Abstract
Muscle atrophy and weakness, characterized by loss of lean muscle mass and function, has a significant effect on the independence and quality of life of older people. The cellular mechanisms that drive the age-related decline in neuromuscular integrity and function are multifactorial. Quiescent and contracting skeletal muscle can endogenously generate reactive oxygen and nitrogen species (RONS) from various cellular sites. Excessive RONS can potentially cause oxidative damage and disruption of cellular signaling pathways contributing to the initiation and progression of age-related muscle atrophy. Altered redox homeostasis and modulation of intracellular signal transduction processes have been proposed as an underlying mechanism of sarcopenia. This chapter summarizes the current evidence that has associated disrupted redox homeostasis and muscle atrophy as a result of skeletal muscle inactivity and aging.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Background
Loss of skeletal muscle mass and function is among the most consistent and striking change associated with the advance of age [1]. Age-related muscle atrophy (sarcopenia) is described as a progressive loss of lean muscle mass and muscle function, which has a significant effect on the quality of life of older people and overall morbidity. A reduction in overall muscle function with age is linked to an increased mortality risk [2], which leads to instability, a subsequent increased risk of falls and consequently an increased demand for medical and social care. Deficits in skeletal muscle begin at a relatively young age and continue until the end of life [3]; human studies have reported that by the age of 70, there is a 25–30% reduction in the fiber cross-sectional area of skeletal muscle and a subsequent reduction in muscle strength by 30–40% [4].
Reduced muscle mass and contractile force inherent with aging have been extensively studied in both murine models and humans and are associated with various neurological impairments including loss of motor units [5, 6], structural alterations and degeneration of neuromuscular junctions (NMJ) [7,8,9,10], a decline in motor nerve function (partial denervation) [9, 11,12,13], impaired nerve redox signaling [14], and changes in fiber type related to continual cycles of denervation and reinnervation [15]. While physical activity can inhibit the decline of muscle functional deficits [16], even physically active older adults exhibit age-related deficits in muscle mass and function [17]. Age-related muscle atrophy and weakness is a lifelong process with a multifactorial and complex etiology that involves both extrinsic and intrinsic factors [15]. However, elucidation of the primary molecular and biochemical mechanisms underlying the age-related decline in neuromuscular integrity and function has yet to be determined.
2 Reactive Oxygen and Nitrogen Species (RONS) Produced by Skeletal Muscle
The cellular damage induced by O2 toxicity was first reported more than 50 years ago and related to the increased generation of reactive species [18, 19], as a result of derivatives of O2 (Fig. 13.1). Studies in the 1980s reported that reactive species are endogenously generated in skeletal muscle [20,21,22]. It has since been determined that both resting and contracting myofibers can generate reactive oxygen and nitrogen species (RONS). Reactive oxygen species (ROS) refer to O2-derived molecules that are reactive species including O2-centered radicals but also non-radical species which are reactive derivatives of O2 [23]. Similarly, the term reactive nitrogen species (RNS) refers to both nitrogen radicals along with other reactive molecules where the reactive center is nitrogen [24,25,26]. RONS generation by skeletal muscle has been detected and quantified by a variety of methods including fluorescence-based microscopic assays [27, 28], spectrophotometry [29, 30], chemiluminescence [31, 32], HPLC techniques [33, 34], electron spin resonance spectroscopy (also known as electron paramagnetic resonance, EPR) [35, 36], and transfection methods including in vivo [37, 38] and in vitro [39]. Using a combination of the above techniques, it has been determined that the primary radical species generated by skeletal muscle include superoxide and nitric oxide (NO) [26, 40, 41].
Reactive oxygen derivatives produced by the sequential reduction of O 2 to H 2 O. Superoxide (O 2 ∙−), hydrogen peroxide (H 2 O 2), hydroxyl radical (● OH). (Redrawn from Sakellariou et al. [88])
2.1 Superoxide
Superoxide is derived either from the incomplete reduction of O2 during metabolism in the electron transport chain (ETC) or as a specific product of dedicated enzymatic systems [42]. The subcellular location of superoxide generation in skeletal muscle is dependent on whether the muscle is quiescent or contracting, as different pathways are involved. Figures 13.2 and 13.3 depict the different sites within skeletal muscle and proposed reactions for RONS generation. Superoxide generation is associated with electron leakage and incomplete O2 metabolism by mitochondrial ETC including complex I and complex III [43, 44] but also more recently complex II [45,46,47]. However, dedicated enzymes such as nicotinamide adenine dinucleotide phosphate (NADPH) oxidase enzymes including NOX2, NOX4, DUOX1, and DUOX2 [28, 29, 32, 48], xanthine oxidase (XO) [49, 50], and the lipoxygenases (LOXs) [51] which are linked to arachidonic acid (AA) release by the phospholipase A2 enzymes (PLA2) [52, 53] are also sources of superoxide; for a detailed review, see Ref. [54].
Schematic representation of the non-mitochondrial sites for nitric oxide and superoxide production in skeletal muscle. Superoxide (O 2 ∙−) is produced by multicomponent NAD(P)H oxidase 2 (NOX2), xanthine oxidase (XO), and the lipoxygenases (LOX) which activity is regulated by the phospholipase A2 enzymes (PLA 2). Arachidonic acid (AA) release by the membrane bound calcium-dependent PLA2 (sPLA 2) facilitates extracellular O 2 ∙− release by the membrane bound LOX. It is uncertain whether the cytosolic LOX enzymes contribute to intracellular O 2 ∙− changes which substrate availability might be regulated by the cytosolic calcium-independent PLA2 (iPLA 2). NAD(P)H oxidase 4 (NOX4) also contributes to ROS changes, though the primary ROS product, O 2 ∙− or hydrogen peroxide (H 2 O 2) of NOX4 is uncertain. Cytosolic and extracellular O 2 ∙− is dismuted into H2O2 by superoxide dismutase (SOD), SOD1 and SOD3, respectively, or reacts rapidly with membrane permeant nitric oxide (NO) produced by the endothelial and neuronal nitric oxide synthase (eNOs and nNOS) to form peroxynitrite (ONOO −). H2O2 formed within the extracellular space is reduced into H2O by the action of glutathione peroxidase 3 (GPX3) or peroxiredoxin IV (PRX4), while cytosolic H2O2 is reduced into H2O by glutathione peroxidase 1 (GPX1), catalase (CAT), or peroxiredoxins (PRXs). Reduced glutathione (GSH) provides the electrons to GPX to catalyze the reduction of H2O2; GSH is oxidized to glutathione disulfide (GSSG). Reduction of GSSG is catalyzed by glutathione reductase (GR), where NAD(P)H is used as the reducing agent. Cytosolic PRXs utilize thioredoxin 1 (Trx1 Red) for their reducing action. Oxidized form of Trx1 (Trx1 Ox) is reduced by thioredoxin reductase 1 (TR1), by utilizing electrons from NAD(P)H. ONOO− can be reduced predominantly into nitrite (NO2 −) by peroxiredoxin V (PRX5). Sarcoplasmic reticulum (SR). (Redrawn from Sakellariou et al. [88])
Schematic representation of the mitochondrial sites for nitric oxide and superoxide production and the channels that mediate the release of superoxide to the cytosolic compartment in skeletal muscle. Superoxide (O 2 ∙−) is produced by complex I, complex II, and complex III of the mitochondrial electron transport chain (ETC) of the inner mitochondrial membrane (IMM) and released into the matrix and the mitochondrial intermembrane space (MIS). NAD(P)H oxidase 4 (NOX4) also contributes to ROS changes, though the primary ROS product, O 2 ∙− or hydrogen peroxide (H 2 O 2) of NOX4 is uncertain. Arachidonic acid (AA) release by the calcium-dependent phospholipase A2 enzymes (sPLA 2) interacts with complex I and enhances superoxide generation by this complex. O 2 ∙− released into the matrix, and the MIS is dismuted into H2O2 by superoxide dismutase (SOD), SOD2 and SOD1, respectively, or reacts rapidly with nitric oxide (NO) produced by the endothelial nitric oxide synthase (eNOS) to form peroxynitrite (ONOO −). H2O2 is reduced into H2O by the action of glutathione peroxidase 4 (GPX4) or peroxiredoxins (PRXs). Reduced glutathione (GSH) provides the electrons to GPX4 to catalyze the reduction of H2O2; GSH is oxidized to glutathione disulfide (GSSG). Reduction of GSSG is catalyzed by glutathione reductase (GR), where NAD(P)H is used as the reducing agent. Mitochondrial PRXs utilize thioredoxin 2 (Trx2 Red) for their reducing action. Oxidized form of Trx2 (Trx2 Ox) is reduced by thioredoxin reductase 2 (TR2), by utilizing electrons from NAD(P)H. ONOO− can be reduced predominantly into nitrite (NO2 −) by peroxiredoxin V (PRX5). O 2 ∙− is essentially membrane impermeant, while H2O2 is readily diffusible. Matrix O 2 ∙− can diffuse to the cytosol through the inner membrane anion channel (iMAC) that spans the IMM and the outer mitochondrial membrane (OMM) or via the mitochondrial permeability transition pore (mPTP) comprised of the voltage-dependent anion channels (VDAC) on the OMM, the adenine nucleotide translocator (ANT) located on the IMM, and cyclophilin D (Cyclo D) located in the matrix. Channels of the OMM including VDAC, BAX, and possibly the translocase of outer membrane 40 (TOM40) can also mediate the release of O 2 ∙− from the MIS to the cytosol. (Redrawn from Sakellariou et al. [88])
2.2 Nitric Oxide
Nitric oxide (NO) is endogenously generated within cells by the nitric oxide synthases (NOS), through the conversion of L-arginine to citrulline utilizing NADPH as a cofactor [55]. NO is a primary radical, and its concentration has been demonstrated to be regulated by NOS isoenzymes: the neuronal NOS (type I or nNOS), the inducible NOS (type II or iNOS), and the endothelial NOS isoenzyme (type III or eNOS) [54, 56]. nNOS was originally discovered in neuronal tissue but has also been shown to be expressed in the plasma membrane of skeletal muscle fibers where it interacts with the dystrophin-glycoprotein complex via a linkage to α1-syntrophin [57]. The eNOS isoenzyme was originally described in the endothelium where it is associated with caveolin-1; in skeletal muscle it is localized in the mitochondria and has been reported to be activated by heat shock protein 90 (HSP90) [58]. The expression of iNOS in skeletal muscle is increased in response to inflammatory conditions or following a septic challenge [59, 60]. NO has shown to interact with a number of different cytoskeletal proteins mainly through reactive cysteine residues and the formation of S-nitrosated residues [61]. The nNOS isoform is particularly expressed in glycolytic or fast muscle fibers [62] and has been suggested to be the primary source of NO release from myocytes [63]. The close proximity of nNOS to the dystrophin-glycoprotein complex has a pivotal role in skeletal muscle physiology as highlighted from studies utilizing the mdx mice [64] but also in humans suffering from muscle dystrophy [57, 65]. It has been suggested that NO has a direct functional signaling role via the formation of S-nitrosylated sites with effects on protein activity or indirectly by interactions with heme or nonheme Fe and Cu [66].
