Abstract
The development of metastasis is the major cause of death in cancer patients. In certain instances, this occurs shortly after primary tumor detection and treatment, indicating these lesions were already expanding at the moment of diagnosis or initiated exponential growth shortly after. However, in many types of cancer, patients succumb to metastatic disease years and sometimes decades after being treated for a primary tumor. This has led to the notion that in these patients residual disease may remain in a dormant state. Tumor cell dormancy is a poorly understood phase of cancer progression and only recently have its underlying molecular mechanisms started to be revealed. Important questions that remain to be elucidated include not only which mechanisms prevent residual disease from proliferating but also which mechanisms critically maintain the long-term survival of these disseminated residual cells. Herein, we review recent evidence in support of genetic and epigenetic mechanisms driving dormancy. We also explore how therapy may cause the onset of dormancy in the surviving fraction of cells after treatment and how autophagy may be a mechanism that maintains the residual cells that are viable for prolonged periods.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Metastasis is responsible for the majority of cancer-related deaths. However, our understanding of this complex process is incomplete, which limits our opportunities to prevent metastatic development. There are several fundamental questions that remain mostly unanswered in this field: How does early dissemination contribute to a dormant cell population and what are the underlying mechanisms? How does the tumor microenvironment aid this process? Are primary tumor niches responsible for programming disseminated tumor cells (DTCs) to grow or enter quiescence in target organs? What role does the microenvironment of the target organ play in determining the timing or extent of DTC dormancy?
The “seed and soil” theory of metastasis proposes that a natural match exists between the DTCs (the seeds) and the target organ (the soil) in which they can grow into overt lesions [1]. This theory is derived from the relatively predictable pattern of target organ metastasis that depends on the tissue origin of the primary tumor. However, it remains difficult to predict the timing of metastasis because, even in those sites propitious for growth, it can take years to decades for metastases to develop [1]. Indeed, certain cancers, such as breast carcinoma and melanoma, are well known for their propensity to relapse after a long disease-free period, often decades after initial diagnosis and treatment of the primary tumor. Moreover, it has been proposed that these long periods of asymptomatic disease are due to minimal residual disease (MRD), because DTCs enter a nonproductive or dormant state [1, 2].
In cancer patients, DTCs can be found in sites where they typically form secondary lesions, as well as in sites where they rarely do [1]. Thus, despite being able to disseminate, these DTCs are presumably “growth-suppressed” by the microenvironments of certain organs. Insights into these mechanisms should lead to the identification of novel biomarkers that indicate whether patients harbor dormant disease, and should uncover new signaling pathways that can be modulated to either maintain the dormancy of DTCs or eliminate them entirely by blocking critical survival pathways.
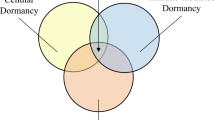
To date, several mechanisms have been proposed to explain clinical dormancy (i.e., asymptomatic disease) in cancers. The lack of proliferation markers in surviving DTCs obtained from patients and findings from experimental studies suggest that solitary DTC dormancy may be controlled by mechanisms of quiescence [1], a reversible growth arrest that can be induced by different signals [3]. Angiogenic dormancy or immune system-mediated tumor mass dormancy may also be responsible for maintaining the dormancy of residual disease [4, 5] (see Almog and Quesnel chapters in this book).
The primary tumor and target organ microenvironments are intimately interconnected by the biology of DTCs (Fig. 5.1). Three potential scenarios that relate to this concept may explain DTC dormancy. First, DTCs from invasive cancers activate stress signals in response to the dissemination process and/or due to a growth-suppressive microenvironment of the target organ (see “The Target Organ Microenvironment and DTC Dormancy” section for examples of such microenvironments and their components), ultimately leading to induction of dormancy [1]. Second, therapy and/or microenvironmental stress conditions (e.g., hypoxia, reactive oxygen species) acting on tumor cells in the primary lesion endow these tumor cells with specific gene expression signatures that prime newly formed DTCs to enter dormancy. Here, specific primary tumor “stress microenvironments” may influence the DTCs to enter long-term dormancy when the cells initially arrive at secondary sites. Third, lesions that are pathologically defined as noninvasive carry a subpopulation of cells that possess the ability to undergo micro-invasion and disseminate. Although these DTCs are able to intravasate into and extravasate out of the systemic circulation, they remain unfit for expansion in secondary sites. Nonetheless, they can survive in an arrested state over an extended period and perhaps undergo occasional cell divisions, progressing via epigenetic and genetic pathways to eventually become a fully metastatic cell able to grow at the secondary sites. In this chapter, we focus both on how solitary DTC fate is influenced by tumor–host interactions occurring in primary tumors and target organs, and on how autophagy may serve as a cell-autonomous survival function in residual disease (Fig. 5.2). We propose that DTCs undergo dormancy to survive specific stressful microenvironments (see section “The Target Organ Microenvironment and DTC Dormancy”) and, therefore, that blockade of the survival signals in dormant cells will ultimately lead to their eradication.
