Abstract
Background:
Skeletal-related events (SREs) including pathologic fracture, spinal cord compression, radiation to bone and surgery to bone, are common in men with bone metastatic castration-resistant prostate cancer (mCRPC). Men with mCRPC are at high risk of death. Whether SREs predict mortality is unclear. We tested the association between SREs and overall survival (OS) in a multiethnic cohort with bone mCRPC, controlling for key covariates unavailable in claims data such as bone pain, number of bone metastases and PSA doubling time (PSADT).
Methods:
We collected data on 233 men diagnosed with nonmetastatic castration-resistant prostate cancer (CRPC) in 2000–2013 at two Veterans Affairs hospitals who later progressed to bone metastases. First occurrence of SRE and OS were collected from the medical records. Cox models were used to test the association between SRE and OS, treating SRE as a time-dependent variable. We adjusted for age, year, race, treatment center, biopsy Gleason, primary treatment to the prostate, PSA, PSADT, months from androgen deprivation therapy to CRPC, months from CRPC to metastasis and number of bone metastases at initial bone metastasis diagnosis. In a secondary analysis, we also adjusted for bone pain.
Results:
During follow-up, 88 (38%) patients had an SRE and 198 (85%) died. After adjusting for risk factors, SRE was associated with increased mortality (hazard ratio (HR)=1.67; 95% confidence interval (CI) 1.22–2.30; P=0.001). When bone pain was added to the model, the association of SREs and OS was attenuated, but remained significant (HR=1.42; 95% CI 1.01–1.99; P=0.042).
Conclusions:
SREs are associated with increased mortality in men with bone mCRPC. Further studies on the impact of preventing SREs to increase survival are warranted.
Similar content being viewed by others
Introduction
Prostate cancer (PC) is the sixth leading cause of cancer death in men worldwide, with an estimated 258 000 deaths in 2008.1 Men are at highest risk of PC death once they become castration-resistant and develop distant metastases. The median survival among patients with bone metastatic castration-resistant PC (mCRPC) is estimated at 16–40 months.2, 3, 4 At this advanced stage, it is important to identify modifiable risk factors to prolong survival.
Prior to death, patients with mCRPC are at risk of other adverse cancer-related sequelae. Particularly concerning adverse events are skeletal-related event (SREs), defined as pathologic fracture, spinal cord compression, radiation to bone or surgery to bone.5 Clinical trials showed several bone-targeted agents (denosumab and zoledronic acid) reduce SREs, but have no impact on overall survival (OS).5, 6 In contrast, other PC therapies (abiraterone, enzalutamide), including bone-targeted therapies (radium-223), showed reductions in risk of SREs and improved OS.7, 8, 9 Meanwhile, a number of population-based studies found an association between SREs and worse OS.10, 11, 12, 13 Although these population-based studies benefited from large sample sizes, they could only capture information on metastases, SREs and disease characteristics from ICD-9 codes. Specifically, these prior observational studies were unable to adjust for bone pain, number of bone metastases and PSA doubling time (PSADT). A further limitation is that the populations were primarily Caucasians. Finally, none of these population-based studies tested the association of SREs and OS specifically among men with bone mCRPC; the reference groups were either all PC patients or those with metastases, but not specifically bone mCRPC.
We tested the association between SREs and OS in a multiethnic cohort of bone mCRPC patients from the Shared Equal Access Cancer Research Hospital (SEARCH) database mostly treated in the pre-abiraterone and pre-enzalutamide era, controlling for demographic and disease characteristics including key covariates unavailable in claims data including bone pain, number of bone metastases and PSADT. We hypothesized that when controlling for these factors, SREs would be associated with worse OS.
