Abstract
Osteosarcoma is a primary malignant tumor of the bone in which proliferating neoplastic cells produce osteoid and/or bone, if only in small amounts. This histological principle defines a tumor that usually affects young males more frequently than females, and disproportionately involves the long bones of the appendicular skeleton. These tumors are generally locally aggressive and tend to produce early, lethal systemic metastases. However, osteosarcoma is not a single disease but a family of neoplasms, sharing the single histological finding of osseous matrix production in association with malignant cells.
The majority (i.e., 75%) of cases are relatively stereotypical from the demographic, clinical, radiographic and histologic points of view. These tumors generally occur in the metaphyseal portion of the medullary cavity of the long bone and are referred to as “Conventional Osteosarcoma.” The group is sub classified by the form of the dominant matrix present within the tumor, which may be bone, cartilage or fibrous tissue, and it is correspondingly referred to as osteoblastic, chondroblastic and fibroblastic osteosarcoma.
The remaining 25% of cases have unique parameters that allow reproducible identification of tumors which are biologically different from conventional osteosarcoma and are referred to as “Variants.” The parameters identifying Variants fall into one of three major groups: (1) clinical factors, (2) histologic findings and (3) location of origin − within or on the cortex. Because of their inherent biological difference from Conventional Osteosarcoma, the Variants identify cases which must be excluded from analysis of data pertaining to the treatment of the majority of cases: Conventional Osteosarcoma.
The diagnostic parameters of osteosarcoma must be sufficiently inclusive to identify all the members of this potentially lethal tumor. Conversely, criteria for sub classification must be restricted to assure homogenous populations of tumors productively incorporating different biological behavior and the potential for development of unique treatment strategies which are different from those for Conventional Osteosarcoma. This can be designated “Classification Based Therapy” or “Therapy Based Osteosarcoma.”
With this background, we will discuss the highly disciplined approach to the management of osteosarcoma from the pathologist’s perspective. Factors governing the assessment of the response to preoperative chemotherapy will also be reviewed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Osteosarcoma is a primary malignant tumor of the bone in which proliferating neoplastic cells produce osteoid and/or bone, even if only in small amounts.1,2 Osteoid is an extra cellular matrix and must be distinguished from type 1 collagen. The distinction, essentially, is between osseous collagen and nonosseous collagen. From a morphological perspective, osteoid can be defined as a pink (eosinophilic) material which is amorphous, homogeneous, refractile, occasionally curvilinear, and randomly oriented (Fig. 1). It can show varying degrees of calcification. Osteoid is intimately associated with the malignant cells that comprise osteosarcoma (Fig. 2).
Classification
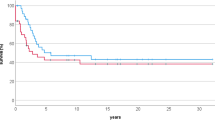
Osteosarcoma may affect any bone, but it predominantly occurs in the metaphyseal regions of the appendicular skeleton. The distribution by age, sex, and site of the lesions in 962 patients seen at the M.D. Anderson Cancer Center is depicted in Fig. 3. Pain and swelling are the cardinal clinical symptoms, often accompanied by restriction in movement. The diagnosis and classification is made in conjunction with imaging studies, which are determined by the amount of ossification and calcification. The tumors may be purely lytic or sclerotic but usually have a combination of both features. Correlation with imaging is crucial for establishing the diagnosis.
From a pathological perspective, osteosarcoma may be classified as “Conventional Osteosarcoma” and “Osteosarcoma Variants.” The osseous matrix (Fig. 4) is the single unifying feature, and classification is dependent on the predominant type. Classifications vary. A classification from Dahlin from the American Journal of Surgical Pathology is reproduced in Table 1 1 and suggested variants from 1977 to the present, from the M.D. Anderson Cancer Center, are depicted in Table 2.