Upon arrival at secondary sites, the crosstalk between the DTCs and the new microenvironment will determine the fate of the DTCs: In a permissive microenvironment (right), such as the lungs, interactions with the extracellular matrix (ECM), and stromal cells of the favorable microenvironment will allow DTCs to adapt and integrate growth-promoting signals, such as those derived from fibronectin, which will result in activation of mitogenic signaling (high ERK/low p38 ratio), thereby promoting DTC proliferation and the formation of micrometastasis. On the contrary, in restrictive microenvironments (left) such as bone marrow or liver for some cancers, either the loss of surface receptors or the interaction with non-growth-permissive ligands will result in activation of stress signaling (low ERK/high p38 ratio) that will induce both quiescence and survival signals, which will in turn lead to a prolonged phase of dormancy. Activation of p38 induces a G0–G1 arrest that is partly mediated by transcriptional activation of BHLHB3, NR2F1, and p53, which control the expression of different regulators of the cell cycle, such as p21, p27, p15, and p18, which mediate tumor cell growth arrest. Furthermore, active p38α induces an ER-stress response that coordinates growth arrest and survival through the activation of PERK, IRE-1, and ATF6. PERK contributes to both quiescence and survival of DTCs. Upon activation, PERK induces phosphorylation of EIF2α and attenuation of translation initiation, which leads to downregulation of cyclin D1/D3 and CDK4 and to the induction of quiescence. On the other hand, the other arms of the ER-stress pathways, ATF6α and IRE1α, contribute to DTC dormancy by promoting survival. IRE1α activation leads to the induction of XBP and the activation of the transcription of survival genes, whereas activation of ATF6α induces survival through the upregulation of Rheb and activation of mTOR signaling, allowing DTCs to adapt to the in vivo microenvironment. In addition to this, as part of the ER-stress response, the chaperone BiP/Grp78 is also activated, and this leads to inhibition of Bax activation to prevent apoptosis and thus, promote survival and drug resistance
Activation of autophagy in response to different forms of stress can promote survival during growth arrest, making autophagy a component of dormant tumor cell survival. Autophagy is a stress-response mechanism that can be activated in response to various microenvironmental stresses such as hypoxia, extracellular matrix (ECM) detachment, endoplasmic reticulum (ER) stress, growth factor withdrawal, metabolic stress, activation of tumor suppressor genes (aplasia Ras homolog member I [ARHI]), or therapy-induced stress (Gleevec). Once activated, autophagy can mediate cell survival through different mechanisms that usually involve the activation of ATG genes, although it can also inhibit TRAIL-mediated apoptosis, for example. Some evidence exists that autophagy might contribute to tumor dormancy through the induction of tumor cell survival; for example, in ovarian carcinoma, ARHI-induced autophagy was shown to contribute to cell survival and tumor dormancy through restoration of PI3K signaling. Furthermore, in gastrointestinal stromal tumors (GIST), autophagy is induced in response to Gleevec, which leads to the induction of a dormant state in which these tumor cells can survive for extremely prolonged periods. Because autophagy can protect cells from different microenvironmental induced stresses, one can speculate that autophagy might be one of the mechanisms activated to promote the survival of dormant disseminated tumor cells in restrictive microenvironments
Early Dissemination as a Contributing Factor to Dormancy and MRD
The present paradigm proposes that metastases arise from rare clones that evolve in the primary tumor and acquire characteristics that allow them to disseminate and grow in secondary sites [6, 7]. This somewhat linear model motivates the prediction that tumor cells will emerge with metastatic capacity only if they are derived from evolutionarily “late-progressed” tumors (i.e., those with multiple malignancy-associated genetic alterations). It also suggests that tumor cells endowed with metastatic capacity should be absent or infrequent in patients carrying premalignant/invasive lesions (with fewer genetic alterations, see below) [6, 7]. However, a major challenge to this theory was posed by a series of studies in breast cancer from the Klein lab, which suggested that dissemination had already occurred in lesions that were considered to develop “early” in tumor progression and were pathologically defined as noninvasive, such as atypical ductal hyperplasia (ADH) and ductal carcinoma in situ (DCIS) [6, 8–11]. These studies also indicated that the pause observed in the progression of early DTCs may be due to a “lead time” [6, 8–11]. This refers to the time when DTCs with a limited number of genetic alterations are able to survive, but are unable to efficiently proliferate to gain additional mutations that would favor growth ectopically. This is supported by the fact that genetic alterations in DTCs detected in patients with ADH or DCIS are very heterogeneous [12]. In contrast, genetic anomalies in DTCs from patients carrying diagnosed metastatic disease are significantly more homogeneous, suggesting that certain genetic traits are selected for active expansion in the secondary site and that the original heterogeneity in DTCs is reduced [6, 8–12].
Modeling of tumor cell dissemination during early stages of cancer progression in MMTV-Neu (Neu) mice showed that premalignant lesions contained micro-invasive cells and that dissemination to lungs and bone marrow (BM) was readily detected [9]. In uveal melanoma, a cancer with 50% incidence of late liver recurrence (>10 years) in humans [13], analysis of tumor doubling times led to the conclusion that dissemination had occurred at least half a decade before diagnosis. In an uveal melanoma mouse model [14], it was shown that dissemination occurred early and dormant (i.e., growth-arrested) DTCs were commonplace. In a Drosophila melanogaster model using CSK (C-terminal Src kinase)-null flies, early dissemination required Src activation without loss of E-cadherin or obvious induction of an epithelial-mesenchymal transition, which is supposedly a prerequisite for dissemination [15].
It is possible that early dissemination accounts for the variable periods of dormancy time because early DTCs are genetically and/or epigenetically unfit for expansion. Alternatively, DTCs carrying genetic alterations that favor growth or those originating from more progressed lesions may be kept “in-check” by the microenvironment, whereby epigenetic or therapy-derived mechanisms [1] contribute to tumor cell dormancy during or after the “lead time” [1, 16]. In support of the microenvironment playing a role, a recent report suggested that breast cancer patients with cells disseminated to the BM had longer disease-free periods than patients who were negative for cells in this site [17]. This suggests that the bone microenvironment may change the timing of cancer progression by favoring dormancy. Nonetheless, it remains unclear how the primary tumor or the target organ microenvironments may control the lead time in solitary DTCs, and the kinetics driving genetic progression during this lead time remain poorly understood.
The possibility of therapy-induced quiescence may follow different mechanisms. In multiple myeloma, treatment with a proteasome inhibitor (bortezomib) has been found to induce post treatment protracted quiescence and survival of a fraction of cancer cells [18]. Furthermore, it has been shown that BCR-ABL blasts detected by fluorescence in situ hybridization (FISH) in chronic myelogenous leukemia patients who had responded to interferon-γ treatment 5–10 years earlier had no detectable mRNA for the oncogene [19, 20]. This suggests that epigenetic or post-transcriptional mechanisms may be dominant and suppress gene expression, including even those genes that are mutated or amplified. This potentially explains why, despite the presence of genetic alterations, these cells remain at a residual level. This dormancy may be explained by mechanisms similar to those controlling hematopoietic stem cell dormancy, whereby inactive STAT1 and Akt1 as well as low Sca-1 levels apparently maintain dormancy of these cells. In fact, it has been proposed that treatment with interferon-α may break the dormancy of leukemic stem cells by activating (activity and expression) the above-mentioned molecules, and that these cells are now prone to being targeted by BCR-ABL inhibitors [21]. This also suggests that, while chemotherapeutic drugs or other treatments kill a large fraction of cells, they can also cause induction of a residual dormant cell population that may subsequently be poised for recurrence (see below).
