Abstract
Antimicrobial behavior in suture materials is a desirable feature that can potentially improve the healing process by inhibiting microbial growth. In this article, we demonstrate a method for the development of antimicrobial polyethylene terephthalate based sutures by plasma functionalization, followed by the immobilization of triclosan (as bioactive agent). The surface functionalization was observed by investigating carboxyl content with varying plasma exposure time. Mechanical strength, surface topography, and morphology were analyzed on these sutures. The homogeneous distribution of triclosan in suture was observed by energy dispersive X-ray analysis. Antimicrobial studies suggest that resulting PET sutures have excellent bacteriostatic and bactericidal properties against S. aureus and E. coli. Our study suggests that developed sutures can inhibit bacterial adherence and colonization on the surgical site and appears to be a promising material for surgical applications.
Access provided by CONRICYT-eBooks. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Smart wound care requires materials which provide scar free optimum healing without any risk of surgical site infection (SSI). Wound closure requires postoperative suturing of a tissue which leaves behind the strong possibility of infection migration through the suture site [1]. Moreover, if the wound is infectious, bacteria may colonize on the suture surface and may lead to serious complications. The investigation of the infection is certainly related to the nature and origin of the suture. This would influence the bacterial adhesion and its transmittance into the wound. The magnitude of the infection is related to the nature and the origin of the suture which would influence the bacterial adhesion, its colonization, and penetration into the tissue. The infection may sometimes grow to such an extent that it may cause septicemia as well [2]. Almost 23% of SSI are due to the colonization leading to significantly high healthcare expenses.
Efforts are being made to develop sutures which are inherently antimicrobial in nature and do not allow bacterial adhesion or invasion by virtue of the bacteriostatic or bactericidal nature against different microbes [3]. The ideal situation would be to have a suture which is antimicrobial in nature and does not allow any infection to grow in its vicinity leading to a healthy tissue growth. Ethicon has developed poly(lactic-co-glycolic acid) suture which is marketed as Vicryl+ and is effective against a large number of microbes. This invention led to a large number of people entering into the suture technology where infection resistance against different bacteria may be achieved [4]. Both the biostable and biodegradable sutures are being investigated for creating the structure that would offer required features in a surgical kit for wound healing systems [5].
Immobilization of the biomolecules on suture surface is an essential aspect to create or generate antimicrobial nature. The important requirement is the surface should be bioreceptive in nature so that biomolecules may be anchored on the surface [6]. One of the obvious approaches may be to coat the suture surface by a bioactive component. However, this needs the suture surface to be bioreceptive so that it may bind with the biomolecule in such a way that it acts against microbes in an effective manner. After surface functionalization and bioimmobilization of bioactive agent on the suture material, the suture must retain its biocompatibility during in vivo application [7]. The nature of the bioactive agent is a prominent factor determining the effectiveness of the suture against microbes. A large number of bioactive moieties exist which show antimicrobial nature. Triclosan, 2,4,4′-trichloro-2-hydroxydiphenylether is the effective antimicrobial and also possesses antifungal and antiviral properties. This has shown a very effective nature in Vicryl+. However, due to ubiquitous situation, researches are trying to get an effective alternative to triclosan [8, 9].
2 Experimental
2.1 Materials
Polyethylene terephthalate (PET) chips used in this study were supplied by Reliance Industries Ltd., India. Triclosan was purchased from Sigma Aldrich. Toluidine Blue O (TBO) (Qualigens, India), glutaraldehyde, sodium hydroxide, and acetic acid from Merck, India were used. Luria broth and agar-agar were obtained from Hi Media Laboratories, India. Bacterial strains of S. aureus and E. coli were provided by IIT Delhi. All chemicals were of analytical grade and used without further purification. Carbon dioxide gas cylinders of high purity were procured from a local supplier.
