Abstract
Skeletal complications in patients with prostate cancer can result in significant morbidity. There is a relatively high prevalence of bone metastasis and reduction of bone mineral density due to androgen deprivation therapy, and together, these can result in the development of multiple skeletal complications in patients with prostate cancer. The relatively long survival (median, 3–4 years) after bone metastases with multiple skeletal complications makes a significant negative impact on patients’ functional status, quality of life, and social resource utilization. To evaluate skeletal complications, the term “skeletal-related events (SREs)” has frequently been used in most randomized trials conducted previously. SREs usually include pathological bone fracture, spinal cord compression, surgery to bone, and radiotherapy to the bone. Recently, symptomatic skeletal events (SSEs), including only symptomatic events, is the recommended term for use in clinical trials. Local therapies for skeletal complications, such as radiation and surgery, are usually performed to reduce local symptoms, such as bone pain or neurological deficits, leading to improvement of the health-related quality of life. Systemic therapies, such as radiopharmaceuticals, bisphosphonates, and monoclonal antibodies against the receptor activator of the nuclear factor-kappa B ligand, are administered to reduce presymptomatic and symptomatic skeletal complications.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Skeletal-related events
- Symptomatic skeletal events
- Bone mineral density
- Pathological bone fracture
- Spinal cord compression
33.1 Introduction
Skeletal complications can lead to significant morbidity in patients with prostate cancer by two viewpoints: first, the prevalence of bone metastasis in patients with prostate cancer is relatively higher than that in other cancers [1]; second, androgen deprivation therapy (ADT) for the treatment of prostate cancer reduces bone mineral density (BMD), leading to an acceleration of osteoporosis and bone metastases [2, 3]. These two factors closely interact with each other, leading to the development of multiple skeletal complications in patients with prostate cancer. The relatively long survival (median, 3–4 years) after bone metastases with multiple skeletal complications in patients with prostate cancer makes a significant negative impact on patients’ functional status, quality of life, and social resource utilization [4].
33.2 Skeletal-Related Events and Symptomatic Skeletal Events
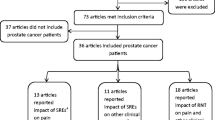
To assess the incidence of skeletal complications as endpoints of clinical trials, the term “skeletal-related events (SREs)” was previously defined by the Food and Drug Administration of the United States and has been used in several trials [5]. In most clinical studies, SREs included four factors: pathological bone fracture, spinal cord compression, surgery to bone, and radiotherapy to the bone; thus, SREs have been defined as a composite endpoint, mostly including the need for local treatments of radiation or orthopedic surgery ([6,7,8,9]; Table 33.1). Radiotherapy is usually indicated for the treatment of uncontrolled pain, pathologic fractures, and spinal cord compression. Surgery usually includes procedures to stabilize or prevent pathologic fractures or spinal cord compression. The definition of SRE, however, is different in several randomized trials. In a broad sense, SREs include a change of antineoplastic therapy to treat bone pain [6, 9]. A reduction in the frequency of SREs has been used in several phase III trials to support the approval of zoledronic acid (ZOL) and denosumab [6, 7]. The definition of SREs includes asymptomatic nonclinical fractures ascertained by serial imaging. Recently, the Prostate Cancer Clinical Trial Working Group 3 [10] stated that they did not consider SREs and instead they recommended using “symptomatic skeletal events (SSEs)” that include only symptomatic events of clear clinical significance. In phase III clinical trial for radium-223, SSEs were defined as symptomatic fracture, radiation or surgery to bone, or spinal cord compression [11].
33.3 Incidence and Prevalence of Skeletal Complications in Patients with CRPC
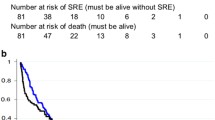
According to data in the placebo arm of the randomized phase III trials evaluating the effectiveness of ZOL, the incidence of SREs was reported to be 44.2% in patients with castration-resistant prostate cancer (CRPC) during approximately 9 months (median) of observation in the study [6]. Furthermore, all types of pathologic fractures were observed in 22.1%, vertebral fractures in 8.2%, non-vertebral fractures in 15.9%, radiation therapy in 29.3%, bone surgery in 3.4%, and spinal cord compression in 6.7% of patients in the placebo arm. In another study comparing the incidence of SREs in patients with bone metastases in the breast, lung, or prostate cancer, the incidence of SREs in patients with prostate cancer was approximately 20% and 30% at 6 and 12 months after the diagnosis of bone metastasis, respectively, which was less than that in patients with breast and lung cancer. However, the incidence eventually reached approximately 45%, which is comparable to the incidence of lung cancer at 36 months when using ZOL in 48.9% of the prostate cancer patients [12] (Fig. 33.1).
