Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Hospitals stay at a critical point in providing first care to people who are affected in a natural or human-made disaster. Pandemics can lead to an increasing spread of disease, with irregular and suddenly increasing patient demands that can affect the capacity of hospitals and the overall functioning of the health system. At these times, risks arising based on hospital location, building, medical staff, patients, and health care process strongly have a negative impact on the fight against the outbreak. In order to cope with the difficulty of such an epidemic disaster, hospitals must have completed their preparations and taken the required measures against risks before these events occur.
Nowadays, the vast majority of the world is struggling against the epidemic of Covid-19. The world is faced with the demand for infected patients who arrive at the hospitals heavily and irregularly. Hospitals are facilities with complex processes, mostly connected to external support and supply lines [1]. Even in regular times, many hospitals operate at full capacity or close to full capacity. In epidemic conditions, with surge demand, hospitals may find it challenging to carry out their basic functional activities, and capacity may no longer meet this demand [2]. Even a well-prepared hospital for disasters will have a hard time coping with the consequences of a Covid-19 pandemic. It is an effective hospital management policy that will reduce these difficulties to some extent. In a report of WHO, it is highlighted that this effective hospital management will help (1) continuity of essential services, (2) well-coordinated implementation of priority action, (3) clear and accurate internal and external communication, (4) swift adaptation to increased demands, (5) effective use of scarce resources, and (6) safe environment for health workers [3].
Considering the possible negative consequences of the Covid-19 pandemic, where the healthcare sector and hospitals are currently in a great struggle, it is clear that making the hospitals prepared and ready for such disaster-based risks should be made quickly and reliably. This reinforces the conclusion that risk assessment studies for determining the hazards that arise in hospitals and eliminating these hazards or reducing their effects to an acceptable level are of great importance to reduce the losses of the epidemic.
During natural disasters and pandemics, necessary measures should be taken to determine the risks in the service process and to minimize these risks in order to increase the service quality of hospitals and to enable the society to access health services more easily. Studies evaluating the risks that may arise in the hospital during the pandemic period are very rare in the literature. In this context, the risks that may arise especially during the pandemic were evaluated and preventive measures were presented.
Therefore, in this study, an interval-valued Pythagorean fuzzy technique for order preferences by similarity to ideal solution (IVPF-TOPSIS) based risk prioritization approach is proposed. Since the risk assessment studies contain uncertainty due to the subjective nature of human judgments, interval-valued Pythagorean fuzzy sets (IVPFSs) can reflect the fuzziness, ambiguity, and uncertainty well in making decisions. The proposed approach is further applied in prioritizing the risks that emerged at hospitals in times of the Covid-19 pandemic.
The rest of the chapter is presented as follows: literature review of IVPFSs and IVPF-TOPSIS are presented in the next section. The situation analysis of Turkey’s covid-19 pandemic is given in Sect. 3. The applied methodology is presented in Sect. 4. The case study is given in Sect. 5. In the last section, the conclusion is presented.
2 Literature Review
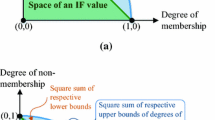
The evaluator role of decision-makers in decision-making problems requires the use of fuzzy logic theory in the face of various uncertainties. Subjectivity and uncertainty in the judgments of the evaluators about the evaluation criteria is an important and difficult problem that also occurs in the solution of the problem addressed in this study. The fuzzy set theory (FST) presented by Zadeh [4] has been previously applied to the solution of many decision problems. This theory has been developed over time and transformed into different versions and these versions have been effectively applied to many decision problems. They have also been merged with various multi-criteria decision-making (MCDM) methods ([5,6,7,8,9,10,11]). One of these extensions is Pythagorean fuzzy sets. Pythagorean fuzzy sets, first proposed by Yager in 2014, are a new extension of intuitionistic fuzzy sets. These sets inherit the durability feature of intuitionistic fuzzy sets. They do not only depict the imprecise and ambiguous information that intuitionistic fuzzy set can capture, but they can also model the more complex uncertainty in practical situations, which the latter cannot identify. An extended version of Pythagorean fuzzy sets is IVPFSs which this study selects as a methodology to handle ambiguous information [12,13,14,15]. IVPFSs allow membership and non-membership degrees to a specific set to have a range value. Therefore, they have wider application potential due to their ability to handle strong uncertainty in the decision-making process and can be used in this research to capture uncertain information in the prioritization of risks that emerged at hospitals in Covid-19 times. When the advantages of the TOPSIS method, which has been successfully applied to many crucial risk prioritization problems, are added to the aforementioned advantage of this special set (IVPFSs), an answer to the question of why the proposed approach is applied to this particular problem can emerged.