2.2 Development of PET Monofilament
Initially, PET chips were vacuum dried for 24 h at 70 °C, then dried chips were fed through the hopper and melt spun at 270 °C to obtain undrawn filaments. These extruded filaments passed through a water bath at 4 °C and were collected by a take-up winder at 30 m/min. Further, undrawn filaments were drawn on a two-stage drawing machine (Cybertex) to different draw ratios at 120 °C, respectively [7]. Drawn PET filament at a draw ratio of 2.5 had a thickness of 235 µm was used for further experiments.
2.3 Plasma Functionalization of PET Monofilament
PET monofilaments were plasma treated with carbon dioxide plasma in a capacitively coupled RF reactor operating at 13.6 MHz. The monofilament was mounted over a sample holder and rotated at 40 rpm by a motor for homogeneous exposure of plasma. The cylindrical vessel was first evacuated to 10−5 Torr and then carbon dioxide gas was purged introduced under the control of mass flow controller. Variables for plasma treatment were exposure time (0–180 s), gas pressure of 100 mTorr, and discharge power 40 W [7].
2.4 Determination of Carboxyl Content
The carboxyl content from the filament surface was determined by colorimetric method with TBO (toluidine blue O) staining, as reported in the literature [10]. Basic solution of TBO dye was prepared and the plasma exposed filament was placed in this solution for 6 h at room temperature. The filament was subsequently removed and washed with sodium hydroxide solution to remove noncomplexed dye adhering on the filament surface. The dye was desorbed from the filament in 50% acetic acid solution and the optical density of the solution was measured by using a UV–Visible spectrophotometer (Perkin Elmer Lambda E Z 201) at 623 nm. The carboxyl content was obtained from the calibration plot of the optical density versus dye concentration with the assumption of 1:1 ratio between the dye and the carboxyl groups.
2.5 Triclosan Immobilization on the Functionalized PET Filament
The plasma exposed PET monofilament was then immediately dipped into triclosan solution. The generated carboxyl groups were interacted with active sites of bioactive agents and hence get attached to the filament surface. Plasma exposed samples were dipped into 1% solution of triclosan in water and ethanol phase. Treated samples were gently washed with water to remove unreacted material and dried at room temperature (henceforth called as suture).
2.6 Energy Dispersive X-ray Analysis (EDX)
The elemental analysis of pristine, triclosan immobilized PET suture was monitored by EDX analysis. The samples were placed on an aluminum stub and coated with carbon using Auto-Fine Coater JFC-1600 (Joel, USA Inc., USA). The images and the elemental quantification of the samples were obtained with RONTEC’s EDX Model QuanTax 200 (SDD technology, USA).
2.7 Mechanical Studies of PET Suture
Mechanical properties of the virgin, plasma exposed, and triclosan immobilized PET sutures were performed on tensile tester, Instron model 4301. Mechanical properties of the samples were observed with a crosshead speed of 50 mm/min and gauge length of 50 mm in ambient conditions of 27 ± 2 °C and 65% ± 2% relative humidity. Tensile strength and elongation are obtained from the stress–strain curves which are an average for 10 specimens [10].
2.8 Surface Topography of PET Suture
Surface topographical information of samples was obtained in air at room temperature by Solver Pro SPM (NT–MDT, Russia) atomic force microscopy (AFM) in semi-contact mode with NSG 10 series tips. Scanning size of each image was kept 2.5 µ × 2.5 µ and scanning rate of 1 Hz was used. Five to ten different locations were analyzed on each sample.
2.9 Antimicrobial Study
Antibacterial study of suture was carried out by colony reduction method against E. coli and S. aureus [11, 12]. Fresh cultured bacterial colonies were suspended in Luria Broth with turbidity of 0.5 McFarland standards. The suture samples (~20 mg) were placed in 6 mL bacterial suspension in Luria Broth having 106 CFU mL−1. All suspensions of bacteria in broth were vortexed and incubated at 37 °C for 24 h. The inoculum (200 μL) was uniformly spread on nutrient agar plate using a sterile L-shape spreader. Plates were incubated at 37 °C and the colonies were counted after 24 h.
