specific primary care medical home intervention. J Autism Dev Disord. 2012;42(6):1087–93. doi:10.1007/s10803-011-1351-5.
Gurney JG, McPheeters ML, Davis MM. Parental report of health conditions and health care use among children with and without autism. Arch Pediatr Adolesc Med. 2006;160:825.
Halfon J, Hochstein M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q. 2002;80:433–79.
Hertz-Picciotto I, Delwiche L. The rise in autism and the role of age at diagnosis. Epidemiology. 2009;20(1):84–90.
Hyman SL, Johnson JJ. Autism and pediatric practice: toward a medical home. J Autism Dev Disord. 2012;42(6):1156–64. doi:10.1007/s10803-012-1474-3.
Johnson CP, Myers SM. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120:1183–215.
Joshi G, Petty C, Wozniak J, Henin A, Fried R, et al. The heavy burden of psychiatric comorbidity in youth with autism spectrum disorders: a large comparative study of psychiatrically referred population. J Autism Dev Disord. 2010;40:1361–70.
Kalkbrenner AE, Daniels JL, Emch M, Morrissey J, Poole C, Chen JC. Geographic access to health services and diagnosis with an autism spectrum disorder. Ann Epidemiol. 2011;21(4):304–10.
Kauss MW, Gulley S, Sciegaj M, Wells N, Taylor SJ. Access to specialty medical care for children with mental retardation, autism, and other special health care needs. Ment Retard. 2003;41(5):329–39.
Kinney DK, Barch DH, Chayka B, Napolean S, Munir KM. Environmental risk factors for autism: do they help cause de novo genetic mutations that contribute to the disorder. Med Hypotheses. 2010;74(1):102–6.
Kogan MD, Strickland BB, Blumberg SJ, Singh GK, Perrin JM, van Dyck PC. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics. 2008;122(6):e1149–58.
Kogan MD, Blumberg SJ, Schieve LA, Boyle CA, Perrin JM, et al. Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US, 2007. Pediatrics. 2009;124(5):1395–403.
Kogan MD, Ghandour RM, Schempf AH. Introduction to the special issue of articles from the 2007 national survey of children’s health. Matern Child Health J. 2012;16 Suppl 1:S1–5. doi:10.1007/s10995-012-1007-x.
Kohane IS, McMurry A, Weber G, MacFadden D, Rappaport L, et al. The co-morbidity burden of children and young adults with autism spectrum disorders. PLoS One. 2012;7(4):e33224. doi:10.1371/journal.pone.0033224.
Krakowiak P, Walker CK, Bremmer AA, Baker AS, Ozonoff S, et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics. 2012;29(5):1121–8.
Lai B, Milano M, Roberts MW, Hooper SR. Unmet dental needs and barriers to dental care among children with autism spectrum disorders. J Autism Dev Disord. 2012;42(7):1294–303. doi:10.1007/s10803-0111-1362-2.
Leslie DL, Martin A. Health care expenditures associated with autism spectrum disorders. Arch Pediatr Adolesc Med. 2007;161:350–5.
Levy SE, Hyman SL. Complementary and alternative medicine treatments for children with autism spectrum disorders. Child Adolesc Psychiatr Clin N Am. 2008;17(4):803–20.
Liptak GS, Benzoni LB, Mruzek DW, et al. Disparities in diagnosis and access to health services for children with autism: data from the national survey of children’s health. J Dev Behav Pediatr. 2008;29(3):152–60.
Mandell DS. Psychiatric hospitalization among children with autism spectrum disorders. J Autism Dev Disord. 2008;38(6):1059–65.
Mandell DS, Wiggins LD, Carpenter LA, Daniels J, DiGuiseppi C, et al. Racial/ethnic disparities in the identification of children with autism spectrum disorders. Am J Public Health. 2009;99(3):493–8.
Mandell DS, Xie M, Morales KH, Lawer L, McCarthy M, et al. The interplay of outpatient services and psychiatric hospitalization among Medicaid-enrolled children with autism spectrum disorders. Arch Pediatr Adolesc Med. 2012;166(1):68–73.