In the literature, many scholars have dealt with IVPFSs and applied it to various areas [12,13,14,15,16,17,18,19,20]. Garg [14], proposes an improved score function for solving MCDM problem with partially known weight information. In another study, new exponential operational laws and their aggregation operators for interval‐valued Pythagorean fuzzy multi-criteria decision‐making are described [15]. Moreover, a new improved accuracy function [12] and a new score function [13] for IVPFSs are developed. Recently, by Garg, linguistic IVPFSs concept is introduced and applied in MCDM domain [16]. In addition to the theoretical contributions of IVPFSs, there are some studies that implemented IVPFSs with TOPSIS. Yu et al. [11] developed a group decision-making sustainable supplier selection approach using extended TOPSIS under IVPFSs. Sajjad Ali Khan et al. [21] extended the TOPSIS under IVPFSs via Choquet integral. Ho et al. [22] proposed a Pearson-like correlation-based TOPSIS method with IVPFSs and applied it to multiple criteria decision analysis of stroke rehabilitation treatments. Ak and Gul [23] used integration of AHP-TOPSIS under IVPFSs for an information security risk analysis problem. Onar et al. [24] assessed cloud service providers by an IVPF-TOPSIS approach. Yucesan and Gul [25] used IVPF-TOPSIS as an auxiliary MCDM method in hospital service quality evaluation.
Considering the findings obtained from both IVPFSs and interval-valued Pythagoras IVPF-TOPSIS literature, this study contributes to the literature by the following aspects and differs from similar existed ones.
-
(1)
Theoretically, although there are many studies on IVPFSs, there are limited studies on IVPF-TOPSIS. Among these, ones that are adapted to real-life problems consist of the mentioned studies above. Therefore, this method (IVPF-TOPSIS) has been applied to the risk prioritization problem for the first time in the literature to capture the uncertainty information of decision-makers. In addition, the special case of Covid-19 increases its importance in terms of showing the originality of the study and the applicability of such methods in the field of public health.
-
(2)
Secondly, to the problem of prioritizing risks, a GRA-TOPSIS integrated approach based on IVPFSs as in Yu et al. [11] has been applied. The distance and similarity between the alternatives are evaluated at the same time, which makes the ranking results more solid.
-
(3)
Thirdly, a comparative analysis with other existing IVPF-TOPSIS approaches is performed to provide its validity.
3 Situation Analysis of Turkey’s Covid-19 Pandemic
This disease first appeared on December 30, 2019, in Wuhan, China [26]. In nearly 6 months, the infection, which first expanded to Iran and Italy, is spread all over the world. The world is faced with the demand for infected patients who apply to hospital emergency units heavily and irregularly. As of July 4, 2020, it has caused nearly 11,2 million cases and 529,882 deaths in the world [3]. The symptoms of Covid-19 are not specific, and they can range from no symptoms (asymptomatic) to severe pneumonia and death. According to the figures of the report “Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (Covid-19)”, typical signs and symptoms are expressed such as fever, dry cough, fatigue, sputum production, shortness of breath, sore throat, and headache[27].