2.3 Hydrogen Peroxide
Hydrogen peroxide (H2O2) is a relatively stable molecule in comparison with the other reactive species with a longer half-life; hence H2O2 been suggested as the most likely candidate for redox signaling pathways [67]. H2O2 can interact with redox-sensitive components or pathways typically via oxidation of sensitive Cys residues and has been demonstrated to regulate the activity of a variety of transcription factors in skeletal muscle [68]. In aqueous solutions, superoxide can be protonated to produce hydroperoxyl radical or reduced undergoing a dismutation reaction to produce H2O2 [69]. In addition, a number of enzyme systems have also been reported to generate H2O2 including NOX4 [70, 71], urate, and amino acid oxidases [72]. Moreover, recent evidence supports endoplasmic reticulum (ER) H2O2 generation in vivo [73] via thiol-disulfide exchange mechanisms [74]. The catalytic activity of a wide range of metabolic enzymes can be modulated by H2O2, typically by oxidation of catalytic Cys residues or residues essential for disulfide bonds [75]. In addition there are a number of different enzymes that use H2O2 as a substrate including the peroxiredoxins, glutathione peroxidases, and catalase; isoforms of these enzymes are located in specific cellular locations which would suggest that it plays an important physiological signaling role.
2.4 Hydroxyl Radical
The hydroxyl radical is a highly reactive molecule due to its strong oxidizing potential and can rapidly react with biomolecules located close to its site of generation. In skeletal muscle fibers and other biological systems, hydroxyl radicals are typically generated as a result of the Fenton reaction that involves the reductive decomposition of H2O2 with reduced transition metal ions, copper (Cu) or iron (Fe) [76]. Oxidation of FeS cluster enzymes can result in an increase of “free iron” within the cell, allowing for the formation of hydroxyl radicals and altered redox homeostasis [77]. Similar to the Fenton reaction, the Haber-Weiss reaction can also generate hydroxyl radicals by Fenton chemistry, Fe or Cu is maintained in a reduced form by superoxide, which can result in the formation of hydroxyls from H2O2 [78]. There is some in vivo evidence to suggest that during skeletal muscle contractile activity, there is enhanced hydroxyl radical generation [79]. An increased intracellular concentration of highly reactive hydroxyl radicals can affect calcium dynamics and maximum force of skeletal myofibers [76]. There are a number of neuromuscular disorders such as including glucocorticoid-induced myopathy [80] and immobilization-induced skeletal muscle atrophy [81] that have reported an increase in hydroxyl radical formation.
2.5 Peroxynitrite
Peroxynitrite is another endogenously generated reactive species that can act as an intracellular oxidant; it is primarily generated by the reaction between NO and superoxide, often as a result of the close proximity of NOX and NOS enzymes [82]. Further evidence to support endogenous generation of peroxynitrite in skeletal muscle is shown in studies using transgenic animals where the levels of NO and/or superoxide were elevated [34]. Similar to the some of the other reactive species, peroxynitrite can oxidize sensitive Cys residues involved in disulfides or catalytic sites [83]. The protonated form, peroxynitrous acid, is also highly reactive and can oxidize Cys residues resulting in protein oxidation, phospholipid and DNA damage [82, 84]. It has also been reported that peroxynitrite is involved in tyrosine nitration [85] as well as the formation of S-nitrosylated Cys residues [86]; mass spectrometry approaches have identified an increasing number of proteins being nitrosylated and nitrated in skeletal muscle. In conditions where there are high concentrations of peroxynitrite, it can result in reversible and irreversible oxidation of cellular compartments of myofibers [34, 87], affecting overall enzymatic activity through structural modifications, including altered cytoskeletal dynamics and an impair cell signal transduction [82].
3 Primary Antioxidant Enzymes Expressed in Skeletal Muscle
Skeletal muscle expresses a sophisticated system to control the production of oxidants and protect the myofibers from oxidative damage. The system that functions to prevent oxidative damage consists of enzymatic and nonenzymatic antioxidants that work in a coordinated fashion to regulate redox disturbances in the muscle cell. An extended coverage of these goes beyond the scope of this chapter (for detailed review, see Ref. [88]. However, we summarize the most important enzymatic systems expressed in skeletal muscle including superoxide dismutases, catalase, glutathione peroxidases, peroxiredoxins, and glutaredoxins.
Superoxide dismutase (SOD) was discovered in 1969 and represents a family of metalloenzymes that catalyze the one electron dismutation of superoxide into O2 and H2O2 [26]. There are three SOD isoenzymes depending on the metal ion bound to the active site. Skeletal muscle expresses copper-zinc SOD (SOD1 or CuZnSOD), which is a highly stable enzyme present within the cytosol and the mitochondrial intermembrane space (MIS), and manganese-SOD (SOD2 or MnSOD) which is found in the mitochondrial matrix [89]. There is however an additional isoform of SOD, the extracellular SOD isoenzyme (SOD3 or EcSOD) [90] which is present in the interstitial spaces of tissues and extracellular fluids of many cell types and tissues and its primary function is to reduce superoxide formed outside the cell membrane [90].
Catalase (CAT), a homotetramer with a molecular mass of 240kDa catalyzes the reduction of H2O2 into H2O and O2. CAT is mainly found in the cytosolic compartment of the muscle fibers and requires heme (Fe3+) bound at the enzyme’s active site for its catalytic function [91]. CAT enzymatic activity increases with increased H2O2, and reports have shown that protein expression and activity is higher in highly oxidative myofibers [92]. CAT does not require reducing equivalents to function as a H2O2 reducer; thus CAT is considered an energy-efficient antioxidant [93].
Glutathione peroxidase (GPX), a homotetramer with each 22kDa subunit containing a selenium atom in the form of a selenocysteine, also catalyzes the reduction of H2O2 to H2O or organic hydroperoxides (ROOH) to alcohol, using reduced glutathione (GSH) or in some cases thioredoxin (TRX) or glutaredoxin (GRX) as an electron donor [94]. In addition, reports also suggest that GPX is also implicated in the reduction of hydroxyl radical by elimination of H2O2 [95]. Mammalian cells express five isoforms of GPX (GPX1-GPX5), which differ in cellular localization and substrate specificity [96] with GPX1 as the cytosolic form [97] and GPX4 as the most widely expressed. GPX4 is a membrane-associated enzyme, partly localized to the MIS. GPX3 also known as plasma or extracellular GPX is present in the extracellular space [98, 99], whereas GPX2 is mainly expressed in the gastrointestinal system [100]. GPX5 is expressed in the epididymis in the mammalian male reproductive tract and is the least studied isoenzyme [100, 101]. The expression of the GPX genes is controlled by different mechanisms including O2 tension, metabolic rate, toxins, and xenobiotics [23] as well as growth and development [102]. Similarly, to CAT, oxidative muscle fibers express higher amounts of GPX compared with glycolytic myofibers [100]. Though there is an overlap between the function of GPX and CAT, GPX has a higher affinity for H2O2 at low concentrations. However, under conditions where H2O2 is significantly increased, CAT becomes more significant in protecting biological systems, and its catalytic function prevails since it cannot be saturated under any H2O2 concentration since there is no apparent Vmax [103].
Peroxiredoxins (PRXs) initially described as thiol-specific antioxidants [104] were discovered in the late 1980s [105, 106] and are a family of cysteine-dependent thioredoxin peroxidases [107]. PRXs are capable of reducing both ROOH and H2O2 [108] with the use of electrons provided by thioredoxins [108]. Skeletal muscles express six isoforms of PRXs, which are present in the cytosolic compartment (PRX I, II, VI), the mitochondrion (PRX III), the extracellular space, and endoplasmic reticulum (PRX IV) [42]. PRXV is expressed in the cytosol, mitochondria, nuclei, and perixosomes [108] and is considered a peroxynitrite reductase [109]. PRX proteins have recently received much attention as they have shown to play a key role in transmitting redox signals into a dynamic biological response and to have subtle changes in both abundance and oxidative state with age [35, 110, 111].
Glutaredoxins (GRXs) are small ubiquitous disulfide oxidoreductases which share many of the functions of TRXs but are reduced by GSH rather than a specific reductase [122]. GRXs are small redox enzymes that exist in either a reduced or oxidized form and are involved in the protection and repair of protein and nonprotein thiols during compromised redox homeostasis [112]. GRXs are divided into monothiol (Cys-X-X-Ser) and dithiol (Cys-X-X-Cys) GRXs [113]. Dithiol GPXs participate in the regulation of H2O2 via PRX pathways [114], proliferation and differentiation [115], transcription regulation via modulating the activity of nuclear factor κB (NFκB) [116], and apoptosis [117]. Monothiol GRXs are implicated in iron sulfur (FeS) cluster biosynthesis and Fe homeostasis [118]. GRX1 prevents oxidative damage and apoptosis and is found in the cytosol, and the MIS. GPX1 has also shown to translocate into the nucleus and exported from the cell [113]. GRX2 is localized in the mitochondria [119] and GRX3 in the nuclear and cytosolic compartment. Monothiol GRX5 has a mitochondrial translocation signal and shares the active-site motif of GRX3 [120]. Reports have also revealed that the GRX system can also catalyze reversible protein glutathionylation [121] and regulate the redox state of thiol groups [122] during aberrant redox control.
In addition to the main antioxidant enzyme defense network, skeletal muscle also expresses glucose-6-phosphate dehydrogenase (G6PD) and isocitrate dehydrogenase (IDH) which do not directly scavenge RONS but play a pivotal role in redox regulation by providing reducing power in the form of NADPH to the antioxidant enzymatic systems [123]. In addition, skeletal muscle also contains nonenzymatic antioxidants, which regulate reactive species and protect muscle cells from oxidative injury. These are H2O soluble and fat soluble and are classified into two categories: (i) the endogenously produced and (ii) dietary antioxidants which cannot be synthesized or induced and must be taken from the diet. The main nonenzymatic antioxidants found in myofibers include GSH, uric acid, bilirubin, and coenzyme Q10 endogenously produced antioxidants but also dietary antioxidants including vitamin C, vitamin E, and carotenoids. An extended coverage of the nonenzymatic defense systems in skeletal muscle goes beyond the scope of this review; for a detailed review, see Refs. [124, 125].