The Target Organ Microenvironment and DTC Dormancy
Solitary DTCs in target organs can establish interactions with the extracellular matrix (ECM), immune cells, and vasculature [22]. Studies using breast cancer cell lines selected for vigorous growth in target organs identified gene expression profiles that favored organ-specific colonization [23]. On the contrary, some genes including the metastasis suppressor gene (MSG) MKK4, via p38, can suppress metastases [24], and this seems to depend on stress signals from the microenvironment (see Fig. 5.1) [25]. MKK4 belongs to a family of genes that selectively blocks metastatic growth, and includes KISS1, MKK6, BHLHLB3/Sharp-1 (another p38-induced gene [26]), and Nm23-H1, among others [25, 27]. Because these genes suppress the growth and expansion of DTCs at target organs, yet fail to impede primary tumor growth, this further supports that the target organs with specific tissue microenvironments are required for these molecules to exert their growth-suppressing functions.
In squamous carcinoma cells (HEp3), reduced expression of urokinase (uPA) receptor (uPAR) deactivates α5β1 integrins, which makes these cells incapable of binding efficiently to fibronectin [28]. This results in reduced focal adhesion kinase (FAK) and epidermal growth factor receptor signaling, as well as in p38 activation. Thus, a failure by tumor cells to establish appropriate interactions with the ECM may induce growth-restrictive signals that fuel a quiescence state [1]. Furthermore, the loss of β1 integrin or FAK signaling in breast cancer models can induce dormancy, and activation of the Src-MLKC pathway can prevent dormancy [1, 29]. In addition, a fibrous collagen-I-enriched microenvironment in lungs can trigger intravenously injected mouse breast cancer cells to exit dormancy [29]. In contrast, microenvironments rich in fibrillar collagen-I induce melanoma quiescence by activating the discoidin domain receptor 2 and p15INK4b induction [13]. Collectively, these studies demonstrate that the loss of growth pathways induced by either therapies or a restrictive (i.e., fibrotic or non-fibrotic target tissues depending on the tumor type) tissue microenvironment is accompanied by the activation of stress pathways; this immediately motivates the hypothesis that the integration of these two types of signals within a DTC is responsible for both entry into and exit from a dormant state (see Fig. 5.1).
In HEp3 squamous carcinoma cells, while the activation of p38α/β inhibits ERK1/2 signaling, it also activates a stress-adaptive response known as the unfolded protein response (UPR) [26, 30, 31]. These signals lead to an epigenetic reprogramming and induction of survival and quiescence of dormant HEp3 (D-HEp3) cells [32]. D-HEp3 cells inoculated in vivo enter a deep G0–G1 arrest characterized by induction of p21, p27, p18, and p15 [26]. At least three transcription factors (TFs), p53, BHLHB3/41/Sharp1 and NR2F1, are regulated by p38α/β and required for dormancy of tumor cells in vivo [26]. This program is activated in dormant DTCs recovered from the bone marrow (BM) but is reversed when tumor cells exit dormancy or grow persistently in lungs (our unpublished results) (see Fig. 5.1). BM-derived dormant HEp3 cells display a low ERK/p38 signaling ratio and induction of BHLHB3/41/Sharp-1, NR2F1, and p53. Interestingly, MSGs, such as MKK4 and MKK6, are upstream activators of p38 [25], whereas BHLHB3 is a target of p38 required for quiescence induction [26]. Thus, it seems that different mechanisms converge in the regulation of the ERK/p38 signaling ratio and result in induction of either proliferation or dormancy.
An important question is whether the target organ microenvironment, where DTCs reside, induces dormancy programs, and if so, how? In tumors like those in head and neck squamous cell carcinoma and breast cancer, bone metastasis occurs at a frequency of 10–30% [7, 33, 34]. However, the detection of BM DTCs is much higher (>50% of patients) [6, 35]. This suggests that not all DTCs ultimately form overt metastasis and/or that a delay takes place. In mouse models of cancer (xenografts or transgenic), BM metastases are rarely observed. For example, in MMTV-Neu transgenic mice, BM DTCs are readily detected but mice never develop bone metastasis [9]. However, if the BM microenvironment is modified via irradiation [9] or if p38α/β is systemically inhibited, then DTCs expand ([9] and our unpublished data). Thus, in certain organs, restrictive signals mediated at least by p38α/β signaling can prevent occult DTCs from expanding.
In the search for signaling mediators that play a role in dormancy of DTCs in the BM, transforming growth factor-beta (TGFβ), a cytokine rich in the BM microenvironment [36–39], has emerged as a potential factor. Although tumors have been shown to depend on TGFβ to metastasize [40, 41], this ligand, depending on the degree of progression of tumors, can also be a potent inhibitor of epithelial tumor cell proliferation [42, 43]. TGFβ is also required to maintain the quiescence of stem cells and progenitors in the BM [36–39]. Thus, some tumors may remain sensitive to TGFβ growth inhibition in microenvironments where this factor is present (i.e., BM) [44]. In early-stage melanoma, TGFβ is anti-proliferative, thus functioning as a tumor-suppressor, but in advanced melanoma it is pro-invasive [45–47]. How these two opposing scenarios develop is not entirely clear [45, 48]. Furthermore, there is clinical evidence of early spread of uveal melanoma and, in a smaller proportion of patients, cutaneous melanoma thinner than 0.76 mm in depth [49–51]. It is possible that, similar to early dissemination in breast cancer [10], melanoma may spread before the conversion from TGFβ-inhibitory phenotype to pro-invasive behavior is activated, and when single cells arrive at distant sites, such as the liver or BM [9], they may remain in cell cycle arrest for prolonged periods due to high levels of and/or high responsiveness to TGFβ.