Conversely, the prevalence of bone metastasis and bone pain at the time of CRPC diagnosis was 84% and 45%, respectively, in a Japanese study [13]. In the present study, the medical charts of the enrolled patients with CRPC were retrospectively reviewed at a single institute, and the patients were not using bone-modifying agents, such as ZOL or denosumab. During a median 18 months of follow-up, the incidences of bone pain, neurological deficits, and pathologic fractures were 80%, 44%, and 14%, respectively. The incidences of taking nonsteroidal anti-inflammatory drugs and opioids were 74% and 43%, respectively, and those of radiation therapies for bone pain and laminectomy for paraplegia were 51% and 10% during the follow-up period, respectively (Fig. 33.2).
33.4 Pathophysiology of Bone Metastases in Prostate Cancer
The metastasizing mechanism of prostate cancer cells to bone involves colonization of the skeletal microenvironment by circulating tumor cells (CTCs). Reportedly, only 0.2% of experimentally introduced CTCs were estimated to colonize distant sites [14]. According to Paget’s well-established “seed and soil” hypothesis published in 1889, a bone microenvironment is ideal “soil” for circulating prostate cancer cells [15]. The three steps of metastatic seeding include survival of CTCs in circulation, homing to skeletal tissue, and attachment to bone parenchyma [16].
Platelets play an important role in the survival of CTCs in that they shield CTCs from NK cell-mediated lysis [17]. In the homing process of CTCs into skeletal tissue, chemotactic factors responsible for the migration of hematopoietic stem cells into bone marrow have been investigated as key molecules [18]. One of these chemotactic factors is stromal-derived factor-1 (SDF-1), also called CXCL12, which is predominantly produced by osteoblasts. C-X-C motif chemokine receptor 4, expressed on the surface of hematopoietic stem cells as well as prostate cancer CTCs, interacts with SDF-1 to induce homing to the bone marrow [19, 20]. In the attachment and invading process of CTCs to bone parenchyma, integrin- and lectin-mediated attachment or protease-dependent invasion has been characterized. Three major integrins, including αvβ3, α2β1, and α4β1, have demonstrated instructive roles in metastatic bone seeding [21].
The activation of osteoclast-mediated bone resorption is one of the most investigated areas in this field. Induction of the receptor activator of nuclear factor-kappa B ligand (RANKL), granulocyte macrophage colony stimulating factor (GM-CSF), and macrophage colony-stimulating factor (M-CSF) from the tumor cells results in maturation of osteoclast precursor cells into multinucleated osteoclasts. Enhanced osteoclast-mediated lysis of the bone matrix releases various cytokines, such as GM-CSF, M-CSF, tumor growth factor beta, insulin-like growth factors, epidermal growth factors, fibroblast growth factors, and interleukin 6 stored in the bone matrix. These growth factors stimulate the expression of pro-metastatic factors, such as Jagged 1 [22], parathyroid hormone-related peptide [23], or cathepsin K [24] from tumor cells, which then stimulate the osteoblasts to release RANKL to promote osteoclast activation [25]. These cycles are called “vicious cycles” in the bone microenvironment in that they promote bone metastasis [23, 26].
Prostate cancer typically presents as osteoblastic lesions, and reportedly 43%, 21%, and 36% of the prostate cancer metastases studied in one report were osteoblastic, osteolytic, and mixed, respectively [27]. The transcription factor runt-related transcription factor 2 (RUNX2) is a promising molecule involved in the osteoblastic lesion formation mechanism and is normally expressed by mesenchymal progenitor cells to differentiate osteoblasts. In the microenvironment of prostate cancer bone metastases, RUNX2 is also expressed by prostate cancer cells [28] and activates bone matrix protein transcription, such as bone sialoprotein and osteocalcin. Serin protease Endothelin-1 (ET-1), which is also secreted from prostate cancer cells in the bone microenvironment, is a well-established osteoblast mitogen that promotes osteoblastic bone metastasis by binding ETA receptor on the osteoblast [29, 30]. The randomized phase III trial for the ET-1 antagonist Atrasentan did not decrease the risk of disease progression in patients with metastatic prostate cancer [31].