4 Age-Related Muscle Atrophy Is Linked to Increased Oxidative Damage
The dual role of RONS to act as signaling molecules at low concentrations but also damage critical cellular compartment when produced at high concentrations is fundamental in skeletal muscle physiology/pathology. Reports in humans [126,127,128] and rodents [87, 129, 130] have provided evidence that age-related muscle atrophy is linked to an altered oxidative status of redox-responsive proteins [131], elevated concentration of oxidized macromolecules including an increase in DNA damage [126, 132], increased levels of lipid peroxidation [133, 134], and accumulation of oxidized proteins [127, 128]. Increased DNA damage has been shown to alter genetic stability which may induce the expression of genes that regulate cell proliferation and/or block the expression of certain genes, thus permitting damage with increasing age [135]. RONS-induced DNA sequence changes or mutations have been suggested to affect the cellular state of differentiation [23, 136] and accumulation of mitochondrial DNA damage [132] which may prevent the rejuvenation of the mitochondrial population and lead to bioenergetic decline and cellular death [137]. In addition, aged skeletal muscle exhibits an accumulation of catalytically inactive or less active forms of enzymes and the observed age-related changes in catalytic activity have been suggested to occur due to oxidative modifications induced by RONS [138, 139].
Recent reports have provided evidence that increased oxidative damage inherent with aging is linked to age-associated changes in RONS, with myofibers from old rodents exhibiting increased intracellular RONS levels compared to young/adult rodents [140, 141]. Oxidants can modulate various intracellular signal transduction pathways, and age-related disruption of these processes due to compromised redox homeostasis has been suggested as contributing factor to muscle atrophy inherent with aging. The role of redox homeostasis in age-related muscle atrophy and weakness has been studied in various model organisms (reviewed in [88]) which have undergone genetic manipulations (transgenic and knockout models) and have provided insight into the function of RONS regulatory systems in neuromuscular aging.
5 Deletion of Cu-Zn Superoxide Dismutase in SOD1 −/− Mice Leads to Accelerated Neuromuscular Aging and Functional Deficits
The association between redox regulation and age-related atrophy has been studied in several mammalian models which have undergone genetic manipulations (reviewed in [88]), to enable the study of disrupted redox signaling on the aging process. Deletion of CuZnSOD in mice (SOD1 −/− mice) leads to a reduction in lifespan and an accelerated aging phenotype associated with myofiber atrophy (Fig. 13.4), neurological impairments (Fig. 13.5), and functional deficits [142]. Elevated oxidative damage has also been observed in skeletal muscles from SOD1 −/− mice [34, 143,144,145,146,147,148,149], and many features of the muscles of SOD1 −/− mice including loss of fibers, reduction in contractile force, a constitutive activation of redox-sensitive transcription factors [146], degeneration of neuromuscular junctions (NMJ), and of loss of innervation resemble those observed in old wild-type mice [144, 145] and in older humans [13, 144]. Hence, it has been suggested that the SOD1 −/− model may potentially provide a useful model to study the role of chronic oxidative stress in loss of skeletal muscle and to uncover potential targets for intervention for preventing age-related muscle wasting.
Gross morphology of skinned hindlimb and forelimb muscles of SOD1 −/− and WT mice at 12 months of age. Arrows indicate the phenotypic hindlimb muscle changes observed in SOD1 −/− compared to WT mice. (Redrawn from Sakellariou et al. [14])
Neuromuscular junction structure and peripheral nerve integrity in SOD1 −/− mice. (a) Intravital immunofluorescence imaging of neuromuscular junctions (NMJ) of an AT muscle from a SOD1 −/− mouse. Presynaptic motor neurons immunolabeled with neuronal class III β-tubulin monoclonal antibody (TUJ1), a neuronal marker (green), and postsynaptic motor endplate acetylcholine receptors (AChRs) stained with Alexa Fluor 594-conjugated α-bungarotoxin (red). Right panels show enlarged area marked by white box in the left panel. 10x original magnification (left panel). Scale bar, 150μm. (b) Transverse section of a sciatic nerve (SN) from a WT (SOD1 +/+) mouse (top panel). 20x original magnification. Scale bar, 100μm; Bottom left panel shows enlarged area marked by red box in the top panel to show the morphology and myelin thickness of motor axons of the peripheral nerve. 60x original magnification. Scale bar, 10μm; Transverse section of a SN from a SOD1 −/− mouse (bottom right panel). Note reduced myelin thickness of motor axons from peripheral nerve of the SOD1 −/− model, indicated by arrowheads. 60x original magnification. Scale bar, 10μm. (Redrawn from Sakellariou et al. [14])
The prominent sarcopenic phenotype observed in the SOD1 −/− model is associated with a number of neurological impairments (Fig. 13.5), including striking alterations in NMJ and peripheral nerve integrity/function (Fig. 13.5), motor axon degeneration, postsynaptic endplate fragmentation, terminal sprouting and axon thinning and irregular swelling, reduced occupancy of the motor endplates by axons, loss of innervation and motor function [143], impaired neurotransmitter release [150], and reduction in isometric force [145]. Collectively, these findings may suggest that the muscle atrophy phenotype shown in the SOD1 −/− model might be initiated by disrupted redox signaling in motor neurons.
Disrupted redox signaling in motor neurons as a potential mechanism of sarcopenia in SOD1 −/− mice has recently been assessed in genetically engineered mouse models including models with targeted deletion of CuZnSOD specifically in skeletal muscle alone [149] or motor neurons [148] but also in a “nerve rescue” SOD1 −/− mouse model with neuron-specific expression of CuZnSOD [147], using a transgenic SOD1−/− mouse model in which SOD1 was expressed under control of the synapsin 1 promoter. The data from these studies provided evidence that CuZnSOD deficits in either the muscle or motor neuron alone are not sufficient to initiate a full sarcopenic phenotype and that deficits in both tissues are required to recapitulate the loss of muscle and function observed in the SOD1−/− model. Moreover, the data further showed that neuron-specific insertion of SOD1 corrected the skeletal muscle aging phenotype observed in SOD1−/− mice indicating that deficits in redox homeostasis in motor nerves appear to be the underlying factor that initiates mitochondrial dysfunction and oxidative damage which triggers a retrograde response leading to further NMJ degeneration and dysfunction. These reports have provided insight into the understanding of (i) the defective redox signaling events that underlie age-related atrophy and (ii) the redox-mediated cross talk between motor neurons and skeletal muscle.
6 Neuromuscular Aging Is Associated with Redox Proteomic Changes
In order to unravel the mechanisms responsible for the structural and functional changes associated with neuromuscular aging, many laboratories have begun to investigate both the proteome and site-specific redox modifications within skeletal muscle, to identify those proteins that change in abundance but also to identify those proteins that are particularly sensitive to redox changes.
Site-specific RONS-induced redox modifications of key regulatory enzymes can alter a wide variety of metabolic pathways related to cellular response to energy and stress. Modulation of the activity of downstream protein targets by redox modifications can also influence a variety of key regulators of distinct posttranslational modifications (PTMs) such as phosphorylation, ubiquitination, and acetylation, including components that control metabolic rate such as AMP-activated protein kinase (AMPK), protein kinase C (PKC), sirtuin 1, and mammalian target of rapamycin (mTOR) [131]. In skeletal muscle a number of redox-sensitive proteins are involved in excitation-contraction coupling; these modifications can specifically affect calcium homeostasis including calcium release, binding, and sequestration through site-specific redox modifications of specific cysteine (Cys), e.g., sarcoplasmic/endoplasmic reticulum Ca2+ ATPase (SERCA) and ryanodine receptor 1 (Ryr1) [151, 152]. The nature or type of RONS-induced redox modification is dependent on a number of factors including the residues modified (typically Cys), the species and concentration of RONS generated, and the properties of the amino acids surrounding the modified residue which can influence the sensitivity to modifications. One of the goals of redox proteomic approaches is to identify the RONS modification, the amino acid residue that has been modified, and the relative quantification of the modified amino acid, including both reversible and irreversible modifications which have shown to influence contractile force [48, 111, 153]. The major reversible RONS-induced modifications of Cys residues include sulfenylation (-SOH), glutathionylation (-SSG), nitrosylation (-SNO), and inter-/intra-disulfide bond formation (-S-S-) [131]. The largely irreversible modifications include sulfonic (-SO3H) or sulfinic (SO2H) acid formation [154].
Neuromuscular aging exhibits an altered redox proteome with subsequent biochemical and physiological effects on the cytoskeleton, mitochondria, calcium signaling and sequestration [155,156,157]. Redox proteomic approaches have demonstrated that skeletal muscle aging is correlated with altered catalytic activity of a number of regulatory enzymes and an overall reduction in the identification of redox-sensitive proteins particularly involved in the generation of precursor metabolites and energy metabolism [111, 131]. These results suggest that age-related redox changes have a significant role in the loss of skeletal muscle mass and function inherent with aging. Reversible redox modifications on specific proteins are essential for correct adaptive response to contractile activity with activation of specific pathways, and skeletal muscle has shown to develop a dysregulated redox response with aging [111, 131]. However, irreversible oxidative modifications as a result of excessive RONS can lead to insoluble protein aggregates and protein degradation, which have been reported to increase in neurodegenerative diseases and aging [158]. Recent reports have demonstrated that reversible and irreversible redox modifications of myofilament proteins can modify both structure and function [159]; several regulatory and cytoskeletal myofilament proteins including troponin C [160], actin, α-actinin [111, 159], and myosin heavy chains [161,162,163] are susceptible to RONS-induced oxidative modifications, thus affecting Ca2+ dynamics and Ca2+ sensitivity [164] and as a result cross-bridge cycling [160] which ultimately affects contractile function.
7 Causative Links Between Disrupted Redox Signaling and Muscle Atrophy
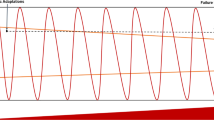
There are a number of studies that have demonstrated a link between increased intracellular RONS concentrations and an altered redox environment in skeletal muscle atrophy, as a result of either muscle disuse [165] or disease [166]. The causative links between redox homeostasis and skeletal muscle atrophy include signaling pathways that regulate both protein synthesis and protein breakdown [167,168,169]. Regular exercise can help maintain skeletal muscle mass, yet contracting skeletal muscle generates RONS predominantly from NOX and NOS systems [28], which in turn are thought to acutely activate a variety of redox-regulated transcription factors (Nrf-2, NF-κB) required for adaptation to exercise [170]. In exercise studies it has been reported that ingesting high doses of vitamin C and E can blunt the beneficial and adaptive responses induced by exercise in skeletal muscle presumably by disrupting the RONS signaling cascade [71]. However, in skeletal muscle from older individuals, there is a higher basal level of RONS, and as a result, chronic activation of many redox-regulated transcription factors may blunt many of the beneficial adaptive responses following an acute RONS-dependent increase during exercise [172].