Materials and methods
Study population
After obtaining Institutional Review Board approval, data from patients with mCRPC were identified from two Veteran Affairs (VA) Medical Centers (San Diego, CA and Durham, NC) in the SEARCH database, regardless of primary treatment modality. The methods to create this cohort have been described.14 First, 7888 patients who received androgen deprivation therapy (ADT) between 1991–2013 and had PSA levels ⩾2 ng ml−1 after initiating ADT were identified. We limited to those with documented CRPC defined by the Prostate Cancer Working Group 2 (relative increase of 25% and absolute increase of ⩾2 ng ml−1 above nadir while receiving continuous ADT, including gonadotropin-releasing hormone agonist, antagonist or bilateral orchiectomy).15 All imaging tests following CRPC diagnosis were read by the trained personnel to determine distant PC metastases. We excluded patients who had metastatic disease at or before CRPC diagnosis or who had CRPC diagnosis prior to 2000. Patients with no scans prior to CRPC were assumed to be nonmetastatic. As castration-sensitive metastases might be different from castration-resistant metastases, we excluded men with metastases prior to CRPC diagnosis. Of 459 men with nonmetastatic CRPC diagnosed with CRPC in 2000 or later, 233 (51%) developed bone metastases during follow-up (median 15 months) and were included in the final cohort. First occurrence of an SRE (pathologic fracture, spinal cord compression, radiation to bone or surgery to bone) was collected from the VA medical records and any notes from outside the VA that were available.5 Bone pain was determined from medical notes within 2 months before or after bone metastasis diagnosis that clearly stated the patient was or was not experiencing bone pain.
Statistical methods
PSADT was calculated by the natural log of 2 divided by the slope of the linear regression of the natural log of PSA over time in months.16 Subjects with calculated PSADT <0 or >120 were assigned 120 months to facilitate analysis. All available PSAs prior to metastases but after CRPC diagnosis were used to calculate PSADT. To calculate PSADT, subjects had to have ⩾2 PSAs over ⩾3 months. Cox proportional hazards models were used to test the association between SRE and OS. Time zero was diagnosis of bone mCRPC, and patients were followed until death or lost to follow-up. SRE was treated as a time-dependent variable as events happened at different times after baseline. In multivariable analysis, we adjusted for age (continuous), year of metastasis (continuous), race (black vs nonblack), treatment center (Center 1 vs Center 2), biopsy Gleason (2–6 vs 7 vs 8–10 vs unknown/no biopsy), primary treatment to the prostate (none vs radical prostatectomy and/or radiation), PSA at metastasis (continuous and log-transformed), PSADT (<9 months vs ⩾9 months vs missing, based on previous literature),17 months from ADT to CRPC (continuous), months from CRPC to metastasis (continuous) and number of bone metastases at initial diagnosis of bone metastases (1 vs 2 vs 3–9 vs ⩾10). A sensitivity analysis was performed dropping patients who received abiraterone, enzalutamide or radium-223 (n=31), because these drugs have been shown to reduce the risk of SREs and prolong SRE, and we wanted to check that the use of these drugs did not alter our results.
As bone pain is often treated with radiation to reduce the pain, which by definition is an SRE, we were concerned the association between SRE and OS may differ based upon the presence or absence of bone pain. Therefore, in secondary analyses, we adjusted the multivariable model for bone pain (yes vs no vs unknown) and stratified the univariable model by bone pain (yes vs no). The interaction between bone pain and SREs was tested by including a product term in the model. Kaplan–Meier curves were used to compare time with SRE and time with death in men with and without bone pain.
Results
Median year of bone metastases was 2007 and median age at diagnosis of bone metastases was 75 (Q1–Q3: 68–81); (Table 1). There were 80 (34%) black patients. During median follow-up of 14.7 months (Q1–Q3: 5.2–33.8), 88 (28%) patients had an SRE and 198 (85%) patients died. Of the SREs, seven (8%) were pathological fractures, 75 (85%) were radiation to bone, four (5%) were spinal cord compression and two (2%) were surgery to bone. Type of SRE, including radiation to bone, was balanced between centers (Fisher’s exact test, P=0.38). The median time to SRE was 17.9 months (Q1–Q3: 13.9-not reached). The median time to death was 12.9 months (Q1–Q3: 10.2–14.4).