33.5 Reduction of BMD Due to ADT and Its Interaction with Bone Metastasis
ADT has been demonstrated to have various adverse effects, including the reduction of BMD. Reportedly, around 45% of patients with prostate cancer receiving ADT develop osteoporosis [32]. The reduction of BMD was maximal in the first year after the initiation of ADT, peaking at 2%–5% [33, 34].
Androgen receptor (AR) is expressed in osteoblasts, osteoclasts, and osteocytes [35,36,37]. ADT has been shown to increase the levels of RANKL in rat serum and bone marrow [38], which caused a reduction in BMD due to osteoclast activation [39]. Moreover, bone-marrow RANKL mRNA levels have been shown to be up-regulated in mice lacking AR [36, 40] and down-regulated in mice overexpressing AR [37]. Conversely, glucocorticoid promotes the production of RANKL by osteoblasts [41, 42]. Previous reports have suggested that AR regulates RANK/RANKL signaling in the bone microenvironment and that ADT enhances this pathway, inducing osteoclast precursors to mature into osteoclasts, leading to a reduced BMD.
The high prevalence of bone metastases in patients with prostate cancer and reduction of BMD due to ADT together make skeletal complications in these patients more common. In a murine model, Ottewell et al. showed that ADT triggered the growth of disseminated PC3 cells to form bone metastases and that this was prevented with ZOL [2]. Takayama et al. also illustrated the ADT-induced acceleration of bone metastases and involvement of the RANK/RANKL signaling in this interaction [3]. These findings suggest that osteoclast suppression by RANK/RANKL signaling from the initiation of ADT is required to prevent the accelerated establishment of new bone metastases in patients with organ-confined or locally advanced high-risk prostate cancer with a high possibility of the existence of CRPC CTCs at the time of ADT initiation.
In the contemporary oncological strategy for patients with CRPC, relatively long-term ADT (median, 3–4 years) after bone metastasis is usually required. The interactions among the high incidence of bone metastases, reduction of BMD due to ADT, and acceleration of bone metastases due to ADT may together lead to frequent skeletal complications resulting in a poorer health-related quality of life (HRQOL) and survival in patients with CRPC despite the anticancer effect of ADT.
33.6 Prognosis, HRQOL, and Health Resource Utilization in Patients with Prostate Cancer Who Have Skeletal Complications
The presence of SREs is significantly associated with a worse survival and poorer HRQOL. Patients who developed a pathologic fracture had a 32% increased risk of death relative to patients without a fracture in an adjusted analysis, with comparable results observed for both vertebral and non-vertebral fractures [43]. Increasing SRE intensity shows a pattern of poorer survival and HRQOL [44, 45]. In patients with SREs, a significantly worse outcome was observed compared with those without SREs in validated assessment instruments, such as the functional assessment of cancer therapy-general and the brief pain inventory [44]. Complications of osteoporosis and fractures in men undergoing ADT have important economic consequences: there is an associated $22,000 cost per person during the 36 months of treatment [46]. All SREs are associated with health resource utilization, including both inpatient hospitalizations and outpatient or emergency room visits, of $12,469 per year per person [47, 48] (Table 33.2). Furthermore, those studies may have underestimated their impact because of the exclusion of patients with a short life expectancy and health resource with bone pain management [49].
33.7 Treatments for Skeletal Complications
Treatments for skeletal complications include local and systemic therapies. Local therapies include radiation and surgical therapies that are usually performed to reduce local symptoms and improve HRQOL regarding bone pain or neurological deficits. Radiation therapy for local lesions reportedly improves mobility, daily life activity, and sphincter control in patients with metastatic spinal cord compression [50]. Moreover, in one study, radiation therapy significantly improved HRQOL of patients suffering from bone pain [45]. It was reported that functional outcomes after radiation therapy were significantly influenced by the amount of time taken to develop motor deficits before radiation therapy and the number of involved vertebrae. Local control was significantly better after long-course radiation, such as 2 Gy × 20 times, than after short courses, such as 8 Gy × 1 time or 4 Gy × 5 times [51].