As of June 28, 2020, similar to the fights of countries against this pandemic throughout the world, Turkey continues its struggle. After the first Covid-19 cases in Turkey were notified on March 11, 2020, higher than 3 million tests were performed in total. Between 1 and 28 June, nearly 1,2 million tests were performed. In total, 198,284 laboratory-confirmed Covid-19 cases and 5,097 deaths due to Covid-19 have been reported in Turkey. The total number of hospitalizations was 105,416 and 5,773 patients were hospitalized between 22 and 28 June. The recovery rate and death rate of all confirmed cases were 86.04% and 2.57%, respectively [28]. All these statistical figures show that Turkey is at a better level than the world average. This is related to Turkey's early isolation decisions and as well as the case of being prepared for such an event. Therefore, hospitals are required to prepare for such pandemics.
4 Applied Methodology
Traditionally, it is assumed that the information obtained when making assessments is known as crisp numbers [14, 15]. Moreover, MCDM-based models merged with fuzzy extensions are frequently applied to occupational risk assessment problems in hospitals [29, 30]. However, the use of MCDM in prioritization problems (such as risk prioritization) along the area of public health or the emerging of Covid-19 pandemic is a new platform to make research [31,32,33]. Therefore, the current study aims to remedy the gap in this respect. This will help hospital decision-makers and national policymakers in making hospitals ready for such outbreaks. The proposed method is presented in Fig. 1. Also, the calculation details are discussed in Sect. 4.
In the applied methodology, the uncertain information of decision-makers is considered in IVPFSs. Weights of decision-makers and criteria are determined in the way of Yu et al. [11]. Then, hazards that emerged due to Covid-19 pandemic at hospitals are evaluated by the grey correlation analysis (GRA) and TOPSIS integrated method [11].
4.1 Preliminaries
In this section, we provide some definitions, notions, and formulae regarding IVPFSs.
Definition 1
Let X be a universe of discourse. A Pythagorean fuzzy set P is an object having the form [11,12,13,14,15]:
where \(\mu_{P} (x):X \mapsto [0,1]\) defines the degree of membership and \(v_{P} (x):X \mapsto [0,\,1][0, 1]\) defines the degree of non-membership of the element \(x \in X\) to P, respectively, and, for every \(x \in X\), it holds:
For any P and \(x \in X\), \(\pi_{P} (x) = \sqrt {1 - \mu^{2}_{P} (x) - v^{2}_{P} (x)}\) is called the degree of indeterminacy of x to P.
Definition 2
Let \(\beta_{1} = P(\mu_{{\beta_{1} }} ,v_{{\beta_{1} }} )\) and \(\beta_{2} = P(\mu_{{\beta_{2} }} ,v_{{\beta_{2} }} )\) be two Pythagorean fuzzy numbers in a simple demonstration then the following operations are defined ([34,35,36,37]):
Definition 3
An IVPFS \({\tilde{P }}_{i}\) of the universe of discourse \(U\) is depicted as follows [38]:
\({\tilde{P }}_{i}=\left\{u, {([\mu }_{{\tilde{P }}_{i}}^{L}\left(u\right),{\mu }_{{\tilde{P }}_{i}}^{U}\left(u\right)], {[v}_{{P}_{i}}^{L}\left(u\right),{v}_{{P}_{i}}^{U}\left(u\right)]|u\epsilon U\right\}\) where \(0\le {\left({\mu }_{{\tilde{P }}_{i}}^{U}\left(u\right)\right)}^{2}+{\left({v}_{{\tilde{P }}_{i}}^{U}\left(u\right)\right)}^{2}\le 1\)
Definition 4:
An intuitionistic entropy of Pythagorean fuzzy set is computed via Eq. (6) [39].
4.2 Procedural Steps of the Proposed IVPF-TOPSIS-based Approach
First, experts should determine the status of risks in the decision-making process [40]. For an MCDM problem, a decision matrix is required to construct the decision-making process. Since, the problem that this study has dealt with a risk prioritization, we have designed the decision matrix whose elements include the values of all alternatives with respect to each criterion under IVPFSs.