On univariable analysis, having an SRE was associated with increased mortality (hazard ratio (HR)=1.54; 95% confidence interval (CI) 1.15–2.07; P=0.004; Table 2). On multivariable analysis, SRE remained associated with increased mortality (HR=1.67; 95% CI 1.22–2.30; P=0.001). When bone pain was added to the multivariable model, the association of SREs and OS was attenuated, but remained significant (HR=1.42; 95% CI 1.01–1.99; P=0.042). The association between SREs and OS was stronger after excluding patients who received abiraterone, enzalutamide or radium-223 during follow-up (HR=2.16; 95% CI 1.54–3.02; P<0.001).
Among 81 patients without bone pain at initial diagnosis of metastases, SRE was associated with increased mortality on univariable (HR=2.35; 95% CI 1.34–4.12; P=0.003) and multivariable analysis (HR=2.24; 95% CI 1.13–4.46; P=0.021; Table 3). Among 103 patients with bone pain, SRE was not associated with OS on univariable (P=0.4) or multivariable analysis (P=0.13). However, the interaction between bone pain and SREs was not significant (P=0.2).
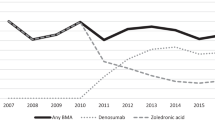
The median time to SRE was 48.5 months in those without bone pain and 8.2 months in those with bone pain (Figure 1). Furthermore, the median overall survival time was 17.8 months in those with no bone pain and 11.0 months in men with bone pain. In men with bone pain, 44% had an SRE within 6 months of bone mCRPC diagnosis, whereas only 11% of men with no bone pain had an SRE within 6 months.
Discussion
To better understand the relationship between SRE and OS, given conflicting results from clinical trials, we tested the association between SRE and OS in a multiethnic cohort who all had bone mCRPC. Importantly, we adjusted for key covariates including number of bone metastases and bone pain, which were unavailable in comparable population-based studies. We found SRE was associated with increased mortality, even after adjusting for bone pain and other key covariates. Future studies are needed to understand whether delaying SREs prolong life in patients with bone mCRPC.
Previous studies used population-based cohorts to test the association between SREs and OS in PC patients. The first study used >23 000 patients from the Danish National Patient Registry from 1999 to 2007.10 They found patients with an SRE and metastases had worse survival than patients without metastases (HR=6.7; 95% CI 6.0–7.6). Similarly, an analysis using the SEER-Medicare database found nearly identical results.11 Among almost 127 000 patients diagnosed with PC between 1999–2002, patients with SREs and metastases were at higher mortality risk than those without metastases (HR=10.2; 95% CI 9.8–10.7). Although both studies adjusted for some variables (age and comorbidity), other covariates were not included (bone pain and number of metastases). Most crucial, however, was the comparison group in both studies was not men with bone metastases who did not develop SREs, but rather men without bone metastases. As metastases are well-known to be linked with increased mortality, it is impossible to state whether the greater mortality risk was due to SREs or the concurrent metastases. Furthermore, as claims data are unable to determine CRPC status, it is likely these men had a mix of CRPC and hormone-sensitive metastases. A more recent study using 3297 men from SEER-Medicare found that among men with metastatic PC, those with >1 SRE had greater than twofold risk of death versus those with no SREs.13 Although the reference group was men with bone metastases but no SREs, the study did not restrict to those with CRPC. Finally, another study used nearly 7000 men diagnosed with metastatic PC between 2000–2007 from SEER-Medicare.12 Using three definitions of SRE, they found HRs for the association between SREs and mortality ranging from 1.05–1.14 (P-values <0.001–0.21), after adjusting for demographic and clinical characteristics. However, they did not include radiation to bone in their SRE definition, which comprised 85% of SREs in our cohort. Thus, no population-based study has addressed whether SREs affect OS using the common SRE definition of pathologic fracture, spinal cord compression, radiation to bone and surgery to bone among men with bone mCRPC.