Surgical treatments for neurological deficits due to spinal cord compression usually consist of posterior decompression and stabilization with pedicle screws or with pedicle screws and hooks. There have only been a few studies that specifically addressed the surgical treatment of metastatic spinal cord compression in patients with prostate cancer [52,53,54]. Furthermore, the criteria for which patient may benefit from the surgical therapy of spinal cord compression are poorly defined; in selected patients, however, aggressive surgical decompression and spinal reconstruction is a useful treatment option [54]. Patients with hormone-naive disease and those with the hormone-refractory disease with good performance status and lacking visceral metastases may benefit from surgery for metastatic spinal cord compression [52].
Systemic therapies, including bisphosphonates, a monoclonal antibody against RANKL, and radiopharmaceuticals, are administered to prevent and reduce presymptomatic and symptomatic SREs. The first agent approved for the management of bone metastases in patients with CRPC was ZOL, a third-generation bisphosphonate. A phase III trial comparing ZOL vs. placebo demonstrated a significant reduction of at least one SRE with ZOL from 49% to 38% during the 24-month study period [6]. Denosumab is a fully humanized monoclonal antibody against RANKL that prevents the activation of its receptor RANK leading to inhibition of osteoclast maturation and bone resorption. In a phase III trial comparing denosumab vs. ZOL in patients with CRPC who have bone metastases, there was a significant improvement in median time (3.6 months) to the first SRE in the denosumab arm [7].
Regarding radiopharmaceuticals, strontium-89 is a pure beta-emitter with a long half-life, whereas samarium-153 is a gamma-emitter with a shorter half-life. Multiple randomized trials have been conducted with strontium-89 and samarium-153 in men with metastatic CRPC that have shown no improvement in OS, but palliative benefits have been demonstrated with both agents [55, 56]. The alpha-emitter radium-223 causes breaks in double-stranded DNA with less irradiation of healthy adjacent bone marrow and normal tissues. In a randomized phase III trial, radium-223 significantly prolonged the median OS in 3.8 months and significantly delayed the time to all SRE components, particularly the components of external-beam radiation therapy and spinal cord compression [11].
References
Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001;27:165–76.
Ottewell PD, Wang N, Meek J, Fowles CA, Croucher PI, Eaton CL, Holen I. Castration-induced bone loss triggers growth of disseminated prostate cancer cells in bone. Endocr Relat Cancer. 2014;21:769–81.
Takayama K, Inoue T, Narita S, Maita S, Huang M, Numakura K, Tsuruta H, Saito M, Maeno A, Satoh S, Tsuchiya N, Habuchi T. Inhibition of the RANK/RANKL signaling with osteoprotegerin prevents castration-induced acceleration of bone metastasis in castration-insensitive prostate cancer. Cancer Lett. 2017;397:103–10.
Vignani F, Bertaglia V, Buttigliero C, Tucci M, Scagliotti GV, Di Maio M. Skeletal metastases and impact of anticancer and bone-targeted agents in patients with castration-resistant prostate cancer. Cancer Treat Rev. 2016;44:61–73.
Clinical Trials Endpoints for the Approval of Cancer Drugs and Biologics, US Department of Health and Human Services, Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Center for Biologics Evaluation and Research (CBER). 2007.
Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L, Chin JL, Vinholes JJ, Goas JA, Chen B, Zoledronic Acid Prostate Cancer Study Group. A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst. 2002;94:1458–68.
Fizazi K, Carducci M, Smith M, Damião R, Brown J, Karsh L, Milecki P, Shore N, Rader M, Wang H, Jiang Q. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet. 2011;377:813–22.
Logothetis CJ, Basch E, Molina A, Fizazi K, North SA, Chi KN, Jones RJ, Goodman OB, Mainwaring PN, Sternberg CN, Efstathiou E, Gagnon DD, Rothman M, Hao Y, Liu CS, Kheoh TS, Haqq CM, Scher HI, de Bono JS. Effect of abiraterone acetate and prednisone compared with placebo and prednisone on pain control and skeletal-related events in patients with metastatic castration-resistant prostate cancer: exploratory analysis of data from the COU-AA-301 randomized trial. Lancet Oncol. 2012;13:1210–7.
Fizazi K, Scher HI, Miller K, Basch E, Sternberg CN, Cella D, Forer D, Hirmand M, de Bono JS. Effect of enzalutamide on time to first skeletal-related event, pain, and quality of life in men with castration-resistant prostate cancer: results from the randomized, phase 3 AFFIRM trial. Lancet Oncol. 2014;15:1147–56.