ER-Stress Signaling Pathways Contribute to Growth Arrest and Survival Programs During Tumor Cell Dormancy
While exploring the mechanisms that drive quiescence and survival of dormant HEp3 cells, the Aguirre-Ghiso lab discovered that HEp3 cells display a high ERK1/2 to p38α/β signaling ratio that favors proliferation in vivo [52–54]. The reprogramming of cells into dormancy (D-HEp3 cells) results in a reversion of this ratio, and now p38 signaling predominates over ERK. In addition, p38 appears to activate a negative feedback loop [28, 55, 56]. Using proteomics and microarray studies, the same group revealed that D-HEp3 cells develop an UPR characterized by enhanced endoplasmic reticulum (ER) signaling (see Fig. 5.1). In fact, all three arms of the UPR—ATF6α, IRE1α, and PERK—are activated in these cells [30, 31, 57, 58]. These studies led to the discovery that, in addition to inducing growth arrest, dormant cells utilized these signals to robustly withstand stress insults and survive in vivo for months. Among the three ER transmembrane signaling molecules, only PERK was found to contribute to the quiescence of D-HEp3 cells [30, 31, 57, 58]. It did so by attenuating translation initiation, which resulted in the downregulation of cyclin D1/D3 and CDK4 in these cells [30]. In fact, inducible activation of PERK signaling using a dimerizable Fv2E-PERK fusion protein and the divalent ligand AP20187 was sufficient to fully abrogate tumorigenicity and induce growth arrest, in some cases irreversibly [30]. PERK also contributes survival signals for D-HEp3 cells. In fact, inhibition of PERK made these cells susceptible to both glucose deprivation and chemotherapeutic drug-induced killing (see Fig. 5.1) [30, 31].
The other arms of the ER-stress pathways, ATF6α and IRE1α, were also found to regulate tumor cell dormancy by promoting survival and adaptation to the in vivo microenvironment [57]. RNA interference (RNAi)-mediated targeting of ATF6α caused a decrease in the number of viable D-HEp3 cells in vivo without interrupting their dormancy [57]. RNAi targeting of XBP-1, a transcription factor (TF) that is exclusively activated by IRE1α through noncanonical splicing, also induced dormant D-HEp3 cell killing [57] (and unpublished results). Neither RNAi to ATF6α or XBP-1 affected the tumorigenicity of T-HEp3 cells. Thus, the survival capacity of these genes seems to operate primarily in the cells that enter quiescence and not in the proliferative counterpart (see Fig. 5.1).
The mechanism of survival for ATF6α has also been explored in more detail. It has been shown the basal survival capacity of D-HEp3 cells to adapt and enter dormancy in vivo is not mediated by classical target genes regulated by ATF6α during the UPR, including genes for the chaperone BiP/Grp78, secretogranin II, and a glucose transporter [57]. We found that ATF6α induced Rheb, a small GTPase of the Ras family that directly activates the survival protein mTOR. Indeed, analysis of the mechanisms revealed that p38-dependent activation of ATF6α results in Rheb induction and stronger activation of mTOR → P-S6K → P-S6 signaling [57]. This pathway confers only dormant cells with resistance to rapamycin, as RNAi targeting of Rheb or ATF6 restored sensitivity to the mTOR inhibitor. Most importantly, dormant D-HEp3 cells can no longer adapt to the in vivo microenvironment and die at least in part through a caspase-3–dependent apoptotic pathway (see Fig. 5.1) [57].
Moreover, p38 also induced the expression of the chaperone BiP/Grp78 (see Fig. 5.1). This chaperone is induced during ER-stress and is an essential survival factor as it is a primary regulator of protein folding in the ER lumen. Numerous studies have shown that BiP serves as a survival factor not only in response to ER-stress but also to other damaging agents, such as chemotherapeutic drugs [31]. The upregulation of BiP in dormant HEp3 cells and its induction by p38 suggests that p38 signaling, like ATF6 activation, could tap into BiP function to provide survival signals [31]. However, as mentioned above, BiP did not provide a survival advantage for basal in vivo adaptation [57], which raises the possibility that BiP may only protect dormant cells under extreme damaging conditions such as those encountered during chemotherapy [31]. In fact, it has been demonstrated that dormant D-HEp3 cells were inherently resistant to chemotherapy compared with their tumorigenic counterpart, and that this was not due to enhanced expression of ATP-binding cassette transporters [31]. Furthermore, RNAi targeting of BiP greatly sensitized dormant D-HEp3 cells to etoposide and doxorubicin treatment. In contrast, the lower levels of BiP in the T-HEp3 cells, when further decreased by RNAi, had no effect on the sensitivity of these cells to chemotherapy. Analysis of the mechanism revealed that BiP inhibited the activation of the pro-apoptotic factor Bax [31]. Recent follow-up on our studies by other investigators revealed that in fact BiP inhibits Bax by regulating its inhibitor Bik (see Fig. 5.1) [59].
These studies highlight a mostly overlooked aspect of dormancy: cells, from either early primary lesions or more advanced tumors, must survive for prolonged periods before resuming growth. Our results suggest that there may be mechanisms that selectively protect quiescent cells from a hostile microenvironment or from stress imposed by the therapies used to treat different cancers. This may be an evolutionary conserved response to stress. For example, organisms like Caenorhabditis elegans are able to pause development and enter a dormant dauer stage in response to nutritional stress or oxidative stress derived from the environment [1, 60–62]. Numerous studies in yeast also suggest that stress signaling and induction of quiescent growth are coupled with the induction of survival pathways that protect the organism from stress conditions during growth arrest [63]. This prompts the question of whether these mechanisms are active in DTCs in patients and whether they can be exploited therapeutically.
Autophagy and Survival of Residual Disease
With increasing scrutiny on how fundamental cellular stress-response pathways impact survival and expansion of dormant tumor cells, autophagy has emerged as an attractive target against dormant tumor cells (see Fig. 5.2). Importantly, multiple routes of autophagic degradation exist within cells, including: (1) macroautophagy, in which cytoplasmic contents are sequestered in double membrane autophagosomes and subsequently delivered to the lysosome; (2) microautophagy, where cytoplasm is directly engulfed by the lysosomal membrane; and (3) chaperone-mediated autophagy, where proteins with a specific signal sequence are transported to the lysosomal lumen by a receptor-mediated process [64]. Of these routes, macroautophagy (hereafter called autophagy) has been most extensively studied for its potential functions in cancer. Macroautophagy is tightly regulated by a limited number of highly conserved genes called ATGs (AuTophaGy-related genes), which were originally identified in yeast [65]. These landmark studies have led to numerous recent breakthroughs in mammals, demonstrating a critical role for autophagy in both physiological and pathological processes, including cancer initiation and progression [64].