Let \(CR=\left\{{cv}_{1},{cv}_{2},\dots ,{cv}_{m}\right\} m\ge 2\) be a set of alternatives (for this study “Covid-19 risk”), \(RP=\left\{{rp}_{1},{rp}_{2},\dots ,{rp}_{n}\right\}\) be a set of criteria set (for this study “risk parameter”), \(w=\left\{{w}_{1},{w}_{2},\dots ,{w}_{n}\right\}\) be a set of criteria weights for this study “risk parameter weight”) that satisfy the conditions of \(0\le {w}_{j}\le 1\) and \({\sum }_{j=1}^{n}{w}_{j}=1\), and \(DM=\left\{{dm}_{1},{dm}_{2},\dots ,{dm}_{h}\right\}\) be a set of decision-makers’ weights for this study “decision-maker (expert) weight”). Also, while \(\lambda =({\lambda }_{1},{\lambda }_{2},\dots ,{\lambda }_{h})\) refers to the optimism degree of experts, \(\eta =({\eta }_{1},{\eta }_{2},\dots .,{\eta }_{h})\) shows the relative weights of experts satisfying \({\sum }_{k=1}^{h}{\eta }_{k}=1\). The procedural steps of our proposed IVPF-TOPSIS-based risk prioritization approach are as follows:
Step 1: This step handles the construction of the decision matrix. In determining the ratings of decision-makers regarding alternatives with respect to the criteria, the IVPFSs-based linguistic scale given in Table 1 is used. Here, k refers to the indices for decision-makers.
Step 2: In this step, expected Pythagorean fuzzy decision matrix of the decision-makers is calculated using the optimism degree \(\lambda\).
Step 3: The group aggregated decision matrix based on all experts’ expected decision matrices by Eq. (9).
Step 4: This step is about weight calculation of risk parameters using entropy measure of each parameter as in Eq. (10)
Also, a divergence is introduced in Eq. (11) and normalized risk parameter weights are computed as in Eq. (12).
Step 5: Positive ideal solution (PIS) and negative ideal solution (NIS) are determined using Eqs. (13)–(14).
where \({{\mu }_{j}}^{+}=max\left\{{\mu }_{ij}\right\}, {{v}_{j}}^{+}=min\left\{{v}_{ij}\right\}, {{\mu }_{j}}^{-}=min\left\{{\mu }_{ij}\right\}, {{v}_{j}}^{-}=max\left\{{v}_{ij}\right\}\),
Step 6: This step concerns with computation of distance values and weighted distance values from PIS and NIS. The required equations are provided in Eqs. (15)–(18).
Step 7: According to the study of Yu et al. [11], grey relational analysis is merged into TOPSIS. The grey relational coefficients and grades are computed as Eqs. (19)–(22), respectively.
Step 8: In this step, the integrated value of distance and grey relational grade is computed as in Eqs. (23)–(24).
Here \(\alpha + \beta =1\). Generally, they are set to 0.5. \({{int}_{i}}^{+}\) and \({{int}_{i}}^{-}\) refer to the closeness of the ith Covid-19 risk to PIS and NIS.
Step 9: The optimized ideal reference point is calculated as in Eq. (25).
Step 10: In this step, the distance from each Covid-19 risk to point R is computed as in Eq. (26).
Step 11: The final step is about prioritizing Covid-19 risks’ \({CC}_{i}\) values in increasing order and obtaining the final priorities.