Another key limitation of these prior population-based studies is that all relied on diagnostic, procedure, and billing codes to detect metastases and SREs. One study noted that there is no billing code specifically for SREs, no common framework for measuring SREs using these codes and dates are not always accurate.18 Thus, SRE prevalence can vary greatly depending on the codes used and studies may underestimate or misclassify SREs. However, in our study, we conducted a thorough review of the medical records using the common definition of SRE to accurately determine date and the type of SRE. Indeed, SRE rates in our study (38%) were very similar to a phase III trial of SRE prevention in men with bone mCRPC (28–38%).5
In the current study of men with bone mCRPC, we found SREs were associated with decreased OS. This suggests delaying or preventing SREs may prolong OS. Multiple large phase III trials tested bone-targeted agents and other PC therapies in patients with metastatic CRPC. Multiple agents have been shown to delay time from metastases to an SRE in men with CRPC,5, 7, 8, 9, 19 of which abiraterone, enzalutamide and radium-223 also improve survival in this population,7, 8, 9 whereas denosumab and zoledronic acid do not.5, 19 Of note, OS was a secondary end point in the zoledronic acid and denosumab trials of mCRPC men, and the studies were not powered to detect survival differences. Although it is commonly thought that zoledronic acid does not impact survival, a careful look at the pivotal phase III zoledronic acid trial shows that median survival in the zoledronic acid arm was almost 3 months longer than placebo5—similar to the survival prolongation from chemotherapy.3 However, with only about 200 people in each arm and modest follow-up, this did not reach statistical significance (P=0.091). Whether a larger study with longer follow-up would show a survival benefit for zoledronic acid is unknown. Though in hormone-sensitive subjects, zoledronic acid had no survival advantage in a well-powered study,20 this does not exclude the possibility of benefit for men with mCRPC. Denosumab was compared against zoledronic acid and OS was comparable (P=0.65), implying that if zoledronic acid does indeed have a survival benefit, then likely so does denosumab.19 Collectively, these data support the hypothesis that preventing SREs may improve OS. Ultimately, the impact of SRE prevention on OS requires further study.
In a secondary analysis, we found SREs were associated with decreased OS in patients without bone pain at baseline, but the association was not significant in patients with bone pain. In men without bone pain, SREs were associated with over double the mortality risk versus those without an SRE (HR=2.24). In contrast, among men with bone pain, the association between SRE and OS was not significant. Of note, although the interaction test was not significant implying the association between SRE and OS did not differ between men with and without bone pain, our study was not powered to detect interactions. Thus, further studies with larger samples are needed to examine whether a true interaction exists. If an interaction is found, we speculate this may be due to the correlation between bone pain and SRE. Radiation to bone was the most common SRE in our data and is usually prescribed for bone pain, though we did not collect the indication for radiation to bone for each patient. Within 6 months of bone mCRPC diagnosis, 11% of men without bone pain versus 44% of men with bone pain had an SRE. Everyone who had bone pain at baseline had a potential indication for an SRE, which is probably why patients with bone pain had four times greater SRE risk within 6 months than patients without bone pain. Therefore, among men with a potential SRE indication at baseline (that is, bone pain), it is difficult to separate the independent effects of the SREs as prognostic for OS. Note that bone pain is a spectrum, and bone pain does not necessarily imply radiation and thus SRE, as moderate bone pain is usually treated medically. Once patients present with bone pain, it may be too late to treat them for SRE prevention. Thus, our data suggest that if SRE-delaying medications are to work and thereby improve OS, they should be given before bone pain presents, though again, this would require validation in future studies.