McGrath RJ, Laflamme DJ, Schwartz AP, Stransky M, Moeschler JB. Access to genetic counseling for children with autism, down syndrome, and intellectual disabilities. Pediatrics. 2009;124 Suppl 4:S443–9.
McPherson M, Arango P, Fox H, et al. A new definition of children with special health care needs. Pediatrics. 1998;102:137–40.
Ming X, Hashim A, Fleishman S, et al. Access to specialty care in autism spectrum disorders-a pilot study of referral source. BMC Health Serv Res. 2011;11:99.
Montes G, Halterman JS. White-black disparities in family-centered care among children with autism in the United States: evidence from the NS-CSHCN 2005–2006. Acad Pediatr. 2011;11(4):297–304.
Montes G, Halterman JS, Magyar CI. Access to and satisfaction with school and community health services for US children with ASD. Pediatrics. 2009;124 Suppl 4:S407–13.
Narendorf SC, Shattuck PT, Sterzing PR. Mental health service use among adolescents with an autism spectrum disorder. Psychiatr Serv. 2011;62(8):975–8.
National Data Resource Center for Child and Adolescent Health. National Survey of Children with Special Health Care Needs. http://www.childhealthdata.org. Accessed 8 June 2012.
National Data Resource Center for Child and Adolescent Health. National Survey of Children’s Health. http://www.childhealthdata.org. Accessed 8 June 2012.
Patient Protection and Affordable Care Act of 2010, Pub L. no. 111-148 Stat 110 (2010). Print.
Perrin JM. How can quality improvement enhance the lives of children with disabilities? Future Child. 2012;22(1):149–68.
Pinborough-Zimmerman J, Bakian AV, Fombonne E, Bilder D, Taylor J, et al. Changes in the administrative prevalence of autism spectrum disorders: contribution of special and health from 2002–2008. J Autism Dev Disord. 2012;42:521–30.
Pringle B, Colpe LJ, Blumberg SJ, Avila RM, & Kogan MD. Diagnostic history and treatment of school-aged children with autism spectrum disorder and special health care needs. NCHS data brief, no 97. Hyattsville: National Center for Health Statistics; 2012.
Ratajczak HV. Theoretical aspects of autism: causes – a review. J Immunotoxicol. 2011;8(1):68–79.
Rice CE. The changing prevalence of the autism spectrum disorders. Am Fam Physician. 2011;83(5):515–20.
Schieve LA, Boulet SL, Kogan MD, Yeargin-Allsopp M, Boyle CA, et al. Parenting aggravation and autism spectrum disorders: 2007 national survey of children’s health. Disabil Health J. 2011;4:143–52. doi:10.1016/j.dhjo.2010.09.002.
Schmidt LJ, Garratt AM, Fitzpatrick R. Child/parent-assessed population health outcome measures: a structured review. Child Care Health Dev. 2002;28:227–37. doi:10.1046/j.1365-2214.2002.00266.x.
Shaikh U, Nettiksimmons J, Bell RA, Tancredi D, Romano PS. Documentation as measures of diet and physical activity counseling. Acad Pediatr. 2012;12(2):81–7.
Shattuck PT, Wagner M, Narendorf S, Sterzing P, Hensley M. Post high school service use among young adults with autism spectrum disorder. Arch Pediatr Adolesc Med. 2011;165(2):141–6.
Sheldrick RC, Perrin EC. Medical home services for children with behavioral conditions. J Dev Behav Pediatr. 2010;31:92–9.
Shelton JF, Tancredi DJ, Hertz-Picciotto I. Independent and dependent contributions of advanced maternal and paternal ages to autism risk. Autism Res. 2010;3:30–9.
Shieve LA, Rice C, Yeargin-Allsopp M, Boyle CA, Kogan MD, et al. Parent-reported prevalence of autism spectrum disorders in US-born children: an assessment of changes within birth cohorts from the 2003 to the 2007 national survey of children’s health. Matern Child Health J. 2012;16 Suppl 1:S151–7.