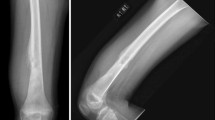
Conventional Osteosarcoma
An algorithm can be formulated to help define the exact diagnosis. It commences with identification of the presence or absence of osteoid. If osteoid is present, the diagnosis is one of osteosarcoma. If osteoid is absent, another diagnosis must be considered. Here, it is important to correlate with radiologic features as core biopsies may not be representative of the lesion. A request for rebiopsy may sometimes be required, especially if the radiologic findings are highly suspicious for osteosarcoma, but the biopsy does not confirm the radiologic impression. The predominant matrix is then identified. This may comprise osteoid/bone, cartilage or fibrous tissue. If osteoid/bone is present, it is considered to be an osteoblastic osteosarcoma (Fig. 5). In imaging studies, it is identified as a bone producing tumor with sclerosis infiltrating the cortex and fine ramifications into the soft tissue, often manifesting as an aggressive periosteal reaction (Fig. 6). The periosteal reaction may demonstrate a Codman’s triangle, if the periosteum is elevated and sparse calcified tumor matrix is present at the junction. Alternatively, an exuberant calcified mass of bone matrix may produce a “sunburst” appearance of the periosteum and cortex. If the predominant matrix is cartilage, it is a chondroblastic osteosarcoma (Fig. 7) and on imaging, it may have a chondroid appearance with destructive infiltrative characteristics (Fig. 8). If the predominant matrix is scarce or absent, the diagnosis is fibroblastic osteosarcoma (Fig. 9). On gross pathologic examination, it has a sarcoma-like, soft and fleshy appearance, and the image is devoid of bone and cartilage (Fig. 10). Regardless of the degree of chondroid or fibrous tissue present, typical osteoid or bone production by tumor cells establishes a diagnosis of osteosarcoma.1
Osteoblastic, chondroblastic and fibroblastic osteosarcoma constitute 70% of the conventional types of osteosarcoma.
Osteosarcoma Variants
Variants can be subdivided into Clinical, Morphological and Surface entities. It is important to recognize this diagnostic and biologic diversity to ensure specific therapy and appropriate data analysis.
Clinical variants (∼9%, overall) comprise jaw osteosarcoma (6%), Paget’s Sarcoma (1%), postradiation osteosarcoma (1%), multicentric (multifocal) osteosarcoma (<1%) and osteosarcoma in other categories (1%). Morphological variants (∼7%, overall) comprise low-grade intraosseous osteosarcoma (1%), telangiectatic osteosarcoma (3%), small cell osteosarcoma (2%) and malignant fibrous histiocytoma (MFH) (2%). Cortical and surface variants (∼7%, overall) comprise parosteal osteosarcoma (4%), dedifferentiated parosteal osteosarcoma (1%), periosteal osteosarcoma (1%) and high-grade surface osteosarcoma (1%).
The list of variants appears daunting (see also Chaps. 3 and 5). However, a comment on the “more frequently” encountered forms is appropriate.
Telangiectatic osteosacoma accounts for less than 5% of osteosarcomas.3 The lesion is rapidly expansile and aggressive, and may simulate aneurysmal bone cyst. It is composed of loculated-blood filled spaces, partially lined by malignant cells producing sparse osteoid.4–6 Small cell osteosarcoma is an uncommon variant which histologically resembles Ewing’s sarcoma. Most of the tumors are composed of small round cells separated by collagenous bands of a fine eosinophilic matrix. The cells have ovoid nuclei and, unlike Ewing’s Sarcoma, have a tendency to spindle.7,8 Modern molecular methods can help define Ewing’s sarcoma and differentiate it from small cell osteosarcoma, but the specificity of this finding and the relationship of these two entities is questioned by some. Malignant fibrocytic histiocytoma tends to involve the ends of long bones; there may be less periosteal reaction. Pleomorphic spindle cells are noted, and multinucleated giant cells may be seen. An inflammatory background is not unusual, with a characteristic storiform or spiral nebular arrangement.9–11 Low grade central osteosarcoma usually involves older patients, with the knee as a predilected site.12 On imaging studies, the lesion may appear benign or may show dense sclerosis without massive destruction, as seen in conventional osteosarcoma. Spindle cells with variable amounts of bone and collagen are seen. The lesion may look more ominous on imaging. Histologically, it may resemble desmoplastic fibroma or fibrous dysplasia. Osteosarcoma developing in the setting of Paget’s disease and in radiated bones is generally pleomorphic, as in conventional osteosarcoma, and the biological behavior is equally grave.