The bulk degradation of cellular material through autophagy allows cells to recycle both nutrients and energy during starvation and stress; in this regard, autophagy is proposed to function as a fitness mechanism that allows tumor cells to survive provided the offending stressor is removed in a timely manner [66, 67]. This indispensable contribution of autophagy as a stress-response mechanism is poignantly illustrated by studies in mice, in which the genetic deletion of critical ATGs results in neonatal lethality within a day of birth [68, 69]. A potential role for autophagy in dormancy was originally broached in C. elegans during dauer diapause, a stress-induced, dormancy-like state that occurs when larvae are exposed to hostile environments [70]. Notably, in this model, defective autophagy (achieved via RNAi against multiple ATGs) potently compromised survival during dauer, implying a conserved mechanism by which autophagy promotes survival during quiescent states [70]. Since autophagy is activated in response to various microenvironmental stresses implicated in tumor dormancy, including the UPR (ER-stress), hypoxia, and ECM detachment, an important outstanding issue is how autophagy impacts the survival, as well as the maintenance of the quiescent state, in dormant tumor cells.
Studies in breast cancer models suggest that decreased mitogenic signaling resulting from impaired integrin and growth factor signaling facilitates tumor dormancy [71, 72]. Specifically, suppression of β1-integrin signaling induces dormancy in the MMTV-PyMT model of breast cancer and squamous carcinoma [28, 72]. Thus, it is possible that, because DTCs cannot efficiently engage a foreign ECM, impaired integrin signaling may stimulate autophagy for survival and maintenance of the dormant state. Consistent with this hypothesis, β1-integrin signaling blockade is a potent inducer of autophagy in ECM-detached cells, and autophagy protects cells from detachment-induced apoptosis (anoikis) (see Fig. 5.2) [73]. Moreover, autophagy may contribute to the ability of solitary dormant cells to resist extrinsic apoptotic stimuli. In breast cancer metastases to bone, where DTCs remain dormant in the BM for extended periods of time, the tissue necrosis factor (TNF) ligand TRAIL is abundantly expressed in the BM microenvironment and can kill tumor cells; nonetheless, mechanisms involving Src-mediated TRAIL resistance promote the survival of indolent cells in the BM [74]. Because autophagy can protect cells from TRAIL-induced apoptosis, one can speculate that autophagy may similarly promote the survival of dormant cells in the BM [75, 76]. Interestingly, we found that D-HEp3 cells have constitutively higher levels of autophagy, as measured by green fluorescence protein-tagged LC3 and endogenous LC3 incorporation into autophagosomes, as well as elevated expression of specific autophagy-regulating genes including ATG6, ATG7, and ATG8 (unpublished results). Our ongoing studies also reveal that ATF6, but not PERK, is responsible for LC3 processing into autophagosomes.
Recently, autophagy has been shown to be crucial for the survival of dormant cells in models of ovarian cancer and gastrointestinal stromal tumor (GIST) [77, 78]. The tumor suppressor aplasia Ras homolog member I (ARHI) is downregulated in over 60% of ovarian cancers and the re-expression of ARHI in a variety of human ovarian cancer cell lines induces autophagy (see Fig. 5.2). In xenograft ovarian tumors, ARHI overexpression promotes the formation of dormant tumors, which correlates with an increased level of autophagosome formation; accordingly, when ARHI expression is subsequently reduced, the tumor regains proliferative potential and rapidly re-grows. However, upon treatment of ARHI-induced dormant tumors with the lysosomal inhibitor chloroquine, this regrowth is dramatically reduced, suggesting that autophagy contributes to survival during ARHI-induced dormancy [77].
Another demonstration of autophagy as a survival pathway in quiescent cells comes from studies of GIST, the first solid tumor to be treated successfully with the small-molecule tyrosine kinase inhibitor imatinib mesylate (Gleevec) (see Fig. 5.2) [78]. However, less than 5% of GISTs regress significantly upon Gleevec treatment; rather, in the vast majority of patients, tumor cells indefinitely remain in a dormant, quiescent state in the presence of imatinib. Recent work indicates that this dormant state, termed stable disease, is closely associated with the induction of autophagy in response to imatinib. Upon inhibiting autophagy using RNAi-mediated ATG depletion or antimalarials, such as hydroxychloroquine and quinacrine, GIST cells undergo high levels of apoptosis both in vitro and in vivo. Thus, autophagy appears critical for the establishment of a dormant state in which GIST cells can survive indefinitely [78]. Moreover, these results in GIST broach the exciting idea that autophagy can be more widely exploited to kill or prevent the expansion of quiescent or dormant cancer cells, which are notorious for their resistance to both conventional and targeted therapies [79].
Tumor dormancy is also postulated to be a stress-management mechanism adopted by DTCs to cope with an unfavorable microenvironment by completely withdrawing from the cell cycle [1]. p27Kip1, the cyclin-dependent kinase inhibitor involved in G0/G1 cell cycle arrest, was identified as a downstream target of the energy-sensing LKB1-AMPK pathway, as well as shown to induce autophagy and facilitate cell survival in response to growth factor withdrawal and metabolic stress (see Fig. 5.2) [80]. Thus, DTCs may depend on p27-mediated autophagy to survive in an inhospitable microenvironment and to resist chemotherapy. HEp3 cells in which p38 signaling induces dormancy also have induced strong expression of p27 during their prolonged dormancy, further supporting this notion [26]. However, the exact biological role for autophagy during quiescence remains largely unknown; if autophagy promotes growth suppression in quiescent cells, one can alternatively hypothesize that it may limit the outgrowth of dormant cells into frank macrometastases. These questions are important, and it will be critical to determine whether autophagy plays a quiescence or survival-inducing role (or both) in quiescent DTCs. If autophagy induces a pro-survival state then strategies to block it could eradicate DTCs. In the case that it contributes to both quiescence and survival, then more detailed mechanistic analysis of these pathways will be required to reveal ways to block only the survival signals without interrupting quiescence.
Overall, these results motivate future work, especially those using in vivo preclinical models, to assess how autophagy influences the quiescence and/or survival and biological behavior of dormant breast cancer cells, and specifically whether autophagy inhibition can be exploited to prevent the development of macrometastases in cancer patients.