5 Case Study: Prioritization of the Risks Emerged at Hospitals During the Covid-19 Pandemic
In this section, a case study for the applied methodology is carried out to prioritize the risks that emerged at hospitals during Covid-19 pandemic. For this aim, twenty-one Covid-19 risks are determined benefiting from the experience of the decision-makers who participated in this study at two different hospitals. These hospitals are state hospitals situated in the Black Sea region of Turkey and face a great number of Covid-19 cases till March 2020. The first expert is an academician who studies mathematical modeling of Covid-19 spreading, MCDM, and fuzzy logic modeling. The second and third experts are working in these hospitals as “assistant hospital manager”. Regarding the risk list, three different pillars are considered as hospital (indicated as an abbreviation of “Hospital risk: HR”), patient & staff (indicated as an abbreviation of “Patient & staff risk: PSR”) and healthcare (indicated as an abbreviation of “Care risk: CR”). Six hospital risks, nine patient & staff risks, and six care risks are identified as in Table 2. The risk parameters are determined as severity, occurrence, and detection which is used as the parameters of a classical failure mode and effect analysis. The twenty-one Covid-19 risks are assessed with respect to these three risk parameters considering the weights of risk parameters, decision-makers, and optimism degree of decision-makers. For this respect, we obtain weights of risk parameters using entropy measures as follows:
\({w}_{j}=\left(0.386, 0.315, 0.299\right), j=severity, occurrence, detection\). Weights of decision-makers are assumed as \(\eta =\left({\eta }_{1},{\eta }_{2},{\eta }_{3}\right)=(0.4, 0.3, 0.3)\). Finally, the optimism degrees of decision-makers are considered as \(\lambda =\left({\lambda }_{1},{\lambda }_{2},{\lambda }_{3}\right)=(0.5, 0.5, 0.5)\) which are all equal.
By completing the requirements for the computational procedural steps of the proposed approach, the following step-by-step operations is performed to find the priorities of the emerged Covid-19-related risks at the hospital sites.
In the first step, following linguistic terms and their corresponding IVPFSs shown in Table 1, the decision matrix assessed by each expert is constructed. Then, the expected decision matrix for each expert is calculated by Eqs. (7) and (8). In the third step of the approach, the group aggregated decision matrix is computed by Eq. (9) and provided in Table 3.
In the fourth step of the proposed approach, we obtained the weight of risk parameters using entropy measure of each parameter using Eqs. (10), (11), and (12). In the fifth step, PIS and NIS values are computed using Eqs. (13) and (14) as in Table 4.
In the sixth step, the weighted distances from each Covid-19 risk to the PIS and the NIS are computed using Eqs. (15)–(18). Then, the grey relational grades are calculated as the seventh step procedures using Eqs. (19)–(22). In the eighth step, the integrated value of distance and grey relational grade is calculated by Eqs. (23)–(24). The computation results are given in Table 5.
In the ninth step, the optimized ideal reference point G is obtained as (0.524, 0.081). Then, the distance from each Covid-19 risk to point G is computed using Eq. (26). The final \({CC}_{i}\) results are given in Fig. 2. Considering the ranking of each Covid-19 risks (by \({CC}_{i}\) values in increasing order), the PSR2 (Risk arising from non-following the personal hygiene rules) is determined as the most crucial risk-related Covid-19 at hospital sites.
As a result of the calculations, PSR2 was determined as the highest risk. Republic of Turkey Ministry of Health has identified the implementation of personal hygiene as an important criterion following the criterion of “usage of masks” in the fight against Covid-19. Although this risk has a high impact on the spread of the virus, it is very difficult to determine whether personal hygiene rules are followed. For this reason, brochures and instructions reminding the personal hygiene rules were placed in the visible places of the hospital. The second most important risk was identified as PSR8. The detectability of this risk is relatively easy. But if action is not taken, it can cause devastating effects. For this reason, Covid-19 suspects are accepted to carry viruses from the moment they enter the hospital. The tomography and other diagnostic devices used in the diagnosis of the disease are disinfected after each use. The third most important risk has been identified as PSR9 medical staff in Turkey as in other countries were affected by the virus. Some measures have been taken to prevent the spread of the virus to medical staff. State-owned guesthouses were made free of charge to healthcare professionals and they were encouraged to reside there. The fourth most important risk has been identified as HR6. Healthcare professionals are closer than 20 cm to take a swab sample, which makes the virus spread possible. In this context, some measures have been taken by the hospitals. Cabins were ordered to prevent contact with medical staff and patients. These cabins are located in areas where there are fewer patients and healthcare professionals. The fifth most important risk has been identified as PSR1. In order to prevent Covid-19 transmission in healthcare professionals, N95 type masks with high protection were provided. Necessary information was provided by announcing the instructions for the use of protective equipment determined by the Ministry of Health to medical staff. The sixth most important risk was identified as PSR4. Patients who needed regular care and treatment during the fight against Covid-19 were adversely affected. For this reason, “clean hospitals ”were determined for each region, and there was no Covid-19 patient in those hospitals, and it was served to combat regular diseases. The seventh most important risk has been identified as HR5. In order to provide social isolation, serious changes have been made especially in emergency departments. Covid-19 suspects were separated from the patients who would receive other emergency services and the two groups were prevented from contacting each other.