Osteosarcoma arising on the surfaces of bones is generally more indolent than those arising centrally. Four major subtypes may be recognized: parosteal osteosarcoma, periosteal osteosarcoma, high grade surface osteosarcoma and dedifferentiated parosteal osteosarcoma.
Parosteal osteosarcoma is a tumor usually seen in the third and fourth decades of life. Most tumours are situated on the surface of the posterior distal femur.13,14 The osteosarcoma usually presents as a dense mass adjacent to the cortex. Histologically, there is a mass of bone with varying stages of maturation, and fibrous stroma is present between the bone spicules. Computer tomography may assist in determining medullary invasion which must be distinguished from a benign potential mimic, myositis ossificans.
Dedifferentiated parosteal osteosarcoma commences as a low grade parosteal osteosarcoma and later develops a high-grade mesenchymal component which, on histological examination, is indistinguishable from conventional osteosarcoma. The tumor resembles parosteal osteosarcoma on imaging, but histologically, areas of high-grade and low-grade bone-forming sarcoma are present. Dedifferentiation has been cited to occur in 20% of low grade osteosarcomas.15
Periosteal osteosarcoma occurs most often in adolescence. It usually occurs on the surface of the shaft of a long bone. The characteristic histological feature is malignant cartilaginous tissue. It may be confused with chondrosarcoma.14 The presence of osteoid, albeit minimally, and its occurrence in younger patients may assist in establishing the diagnosis and distinguishing it from chondrosarcoma.16 , 17
High-grade surface osteosarcoma is a highly malignant surface tumor of bone. The imaging features may be similar to those of parosteal or periosteal osteosarcoma. It generally arises on the bone surface along the midshaft and usually does not invade the medullary cavity. The histological features are identical to those of high-grade conventional osteosarcoma. The matrix is not well-differentiated when contrasted with dedifferentiated parosteal osteosarcoma.18
Osteosarcomas of the jaw and skull are seen more often in an older age group compared to pediatric and adolescent patients.19 Many osteosarcomas of the jaw show cartilaginous differentiation. They generally do not metastasize to distant sites.20
Osteosarcoma of the skull is extremely rare. It is highly malignant and, interestingly, does not exhibit chondroblastic differentiation.15
Radiation induced osteosarcoma develops in previously radiated bones. It is highly malignant and equivalent to conventional osteosarcoma. Multifocal sclerosing (multicentric) osteosarcoma is highly malignant and affects multiple bones simultaneously.
The above classification lends itself to “Therapy Based Osteosarcoma.” Standard primary chemotherapy is generally administered for osteoblastic, chondroblastic, fibroblastic and telangiectatic osteosarcoma. Intensification of chemotherapy may be recommended for postradiation osteosarcoma, Paget’s disease, multicentric osteosarcoma, small-cell osteosarcoma (therapy integrated with that recommended for Ewing’s sarcoma), dedifferentiated parosteal osteosarcoma and high-grade surface osteosarcoma. In contrast, surgical excision alone may be recommended for low grade central osteosarcoma, parosteal osteosarcoma, periosteal osteosarcoma and jaw osteosarcoma, provided there is no evidence of progression to high-grade mitotic activity.
Diagnostic Biopsy
Biopsy may be obtained by two different mechanisms: open and closed. Open biopsy is a surgical procedure performed under general anesthesia and may involve incision or excision of the tumor. It usually provides liberal amounts of tissue for diagnostic and investigational purposes. An open biopsy should preferably be performed by the surgeon who will perform the limb salvage procedure as the biopsy site and track must be completely excised in the subsequent definitive surgical procedure. Closed biopsy is obtained with a needle. This provides an aspirate and a core (Fig. 11). Several “passes” may have to be made to provide sufficient material for investigational purposes. The instruments employed for needle biopsy are illustrated in Fig. 12. A needle biopsy may be performed by an interventional radiologist. It is generally performed as an outpatient procedure under local anesthesia or conscious sedation. A rapid definitive strategy of treatment can be planned shortly upon receipt of the diagnosis.