Simon AE, Chan KS, Forrest CB. Assessment of children’s health-related quality of life in the United States with a multidimensional index. Pediatrics. 2008;21:e118.
Simonoff E, Pickels A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47:921–9.
Thomas KC, Parish SL, Rose RA, Kilany M. Access to care for children with autism in the context of state medicaid reimbursement. Matern Child Health J. 2012;16(8):1636–44.
US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. The national survey of children with special health care needs Chartbook 2005–2006. Rockville: US Department of Health and Human Services; 2008.
US Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. Children with special health care needs in context: a portrait of States and the Nation 2007. Rockville: US Department of Health and Human Services; 2011.
Victorino CC, Gauthier AH. The social determinants of child health: variations across health outcomes – a population-based cross-sectional analysis. BMC Pediatr. 2009;9:53.
Wise MD, Little AA, Holliman JB, Wise PH, Wang CJ. Can state early intervention programs meet increased demand of children suspected of having autism spectrum disorders. J Dev Behav Pediatr. 2010;31(6):469–76.
Acknowledgments
The authors would like to thank Richard LeDonne and Julie Robertson, MPH, and other members of the Child and Adolescent Health Measurement Initiative team, for their assistance in the preparation of the references and the data tables and graphs for this chapter.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Technical Methods Appendix
Technical Methods Appendix
Data were drawn from the 2009–2010 NS-CSHCN and 2007 NSCH public use data files prepared by the Child and Adolescent Health Measurement Initiative through the Data Resource Center for Child and Adolescent Health (National Data Resource Center for Child and Adolescent Health 2012a, b). Both surveys are led and funded by the federal MCHB and administered by the National Center for Health Statistics’ (NCHS) State and Local Area Integrated Telephone Survey Program, using the National Immunization Survey sampling frame. Both surveys’ methods have been previously described (Blumberg et al. 2009; CDC 2011). Random-digit dial telephone interview methods were employed to identify households and children under the age of 18 years. Respondents were a parent or other adult in the household who knew about the child’s health and health care. Interviews were conducted in English, Spanish, and four Asian languages. In both surveys, the five-item CSHCN Screener was used to identify CSHCN based on consequences children with ongoing conditions are expected to experience (Bethell et al. 2002). Both surveys additionally used the following three items to determine ASD status and severity:
-
1.
Has a doctor or other health-care provider ever told you that [your child] had autism, Asperger’s disorder, pervasive developmental disorder, or other autism spectrum disorder – ASD?
-
2.
Does [your child] currently have autism or ASD?
-
3.
Would you describe his/her autism or ASD as mild, moderate, or severe?
Data analyses were limited to the 37,826 CSHCN aged 3–17 years who were sampled in the 2009–2010 NS-CSHCN and the 78,037 children aged 3–17 years from the 2007 NSCH. Estimates from each survey were adjusted by NCHS for nonresponse bias and weighted to represent the noninstitutionalized population of children aged 3–17 years in each state and the District of Columbia, resulting in an estimated 61.6 million US children based on the 2007 NSCH and an estimated 10.2 million US CSHCN based on the 2009–2010 NS-CSHCN. Slight differences in NS-CSHCN and NSCH methods may contribute to discrepancies in CSHCN prevalence estimates as well as the complexity of health and service needs represented among the pediatric populations sampled (Bethell et al. 2008). Missing data on household income, race, ethnicity/language, and highest level of education achieved by parent in the household were imputed by NCHS using multiple-imputation methods (Blumberg et al. 2009; CDC 2011).
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this entry
Cite this entry
Bethell, C.D., Lindly, O., Kogan, M., Zuckerman, K. (2014). Health Care Quality for Children: The Position of Autism Spectrum Disorder. In: Patel, V., Preedy, V., Martin, C. (eds) Comprehensive Guide to Autism. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4788-7_3
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4788-7_3
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4787-0
Online ISBN: 978-1-4614-4788-7
eBook Packages: Behavioral ScienceReference Module Humanities and Social SciencesReference Module Business, Economics and Social Sciences