5.1 Comparative Study
To compare the performance of our approach in this case with other similar IVPF-TOPSIS approaches, we conducted a comparative study. In this study, the results of our current study (final TOPSIS scores and risk rankings) were compared with the analysis results obtained by applying IVPF-TOPSIS of Garg [13] to our case which uses a modified score function. The results obtained are summarized in Table 6.
In applying Garg’s IVPF-TOPSIS to our data, we used interval-valued Pythagorean fuzzy weighted average operator (IVPFWAO) of Peng and Yang [41] in aggregating evaluation of each three decision-maker. The weights of decision-makers and weights of three risk parameters are set to the same in the current approach. Figure 3 presents the comparison of the results obtained from the current approach with the results we obtained by applying Garg [13]. Therefore, it was concluded from Fig. 3 that the results calculated by the approach taken from the literature coincide with the results of the proposed approach. The correlation test for final scores and risk rankings also supports this result. The Spearman's Rank Correlation Coefficient (Rho) gives a value of 0.819 (approximately 82%) for both method ranking order results. Also, the Pearson correlation analysis is performed in final IVPF-TOPSIS results of both approaches and value of -0.753 (approximately 75%) is obtained. The negative and higher value shows a strong and inverse relationship between the results. In our proposed approach, a lower final CCi value is desired unlike in Garg’s IVPF-TOPSIS CCi value. In Garg’s approach, a higher CCi is desired. This is why we obtained a negative correlation coefficient.
6 Conclusion
The quality and continuity of hospital services play an important role in reducing the social and economic impacts of the pandemic on countries. In many countries, the health system is not ready for a pandemic. Moreover, the system is locked and there is a serious weakness both in the fight against pandemic and in routine health services. In this context, in order to ensure the continuity of hospital services and to increase the quality of service, the risks that may arise in hospitals, especially during the pandemic period, were identified and preventive actions were taken for high-priority risks.
The time of the pandemic and the risks in the hospital during regular times differ from each other. In this study, risks that may arise in the hospital are arranged by considering pandemic conditions. In the light of the evaluations, the most important risks were identified, and preventive measures were presented. During the pandemic, it may be necessary to change the infrastructure, revise the processes, differentiate the measures, and reorganize the personnel management. In addition, the interests and concerns of healthcare personnel and patients differ during these periods. When all these factors are considered, while preventing the detected risks improves the quality of health care; It will be a helpful element in the decision-making mechanisms of hospital management. It is not enough to evaluate only one hospital to be able to analyze pandemic situation. The authors will conduct a risk analysis of all hospitals in the region in future studies. In addition, it is planned to integrate the discrete event simulation with the risk analysis for hospitals. Thus, the effects of the preventive measures can be determined and how hospitals can serve in pandemics and natural disasters can be tested with different scenarios. This information will assist decision-makers on which regional hospitals can be declared “pandemic hospitals”.