The hazards of biopsy in patients with malignant primary bone and soft tissue tumors have been addressed.21 An open biopsy may be fraught with complications, including tissue contamination, which may jeopardize the patient’s candidacy for a limb salvage procedure. There is minimal contamination with needle biopsy (Fig. 13). The procedure was found to be accurate in 89% of 265 osteosarcoma patients in whom needle biopsy was performed at the M.D. Anderson Cancer Center.
Specimen Therapy Evaluation
The goals of therapy evaluation comprise confirmation of the diagnosis, status of the margin and extent of the disease, classification and subclassification of the neoplasm, imaging correlation and response to therapy. The response is both qualitative and quantitative. To achieve these goals, representative sections of the tumor must be obtained. This is undertaken through a standardized work-up. One of the most important aspects of this workup is to identify the viable tumor, which is utilized as a guide for planning postoperative treatment.
Preparation of Gross Specimen
Specimens submitted from orthopedic oncologic surgical procedures range from resection to major ablative extirpation. The latter tends to be large, complex and somewhat intimidating. The goal of specimen examination is to reduce the specimen to the tumor and the parent bone. Details regarding the preparation of orthopedic specimens have been published.22 , 23 The pathologist should also review the clinical and imaging material before commencing preparation and examination.
External examination of the gross specimen of the skin is brief. The extent of contamination of the biopsy site by tumor and coexisting diseases are noted. Extensive vascular invasion can be grossly assessed by a cross-section of the significant draining vein or veins in the location where their paths are relatively consistent (e.g., popliteal or anticubital fossa). The specimen is dissected so that only the tumor and the parent bone remain (Fig. 14). After the soft tissues have been removed, the tumor-distorted bone is sectioned in one of the long axes in a plane that will maximally demonstrate the areas suspected for residual viable tumor. This results in a central “slab section” and two opposing “hemispheres” (Fig. 15). A Toledo Meat Saw (Toledo Scale, Toledo OH) or equivalent is utilized. The specimen should be photographed for permanent record.
Tumor and parent bone following dissection for assessment of chemotherapy response. The blue area represents the neoplasm and the red area, the site of suspected residual viable tumor. Reprinted with permission from Reprinted with permission from Raymond AK et al: Osteosarcoma chemotherapy effect: A prognostic factor: Semin Diag Pathol 4: 212–236. 1987
A review of the preoperative angiogram in a patient treated with intra-arterial chemotherapy will assist in the above-mentioned process. More than 95% of osteosarcomas are hypervascular. Reduction and/or disappearance of tumor neovasculartiy and stain are sensitive but nonspecific indicators of a good response to therapy. Persistence of residual neovascularity after three courses of chemotherapy is almost always an indication of poor response to treatment, with significant amounts of residual viable tumor.25–29 Response may also manifest with progressive mineralization (i.e., opacification) and reduction in tumor size.
The slab section is cut from end-to-end (for “mapping”) and submitted for decalcification, processing and histologic analysis. An Isomet saw is used for this part of the dissection (Buechler, Lake Bluff, IL). This is a geologic saw with a diamond impregnated circular blade and water bath (Fig. 16).
Before decalcification of the cut slab, sections are reassembled into their prior anatomic configuration and a specimen radiograph is obtained. Each piece is assigned a section code that is recorded on the specimen radiograph (Figs. 17–20). The radiograph is labeled to match the numbering system (section code) of the processing cassettes. It also provides a permanent record of the submitted sections (“map”). Additional sections are taken from the unsampled hemispheres. These are referred to as “random” sections, as there is no corresponding radiographic record of their precise anatomic location.