Bacterial adherence on suture surface was observed by field emission scanning electron microscope (FEI Quanta 200F, Netherlands) with gold coating. Each suture sample was inoculated in freshly prepared suspension consisting of 1 mL of bacterial colonies and 3 mL of Luria broth. Suture samples were cultured for 24 h overnight incubation at 37 °C, 95% air/5% CO2. Suture samples were rinsed with sterile water to remove non-adherent bacteria from the surface. Subsequently, suture samples were transferred to a sterile glass tube using sterile forcep, containing 3 mL of 2.5% glutaraldehyde solution for 24 h for the fixation of the substratum for FE-SEM analysis. Excess glutaraldehyde was removed by gentle rinses with sterile water and then serially dehydrated in ethanol than mounted on metal stubs, and sputter coated with gold [13].
3 Results and Discussion
3.1 Plasma Functionalization
The designing of an antimicrobial suture is extremely careful approach where the right choice of the material and the antimicrobial processing need to be integrated so that material retains it biocompatibility and inherent physical features during its application. The processing however involves the functionalization and the immobilization of a bioactive agent to the suture surface. The functionalization route itself may be executed depending on the nature of the suture material. PET suture may be functionalized by plasma processing. It is interesting to see that desired functional groups are created by proper selection of the carrier gas in the plasma system. While ammonia creates amino groups, CO2 leads to the formation of the carboxyl functionality. However, oxygen creates hydroxyl as well as peroxide functionality on the suture surface (Fig. 1).
The peroxide may be subsequently used to initiate a graft polymerization process so that a high level of functional groups is achieved. The beauty of plasma activation is that it creates specific functional groups on the surface without any impact on the bulk properties and has been demonstrated to be an effective approach towards developing antimicrobial surgical implants [14]. This approach has been used to develop PET sutures with effective control over microbial infection. The functionalization in fact requires a very short exposure of few seconds leading to the activation confined to the nanoscale on the surface.
The variation of carboxyl content with plasma exposure time is shown in Fig. 2. It is evident that from 2 to 180 s plasma exposure time, the carboxyl content value increases with the increase in plasma exposure time. The increase in carboxyl content is achieved due to an increase in the number of active sites, resulting from increases in plasma exposure time. The presence of readily active carboxyl groups on the PET suture surface is allowed to the subsequent immobilization of biofunctional molecules such as triclosan on the PET suture surface (Fig. 3).
3.2 Characterizations
The tensile strength of PET suture after plasma functionalization is presented in Fig. 4. Initially, PET suture has tensile strength of 393 MPa while after plasma treatment this value increases as plasma time is increased.
At 120 s of plasma treatment, the tensile strength value reaches to 416 MPa after 120 s of plasma and this value does not show any relevant change. The tensile strength value of triclosan immobilized PET suture is almost similar to plasma functionalized suture because immobilization of triclosan has not altered the bulk property of the material.
The elemental analysis of pristine and triclosan immobilized samples was carried out by EDX analysis and presented in Fig. 5. The EDX spectrum of pristine PET suture (Fig. 5a) shows a distinctive energy peak at around 0.2 keV, characteristic peaks of carbon and oxygen with total content of O and C with 43.9, and 54.8% respectively. In PET-triclosan suture along with characteristic peaks, one new strong peak appears at ~2.5 keV, which confirmed the presence of chlorine (Fig. 5b). Furthermore, the EDX pattern of the material was found to be Cl, O, and C with 3.2, 48.7, and 47.2%, respectively.
Surface topography of the pristine, plasma functionalized, and triclosan immobilized PET suture were studied by AFM and depicted in Fig. 6. AFM image of pristine PET suture shows relatively flat and homogeneous surface, having Sq of 6.27 ± 4.7 nm with the presence of fibrils in the direction of filament long axis (Fig. 6a).