The IGF1-Akt pathway is one of the key global regulators of protein synthesis; a number of studies have demonstrated that activation of IGF1 receptor can promote muscle hypertrophy, while inactivation is related to an impairment of muscle growth. [173]. The role of oxidative damage in relation to IGF1 signaling is unclear with reports suggesting that it may result in the promotion and inhibition of Akt signaling [174]. Studies using C2C12 myotubes have shown that oxidative damage due to chronic exposure to low levels of H2O2 attenuates Akt phosphorylation which would be predicted to result in an overall decrease in protein synthesis, increased proteolysis, and as a result increased muscle atrophy [174]. In support of this finding, a recent report demonstrated that administration of the mitochondrial targeted antioxidant peptide SS-31 resulted in an increase in the phosphorylated form of Akt and mTORC1 indicating that aberrant redox homeostasis can attenuate muscle protein synthesis by inhibiting the Akt/mTORC1 signaling pathway [175].
Growing evidence suggests that disrupted redox signaling due to enhanced RONS generation effects autophagy-mediated protein breakdown, a highly regulated lysosomal pathway used for the degradation of non-myofibril cytosolic proteins and organelles in skeletal muscle [167]. RONS can directly affect this process as oxidative damage induced by H2O2 treatment of fibroblasts can result in an increase in the expression of key autophagy components such as LC3, beclin1, and increased formation of autophagosomes [176]. RONS may also alter the activity of the regulators of autophagy; for example, the inactivation of ATG4 can prevent the cleavage of LC3 during the generation of the autophagosome, which is an essential step in the process of autophagy [167, 177].
Furthermore, the regulation of the proteasomal degradation pathway can also be regulated by intracellular RONS. In vivo studies have demonstrated that increased RONS can promote muscle protein breakdown via increased activity of the proteasome system [178], [14] but also through the activation of calpains, specific proteases that are involved in the selective cleavage of target proteins [179].
8 Perspectives
Muscle atrophy and weakness, in the context of neuromuscular aging and a wide range of myopathies, has a significant effect on individuals with respect to independence and overall quality of life. There is ongoing research to develop both pharmacological and non-pharmacological therapeutic approaches to inhibit or prevent loss of skeletal muscle mass and function [180]. Age-related skeletal muscle atrophy is a multifactorial process, involving a variety of metabolic processes and signaling pathways whose disruption ultimately result in skeletal muscle loss and functional deficits. The primary biochemical and molecular mechanisms responsible for muscle atrophy have not been fully identified. Considerable evidence in both humans and various organisms has shown that the myofibrillar redox environment can influence the activity of crucial pathways involved in biogenesis and degradation but also the regulation of excitation contraction coupling, making it an attractive target for interventional approaches. There is a wealth of scientific research from both human and animal studies that have described an altered redox environment within skeletal muscle with age, in particular increased oxidation of redox-sensitive proteins and macromolecules correlated with age-related atrophy. An altered redox environment has also been described in many age-related diseases including neurodegenerative disorders, neuromuscular diseases, and diabetes. However, whether disrupted redox signaling is the initial cause of disease, development or a consequence leading to disease progression has yet to be fully determined. To elucidate the role of redox homeostasis in age-related disease, particularly in neuromuscular integrity and function, the generation of tissue-specific knockout models and the development of sensitive tools for measuring RONS generation and the subsequent redox modifications and signaling roles are warranted. Identification of the precise signaling roles of endogenously generated RONS and the balance between RONS signaling and oxidative damage will increase our understanding of the role of redox homeostasis in skeletal muscle adaptation to exercise and maintaining neuromuscular integrity. Increased understanding of the precise molecular pathways that regulate the balance between adaptation and muscle growth compared with disuse and atrophy may reveal potential therapeutic targets for intervention and ultimately prevent sarcopenia in humans.
References
Evans WJ (2010) Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr 91(4):1123S–1127S. https://doi.org/10.3945/ajcn.2010.28608A
Newman AB, Kupelian V, Visser M, Simonsick EM, Goodpaster BH, Kritchevsky SB, Tylavsky FA, Rubin SM, Harris TB (2006) Strength, but not muscle mass, is associated with mortality in the health, aging and body composition study cohort. J Gerontol A Biol Sci Med Sci 61(1):72–77
Larsson L (1983) Histochemical characteristics of human skeletal muscle during aging. Acta Physiol Scand 117(3):469–471
Porter MM, Vandervoort AA, Lexell J (1995) Aging of human muscle: structure, function and adaptability. Scand J Med Sci Sports 5(3):129–142
Campbell MJ, McComas AJ, Petito F (1973) Physiological changes in ageing muscles. J Neurol Neurosurg Psychiatry 36(2):174–182
McNeil CJ, Rice CL (2007) Fatigability is increased with age during velocity-dependent contractions of the dorsiflexors. J Gerontol A Biol Sci Med Sci 62(6):624–629
Hourigan ML, McKinnon NB, Johnson M, Rice CL, Stashuk DW, Doherty TJ (2015) Increased motor unit potential shape variability across consecutive motor unit discharges in the tibialis anterior and vastus medialis muscles of healthy older subjects. Clin Neurophysiol 126(12):2381–2389. https://doi.org/10.1016/j.clinph.2015.02.002
Oda K (1984) Age changes of motor innervation and acetylcholine receptor distribution on human skeletal muscle fibres. J Neurol Sci 66(2-3):327–338
Valdez G, Tapia JC, Kang H, Clemenson GD Jr, Gage FH, Lichtman JW, Sanes JR (2010) Attenuation of age-related changes in mouse neuromuscular synapses by caloric restriction and exercise. Proc Natl Acad Sci U S A 107(33):14863–14868. https://doi.org/10.1073/pnas.1002220107
Wokke JH, Jennekens FG, van den Oord CJ, Veldman H, Smit LM, Leppink GJ (1990) Morphological changes in the human end plate with age. J Neurol Sci 95(3):291–310
Krantic S, Mechawar N, Reix S, Quirion R (2005) Molecular basis of programmed cell death involved in neurodegeneration. Trends Neurosci 28(12):670–676. https://doi.org/10.1016/j.tins.2005.09.011
Jang YC, Van Remmen H (2011) Age-associated alterations of the neuromuscular junction. Exp Gerontol 46(2-3):193–198. https://doi.org/10.1016/j.exger.2010.08.029
Ward RE, Boudreau RM, Caserotti P, Harris TB, Zivkovic S, Goodpaster BH, Satterfield S, Kritchevsky S, Schwartz AV, Vinik AI, Cauley JA, Newman AB, Strotmeyer ES, Health ABCs (2015) Sensory and motor peripheral nerve function and longitudinal changes in quadriceps strength. J Gerontol A Biol Sci Med Sci 70(4):464–470. https://doi.org/10.1093/gerona/glu183
Sakellariou GK, McDonagh B, Porter H, Giakoumaki II, Earl KE, Nye GA, Vasilaki A, Brooks SV, Richardson A, Van Remmen H, McArdle A, Jackson MJ (2018) Comparison of whole body SOD1 knockout with muscle-specific SOD1 knockout mice reveals a role for nerve redox signaling in regulation of degenerative pathways in skeletal muscle. Antioxid Redox Signal 28(4):275–295. https://doi.org/10.1089/ars.2017.7249
Hepple RT, Rice CL (2016) Innervation and neuromuscular control in ageing skeletal muscle. J Physiol 594(8):1965–1978. https://doi.org/10.1113/JP270561
Hughes VA, Roubenoff R, Wood M, Frontera WR, Evans WJ, Fiatarone Singh MA (2004) Anthropometric assessment of 10-y changes in body composition in the elderly. Am J Clin Nutr 80(2):475–482
Wiswell RA, Hawkins SA, Jaque SV, Hyslop D, Constantino N, Tarpenning K, Marcell T, Schroeder ET (2001) Relationship between physiological loss, performance decrement, and age in master athletes. J Gerontol A Biol Sci Med Sci 56(10):M618–M626
Fenn WO, Gerschman R, Gilbert DL, Terwilliger DE, Cothran FV (1957) Mutagenic effects of high oxygen tensions on Escherichia Coli. Proc Natl Acad Sci U S A 43(12):1027–1032
Gerschman R, Gilbert DL, Nye SW, Dwyer P, Fenn WO (1954) Oxygen poisoning and x-irradiation: a mechanism in common. Science 119(3097):623–626
Davies KJ, Quintanilha AT, Brooks GA, Packer L (1982) Free radicals and tissue damage produced by exercise. Biochem Biophys Res Commun 107(4):1198–1205
Dillard CJ, Litov RE, Savin WM, Dumelin EE, Tappel AL (1978) Effects of exercise, vitamin E, and ozone on pulmonary function and lipid peroxidation. J Appl Physiol 45(6):927–932
Jackson MJ, Edwards RH, Symons MC (1985) Electron spin resonance studies of intact mammalian skeletal muscle. Biochim Biophys Acta 847(2):185–190 doi:0167-4889(85)90019-9 [pii]
Halliwell B, Gutteridge J (2007) Free radicals in biology and medicine. Oxford University Press, Oxford