Slab section is completely sectioned and will be entirely submitted for histologic analysis. Prior to decalcification and processing, the pieces are reassembled and used to prepare a specimen radiograph (Fig. 18). Reprinted with permission from Raymond AK et al: Osteosarcoma chemotherapy effect: A prognostic factor: Semin Diag Pathol 4: 212–236. 1987
Osteosarcoma mapping. Specimen radiograph with mapping code. The specimen was cut, reassembled, coded, and submitted for specimen radiograph prior to decalcification. Cells demonstrating extensive therapeutic effect and indeterminate viability. Reprinted with permission from Raymond AK et al: Osteosarcoma chemotherapy effect: A prognostic factor: Semin Diag Pathol 4: 212–236. 1987
“Map” created by using the specimen radiograph. Areas containing viable tumor indicated in white (periosteum, cortex, articular cartilage, epiphyseal plate and normal bone marrow). Reprinted with permission from Reprinted with permission from Raymond AK et al: Osteosarcoma chemotherapy effect: A prognostic factor: Semin Diag Pathol 4: 212–236. 198722
Histologic Analysis
A large number of morphological parameters are reviewed: classification and sub classification; the presence or absence of tumor; anatomic distribution, if tumor is present; qualitative and quantitative analysis of viable tumor; qualitative and quantitative analysis of tumor necrosis; and documentation of any reactive processes. Correlation with clinical and imaging findings and review of any additional investigational parameters are also noted.
Evaluation of chemotherapy effect requires not only the ability to detect tumor necrosis, but also makes the assumption that there has been adequate representation of the tumor. This can be tedious and time consuming. The single best prognostic factor following preoperative chemotherapy is tumor necrosis of above 90%.29 It has been advocated that postoperative chemotherapy be modified according to the histologic response of the effect of preoperative chemotherapy on the primary tumor.29 However, this strategy is not universally accepted because of disparate histologic responses in simultaneously resected primary and metastatic tumors following treatment with neaoadjuvant therapy.30
The effects of chemotherapy are analyzed in terms of percent tumor necrosis. The hallmark of osteosarcoma necrosis is the dropout of neoplastic cells. Acellular tumor-produced matrix (i.e., osteoid, bone and cartilage) remains in areas previously occupied by viable tumor. Residual matrix is frequently accompanied by cellular debris and an ingrowth of rudimentary granulation tissue, hemosiderin deposition and/or fibrosis of varying density. An important criterion is the definitive absence of tumor cells. There may be scattered cells with significantly bizarre nuclear and/or cytoplasmic features or both; it can be difficult to assess whether these likely therapy-induced changes are malignant cells or atypical stromal cells. Questionable cellular changes in which there is no way to prove viability or identity also create confusion, and these are, perhaps, best reported solely as “Present” or “Absent” (Fig. 21) in an accompanying note. Response to the treatment of the three major types of osteosarcoma is depicted in Figs. 22– 24.
Response to preoperative chemotherapy is a sensitive prognostic indicator that enables early identification of tumors in patients who have a high probability of surviving vs. those who potentially will not respond to treatment. The method is used to perform analyses of the effects of treatment and is not arbitrary. Reporting of the results must be clear, concise and accurate. This will also assist in planning the administration of optimum postoperative adjuvant chemotherapy.
References
Dahlin DC, Unni KK. Osteosarcoma and its important recognizable variants. Am J Surg Pathol. 1977;1:61-72.
Lichtenstein L. Bone Tumors. 4th ed. St Louis: CV Mosby Company; 1972:215-243.
Unni KK. Osteosarcoma in bone. In: Unni KK, ed. Bone Tumors. New York: Churchill Livingston; 1988:107-133.
Matsuno T, Unni KK, Mc Cleod RA, et al. Telangiectatic osteosarcoma. Cancer. 1976;38:2538-2547.
Farr GH, Huvos SG, Marcove RC, et al. Telangiectatic osteogenic sarcoma: a review of twenty eight cases. Cancer. 1974;34:1150-1158.
Huvos AG, Rosen G, Bretsky SS, et al. Telangiectatic osteosarcoma; a clinicopathologic study of 124 cases. Cancer. 1982;49:1679-1689.
Eidekin J, Raymond AK, Ayala AC, et al. Small cell oseosarcoma. Skeletal Radiol. 1987;16:621-628.
Sim FH, Unni KK, Beabout JW, et al. Osteosarcoma with small cells simulating Ewing’s tumor. J Bone Joint Surg. 1979;61A:207-215.
Dahlin DC, Unni KK, Matsumo T. Malignant (fibrous) histiocytoma of bone – fact or fancy? Cancer. 1977;39:1508-1516.