Concluding Remarks
Our knowledge on how the biology and genetics of DTCs influence dormancy and progression of metastasis remains limited. Many open questions still exist, which will likely become central themes in the future. For example, how is DTC fate affected by the primary tumor microenvironment, how do therapies applied to patients affect DTCs, and how do the target organs condition these responses? If DTCs are indeed the “seeds” of metastases, it will be imperative to directly investigate these questions by analyzing DTCs from patients. Importantly, an analysis of DTCs that survive therapy of the primary tumor will inform us on how these treatments, as well as target organs, impact adaptation and/or selection of subsequent recurrent metastatic disease. For example, the demonstration that DTCs undergo autophagy or tap into UPR survival signals to survive and persist for prolonged periods will be a promising finding that will motivate clinical trials targeting specific components of the autophagy or UPR machinery to eradicate these cells (i.e., maintenance therapy). Studies on dormancy may also yield information on how to maintain signals that propel quiescence, such as a combination of MEK inhibitors and agonists that mimic p38α/β activation. A deeper understanding of the signals that maintain dormancy may lead to the identification of drugs that should be avoided in patients because of their potential to break this state, and thus, enhance disease progression. Although the study of DTCs and dormant disease is difficult, unraveling the inherent complexity of this poorly understood step of metastasis biology should profoundly impact cancer patients.
References
Aguirre-Ghiso JA (2007) Models, mechanisms and clinical evidence for cancer dormancy. Nat Rev Cancer 7:834–846
Klein CA (2011) Framework models of tumor dormancy from patient-derived observations. Curr Opin Genet Dev 21(1):42–49
Sang L, Coller HA, Roberts JM (2008) Control of the reversibility of cellular quiescence by the transcriptional repressor HES1. Science 321:1095–1100
Almog N, Ma L, Raychowdhury R, Schwager C, Erber R, Short S et al (2009) Transcriptional switch of dormant tumors to fast-growing angiogenic phenotype. Cancer Res 69:836–844
Mahnke YD, Schwendemann J, Beckhove P, Schirrmacher V (2005) Maintenance of long-term tumour-specific T-cell memory by residual dormant tumour cells. Immunology 115:325–336
Klein CA (2008) The direct molecular analysis of metastatic precursor cells in breast cancer: a chance for a better understanding of metastasis and for personalised medicine. Eur J Cancer 44(18):2721–2725
Pantel K, Brakenhoff RH (2004) Dissecting the metastatic cascade. Nat Rev Cancer 4: 448–456
Stoecklein NH, Hosch SB, Bezler M, Stern F, Hartmann CH, Vay C et al (2008) Direct genetic analysis of single disseminated cancer cells for prediction of outcome and therapy selection in esophageal cancer. Cancer Cell 13:441–453
Husemann Y, Geigl JB, Schubert F, Musiani P, Meyer M, Burghart E et al (2008) Systemic spread is an early step in breast cancer. Cancer Cell 13:58–68
Schardt JA, Meyer M, Hartmann CH, Schubert F, Schmidt-Kittler O, Fuhrmann C et al (2005) Genomic analysis of single cytokeratin-positive cells from bone marrow reveals early mutational events in breast cancer. Cancer Cell 8:227–239
Schmidt-Kittler O, Ragg T, Daskalakis A, Granzow M, Ahr A, Blankenstein TJ et al (2003) From latent disseminated cells to overt metastasis: genetic analysis of systemic breast cancer progression. Proc Natl Acad Sci USA 100:7737–7742
Klein CA (2009) Parallel progression of primary tumours and metastases. Nat Rev Cancer 9:302–312
Ossowski L, Aguirre-Ghiso JA (2010) Dormancy of metastatic melanoma. Pigment Cell Melanoma Res 23:41–56
Eyles J, Puaux AL, Wang X, Toh B, Prakash C, Hong M et al (2010) Tumor cells disseminate early, but immunosurveillance limits metastatic outgrowth, in a mouse model of melanoma. J Clin Invest 120:2030–2039
Vidal M, Larson DE, Cagan RL (2006) Csk-deficient boundary cells are eliminated from normal Drosophila epithelia by exclusion, migration, and apoptosis. Dev Cell 10:33–44
Klein CA, Hölzel D (2006) Systemic cancer progression and tumor dormancy: mathematical models meet single cell genomics. Cell Cycle 5(16):1788–1798
Bidard FC, Vincent-Salomon A, Sigal-Zafrani B, Rodrigues M, Dieras V, Mignot L et al (2008) Time to metastatic relapse and breast cancer cells dissemination in bone marrow at metastatic relapse. Clin Exp Metastasis 25:871–875
Schewe DM, Aguirre-Ghiso JA (2009) Inhibition of eIF2alpha dephosphorylation maximizes bortezomib efficiency and eliminates quiescent multiple myeloma cells surviving proteasome inhibitor therapy. Cancer Res 69:1545–1552
Kitzis A, Brizard F, Dascalescu C, Chomel JC, Guilhot F, Brizard A (2001) Persistence of transcriptionally silent BCR-ABL rearrangements in chronic myeloid leukemia patients in sustained complete cytogenetic remission. Leuk Lymphoma 42:933–944
Talpaz M, Estrov Z, Kantarjian H, Ku S, Foteh A, Kurzroc R (1994) Persistence of dormant leukemic progenitors during interferon-induced remission in chronic myelogenous leukemia. Analysis by polymerase chain reaction of individual colonies. J Clin Invest 94:1383–1389
Essers MA, Offner S, Blanco-Bose WE, Waibler Z, Kalinke U, Duchosal MA et al (2009) IFNalpha activates dormant haematopoietic stem cells in vivo. Nature 458:904–908
Joyce JA, Pollard JW (2009) Microenvironmental regulation of metastasis. Nat Rev Cancer 9:239–252
Nguyen DX, Bos PD, Massague J (2009) Metastasis: from dissemination to organ-specific colonization. Nat Rev Cancer 9:274–284