Jackson MJ (2008) Free radicals generated by contracting muscle: by-products of metabolism or key regulators of muscle function? Free Radic Biol Med 44(2):132–141. doi:S0891-5849(07)00388-7 [pii]. https://doi.org/10.1016/j.freeradbiomed.2007.06.003
Jackson MJ (2009) Redox regulation of adaptive responses in skeletal muscle to contractile activity. Free Radic Biol Med 47(9):1267–1275. doi:S0891-5849(09)00531-0 [pii]. https://doi.org/10.1016/j.freeradbiomed.2009.09.005
Palomero J, Jackson MJ (2010) Redox regulation in skeletal muscle during contractile activity and aging. J Anim Sci 88(4):1307–1313. doi:jas.2009-2436 [pii]. https://doi.org/10.2527/jas.2009-2436
Picard M, Ritchie D, Wright KJ, Romestaing C, Thomas MM, Rowan SL, Taivassalo T, Hepple RT (2010) Mitochondrial functional impairment with aging is exaggerated in isolated mitochondria compared to permeabilized myofibers. Aging Cell 9(6):1032–1046. https://doi.org/10.1111/j.1474-9726.2010.00628.x
Sakellariou GK, Vasilaki A, Palomero J, Kayani A, Zibrik L, McArdle A, Jackson MJ (2013) Studies of mitochondrial and nonmitochondrial sources implicate nicotinamide adenine dinucleotide phosphate oxidase(s) in the increased skeletal muscle superoxide generation that occurs during contractile activity. Antioxid Redox Signal 18(6):603–621. https://doi.org/10.1089/ars.2012.4623
Hidalgo C, Sanchez G, Barrientos G, Aracena-Parks P (2006) A transverse tubule NADPH oxidase activity stimulates calcium release from isolated triads via ryanodine receptor type 1 S -glutathionylation. J Biol Chem 281(36):26473–26482. doi:M600451200 [pii]. https://doi.org/10.1074/jbc.M600451200
Xia R, Webb JA, Gnall LL, Cutler K, Abramson JJ (2003) Skeletal muscle sarcoplasmic reticulum contains a NADH-dependent oxidase that generates superoxide. Am J Physiol Cell Physiol 285(1):C215–C221. https://doi.org/10.1152/ajpcell.00034.2002 00034.2002 [pii]
Mofarrahi M, Brandes RP, Gorlach A, Hanze J, Terada LS, Quinn MT, Mayaki D, Petrof B, Hussain SN (2008) Regulation of proliferation of skeletal muscle precursor cells by NADPH oxidase. Antioxid Redox Signal 10(3):559–574. https://doi.org/10.1089/ars.2007.1792
Whitehead NP, Yeung EW, Froehner SC, Allen DG (2010) Skeletal muscle NADPH oxidase is increased and triggers stretch-induced damage in the mdx mouse. PLoS One 5(12):e15354. https://doi.org/10.1371/journal.pone.0015354
Kalyanaraman B, Darley-Usmar V, Davies KJ, Dennery PA, Forman HJ, Grisham MB, Mann GE, Moore K, Roberts LJ 2nd, Ischiropoulos H (2012) Measuring reactive oxygen and nitrogen species with fluorescent probes: challenges and limitations. Free Radic Biol Med 52(1):1–6. https://doi.org/10.1016/j.freeradbiomed.2011.09.030
Sakellariou GK, Pye D, Vasilaki A, Zibrik L, Palomero J, Kabayo T, McArdle F, Van Remmen H, Richardson A, Tidball JG, McArdle A, Jackson MJ (2011) Role of superoxide-nitric oxide interactions in the accelerated age-related loss of muscle mass in mice lacking Cu,Zn superoxide dismutase. Aging Cell 10(5):749–760. https://doi.org/10.1111/j.1474-9726.2011.00709.x
McDonagh B, Scullion SM, Vasilaki A, Pollock N, McArdle A, Jackson MJ (2016) Ageing-induced changes in the redox status of peripheral motor nerves imply an effect on redox signalling rather than oxidative damage. Free Radic Biol Med 94:27–35. https://doi.org/10.1016/j.freeradbiomed.2016.02.008
Pattwell D, Ashton T, McArdle A, Griffiths RD, Jackson MJ (2003) Ischemia and reperfusion of skeletal muscle lead to the appearance of a stable lipid free radical in the circulation. Am J Physiol Heart Circ Physiol 284(6):H2400–H2404. https://doi.org/10.1152/ajpheart.00931.2002
Sartoretto JL, Kalwa H, Pluth MD, Lippard SJ, Michel T (2011) Hydrogen peroxide differentially modulates cardiac myocyte nitric oxide synthesis. Proc Natl Acad Sci U S A 108(38):15792–15797. https://doi.org/10.1073/pnas.1111331108
Loehr JA, Abo-Zahrah R, Pal R, Rodney GG (2014) Sphingomyelinase promotes oxidant production and skeletal muscle contractile dysfunction through activation of NADPH oxidase. Front Physiol 5:530. https://doi.org/10.3389/fphys.2014.00530
Espinosa A, Garcia A, Hartel S, Hidalgo C, Jaimovich E (2009) NADPH oxidase and hydrogen peroxide mediate insulin-induced calcium increase in skeletal muscle cells. J Biol Chem 284(4):2568–2575. https://doi.org/10.1074/jbc.M804249200
McArdle A, Jackson MJ (2000) Exercise, oxidative stress and ageing. J Anat 197(Pt 4):539–541
Jackson MJ, McArdle A (2011) Age-related changes in skeletal muscle reactive oxygen species generation and adaptive responses to reactive oxygen species. J Physiol 589(Pt 9):2139–2145. doi:jphysiol.2011.206623 [pii]. https://doi.org/10.1113/jphysiol.2011.206623
Powers SK, Jackson MJ (2008) Exercise-induced oxidative stress: cellular mechanisms and impact on muscle force production. Physiol Rev 88(4):1243–1276. doi:88/4/1243 [pii]. https://doi.org/10.1152/physrev.00031.2007
Muller FL, Liu Y, Van Remmen H (2004) Complex III releases superoxide to both sides of the inner mitochondrial membrane. J Biol Chem 279(47):49064–49073
Murphy MP (2009) How mitochondria produce reactive oxygen species. Biochem J 417(1):1–13
Goncalves RL, Quinlan CL, Perevoshchikova IV, Hey-Mogensen M, Brand MD (2015) Sites of superoxide and hydrogen peroxide production by muscle mitochondria assessed ex vivo under conditions mimicking rest and exercise. J Biol Chem 290(1):209–227. https://doi.org/10.1074/jbc.M114.619072
Quinlan CL, Orr AL, Perevoshchikova IV, Treberg JR, Ackrell BA, Brand MD (2012) Mitochondrial complex II can generate reactive oxygen species at high rates in both the forward and reverse reactions. J Biol Chem 287(32):27255–27264. https://doi.org/10.1074/jbc.M112.374629
Brand MD (2016) Mitochondrial generation of superoxide and hydrogen peroxide as the source of mitochondrial redox signaling. Free Radic Biol Med. https://doi.org/10.1016/j.freeradbiomed.2016.04.001
Sun QA, Hess DT, Nogueira L, Yong S, Bowles DE, Eu J, Laurita KR, Meissner G, Stamler JS (2011) Oxygen-coupled redox regulation of the skeletal muscle ryanodine receptor-Ca2+ release channel by NADPH oxidase 4. Proc Natl Acad Sci U S A 108(38):16098–16103. https://doi.org/10.1073/pnas.1109546108
Gomez-Cabrera MC, Close GL, Kayani A, McArdle A, Vina J, Jackson MJ (2010) Effect of xanthine oxidase-generated extracellular superoxide on skeletal muscle force generation. Am J Physiol Regul Integr Comp Physiol 298(1):R2–R8. doi:00142.2009 [pii]. https://doi.org/10.1152/ajpregu.00142.2009
Hellsten Y, Frandsen U, Orthenblad N, Sjodin B, Richter EA (1997) Xanthine oxidase in human skeletal muscle following eccentric exercise: a role in inflammation. J Physiol 498(Pt 1):239–248
Zuo L, Christofi FL, Wright VP, Bao S, Clanton TL (2004) Lipoxygenase-dependent superoxide release in skeletal muscle. J Appl Physiol 97(2):661–668. https://doi.org/10.1152/japplphysiol.00096.2004 00096.2004 [pii]
Gong MC, Arbogast S, Guo Z, Mathenia J, Su W, Reid MB (2006) Calcium-independent phospholipase A2 modulates cytosolic oxidant activity and contractile function in murine skeletal muscle cells. J Appl Physiol 100(2):399–405. doi:00873.2005 [pii]. https://doi.org/10.1152/japplphysiol.00873.2005
Nethery D, Stofan D, Callahan L, DiMarco A, Supinski G (1999) Formation of reactive oxygen species by the contracting diaphragm is PLA(2) dependent. J Appl Physiol 87(2):792–800
Sakellariou GK, Jackson MJ, Vasilaki A (2014) Redefining the major contributors to superoxide production in contracting skeletal muscle. The role of NAD(P)H oxidases. Free Radical Res 48(1):12–29. https://doi.org/10.3109/10715762.2013.830718
Moncada S, Palmer RM, Higgs EA (1991) Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacol Rev 43(2):109–142
Reid MB (1998) Role of nitric oxide in skeletal muscle: synthesis, distribution and functional importance. Acta Physiol Scand 162(3):401–409. https://doi.org/10.1046/j.1365-201X.1998.0303f.x
Allen DG, Whitehead NP, Froehner SC (2016) Absence of dystrophin disrupts skeletal muscle signaling: roles of ca2+, reactive oxygen species, and nitric oxide in the development of muscular dystrophy. Physiol Rev 96(1):253–305. https://doi.org/10.1152/physrev.00007.2015
Garcia-Cardena G, Fan R, Shah V, Sorrentino R, Cirino G, Papapetropoulos A, Sessa WC (1998) Dynamic activation of endothelial nitric oxide synthase by Hsp90. Nature 392(6678):821–824. https://doi.org/10.1038/33934
Rigamonti E, Touvier T, Clementi E, Manfredi AA, Brunelli S, Rovere-Querini P (2013) Requirement of inducible nitric oxide synthase for skeletal muscle regeneration after acute damage. J Immunol 190(4):1767–1777. https://doi.org/10.4049/jimmunol.1202903
Adams V, Nehrhoff B, Spate U, Linke A, Schulze PC, Baur A, Gielen S, Hambrecht R, Schuler G (2002) Induction of iNOS expression in skeletal muscle by IL-1beta and NFkappaB activation: an in vitro and in vivo study. Cardiovasc Res 54(1):95–104
Tidball JG, Spencer MJ, Wehling M, Lavergne E (1999) Nitric-oxide synthase is a mechanical signal transducer that modulates talin and vinculin expression. J Biol Chem 274(46):33155–33160
Hirschfield W, Moody MR, O’Brien WE, Gregg AR, Bryan RM Jr, Reid MB (2000) Nitric oxide release and contractile properties of skeletal muscles from mice deficient in type III NOS. Am J Physiol Regul Integr Comp Physiol 278(1):R95–R100