References
Haghani M, Bliemer MC, Goerlandt F, Li J (2020) The scientific literature on coronaviruses, COVID-19 and its associated safety-related research dimensions: a scientometric analysis and scoping review. Saf Sci 104806
Singer DR (2020) A new pandemic out of China: the Wuhan 2019-nCoV coronavirus syndrome. Health Policy Technol 9(1):1
World Health Organization (2020) Coronavirus disease 2019 (COVID-19) Situation Report–93. Accessed from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200422-sitrep-93-covid-19.pdf?sfvrsn=35cf80d7_4
Zadeh L (1965) Fuzzy sets. Information and Control, 8(3):338–356
Yanmaz O, Turgut Y, Can EN, Kahraman C (2020) Interval-valued Pythagorean Fuzzy EDAS method: an application to car selection problem. J Intell Fuzzy Syst (Preprint), 1–17
Biswas A, Sarkar B (2019) Interval-valued Pythagorean fuzzy TODIM approach through point operator-based similarity measures for multicriteria group decision making. Kybernetes
Gul M, Ak MF, Guneri AF (2019) Pythagorean fuzzy VIKOR-based approach for safety risk assessment in mine industry. J Saf Res 69:135–153
Haktanır E, Kahraman C (2019) A novel interval-valued Pythagorean fuzzy QFD method and its application to solar photovoltaic technology development. Comput Ind Eng 132:361–372
Ilbahar E, Kahraman C (2018) Retail store performance measurement using a novel interval-valued Pythagorean fuzzy WASPAS method. J Intell Fuzzy Syst 35(3):3835–3846
Liang D, Darko AP, Zeng J (2019) Interval-valued pythagorean fuzzy power average-based MULTIMOORA method for multi-criteria decision-making. J Exp Theor Artif Intell 1–30
Yu C, Shao Y, Wang K, Zhang L (2019) A group decision making sustainable supplier selection approach using extended TOPSIS under interval-valued Pythagorean fuzzy environment. Expert Syst Appl 121:1–17
Garg H (2017) A novel improved accuracy function for interval valued Pythagorean fuzzy sets and its applications in the decision-making process. Int J Intell Syst 32(12):1247–1260
Garg H (2017) A new improved score function of an interval-valued Pythagorean fuzzy set based TOPSIS method. Int J Uncertain Quantif 7(5):463–474
Garg H (2018) A linear programming method based on an improved score function for interval-valued Pythagorean fuzzy numbers and its application to decision-making. Int J Uncertain Fuzziness Knowl Based Syst 26(01):67–80
Garg H (2018) New exponential operational laws and their aggregation operators for interval-valued Pythagorean fuzzy multicriteria decision-making. Int J Intell Syst 33(3):653–683
Garg H (2020) Linguistic interval-valued Pythagorean fuzzy sets and their application to multiple attribute group decision-making process, Cognit Comput. https://doi.org/10.1007/s12559-020-09750-4
Liu Y, Qin Y, Han Y (2018) Multiple criteria decision making with probabilities in interval-valued Pythagorean fuzzy setting. Int J Fuzzy Syst 20(2):558–571
Peng X (2019) New operations for interval-valued Pythagorean fuzzy set. Sci Iran Trans E Ind Eng 26(2), 1049–1076
Rahman K, Abdullah S (2019) Generalized interval-valued Pythagorean fuzzy aggregation operators and their application to group decision-making. Granul Comput 4(1):15–25
Rahman K, Abdullah S, Ali A (2019) Some induced aggregation operators based on interval-valued Pythagorean fuzzy numbers. Granul Comput 4(1):53–62
Sajjad Ali Khan M, Abdullah S, Yousaf Ali M, Hussain I, Farooq M (2018) Extension of TOPSIS method base on Choquet integral under interval-valued Pythagorean fuzzy environment. J Intell Fuzzy Syst 34(1), 267–282
Ho LH, Lin YL, Chen TY (2020) A Pearson-like correlation-based TOPSIS method with interval-valued Pythagorean fuzzy uncertainty and its application to multiple criteria decision analysis of stroke rehabilitation treatments. Neural Comput Appl 32(12):8265–8295