Hickson JA, Huo D, Vander Griend DJ, Lin A, Rinker-Schaeffer CW, Yamada SD (2006) The p38 kinases MKK4 and MKK6 suppress metastatic colonization in human ovarian carcinoma. Cancer Res 66:2264–2270
Taylor J, Hickson J, Lotan T, Yamada DS, Rinker-Schaeffer C (2008) Using metastasis suppressor proteins to dissect interactions among cancer cells and their microenvironment. Cancer Metastasis Rev 27:67–73
Adam AP, George A, Schewe D, Bragado P, Iglesias BV, Ranganathan AC et al (2009) Computational identification of a p38SAPK-regulated transcription factor network required for tumor cell quiescence. Cancer Res 69:5664–5672
Adorno M, Cordenonsi M, Montagner M, Dupont S, Wong C, Hann B et al (2009) A mutant-p53/Smad complex opposes p63 to empower TGFbeta-induced metastasis. Cell 137:87–98
Aguirre Ghiso JA, Kovalski K, Ossowski L (1999) Tumor dormancy induced by downregulation of urokinase receptor in human carcinoma involves integrin and MAPK signaling. J Cell Biol 147:89–104
Barkan D, El Touny LH, Michalowski AM, Smith JA, Chu I, Davis AS et al (2010) Metastatic growth from dormant cells induced by a col-I-enriched fibrotic environment. Cancer Res 70:5706–5716
Ranganathan AC, Ojha S, Kourtidis A, Conklin DS, Aguirre-Ghiso JA (2008) Dual function of pancreatic endoplasmic reticulum kinase in tumor cell growth arrest and survival. Cancer Res 68:3260–3268
Ranganathan AC, Zhang L, Adam AP, Aguirre-Ghiso JA (2006) Functional coupling of p38-induced up-regulation of BiP and activation of RNA-dependent protein kinase-like endoplasmic reticulum kinase to drug resistance of dormant carcinoma cells. Cancer Res 66: 1702–1711
Ranganathan AC, Adam AP, Aguirre-Ghiso JA (2006) Opposing roles of mitogenic and stress signaling pathways in the induction of cancer dormancy. Cell Cycle 5(16):1799–1807
Harrison LB, Sessions RB, Ki-Hong W (2003) Head and neck cancer. A multidisciplinary approach, 3rd edn. Lippincott Williams & Wilkins, Philadelphia
Gath HJ, Brakenhoff RH (1999) Minimal residual disease in head and neck cancer. Cancer Metastasis Rev 18:109–126
Wikman H, Vessella R, Pantel K (2008) Cancer micrometastasis and tumour dormancy. APMIS 116:754–770
Fan X, Valdimarsdottir G, Larsson J, Brun A, Magnusson M, Jacobsen SE et al (2002) Transient disruption of autocrine TGF-beta signaling leads to enhanced survival and proliferation potential in single primitive human hemopoietic progenitor cells. J Immunol 168:755–762
Fortunel N, Hatzfeld J, Kisselev S, Monier MN, Ducos K, Cardoso A et al (2000) Release from quiescence of primitive human hematopoietic stem/progenitor cells by blocking their cell-surface TGF-beta type II receptor in a short-term in vitro assay. Stem Cells 18:102–111
Scandura JM, Boccuni P, Massague J, Nimer SD (2004) Transforming growth factor beta-induced cell cycle arrest of human hematopoietic cells requires p57KIP2 up-regulation. Proc Natl Acad Sci USA 101:15231–15236
Yamazaki S, Iwama A, Takayanagi S, Eto K, Ema H, Nakauchi H (2009) TGF-beta as a candidate bone marrow niche signal to induce hematopoietic stem cell hibernation. Blood 113:1250–1256
Muraoka-Cook RS, Kurokawa H, Koh Y, Forbes JT, Roebuck LR, Barcellos-Hoff MH et al (2004) Conditional overexpression of active transforming growth factor beta1 in vivo accelerates metastases of transgenic mammary tumors. Cancer Res 64:9002–9011
Kang Y, Siegel PM, Shu W, Drobnjak M, Kakonen SM, Cordon-Cardo C et al (2003) A multigenic program mediating breast cancer metastasis to bone. Cancer Cell 3:537–549
Dumont N, Arteaga CL (2003) Targeting the TGF beta signaling network in human neoplasia. Cancer Cell 3:531–536
Siegel PM, Massague J (2003) Cytostatic and apoptotic actions of TGF-beta in homeostasis and cancer. Nat Rev Cancer 3:807–821
Hideshima T, Podar K, Chauhan D, Anderson KC (2005) Cytokines and signal transduction. Best Pract Res Clin Haematol 18:509–524
Javelaud D, Alexaki VI, Mauviel A (2008) Transforming growth factor-beta in cutaneous melanoma. Pigment Cell Melanoma Res 21:123–132
Hussein MR (2005) Transforming growth factor-beta and malignant melanoma: molecular mechanisms. J Cutan Pathol 32:389–395
Hsu MY, Rovinsky S, Penmatcha S, Herlyn M, Muirhead D (2005) Bone morphogenetic proteins in melanoma: angel or devil? Cancer Metastasis Rev 24:251–263
Reed JA, Bales E, Xu W, Okan NA, Bandyopadhyay D, Medrano EE (2001) Cytoplasmic localization of the oncogenic protein Ski in human cutaneous melanomas in vivo: functional implications for transforming growth factor beta signaling. Cancer Res 61:8074–8078
Zapas JL, Coley HC, Beam SL, Brown SD, Jablonski KA, Elias EG (2003) The risk of regional lymph node metastases in patients with melanoma less than 1.0 mm thick: recommendations for sentinel lymph node biopsy. J Am Coll Surg 197:403–407
Gamel JW, George SL, Edwards MJ, Seigler HF (2002) The long-term clinical course of patients with cutaneous melanoma. Cancer 95:1286–1293
Eskelin S, Pyrhonen S, Summanen P, Hahka-Kemppinen M, Kivela T (2000) Tumor doubling times in metastatic malignant melanoma of the uvea: tumor progression before and after treatment. Ophthalmology 107:1443–1449
Aguirre-Ghiso JA, Ossowski L, Rosenbaum SK (2004) Green fluorescent protein tagging of extracellular signal-regulated kinase and p38 pathways reveals novel dynamics of pathway activation during primary and metastatic growth. Cancer Res 64:7336–7345
Aguirre-Ghiso JA, Estrada Y, Liu D, Ossowski L (2003) ERK(MAPK) activity as a determinant of tumor growth and dormancy; regulation by p38(SAPK). Cancer Res 63:1684–1695
Aguirre-Ghiso JA, Liu D, Mignatti A, Kovalski K, Ossowski L (2001) Urokinase receptor and fibronectin regulate the ERK(MAPK) to p38(MAPK) activity ratios that determine carcinoma cell proliferation or dormancy in vivo. Mol Biol Cell 12:863–879