The aspect of the statistical distribution of z-values within the image confirmed that the suture surface was uniform. After plasma functionalization, the PET suture surface shows hill valley structure with significant nonhomogeneity where surface started filling up with small conical protrusions. Further, these conical protrusions converted into nano hills and valley structure (Fig. 6b). After triclosan immobilization, the surface topography did not show any appreciable change as compared to the plasma exposed sample because triclosan is single molecule which can be placed in between the small conical protrusions. Surface roughness of triclosan immobilized sample was Sq of 12 ± 5.7 nm which is very much identical to the plasma exposed sample (Fig. 6c).
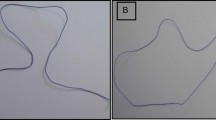
3.3 Bacterial Adherence on PET Suture
Bacterial adherence on suture samples was investigated by FE-SEM analysis and images are shown in Fig. 7. In bacterial adherence study, the results are evaluated after 24 h of incubation of suture samples and observe the biofilm formation. Regarding the adherence of S. aureus and E. coli onto the samples, drastic change is observed in the number of viable colonies adhered onto the surface of triclosan immobilized sample as compared to the pristine PET sample implying the efficiency of the modifications in reducing the adherence of bacteria onto the surface. Bacterial adhesion on suture samples might assist the infection on site and impaired wound healing so to overcome this issue, here we used triclosan as an antimicrobial agent. Triclosan is found to be effective against a broad range of microbes with documented safety along with both bactericidal as well as bacteriostatic property, depending on its concentration. Therefore, triclosan immobilized suture samples did not allow any bacterial growth on the surface and help in infection control.
The antibacterial activity of suture was evaluated against S. aureus and E. coli by colony formation methods and result shown in Fig. 8. It is seen that the triclosan immobilized PET suture has high antibacterial activity as evidenced by maximum reduction in the bacterial growth. The antimicrobial action of triclosan involves inhibiting fatty acid synthesis that is necessary for building and reproducing cell membranes [15]. Triclosan binds to bacterial enoyl-acyl carrier protein reductase (ENR) enzyme which increases the enzyme’s affinity for nicotinamide adenine dinucleotide (NAD+).
This results in the formation of a stable, ternary complex of ENR-NAD+-triclosan, which is unable to participate in fatty acid synthesis. This way, triclosan permeabilizes the bacterial envelope which allows for leakage of components leading to cell death.
4 Conclusion
Infection during wound closure is a serious problem and needs a very precise approach to this problem. The proactive approach may be to design a suture that would exhibit antimicrobial nature and would be effective against all the microbes. Sutures, therefore, need to be biofunctionalized in such a way that they acquire antimicrobial nature but without any compromise over the physical properties and the biocompatibility. Plasma processing to create specific functionality and the immobilization of the bioactive component is an attractive approach to develop infection-resistant sutures. Triclosan used as bioactive moiety and exhibited excellent antibacterial activity at much lower concentration. Results of the antimicrobial studies explicitly prove that the material is effective against microbes and has bacteriostatic and bactericidal nature.