Pye D, Palomero J, Kabayo T, Jackson MJ (2007) Real-time measurement of nitric oxide in single mature mouse skeletal muscle fibres during contractions. J Physiol 581(Pt 1):309–318. doi:jphysiol.2006.125930 [pii]. https://doi.org/10.1113/jphysiol.2006.125930
Tidball JG, Wehling-Henricks M (2004) Expression of a NOS transgene in dystrophin-deficient muscle reduces muscle membrane damage without increasing the expression of membrane-associated cytoskeletal proteins. Mol Genet Metab 82(4):312–320. https://doi.org/10.1016/j.ymgme.2004.06.006
Brenman JE, Chao DS, Xia H, Aldape K, Bredt DS (1995) Nitric oxide synthase complexed with dystrophin and absent from skeletal muscle sarcolemma in Duchenne muscular dystrophy. Cell 82(5):743–752
Stamler JS, Meissner G (2001) Physiology of nitric oxide in skeletal muscle. Physiol Rev 81(1):209–237
Marinho HS, Real C, Cyrne L, Soares H, Antunes F (2014) Hydrogen peroxide sensing, signaling and regulation of transcription factors. Redox Biol 2:535–562. https://doi.org/10.1016/j.redox.2014.02.006
Jackson MJ, McArdle A (2016) Role of reactive oxygen species in age-related neuromuscular deficits. J Physiol. https://doi.org/10.1113/JP270564
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J (2007) Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol 39(1):44–84. doi:S1357-2725(06)00219-6 [pii]. https://doi.org/10.1016/j.biocel.2006.07.001
Takac I, Schroder K, Zhang L, Lardy B, Anilkumar N, Lambeth JD, Shah AM, Morel F, Brandes RP (2011) The E-loop is involved in hydrogen peroxide formation by the NADPH oxidase Nox4. J Biol Chem 286(15):13304–13313. https://doi.org/10.1074/jbc.M110.192138
Koziel R, Pircher H, Kratochwil M, Lener B, Hermann M, Dencher NA, Jansen-Durr P (2013) Mitochondrial respiratory chain complex I is inactivated by NADPH oxidase Nox4. Biochem J 452(2):231–239. https://doi.org/10.1042/BJ20121778
Halliwell B, Clement MV, Long LH (2000) Hydrogen peroxide in the human body. FEBS Lett 486(1):10–13
Mehmeti I, Lortz S, Lenzen S (2012) The H2O2-sensitive HyPer protein targeted to the endoplasmic reticulum as a mirror of the oxidizing thiol-disulfide milieu. Free Radic Biol Med 53(7):1451–1458. https://doi.org/10.1016/j.freeradbiomed.2012.08.010
Ramming T, Okumura M, Kanemura S, Baday S, Birk J, Moes S, Spiess M, Jeno P, Berneche S, Inaba K, Appenzeller-Herzog C (2015) A PDI-catalyzed thiol-disulfide switch regulates the production of hydrogen peroxide by human Ero1. Free Radic Biol Med 83:361–372. https://doi.org/10.1016/j.freeradbiomed.2015.02.011
Sigel A, Sigel H, Sigel RKO (2013) Interrelations between essential metal ions and human diseases. Springer
Murphy RM, Dutka TL, Lamb GD (2008) Hydroxyl radical and glutathione interactions alter calcium sensitivity and maximum force of the contractile apparatus in rat skeletal muscle fibres. J Physiol 586(8):2203–2216. https://doi.org/10.1113/jphysiol.2007.150516
Imlay JA (2014) The mismetallation of enzymes during oxidative stress. J Biol Chem 289(41):28121–28128. https://doi.org/10.1074/jbc.R114.588814
Kehrer JP (2000) The Haber-Weiss reaction and mechanisms of toxicity. Toxicology 149(1):43–50
O’Neill CA, Stebbins CL, Bonigut S, Halliwell B, Longhurst JC (1996) Production of hydroxyl radicals in contracting skeletal muscle of cats. J Appl Physiol 81(3):1197–1206
Konno S (2005) Hydroxyl radical formation in skeletal muscle of rats with glucocorticoid-induced myopathy. Neurochem Res 30(5):669–675
Kondo H, Nishino K, Itokawa Y (1994) Hydroxyl radical generation in skeletal muscle atrophied by immobilization. FEBS Lett 349(2):169–172
Pacher P, Beckman JS, Liaudet L (2007) Nitric oxide and peroxynitrite in health and disease. Physiol Rev 87(1):315–424. https://doi.org/10.1152/physrev.00029.2006
Radi R, Beckman JS, Bush KM, Freeman BA (1991) Peroxynitrite oxidation of sulfhydryls. The cytotoxic potential of superoxide and nitric oxide. J Biol Chem 266(7):4244–4250
Powers SK, Ji LL, Kavazis AN, Jackson MJ (2011) Reactive oxygen species: impact on skeletal muscle. Compr Physiol 1(2):941–969. https://doi.org/10.1002/cphy.c100054
Greenacre SA, Ischiropoulos H (2001) Tyrosine nitration: localisation, quantification, consequences for protein function and signal transduction. Free Radic Res 34(6):541–581
Montagna C, Di Giacomo G, Rizza S, Cardaci S, Ferraro E, Grumati P, De Zio D, Maiani E, Muscoli C, Lauro F, Ilari S, Bernardini S, Cannata S, Gargioli C, Ciriolo MR, Cecconi F, Bonaldo P, Filomeni G (2014) S-nitrosoglutathione reductase deficiency-induced S-nitrosylation results in neuromuscular dysfunction. Antioxid Redox Signal 21(4):570–587. https://doi.org/10.1089/ars.2013.5696
Vasilaki A, Simpson D, McArdle F, McLean L, Beynon RJ, Van Remmen H, Richardson AG, McArdle A, Faulkner JA, Jackson MJ (2007) Formation of 3-nitrotyrosines in carbonic anhydrase III is a sensitive marker of oxidative stress in skeletal muscle. Proteomics Clin Appl 1(4):362–372. https://doi.org/10.1002/prca.200600702
Sakellariou GK, Lightfoot AP, Earl KE, Stofanko M, McDonagh B (2017) Redox homeostasis and age-related deficits in neuromuscular integrity and function. J Cachexia Sarcopenia Muscle 8(6):881–906. https://doi.org/10.1002/jcsm.12223
Jackson MJ (2011) Control of reactive oxygen species production in contracting skeletal muscle. Antioxid Redox Signal 15(9):2477–2486. https://doi.org/10.1089/ars.2011.3976
Radak Z (2000) Free Radicals in exercise and aging. Human Kinetics, Champaign
Kirkman HN, Gaetani GF (2007) Mammalian catalase: a venerable enzyme with new mysteries. Trends Biochem Sci 32(1):44–50. https://doi.org/10.1016/j.tibs.2006.11.003
Pereira B, Costa Rosa LF, Safi DA, Medeiros MH, Curi R, Bechara EJ (1994) Superoxide dismutase, catalase, and glutathione peroxidase activities in muscle and lymphoid organs of sedentary and exercise-trained rats. Physiol Behav 56(5):1095–1099
Fuchs J, Podda M, Packer L (2003) Redox-genome interactions in health and disease. Taylor & Francis
Lawler JM, Powers SK (1998) Oxidative stress, antioxidant status, and the contracting diaphragm. Can J Appl Physiol 23(1):23–55
Landis GN, Tower J (2005) Superoxide dismutase evolution and life span regulation. Mech Ageing Dev 126(3):365–379. https://doi.org/10.1016/j.mad.2004.08.012
Brigelius-Flohe R (1999) Tissue-specific functions of individual glutathione peroxidases. Free Radic Biol Med 27(9-10):951–965
Frey RS, Ushio-Fukai M, Malik AB (2009) NADPH oxidase-dependent signaling in endothelial cells: role in physiology and pathophysiology. Antioxid Redox signal 11(4):791–810. https://doi.org/10.1089/ARS.2008.2220
Jin RC, Mahoney CE, Coleman Anderson L, Ottaviano F, Croce K, Leopold JA, Zhang YY, Tang SS, Handy DE, Loscalzo J (2011) Glutathione peroxidase-3 deficiency promotes platelet-dependent thrombosis in vivo. Circulation 123(18):1963–1973. https://doi.org/10.1161/CIRCULATIONAHA.110.000034
Olson GE, Whitin JC, Hill KE, Winfrey VP, Motley AK, Austin LM, Deal J, Cohen HJ, Burk RF (2010) Extracellular glutathione peroxidase (Gpx3) binds specifically to basement membranes of mouse renal cortex tubule cells. Am J Physiol Renal Physiol 298(5):F1244–F1253. https://doi.org/10.1152/ajprenal.00662.2009
Brigelius-Flohe R (2006) Glutathione peroxidases and redox-regulated transcription factors. Biol Chem 387(10-11):1329–1335. https://doi.org/10.1515/BC.2006.166
Williams K, Frayne J, Hall L (1998) Expression of extracellular glutathione peroxidase type 5 (GPX5) in the rat male reproductive tract. Mol Hum Reprod 4(9):841–848
Moscow JA, Morrow CS, He R, Mullenbach GT, Cowan KH (1992) Structure and function of the 5’-flanking sequence of the human cytosolic selenium-dependent glutathione peroxidase gene (hgpx1). J Biol Chem 267(9):5949–5958
Mates JM, Sanchez-Jimenez F (1999) Antioxidant enzymes and their implications in pathophysiologic processes. Front Biosci 4:D339–D345
Chae HZ, Kim IH, Kim K, Rhee SG (1993) Cloning, sequencing, and mutation of thiol-specific antioxidant gene of Saccharomyces cerevisiae. J Biol Chem 268(22):16815–16821
Kim K, Kim IH, Lee KY, Rhee SG, Stadtman ER (1988) The isolation and purification of a specific “protector” protein which inhibits enzyme inactivation by a thiol/Fe(III)/O2 mixed-function oxidation system. J Biol Chem 263(10):4704–4711
Kim K, Rhee SG, Stadtman ER (1985) Nonenzymatic cleavage of proteins by reactive oxygen species generated by dithiothreitol and iron. J Biol Chem 260(29):15394–15397
Wood ZA, Schroder E, Robin Harris J, Poole LB (2003) Structure, mechanism and regulation of peroxiredoxins. Trends Biochem Sci 28(1):32–40
Rhee SG, Chae HZ, Kim K (2005) Peroxiredoxins: a historical overview and speculative preview of novel mechanisms and emerging concepts in cell signaling. Free Radic Biol Med 38(12):1543–1552. doi:S0891-5849(05)00098-5 [pii]. https://doi.org/10.1016/j.freeradbiomed.2005.02.026
Dubuisson M, Vander Stricht D, Clippe A, Etienne F, Nauser T, Kissner R, Koppenol WH, Rees JF, Knoops B (2004) Human peroxiredoxin 5 is a peroxynitrite reductase. FEBS Lett 571(1-3):161–165. https://doi.org/10.1016/j.febslet.2004.06.080
Wadley AJ, Aldred S, Coles SJ (2015) An unexplored role for Peroxiredoxin in exercise-induced redox signalling? Redox Biol 8:51–58. https://doi.org/10.1016/j.redox.2015.10.003