Scher HI, Morris MJ, Stadler WM, Higano C, Basch E, Fizazi K, Antonarakis ES, Beer TM, Carducci MA, Chi KN, Corn PG. Trial design and objectives for castration-resistant prostate cancer: updated recommendations from the Prostate Cancer Clinical Trials Working Group 3. J Clin Oncol. 2016;34:1402–18.
Sartor O, Coleman R, Nilsson S, Heinrich D, Helle SI, O'Sullivan JM, Fosså SD, Chodacki A, Wiechno P, Logue J, Widmark A, Johannessen DC, Hoskin P, James ND, Solberg A, Syndikus I, Vogelzang NJ, O’Bryan-Tear CG, Shan M, Bruland ØS, Parker C. Effect of radium-223 dichloride on symptomatic skeletal events in patients with castration-resistant prostate cancer and bone metastases: results from a phase 3, double-blind, randomised trial. Lancet Oncol. 2014;15:738–46.
Oster G, Lamerato L, Glass AG, Richert-Boe KE, Lopez A, Chung K, Richhariya A, Dodge T, Wolff GG, Balakumaran A, Edelsberg J. Natural history of skeletal-related events in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systems. Support Care Cancer. 2013;21:3279–86.
Inoue T, Segawa T, Kamba T, Yoshimura K, Nakamura E, Nishiyama H, Ito N, Kamoto T, Habuchi T, Ogawa O. Prevalence of skeletal complications and their impact on survival of hormone refractory prostate cancer patients in Japan. Urology. 2009;73:1104–9.
Chambers AF, Groom AC, MacDonald IC. Dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer. 2002;2:563–72.
Paget S. The distribution of secondary growths in cancer of the breast. 1889. Cancer Metastasis Rev. 1989;8:98–101.
Esposito M, Kang Y. Targeting tumor-stromal interactions in bone metastasis. Pharmacol Ther. 2014;141:222–33.
Nieswandt B, Hafner M, Echtenacher B, Männel DN. Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res. 1999;59:1295–300.
Weilbaecher KN, Guise TA, McCauley LK. Cancer to bone: a fatal attraction. Nat Rev Cancer. 2011;11:411–25.
Sun YX, Wang J, Shelburne CE, Lopatin DE, Chinnaiyan AM, Rubin MA, Pienta KJ, Taichman RS. Expression of CXCR4 and CXCL12 (SDF-1) in human prostate cancers (PCa) in vivo. J Cell Biochem. 2003;89:462–73.
Sun YX, Fang M, Wang J, Cooper CR, Pienta KJ, Taichman RS. Expression and activation of alpha v beta 3 integrins by SDF-1/CXC12 increases the aggressiveness of prostate cancer cells. Prostate. 2007;67:61–73.
Schneider JG, Amend SR, Weilbaecher KN. Integrins and bone metastasis: integrating tumor cell and stromal cell interactions. Bone. 2011;48:54–65.
Sethi N, Dai X, Winter CG, Kang Y. Tumor-derived JAGGED1 promotes osteolytic bone metastasis of breast cancer by engaging notch signaling in bone cells. Cancer Cell. 2011;19:192–205.
Roodman GD. Mechanisms of bone metastasis. N Engl J Med. 2004;350:1655–64.
Brubaker KD, Vessella RL, True LD, Thomas R, Corey E. Cathepsin K mRNA and protein expression in prostate cancer progression. J Bone Miner Res. 2003;18:222–30.
Hauschka PV, Mavrakos AE, Iafrati MD, Doleman SE, Klagsbrun M. Growth factors in bone matrix. Isolation of multiple types by affinity chromatography on heparin-Sepharose. J Biol Chem. 1986;261:1266574.
Mundy GR. Metastasis to bone: causes, consequences and therapeutic opportunities. Nat Rev Cancer. 2002;2:584–93.
Reddington JA, Mendez GA, Ching A, Kubicky CD, Klimo P Jr, Ragel BT. Imaging characteristic analysis of metastatic spine lesions from breast, prostate, lung, and renal cell carcinomas for surgical planning: osteolytic versus osteoblastic. Surg Neurol Int. 2016;7:S361–5.