References
Masini, B.D., Stinner, D.J., Waterman, S.M., Wenke, J.C.: Bacterial adherence to suture materials. J. Surg. Educ. 68, 101–104 (2011). https://doi.org/10.1016/j.jsurg.2010.09.015
Tummapalli, M., Anjum, S., Kumari, S., Gupta, A., Gupta, B.: Antimicrobial surgical sutures: recent developments and strategies. Polym. Rev. 56, 607–630 (2016). https://doi.org/10.1080/15583724.2015.1119163
Li, Y., Kumar, K.N., Dabkowski, J.M., Corrigan, M., Scott, R.W., Nüsslein, K., Tew, G.N.: New bactericidal surgical suture coating. Langmuir 28, 12134–12139 (2012). https://doi.org/10.1021/la302732w
Marco, F., Vallez, R., Gonzalez, P., Ortega, L., de la Lama, J.; Lopez-Duran, L.: Study of the efficacy of coated vicryl plus antibacterial suture in an animal model of orthopedic surgery. Surg. Infect. (Larchmt) 8, 359–366 (2007). https://doi.org/10.1089/sur.2006.013
Bretcanu, O., Verne, E., Borello, L., Boccaccini, A.R.: Bioactivity of degradable polymer sutures coated with bioactive glass. J. Mater. Sci. Mater. Med. 15, 893–899 (2004). https://doi.org/10.1023/b:jmsm.0000036277.99450.a2
Anjum, S., Gupta, A., Sharma, D., Dadal, P., Gupta, B.: Skin biocompatibility and infection-resistance in plasma functionalized nanogel coated polypropylene nonwoven fabric. Mater. Sci. Eng. C 69, 1043–1050 (2016). https://doi.org/10.1016/j.msec.2016.08.009
Anjum, S., Gupta, A., Sharma, D., Kumari, S., Sahariah, P., Bora, J., Bhan, S., Gupta, B.: Antimicrobial nature and healing behavior of plasma functionalized polyester suture. J. Bioact. Comp. Polym. 32, 263–279 (2017). https://doi.org/10.1177/0883911516668665
Galal, I., El-Hindawy, K.: Impact of using triclosan-antibacterial sutures on incidence of surgical site infection. Am. J. Surg. 202, 133–138 (2011). https://doi.org/10.1016/j.amjsurg.2010.06.011
Edmiston, C.E., Daoud, F.C., Leaper, D.: Is there an evidence-based argument for embracing an antimicrobial (triclosan)-coated suture technology to reduce the risk for surgical-site infections? A meta-analysis. Surgery 154, 89–100 (2013). https://doi.org/10.1016/j.surg.2013.03.008
Saxena, S., Ray, A.R., Gupta, B.: Graft polymerization of acrylic acid onto polypropylene monofilament by RF plasma. J. Appl. Polym. Sci. 116, 2884–2892 (2010). https://doi.org/10.1002/app.31823
Anjum, S., Gupta, A., Sharma, D., Gautam, D., Kapil, A., Sharma, A., Bhan, S., Gupta, B.: Development of novel wound care systems based on nanosilver nanohydrogels of polymethacrylic acid with aloe vera and curcumin, Mater. Sci. Eng. C 64, 157–166 (2016). https://doi.org/10.1016/j.msec.2016.03.069
Anjum, S., Arora, A., Alam, M.S., Gupta, B.: Development of antimicrobial and scar preventive chitosan hydrogel wound dressings. Int. J. Pharm. 508, 92–101 (2016). https://doi.org/10.1016/j.ijpharm.2016.05.013
Ahmad, A., Igor, N., Marián, L., Vladimir, S., Alenka, V., Ita, J., Petr, S., Ivan, C.: An in vitro bacterial adhesion assessment of surface-modified medical-grade PVC. Colloids Surf. B Biointerfaces 77, 246–256 (2010). https://doi.org/10.1016/j.colsurfb.2010.02.006
Lee, H.S., Park, S.H., Lee, J.H., Jeong, B.Y., Ahn, S.K., Choi, Y.M., Choi, D.J., Chang, J.H.: Antimicrobial and biodegradable PLGA medical sutures with natural grapefruit seed extracts. Mater. Lett. 95, 40–43 (2013). https://doi.org/10.1016/j.matlet.2012.12.090
Sadeghnejad, A., Aroujalian, A., Raisi, A., Fazel, S.: Antibacterial nano silver coating on the surface of polyethylene films using corona discharge. Surf. Coat Technol. 245, 1–8 (2014). https://doi.org/10.1016/j.surfcoat.2014.02.023
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper
Anjum, S., Gupta, B. (2018). Designing and Nanofunctionalization of Infection-Resistant Polyester Suture. In: Gupta, B., Ghosh, A., Suzuki, A., Rattan, S. (eds) Advances in Polymer Sciences and Technology. Materials Horizons: From Nature to Nanomaterials. Springer, Singapore. https://doi.org/10.1007/978-981-13-2568-7_1
Download citation
DOI: https://doi.org/10.1007/978-981-13-2568-7_1
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-2567-0
Online ISBN: 978-981-13-2568-7
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)