Ak MF, Gul M (2019) AHP–TOPSIS integration extended with Pythagorean fuzzy sets for information security risk analysis. Complex Intell Syst 5(2):113–126
Onar SC, Oztaysi B, Kahraman C (2018) Multicriteria evaluation of cloud service providers using Pythagorean fuzzy TOPSIS. J Mult Valued Logic Soft Comput 30
Yucesan M, Gul M (2020) Hospital service quality evaluation: an integrated model based on Pythagorean fuzzy AHP and fuzzy TOPSIS. Soft Comput 24(5):3237–3255
Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD (2020) How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet 395(10228):931–934
World Health Organization (2020) Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). Accessed from https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
Ministry of Health of the Republic of Turkey (2020) Covid-19 current situation in Turkey. Accessed from https://covid19.saglik.gov.tr, https://dosyamerkez.saglik.gov.tr/Eklenti/37743,covid-19-situation-report-v4pdf.pdf?0
Gul M (2018) A review of occupational health and safety risk assessment approaches based on multi-criteria decision-making methods and their fuzzy versions. Human Ecol Risk Assess Int J 24(7):1723–1760
Gul M, Ak MF, Guneri AF (2017) Occupational health and safety risk assessment in hospitals: a case study using two-stage fuzzy multi-criteria approach. Human Ecol Risk Assess Int J 23(2):187–202
Koh D (2020) Occupational risks for COVID-19 infection. Occup Med (Oxford, England) 70(1):3
Ocampo L, Yamagishi K (2020) Modeling the lockdown relaxation protocols of the Philippine government in response to the COVID-19 pandemic: An intuitionistic fuzzy DEMATEL analysis. Socio-Econ Plan Sci 100911
Wong J, Goh QY, Tan Z, Lie SA, Tay YC, Ng SY, Soh CR (2020) Preparing for a COVID-19 pandemic: a review of operating room outbreak response measures in a large tertiary hospital in Singapore. Can J Anesth/J Can d'anesthésie 1–14
Liang D, Xu Z (2017) The new extension of TOPSIS method for multiple criteria decision making with hesitant Pythagorean fuzzy sets. Appl Soft Comput 60:167–179
Zeng S, Chen J, Li X (2016) A hybrid method for pythagorean fuzzy multiple-criteria decision making. Int J Inf Technol Decis Mak 15(02):403–422
Zhang X, Xu Z (2014) Extension of TOPSIS to multiple criteria decision making with Pythagorean fuzzy sets. Int J Intell Syst 29(12):1061–1078
Yager RR (2014) Pythagorean membership grades in multicriteria decision making. IEEE Trans Fuzzy Syst 22(4):958–965
Garg H (2016) A novel accuracy function under interval-valued Pythagorean fuzzy environment for solving multicriteria decision making problem. J Intell Fuzzy Syst 31(1):529–540
Dharmarajan R (2017) An intuitionistic fuzzy TOPSIS DSS model with weight determining methods. Int J Eng Comput Sci 6:20354–20361
Garg H, Kaur G (2020) Quantifying gesture information in brain hemorrhage patients using probabilistic dual hesitant fuzzy sets with unknown probability information. Comput Ind Eng 140:106211
Peng X, Yang Y (2016) Fundamental properties of interval-valued Pythagorean fuzzy aggregation operators. Int J Intell Syst 31(5):444–487
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Gul, M., Yucesan, M. (2021). A Risk Prioritization Method Based on Interval-Valued Pythagorean Fuzzy TOPSIS and Its Application for Prioritization of the Risks Emerged at Hospitals During the Covid-19 Pandemic. In: Garg, H. (eds) Pythagorean Fuzzy Sets. Springer, Singapore. https://doi.org/10.1007/978-981-16-1989-2_6
Download citation
DOI: https://doi.org/10.1007/978-981-16-1989-2_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-1988-5
Online ISBN: 978-981-16-1989-2
eBook Packages: Mathematics and StatisticsMathematics and Statistics (R0)