McDonagh B, Sakellariou GK, Smith NT, Brownridge P, Jackson MJ (2014) Differential cysteine labeling and global label-free proteomics reveals an altered metabolic state in skeletal muscle aging. J Proteome Res 13(11):5008–5021. https://doi.org/10.1021/pr5006394
Berndt C, Lillig CH, Holmgren A (2007) Thiol-based mechanisms of the thioredoxin and glutaredoxin systems: implications for diseases in the cardiovascular system. Am J Physiol Heart Circ Physiol 292(3):H1227–H1236. https://doi.org/10.1152/ajpheart.01162.2006
Hanschmann EM, Godoy JR, Berndt C, Hudemann C, Lillig CH (2013) Thioredoxins, glutaredoxins, and peroxiredoxins--molecular mechanisms and health significance: from cofactors to antioxidants to redox signaling. Antioxid Redox Signal 19(13):1539–1605. https://doi.org/10.1089/ars.2012.4599
Hanschmann EM, Lonn ME, Schutte LD, Funke M, Godoy JR, Eitner S, Hudemann C, Lillig CH (2010) Both thioredoxin 2 and glutaredoxin 2 contribute to the reduction of the mitochondrial 2-Cys peroxiredoxin Prx3. J Biol Chem 285(52):40699–40705. https://doi.org/10.1074/jbc.M110.185827
Murata H, Ihara Y, Nakamura H, Yodoi J, Sumikawa K, Kondo T (2003) Glutaredoxin exerts an antiapoptotic effect by regulating the redox state of Akt. J Biol Chem 278(50):50226–50233. https://doi.org/10.1074/jbc.M310171200
Daily D, Vlamis-Gardikas A, Offen D, Mittelman L, Melamed E, Holmgren A, Barzilai A (2001) Glutaredoxin protects cerebellar granule neurons from dopamine-induced apoptosis by activating NF-kappa B via Ref-1. J Biol Chem 276(2):1335–1344. https://doi.org/10.1074/jbc.M008121200
Pan S, Berk BC (2007) Glutathiolation regulates tumor necrosis factor-alpha-induced caspase-3 cleavage and apoptosis: key role for glutaredoxin in the death pathway. Circ Res 100(2):213–219. https://doi.org/10.1161/01.RES.0000256089.30318.20
Rodriguez-Manzaneque MT, Tamarit J, Belli G, Ros J, Herrero E (2002) Grx5 is a mitochondrial glutaredoxin required for the activity of iron/sulfur enzymes. Mol Biol Cell 13(4):1109–1121. https://doi.org/10.1091/mbc.01-10-0517
Lonn ME, Hudemann C, Berndt C, Cherkasov V, Capani F, Holmgren A, Lillig CH (2008) Expression pattern of human glutaredoxin 2 isoforms: identification and characterization of two testis/cancer cell-specific isoforms. Antioxid Redox Signal 10(3):547–557. https://doi.org/10.1089/ars.2007.1821
Johansson C, Roos AK, Montano SJ, Sengupta R, Filippakopoulos P, Guo K, von Delft F, Holmgren A, Oppermann U, Kavanagh KL (2011) The crystal structure of human GLRX5: iron-sulfur cluster co-ordination, tetrameric assembly and monomer activity. Biochem J 433(2):303–311. https://doi.org/10.1042/BJ20101286
Beer SM, Taylor ER, Brown SE, Dahm CC, Costa NJ, Runswick MJ, Murphy MP (2004) Glutaredoxin 2 catalyzes the reversible oxidation and glutathionylation of mitochondrial membrane thiol proteins: implications for mitochondrial redox regulation and antioxidant DEFENSE. J Biol Chem 279(46):47939–47951. https://doi.org/10.1074/jbc.M408011200
Kozakowska M, Pietraszek-Gremplewicz K, Jozkowicz A, Dulak J (2015) The role of oxidative stress in skeletal muscle injury and regeneration: focus on antioxidant enzymes. J Muscle Res Cell Motil 36(6):377–393. https://doi.org/10.1007/s10974-015-9438-9
Theodorou AA, Nikolaidis MG, Paschalis V, Sakellariou GK, Fatouros IG, Koutedakis Y, Jamurtas AZ (2010) Comparison between glucose-6-phosphate dehydrogenase-deficient and normal individuals after eccentric exercise. Med Sci Sports Exerc 42(6):1113–1121. https://doi.org/10.1249/MSS.0b013e3181c67ecd
Gomes EC, Silva AN, de Oliveira MR (2012) Oxidants, antioxidants, and the beneficial roles of exercise-induced production of reactive species. Oxid Med Cell Longev 2012:756132. https://doi.org/10.1155/2012/756132
Sen C, Packer L, Hänninen O (2000) Handbook of oxidants and antioxidants in exercise. Elsevier Science
Cobley JN, Sakellariou GK, Murray S, Waldron S, Gregson W, Burniston JG, Morton JP, Iwanejko LA, Close GL (2013) Lifelong endurance training attenuates age-related genotoxic stress in human skeletal muscle. Longevity & Healthspan 2(1):11. https://doi.org/10.1186/2046-2395-2-11
Cobley JN, Sakellariou GK, Owens DJ, Murray S, Waldron S, Gregson W, Fraser WD, Burniston JG, Iwanejko LA, McArdle A, Morton JP, Jackson MJ, Close GL (2014) Lifelong training preserves some redox-regulated adaptive responses after an acute exercise stimulus in aged human skeletal muscle. Free Radic Biol Med 70:23–32. https://doi.org/10.1016/j.freeradbiomed.2014.02.004
Mecocci P, Fano G, Fulle S, MacGarvey U, Shinobu L, Polidori MC, Cherubini A, Vecchiet J, Senin U, Beal MF (1999) Age-dependent increases in oxidative damage to DNA, lipids, and proteins in human skeletal muscle. Free Radic Biol Med 26(3-4):303–308
Broome CS, Kayani AC, Palomero J, Dillmann WH, Mestril R, Jackson MJ, McArdle A (2006) Effect of lifelong overexpression of HSP70 in skeletal muscle on age-related oxidative stress and adaptation after nondamaging contractile activity. FASEB J 20(9):1549–1551. https://doi.org/10.1096/fj.05-4935fje
Lee HY, Choi CS, Birkenfeld AL, Alves TC, Jornayvaz FR, Jurczak MJ, Zhang D, Woo DK, Shadel GS, Ladiges W, Rabinovitch PS, Santos JH, Petersen KF, Samuel VT, Shulman GI (2010) Targeted expression of catalase to mitochondria prevents age-associated reductions in mitochondrial function and insulin resistance. Cell Metab 12(6):668–674. https://doi.org/10.1016/j.cmet.2010.11.004
McDonagh B, Sakellariou GK, Jackson MJ (2014) Application of redox proteomics to skeletal muscle aging and exercise. Biochem Soc Trans 42(4):965–970. https://doi.org/10.1042/BST20140085
Wang AL, Lukas TJ, Yuan M, Neufeld AH (2010) Age-related increase in mitochondrial DNA damage and loss of DNA repair capacity in the neural retina. Neurobiol Aging 31(11):2002–2010. https://doi.org/10.1016/j.neurobiolaging.2008.10.019
Miro O, Casademont J, Casals E, Perea M, Urbano-Marquez A, Rustin P, Cardellach F (2000) Aging is associated with increased lipid peroxidation in human hearts, but not with mitochondrial respiratory chain enzyme defects. Cardiovasc Res 47(3):624–631
Rosa EF, Silva AC, Ihara SS, Mora OA, Aboulafia J (1985) Nouailhetas VL (2005) Habitual exercise program protects murine intestinal, skeletal, and cardiac muscles against aging. J Appl Physiol 99(4):1569–1575. https://doi.org/10.1152/japplphysiol.00417.2005
Simic MG (1992) The rate of DNA damage and aging. In: Free radicals and aging. Verlag, Birkhauser
Cutler RG (1991) Human longevity and aging: possible role of reactive oxygen species. Ann N Y Acad Sci 621:1–28
Miquel J, Ramirez-Bosca A, Soler A, Diez A, Carrion-Gutierrez MA, Diaz-Alperi J, Quintanilla-Ripoll E, Bernd A, Quintanilla-Almagro E (1998) Increase with age of serum lipid peroxides: implications for the prevention of atherosclerosis. Mech Ageing Dev 100(1):17–24
McDonagh B, Sakellariou GK, Smith NT, Brownridge P, Jackson MJ (2014a) Differential cysteine labeling and global label-free proteomics reveals an altered metabolic state in skeletal muscle aging. J Proteome Res 13(11):5008–5021. https://doi.org/10.1021/pr5006394
McDonagh B, Sakellariou GK, Jackson MJ (2014b) Application of redox proteomics to skeletal muscle aging and exercise. Biochem Soc Trans 42(4):965–970. https://doi.org/10.1042/BST20140085
Palomero J, Vasilaki A, Pye D, McArdle A, Jackson MJ (2013) Aging increases the oxidation of dichlorohydrofluorescein in single isolated skeletal muscle fibers at rest, but not during contractions. Am J Physiol Regul Integr Comp Physiol. https://doi.org/10.1152/ajpregu.00530.2012
Sakellariou GK, Pearson T, Lightfoot AP, Nye GA, Wells N, Giakoumaki II, Vasilaki A, Griffiths RD, Jackson MJ, McArdle A (2016) Mitochondrial ROS regulate oxidative damage and mitophagy but not age-related muscle fiber atrophy. Sci Rep 6:33944. https://doi.org/10.1038/srep33944
Ivannikov MV, Van Remmen H (2015) Sod1 gene ablation in adult mice leads to physiological changes at the neuromuscular junction similar to changes that occur in old wild-type mice. Free Radic Biol Med 84:254–262. https://doi.org/10.1016/j.freeradbiomed.2015.03.021
Jang YC, Lustgarten MS, Liu Y, Muller FL, Bhattacharya A, Liang H, Salmon AB, Brooks SV, Larkin L, Hayworth CR, Richardson A, Van Remmen H (2010) Increased superoxide in vivo accelerates age-associated muscle atrophy through mitochondrial dysfunction and neuromuscular junction degeneration. FASEB J 24(5):1376–1390. https://doi.org/10.1096/fj.09-146308
Larkin LM, Davis CS, Sims-Robinson C, Kostrominova TY, Remmen HV, Richardson A, Feldman EL, Brooks SV (2011) Skeletal muscle weakness due to deficiency of CuZn-superoxide dismutase is associated with loss of functional innervation. Am J Physiol Regul Integr Comp Physiol 301(5):R1400–R1407. https://doi.org/10.1152/ajpregu.00093.2011
Muller FL, Song W, Liu Y, Chaudhuri A, Pieke-Dahl S, Strong R, Huang TT, Epstein CJ, Roberts LJ 2nd, Csete M, Faulkner JA, Van Remmen H (2006) Absence of CuZn superoxide dismutase leads to elevated oxidative stress and acceleration of age-dependent skeletal muscle atrophy. Free Radic Biol Med 40(11):1993–2004. https://doi.org/10.1016/j.freeradbiomed.2006.01.036