Akech J, Wixted JJ, Bedard K, van der Deen M, Hussain S, Guise TA, van Wijnen AJ, Stein JL, Languino LR, Altieri DC, Pratap J, Keller E, Stein GS, Lian JB. Runx2 association with progression of prostate cancer in patients: mechanisms mediating bone osteolysis and osteoblastic metastatic lesions. Oncogene. 2010;29:811–21.
Nelson JB, Hedican SP, George DJ, Reddi AH, Piantadosi S, Eisenberger MA, Simons JW. Identification of endothelin-1 in the pathophysiology of metastatic adenocarcinoma of the prostate. Nat Med. 1995;1(9):944.
Yin JJ, Mohammad KS, Käkönen SM, Harris S, Wu-Wong JR, Wessale JL, Padley RJ, Garrett IR, Chirgwin JM, Guise TA. A causal role for endothelin-1 in the pathogenesis of osteoblastic bone metastases. Proc Natl Acad Sci U S A. 2003;100:10954–9.
Carducci MA, Saad F, Abrahamsson PA, Dearnaley DP, Schulman CC, North SA, Sleep DJ, Isaacson JD, Nelson JB, Atrasentan Phase III Study Group Institutions. A phase 3 randomized controlled trial of the efficacy and safety of atrasentan in men with metastatic hormone-refractory prostate cancer. Cancer. 2007;110:1959–66.
Morote J, Morin JP, Orsola A, Abascal JM, Salvador C, Trilla E, Raventos CX, Cecchini L, Encabo G, Reventos J. Prevalence of osteoporosis during long-term androgen deprivation therapy in patients with prostate cancer. Urology. 2007;69:500–4.
Greenspan SL, Coates P, Sereika SM, Nelson JB, Trump DL, Resnick NM. Bone loss after initiation of androgen deprivation therapy in patients with prostate cancer. J Clin Endocrinol Metab. 2005;90:6410–7.
Morote J, Orsola A, Abascal JM, Planas J, Trilla E, Raventos CX, Cecchini L, Encabo G, Reventos J. Bone mineral density changes in patients with prostate cancer during the first 2 years of androgen suppression. J Urol. 2006;175:1679–83.
Colvard DS, Eriksen EF, Keeting PE, Wilson EM, Lubahn DB, French FS, Riggs BL, Spelsberg TC. Identification of androgen receptors in normal human osteoblast-like cells. Proc Natl Acad Sci U S A. 1989;86:854–7.
Russell PK, Clarke MV, Skinner JP, Pang TP, Zajac JD, Davey RA. Identification of gene pathways altered by deletion of the androgen receptor specifically in mineralizing osteoblasts and osteocytes in mice. J Mol Endocrinol. 2012;49:1–10.
Wiren KM, Zhang XW, Toombs AR, Kasparcova V, Gentile MA, Harada S, Jepsen KJ. Targeted overexpression of androgen receptor in osteoblasts: unexpected complex bone phenotype in growing animals. Endocrinology. 2004;145:3507–22.
Proell V, Xu H, Schüler C, Weber K, Hofbauer LC, Erben RG. Orchiectomy upregulates free soluble RANKL in bone marrow of aged rats. Bone. 2009;45:677–81.
Li X, Ominsky MS, Stolina M, Warmington KS, Geng Z, Niu QT, Asuncion FJ, Tan HL, Grisanti M, Dwyer D, Adamu S. Increased RANK ligand in bone marrow of orchiectomized rats and prevention of their bone loss by the RANK ligand inhibitor osteoprotegerin. Bone. 2009;45:669–76.
Kawano H, Sato T, Yamada T, Matsumoto T, Sekine K, Watanabe T, Nakamura T, Fukuda T, Yoshimura K, Yoshizawa T, Aihara K, Yamamoto Y, Nakamichi Y, Metzger D, Chambon P, Nakamura K, Kawaguchi H, Kato S. Suppressive function of androgen receptor in bone resorption. Proc Natl Acad Sci U S A. 2003;100:9416–21.
Humphrey EL, Williams JH, Davie MW, Marshall MJ. Effects of dissociated glucocorticoids on OPG and RANKL in osteoblastic cells. Bone. 2006;38:652–61.
