Abstract
Blood flow oscillations of 0.001–0.2 Hz are called vasomotion whose physiological mechanism has not been understood. This vasomotion can mirror human body conditions and initiate the pathogenesis sequence in some diseases. In the preliminary measurement of blood flow oscillations in radial artery at the wrist, a strong power spectral density (PSD) at ~0.1 Hz was found, indicating that low frequency flow oscillations play a dominate role in radial pulse pattern. To understand the interaction between vasomotion and cardiac rhythm in radial artery, numerical simulations were carried out. It is found that the natural frequency of the system decreases with the complexity of microvasculature system, and the inlet oscillating velocity interacts with the natural frequency to generate subharmonics. As the natural frequency in the constructed vessel system can be as low as 0.37 Hz, we speculate that the natural frequency of actual microcirculation is much lower, and the mechanism of vasomotion is actually due to the interaction of cardiac rhythm and microvasculature natural frequency.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
The radial stretch of the ascending aorta brought about by left ventricular ejection initiates a pressure wave that is propagated down the aorta and its branches. The typical heart rate is ~1 Hz. However, in our preliminary laser Doppler Flowmetry (LDF) measurement of blood flow oscillation in radial artery at the wrist, we found that the power spectral density (PSD) at 0.001–0.1 Hz is much higher than that at heart rate (Fig. 1a), indicating that low frequency flow oscillations play a dominant role in radial pulse pattern. Spectral intervals of blood flow oscillation are related to several types of activities, ~1 Hz is related to cardiac activity, ~0.3 Hz is related to respiratory activity, and 0.001–0.2 Hz is related to endothelial and myogenic activities. Vasomotion is spontaneous time-dependent contraction and relaxation of micro arteries, and there is evidence that microcirculation may mirror the vascular function of other parts of the body and the microvascular abnormalities may initiate the pathogenesis sequence in some diseases [3]. Thus, the thorough understanding of the interaction between vasomotion related and cardiac activity related pressure waves would enable us to develop novel diagnostic technique. In this research, the experimental and numerical studies are carried out to understand the interaction between vasomotion and cardiac rhythm in radial artery at the wrist, which is an attractive fluid-structure interaction research topic in itself.
2 Methodology
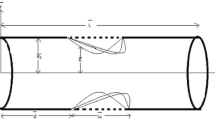
The blood vessel model of the palmar arch is shown as Fig. 1b, the two examples of constructed models are indicated in Fig. 1c, d, and in our simulation the numbers of connected tubes in the Fig. 1d is 5, 6, 8, 16 and 32. The diameter of vessels is set to be 0.02 m. The density of the blood is set as 1050 kg/m3, and dynamic viscosity is 4 × 10−3 kg/m s. The blood is considered as Newtonian fluid, as the current study is focused on the spectral characteristics, and the non-linearity of viscosity does not have significant effect on spectral analysis. The numerical models were built in ANSYS, and were calculated with CFX. The actual velocity waveform was used to simulate the inlet velocity with different frequencies [2]. The no-slip wall boundary condition was adopted. The calculated and measured time series were analyzed by Fast Fourier Transformation (FFT) and morlet wavelet analysis.
3 Results and Discussion
3.1 Natural Frequency of Microvasculature
Every vibration mode has its own characteristic frequency, which depends on the geometry, the mass density, and the tethering of the arterial system [1]. For the vasculature model in Fig. 1c, the root mean square (RMS) of oscillating pressure at different inlet frequencies is tabulated in Table 1. The RMS of oscillating pressure increases dramatically from 1.0 to 1.87 Hz and then decreases gradually, indicating the natural frequency of the vasculature is 1.87 Hz.