Vasilaki A, van der Meulen JH, Larkin L, Harrison DC, Pearson T, Van Remmen H, Richardson A, Brooks SV, Jackson MJ, McArdle A (2010) The age-related failure of adaptive responses to contractile activity in skeletal muscle is mimicked in young mice by deletion of Cu,Zn superoxide dismutase. Aging Cell 9(6):979–990. https://doi.org/10.1111/j.1474-9726.2010.00635.x
Sakellariou GK, Davis CS, Shi Y, Ivannikov MV, Zhang Y, Vasilaki A, Macleod GT, Richardson A, Van Remmen H, Jackson MJ, McArdle A, Brooks SV (2014) Neuron-specific expression of CuZnSOD prevents the loss of muscle mass and function that occurs in homozygous CuZnSOD-knockout mice. FASEB J 28(4):1666–1681. https://doi.org/10.1096/fj.13-240390
Sataranatarajan K, Qaisar R, Davis C, Sakellariou GK, Vasilaki A, Zhang Y, Liu Y, Bhaskaran S, McArdle A, Jackson M, Brooks SV, Richardson A, Van Remmen H (2015) Neuron specific reduction in CuZnSOD is not sufficient to initiate a full sarcopenia phenotype. Redox Biol 5:140–148. https://doi.org/10.1016/j.redox.2015.04.005
Zhang Y, Davis C, Sakellariou GK, Shi Y, Kayani AC, Pulliam D, Bhattacharya A, Richardson A, Jackson MJ, McArdle A, Brooks SV, Van Remmen H (2013) CuZnSOD gene deletion targeted to skeletal muscle leads to loss of contractile force but does not cause muscle atrophy in adult mice. FASEB J. https://doi.org/10.1096/fj.13-228130
Shi Y, Ivannikov MV, Walsh ME, Liu Y, Zhang Y, Jaramillo CA, Macleod GT, Van Remmen H (2014) The lack of CuZnSOD leads to impaired neurotransmitter release, neuromuscular junction destabilization and reduced muscle strength in mice. PLoS One 9(6):e100834. https://doi.org/10.1371/journal.pone.0100834
Sun QA, Wang B, Miyagi M, Hess DT, Stamler JS (2013) Oxygen-coupled redox regulation of the skeletal muscle ryanodine receptor/Ca2+ release channel (RyR1): sites and nature of oxidative modification. J Biol Chem 288(32):22961–22971. https://doi.org/10.1074/jbc.M113.480228
Tong X, Hou X, Jourd’heuil D, Weisbrod RM, Cohen RA (2010) Upregulation of Nox4 by TGF{beta}1 oxidizes SERCA and inhibits NO in arterial smooth muscle of the prediabetic Zucker rat. Circ Res 107(8):975–983. https://doi.org/10.1161/CIRCRESAHA.110.221242
McDonagh B, Sakellariou GK, Smith NT, Brownridge P, Jackson MJ (2015) Redox proteomic analysis of the gastrocnemius muscle from adult and old mice. Data Brief 4:344–348. https://doi.org/10.1016/j.dib.2015.06.012
Kramer PA, Duan J, Qian WJ, Marcinek DJ (2015) The measurement of reversible redox dependent post-translational modifications and their regulation of mitochondrial and skeletal muscle function. Front Physiol 6:347. https://doi.org/10.3389/fphys.2015.00347
Labunskyy VM, Gladyshev VN (2012) Role of reactive oxygen species-mediated signaling in aging. Antioxid Redox Signal. https://doi.org/10.1089/ars.2012.4891
Egan B, Zierath JR (2013) Exercise metabolism and the molecular regulation of skeletal muscle adaptation. Cell Metab 17(2):162–184. https://doi.org/10.1016/j.cmet.2012.12.012
Aachmann FL, Sal LS, Kim HY, Marino SM, Gladyshev VN, Dikiy A (2010) Insights into function, catalytic mechanism, and fold evolution of selenoprotein methionine sulfoxide reductase B1 through structural analysis. J Biol Chem 285(43):33315–33323. https://doi.org/10.1074/jbc.M110.132308
Calabrese V, Sultana R, Scapagnini G, Guagliano E, Sapienza M, Bella R, Kanski J, Pennisi G, Mancuso C, Stella AM, Butterfield DA (2006) Nitrosative stress, cellular stress response, and thiol homeostasis in patients with Alzheimer’s disease. Antioxid Redox Signal 8(11–12):1975–1986. https://doi.org/10.1089/ars.2006.8.1975
Smuder AJ, Kavazis AN, Hudson MB, Nelson WB, Powers SK (2010) Oxidation enhances myofibrillar protein degradation via calpain and caspase-3. Free Radic Biol Med 49(7):1152–1160. https://doi.org/10.1016/j.freeradbiomed.2010.06.025
Pinto JR, de Sousa VP, Sorenson MM (2011) Redox state of troponin C cysteine in the D/E helix alters the C-domain affinity for the thin filament of vertebrate striated muscle. Biochim Biophys Acta 1810(4):391–397. https://doi.org/10.1016/j.bbagen.2010.11.008
Coirault C, Guellich A, Barbry T, Samuel JL, Riou B, Lecarpentier Y (2007) Oxidative stress of myosin contributes to skeletal muscle dysfunction in rats with chronic heart failure. Am J Physiol Heart Circ Physiol 292(2):H1009–H1017. https://doi.org/10.1152/ajpheart.00438.2006
Li M, Ogilvie H, Ochala J, Artemenko K, Iwamoto H, Yagi N, Bergquist J, Larsson L (2015) Aberrant post-translational modifications compromise human myosin motor function in old age. Aging Cell 14(2):228–235. https://doi.org/10.1111/acel.12307
Prochniewicz E, Spakowicz D, Thomas DD (2008) Changes in actin structural transitions associated with oxidative inhibition of muscle contraction. Biochemistry 47(45):11811–11817. https://doi.org/10.1021/bi801080x
Andrade FH, Reid MB, Allen DG, Westerblad H (1998) Effect of hydrogen peroxide and dithiothreitol on contractile function of single skeletal muscle fibres from the mouse. J Physiol 509(Pt 2):565–575
Tisdale MJ (2009) Mechanisms of cancer cachexia. Physiol Rev 89(2):381–410. https://doi.org/10.1152/physrev.00016.2008
Maltais F, Decramer M, Casaburi R, Barreiro E, Burelle Y, Debigare R, Dekhuijzen PN, Franssen F, Gayan-Ramirez G, Gea J, Gosker HR, Gosselink R, Hayot M, Hussain SN, Janssens W, Polkey MI, Roca J, Saey D, Schols AM, Spruit MA, Steiner M, Taivassalo T, Troosters T, Vogiatzis I, Wagner PD, COPD AEAHCoLMDi (2014) An official American Thoracic Society/European Respiratory Society statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 189(9):e15–e62. https://doi.org/10.1164/rccm.201402-0373ST
Powers SK, Morton AB, Ahn B, Smuder AJ (2016) Redox control of skeletal muscle atrophy. Free Radic Biol Med. https://doi.org/10.1016/j.freeradbiomed.2016.02.021
Rodney GG, Pal R, Abo-Zahrah R (2016) Redox regulation of autophagy in skeletal muscle. Free Radic Biol Med 98:103–112. https://doi.org/10.1016/j.freeradbiomed.2016.05.010
Romanello V, Sandri M (2015) Mitochondrial quality control and muscle mass maintenance. Front Physiol 6:422. https://doi.org/10.3389/fphys.2015.00422
Vasilaki A, McArdle F, Iwanejko LM, McArdle A (2006) Adaptive responses of mouse skeletal muscle to contractile activity: the effect of age. Mech Ageing Dev 127(11):830–839. https://doi.org/10.1016/j.mad.2006.08.004
Ristow M, Zarse K, Oberbach A, Kloting N, Birringer M, Kiehntopf M, Stumvoll M, Kahn CR, Bluher M (2009) Antioxidants prevent health-promoting effects of physical exercise in humans. Proc Natl Acad Sci U S A 106(21):8665–8670. https://doi.org/10.1073/pnas.0903485106
Jackson MJ (2016) Reactive oxygen species in sarcopenia: Should we focus on excess oxidative damage or defective redox signalling? Mol Aspects Med 50:33–40. https://doi.org/10.1016/j.mam.2016.05.002
Schiaffino S, Dyar KA, Ciciliot S, Blaauw B, Sandri M (2013) Mechanisms regulating skeletal muscle growth and atrophy. FEBS J 280(17):4294–4314. https://doi.org/10.1111/febs.12253
Tan PL, Shavlakadze T, Grounds MD, Arthur PG (2015) Differential thiol oxidation of the signaling proteins Akt, PTEN or PP2A determines whether Akt phosphorylation is enhanced or inhibited by oxidative stress in C2C12 myotubes derived from skeletal muscle. Int J Biochem Cell Biol 62:72–79. https://doi.org/10.1016/j.biocel.2015.02.015
Hudson MB, Smuder AJ, Nelson WB, Wiggs MP, Shimkus KL, Fluckey JD, Szeto HH, Powers SK (2015) Partial support ventilation and mitochondrial-targeted antioxidants protect against ventilator-induced decreases in diaphragm muscle protein synthesis. PLoS One 10(9):e0137693. https://doi.org/10.1371/journal.pone.0137693
Kim RJ, Hah YS, Sung CM, Kang JR, Park HB (2014) Do antioxidants inhibit oxidative-stress-induced autophagy of tenofibroblasts? J Orthop Res 32(7):937–943. https://doi.org/10.1002/jor.22608
Scherz-Shouval R, Shvets E, Fass E, Shorer H, Gil L, Elazar Z (2007) Reactive oxygen species are essential for autophagy and specifically regulate the activity of Atg4. EMBO J 26(7):1749–1760. https://doi.org/10.1038/sj.emboj.7601623
Betters JL, Criswell DS, Shanely RA, Van Gammeren D, Falk D, Deruisseau KC, Deering M, Yimlamai T, Powers SK (2004) Trolox attenuates mechanical ventilation-induced diaphragmatic dysfunction and proteolysis. Am J Respir Crit Care Med 170(11):1179–1184. https://doi.org/10.1164/rccm.200407-939OC
Dargelos E, Brule C, Stuelsatz P, Mouly V, Veschambre P, Cottin P, Poussard S (2010) Up-regulation of calcium-dependent proteolysis in human myoblasts under acute oxidative stress. Exp Cell Res 316(1):115–125. https://doi.org/10.1016/j.yexcr.2009.07.025
Choi MH, Ow JR, Yang ND, Taneja R (2016) Oxidative stress-mediated skeletal muscle degeneration: molecules, mechanisms, and therapies. Oxid Med Cell Longev 2016:6842568. https://doi.org/10.1155/2016/6842568
Competing Financial Interests
The authors declare no competing financial interests.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Sakellariou, G.K., McDonagh, B. (2018). Redox Homeostasis in Age-Related Muscle Atrophy. In: Xiao, J. (eds) Muscle Atrophy. Advances in Experimental Medicine and Biology, vol 1088. Springer, Singapore. https://doi.org/10.1007/978-981-13-1435-3_13
Download citation
DOI: https://doi.org/10.1007/978-981-13-1435-3_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-13-1434-6
Online ISBN: 978-981-13-1435-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)