Liu D, Aguirre Ghiso J, Estrada Y, Ossowski L (2002) EGFR is a transducer of the urokinase receptor initiated signal that is required for in vivo growth of a human carcinoma. Cancer Cell 1:445–457
Aguirre Ghiso JA (2002) Inhibition of FAK signaling activated by urokinase receptor induces dormancy in human carcinoma cells in vivo. Oncogene 21:2513–2524
Schewe DM, Aguirre-Ghiso JA (2008) ATF6alpha-Rheb-mTOR signaling promotes survival of dormant tumor cells in vivo. Proc Natl Acad Sci USA 105:10519–10524
Ranganathan AC, Adam AP, Zhang L, Aguirre-Ghiso JA (2006) Tumor cell dormancy induced by p38(SAPK) and ER-stress signaling: an adaptive advantage for metastatic cells? Cancer Biol Ther 5:729–735
Fu Y, Li J, Lee AS (2007) GRP78/BiP inhibits endoplasmic reticulum BIK and protects human breast cancer cells against estrogen starvation-induced apoptosis. Cancer Res 67:3734–3740
Fukuyama M, Rougvie AE, Rothman JH (2006) C. elegans DAF-18/PTEN mediates nutrient-dependent arrest of cell cycle and growth in the germline. Curr Biol 16:773–779
Wang J, Kim SK (2003) Global analysis of dauer gene expression in Caenorhabditis elegans. Development 130:1621–1634
Long X, Spycher C, Han ZS, Rose AM, Muller F, Avruch J (2002) TOR deficiency in C. elegans causes developmental arrest and intestinal atrophy by inhibition of mRNA translation. Curr Biol 12:1448–1461
Lopez-Maury L, Marguerat S, Bahler J (2008) Tuning gene expression to changing environments: from rapid responses to evolutionary adaptation. Nat Rev Genet 9:583–593
Mizushima N, Levine B, Cuervo AM, Klionsky DJ (2008) Autophagy fights disease through cellular self-digestion. Nature 451:1069–1075
Klionsky DJ, Cregg JM, Dunn WA Jr, Emr SD, Sakai Y, Sandoval IV et al (2003) A unified nomenclature for yeast autophagy-related genes. Dev Cell 5:539–545
Lum JJ, Bauer DE, Kong M, Harris MH, Li C, Lindsten T et al (2005) Growth factor regulation of autophagy and cell survival in the absence of apoptosis. Cell 120:237–248
Roy S, Debnath J (2010) Autophagy and tumorigenesis. Semin Immunopathol 32:383–396
Komatsu M, Waguri S, Ueno T, Iwata J, Murata S, Tanida I et al (2005) Impairment of starvation-induced and constitutive autophagy in Atg7-deficient mice. J Cell Biol 169:425–434
Kuma A, Hatano M, Matsui M, Yamamoto A, Nakaya H, Yoshimori T et al (2004) The role of autophagy during the early neonatal starvation period. Nature 432:1032–1036
Melendez A, Talloczy Z, Seaman M, Eskelinen E-L, Hall DH, Levine B (2003) Autophagy genes are essential for dauer development and life-span extension in C. elegans. Science 301:1387–1391
Korah R, Boots M, Wieder R (2004) Integrin alpha5beta1 promotes survival of growth-arrested breast cancer cells: an in vitro paradigm for breast cancer dormancy in bone marrow. Cancer Res 64:4514–4522
White DE, Kurpios NA, Zuo D, Hassell JA, Blaess S, Mueller U et al (2004) Targeted disruption of beta1-integrin in a transgenic mouse model of human breast cancer reveals an essential role in mammary tumor induction. Cancer Cell 6:159–170
Fung C, Lock R, Gao S, Salas E, Debnath J (2008) Induction of autophagy during extracellular matrix detachment promotes cell survival. Mol Biol Cell 19:797–806
Zhang XH, Wang Q, Gerald W, Hudis CA, Norton L, Smid M et al (2009) Latent bone metastasis in breast cancer tied to Src-dependent survival signals. Cancer Cell 16:67–78
Han J, Hou W, Goldstein LA, Lu C, Stolz DB, Yin XM et al (2008) Involvement of protective autophagy in TRAIL resistance of apoptosis-defective tumor cells. J Biol Chem 283:19665–19677
Herrero-Martin G, Hoyer-Hansen M, Garcia-Garcia C, Fumarola C, Farkas T, Lopez-Rivas A et al (2009) TAK1 activates AMPK-dependent cytoprotective autophagy in TRAIL-treated epithelial cells. EMBO J 28:677–685
Lu Z, Luo RZ, Lu Y, Zhang X, Yu Q, Khare S et al (2008) The tumor suppressor gene ARHI regulates autophagy and tumor dormancy in human ovarian cancer cells. J Clin Invest 118: 3917–3929
Gupta A, Roy S, Lazar AJ, Wang WL, McAuliffe JC, Reynoso D et al (2010) Autophagy inhibition and antimalarials promote cell death in gastrointestinal stromal tumor (GIST). Proc Natl Acad Sci USA 107:14333–14338
Rubin BP, Debnath J (2010) Therapeutic implications of autophagy-mediated cell survival in gastrointestinal stromal tumor after treatment with imatinib mesylate. Autophagy 6: 1190–1191
Liang J, Shao SH, Xu ZX, Hennessy B, Ding Z, Larrea M et al (2007) The energy sensing LKB1-AMPK pathway regulates p27(kip1) phosphorylation mediating the decision to enter autophagy or apoptosis. Nat Cell Biol 9:218–224
Acknowledgements
This work is supported by grants from the Samuel Waxman Cancer Research Foundation Tumor Dormancy Program, NIH/National Cancer Institute (CA109182, CA163131), NIEHS (ES017146), and NYSTEM to J.A.A-G, DoD Breast Cancer Postdoctoral Fellowship to M.S.S. and NIH RO1 CA126792, CA126792-S1 (ARRA), and a DOD BCRP Era of Hope Scholar Award (W81XWH-11-1-0310) to J.D.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Sosa, M.S., Bragado, P., Debnath, J., Aguirre-Ghiso, J.A. (2013). Regulation of Tumor Cell Dormancy by Tissue Microenvironments and Autophagy. In: Enderling, H., Almog, N., Hlatky, L. (eds) Systems Biology of Tumor Dormancy. Advances in Experimental Medicine and Biology, vol 734. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-1445-2_5
Download citation
DOI: https://doi.org/10.1007/978-1-4614-1445-2_5
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-1444-5
Online ISBN: 978-1-4614-1445-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)