Using the same method, the natural frequency of systems in Fig. 1d with different number of connected tubes are investigated. As shown in Fig. 2, the natural frequency is 2.29 Hz for single connected tube, 0.67 Hz for 16 connected tubes, and 0.37 Hz for 32 connected tubes, indicating that the natural frequency decreases with the complexity of the microvasculature. The real human microvasculature is much more complicated than the vasculature in Fig. 1d, therefore, we speculate that the natural frequency of human microvasculature is lower than 0.37 Hz. We wonder if the low frequency vasomotion is due to the interaction between cardiac rhythm and natural frequency of vasculature.
3.2 Interaction Between Inlet Oscillating Velocity and Natural Frequency
Figure 3a, b illustrate the FFT analysis for the 16-connected-tube model with two different inlet frequencies. When the inlet frequency is 0.67 Hz (natural frequency), the PSD is dominant, and the PSD at lower subharmonic frequency is much lower than that at 0.67 Hz. When the inlet frequency is 1.0 Hz, the PSD at lower subharmonic frequency is comparable to that at inlet frequency. To further investigate the effect of inlet frequency on lower subharmonics, we carried out the simulation with various inlet frequencies, i.e., 0.67 Hz, 1.0 Hz, 2.0 Hz, 10 Hz, 25 Hz and 50 Hz, respectively. The ratio of PSD at lower subharmonic frequency to that at inlet frequency is tabulated in Table 2. When the inlet frequencies are far away from the natural frequency, for example at 10, 25 and 50 Hz, the PSD ratio at lower subharmonic is quite low, only 2–5%. When the inlet frequencies are at natural frequency or its harmonic, for example at 0.67 and 2.0 Hz, the PSD ratio at lower subharmonic is about 10%. When the inlet frequency is at 1.0 Hz, the PSD ratio can be 95%. The similar phenomenon can also be found in the cases with 32 and 8 connections These findings indicate that the interaction between inlet oscillating flow and natural frequency of vasculature is very strong, and would affect the flow oscillating pattern.
In real human vasculature, the natural frequency should be lower than 0.37 Hz, the typical inlet frequency is 1.0 Hz, and the interaction between inlet frequency and natural frequency would generate strong oscillation at subharmonic frequencies. As the frequency of vasomotion is 0.001–0.1 Hz, we could speculate that the so-called vasomotion is initiated by the subharmonic oscillation, and this oscillation triggers the myogenic and endothelial activities.
4 Conclusions
The numerical simulation of blood flow in microvasculature has been carried out, and the spectral analysis leads to following conclusion: (i) the natural frequency of vasculature has significant effect on vasomotion at lower frequency; (ii) the natural frequency of the system decreases with the complexity of system; (iii) the interaction between natural frequency and inlet oscillating frequency would generate lower subharmonic oscillation in vasculature which is the mechanism of vasomotion.
References
Lin Wang YY, Jan MY, Shyu CS et al (2004) The natural frequencies of the arterial system and their relation to the heart rate. IEEE Trans Biomed Eng 51(1):193–195
Mills CJ, Gabe IT, Gault JH et al (1970) Pressure-flow relationships and vascular impedance in man. Cardiovasc Res 4(4):405–417
Rossi M, Carpi A, Di Maria C et al (2006) Spectral analysis of laser Doppler skin blood flow oscillations in human essential arterial hypertension. Microvasc Res 72(1–2):34–41
Acknowledgements
Supports given by HKRGC PolyU 5202/13E and PolyU G-YBG9 & G-UACM are gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper
Liu, S.H., Chi, T.X., Tian, S., Su, Z.D., Liu, Y., Luo, X.Y. (2019). Numerical Study of Fluid-Structure Interaction of Microvasculature. In: Zhou, Y., Kimura, M., Peng, G., Lucey, A., Huang, L. (eds) Fluid-Structure-Sound Interactions and Control. FSSIC 2017. Lecture Notes in Mechanical Engineering. Springer, Singapore. https://doi.org/10.1007/978-981-10-7542-1_39
Download citation
DOI: https://doi.org/10.1007/978-981-10-7542-1_39
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-7541-4
Online ISBN: 978-981-10-7542-1
eBook Packages: EngineeringEngineering (R0)