Swanson C, Lorentzon M, Conaway HH, Lerner UH. Glucocorticoid regulation of osteoclast differentiation and expression of receptor activator of nuclear factor-kappaB (NF-kappaB) ligand, osteoprotegerin, and receptor activator of NF-kappaB in mouse calvarial bones. Endocrinology. 2006;147:3613–22.
Saad F, Lipton A, Cook R, Chen YM, Smith M, Coleman R. Pathologic fractures correlate with reduced survival in patients with malignant bone disease. Cancer. 2007;110:1860–7.
DePuy V, Anstrom KJ, Castel LD, Schulman KA, Weinfurt KP, Saad F. Effects of skeletal morbidities on longitudinal patient-reported outcomes and survival in patients with metastatic prostate cancer. Support Care Cancer. 2007;15:869–76.
Weinfurt KP, Li Y, Castel LD, Saad F, Timbie JW, Glendenning GA, Schulman KA. The significance of skeletal-related events for the health-related quality of life of patients with metastatic prostate cancer. Ann Oncol. 2005;16:579–84.
Krupski TL, Foley KA, Baser O, Long S, Macarios D, Litwin MS. Health care cost associated with prostate cancer, androgen deprivation therapy and bone complications. J Urol. 2007;178:1423–8.
Hagiwara M, Delea TE, Saville MW, Chung K. Healthcare utilization and costs associated with skeletal-related events in prostate cancer patients with bone metastases. Prostate Cancer Prostatic Dis. 2013;16:23–7.
Lage MJ, Barber BL, Harrison DJ, Jun S. The cost of treating skeletal-related events in patients with prostate cancer. Am J Manag Care. 2008;14:317–22.
Hechmati G, Cure S, Gouépo A, Hoefeler H, Lorusso V, Lüftner D, Duran I, Garzon-Rodriguez C, Ashcroft J, Wei R, Ghelani P, Bahl A. Cost of skeletal-related events in European patients with solid tumours and bone metastases: data from a prospective multinational observational study. J Med Econ. 2013;16:691–700.
Aass N, Fosså SD. Pre- and post-treatment daily life function in patients with hormone resistant prostate carcinoma treated with radiotherapy for spinal cord compression. Radiother Oncol. 2005;74:259–65.
Rades D, Stalpers LJ, Veninga T, Rudat V, Schulte R, Hoskin PJ. Evaluation of functional outcome and local control after radiotherapy for metastatic spinal cord compression in patients with prostate cancer. J Urol. 2006;175:552–6.
Crnalic S, Hildingsson C, Wikström P, Bergh A, Löfvenberg R, Widmark A. Outcome after surgery for metastatic spinal cord compression in 54 patients with prostate cancer. Acta Orthop. 2012;83:80–6.
Shoskes DA, Perrin RG. The role of surgical management for symptomatic spinal cord compression in patients with metastatic prostate cancer. J Urol. 1989;142:337–9.
Williams BJ, Fox BD, Sciubba DM, Suki D, Tu SM, Kuban D, Gokaslan ZL, Rhines LD, Rao G. Surgical management of prostate cancer metastatic to the spine. J Neurosurg Spine. 2009;10:414–22.
Lewington VJ, McEwan AJ, Ackery DM, Bayly RJ, Keeling DH, Macleod PM, Porter AT, Zivanovic MA. A prospective, randomized double-blind crossover study to examine the efficacy of strontium-89 in pain palliation in patients with advanced prostate cancer metastatic to bone. Eur J Cancer. 1991;27:954–8.
Serafini AN, Houston SJ, Resche I, Quick DP, Grund FM, Ell PJ, Bertrand A, Ahmann FR, Orihuela E, Reid RH, Lerski RA, Collier BD, McKillop JH, Purnell GL, Pecking AP, Thomas FD, Harrison KA. Palliation of pain associated with metastatic bone cancer using samarium-153 lexidronam: a double-blind placebo-controlled clinical trial. J Clin Oncol. 1998;16:1574–81.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Inoue, T., Habuchi, T. (2018). Skeletal Complications in Patients with CRPC. In: Arai, Y., Ogawa, O. (eds) Hormone Therapy and Castration Resistance of Prostate Cancer. Springer, Singapore. https://doi.org/10.1007/978-981-10-7013-6_33
Download citation
DOI: https://doi.org/10.1007/978-981-10-7013-6_33
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-10-7012-9
Online ISBN: 978-981-10-7013-6
eBook Packages: MedicineMedicine (R0)