Wold LE. Fibrohistiocytic tumors of bone. In: Unni KK, ed. Bone Tumors. New York: Churchill Livingstone; 1988:183-197.
Balance WA, Mendelson G, Carter JA, et al. Osteogenic sarcoma. Malignant fibrous histiocytoma subtype. Cancer. 1988;62:763-771.
Unni KK, Dahlin DC, Mc Cleod RA. Intraosseous well differentiated osteosacoma. Cancer. 1977;40:1337-1347.
Ahuja SC, Villacin AB, Smith J, et al. Juxtacortical (parosteal) osteogenic sarcoma: histological grading and prognosis. J Bone Joint Surg. 1977;59:632-647.
Schajowicz F, Mc Guire MH, Araiyo ES, et al. Osteosarcomas arising on the surfaces of long bones. J Bone Joint Surg. 1988;70A:555-564.
Unni KK. Osteosarcoma of bone. In: Unni KK, ed. Bone Tumors. New York: Churchill Livingstone; 1988:107-133.
Hall RB, Robinson LH, Malawer MM, et al. Periosteal osteosarcoma. Cancer. 1985;55:165-171.
Unni KK, Dahlin DC, Beabout JW. Periosteal osteosarcoma. Cancer. 1976;37:2476-2485.
Wold LE, Unni KK, Beabout JW, et al. High-grade surface osteosarcoma. Am J Surg Pathol. 1984;8:181-186.
Unni KK. Osteosarcoma of bone. In: Unni KK, ed. Bone Tumors. New York: Churchill Livingstone; 1988:107-133.
Clark JL, Unni KK, Dahlin DC, et al. Osteosarcoma of the jaw. Cancer. 1983;51:2311-2316.
Mankin HJ, Lange TA, Spanier SS. The hazards of biopsy in patients with malignant primary bone and soft tissue tumors. J Bone Joint Surg. 1982;64:1121-1127.
Raymond AK, Ayala AG. Specimen management after chemotherapy. In: Unni KK, ed. Bone Tumors. New York: Churchill Livingstone; 1988:157-181.
Weatherby RP, Unni KK. Practical aspects of handling orthopedic specimens in the surgical pathology laboratory. Pathol Annu. 1982;17:1-31.
Raymond AK, Chawla SP, Carrasco HC, et al. Osteosarcoma chemotherapy effect: a prognostic factor. Semin Diagn Pathol. 1987;4:212-236.
Jaffe N, Knapp J, Chuang VP, et al. Osteosarcoma: Intra-arterial treatment of the primary tumor with cis-diamminedichloroplatinum-II (CDP) angiographic, pathologic, and pharmacologic studies. Cancer. 1983;51:402-407.
Carrasco CH, Chawla EP, Benjamin RS, et al. Arteriographic production of tumor necrosis after primary treatment of osteosarcoma in adults (abstract). Proc Am Soc Clin Oncol. 1987;6:126.
Carrasco CH, Charnasangavej C, Richli WR, et al. Angiographic response of assessment to preoperative chemotherapy in osteosarcoma. Radiology. 1989;170:839-843.
Kupman W, Lechner G, Wittich GR. The angiographic response of osteosarcoma following preoperative chemotherapy. Skeletal Radiol. 1985;15:96-102.
Benjamin RS. Chemotherapy for osteosarcoma. In: Unni KK, ed. Bone Tumors. New York: Churchill Livingstone; 1988:149-156.
Nachman J, Simon MA, Dean L, et al. Disparate histologic response in simultaneously resected primary and metastatic osteosarcoma. J Clin Oncol. 1987;5:1185-1190.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Raymond, A.K., Jaffe, N. (2009). Osteosarcoma Multidisciplinary Approach to the Management from the Pathologist’s Perspective. In: Jaffe, N., Bruland, O., Bielack, S. (eds) Pediatric and Adolescent Osteosarcoma. Cancer Treatment and Research, vol 152. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-0284-9_4
Download citation
DOI: https://doi.org/10.1007/978-1-4419-0284-9_4
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4419-0283-2
Online ISBN: 978-1-4419-0284-9
eBook Packages: MedicineMedicine (R0)