Our study has some limitations. Our cohort consisted of CRPC patients being treated at two VA hospitals, which limits the generalizability of our findings. We did not have enough power to examine whether specific SRE subtypes were related to survival as 85% of the SREs were radiation to bone. We only collected information on the first SRE, so we could not assess the effect of having multiple SREs. As this was an observational study, we only had data available from the VA medical records to evaluate bone pain and number of bone metastasis, and we did not have complete information on outside care. Although our bone pain definition has not been validated, bone pain was a significant predictor of SRE as shown in previous studies21 which gives it some validity. Because this was an observational study, not all patients had a bone scan to confirm that they were nonmetastatic at the time of CRPC diagnosis, so we assumed that men with no metastases detected were nonmetastatic. Our results might be biased if men with undetected metastases at CRPC diagnosis progress more quickly. When stratifying our models by bone pain, our models were overfit with a modest number of events in each model. Finally, we did not have enough patients to stratify our analysis by disease grade or race.
We found that SREs are associated with increased mortality in men with bone mCRPC, even after adjusting for factors such as bone pain, number of bone metastases and PSADT. Larger studies are needed to confirm whether SREs increase risk of mortality. If validated in a larger study, then future studies are needed to test whether preventing SREs may prolong survival.
References
Center MM, Jemal A, Lortet-Tieulent J, Ward E, Ferlay J, Brawley O et al. International variation in prostate cancer incidence and mortality rates. Eur Urol 2012; 61: 1079–1092.
Sturge J, Caley MP, Waxman J . Bone metastasis in prostate cancer: emerging therapeutic strategies. Nat Rev Clin Oncol 2011; 8: 357–368.
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 2004; 351: 1502–1512.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med 2014; 371: 424–433.
Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L et al. A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst 2002; 94: 1458–1468.
Smith MR, Coleman RE, Klotz L, Pittman K, Milecki P, Ng S et al. Denosumab for the prevention of skeletal complications in metastatic castration-resistant prostate cancer: comparison of skeletal-related events and symptomatic skeletal events. Ann Oncol 2015; 26: 368–374.
Logothetis CJ, Basch E, Molina A, Fizazi K, North SA, Chi KN et al. Effect of abiraterone acetate and prednisone compared with placebo and prednisone on pain control and skeletal-related events in patients with metastatic castration-resistant prostate cancer: exploratory analysis of data from the COU-AA-301 randomised trial. Lancet Oncol 2012; 13: 1210–1217.
Fizazi K, Scher HI, Miller K, Basch E, Sternberg CN, Cella D et al. Effect of enzalutamide on time to first skeletal-related event, pain, and quality of life in men with castration-resistant prostate cancer: results from the randomised, phase 3 AFFIRM trial. Lancet Oncol 2014; 15: 1147–1156.
Parker C, Nilsson S, Heinrich D, Helle SI, O'Sullivan JM, Fossa SD et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med 2013; 369: 213–223.
Norgaard M, Jensen AO, Jacobsen JB, Cetin K, Fryzek JP, Sorensen HT . Skeletal related events, bone metastasis and survival of prostate cancer: a population based cohort study in Denmark (1999 to 2007). J Urol 2010; 184: 162–167.
Sathiakumar N, Delzell E, Morrisey MA, Falkson C, Yong M, Chia V et al. Mortality following bone metastasis and skeletal-related events among men with prostate cancer: a population-based analysis of US Medicare beneficiaries, 1999-2006. Prostate Cancer Prostatic Dis 2011; 14: 177–183.
Onukwugha E, Yong C, Mullins CD, Seal B, McNally D, Hussain A . Skeletal-related events and mortality among older men with advanced prostate cancer. J Geriatr Oncol 2014; 5: 281–289.
McDougall JA, Bansal A, Goulart BH, McCune JS, Karnopp A, Fedorenko C et al. The clinical and economic impacts of skeletal-related events among medicare enrollees with prostate cancer metastatic to bone. Oncologist 2016; 21: 320–326.
Moreira DM, Howard LE, Sourbeer KN, Amarasekara HS, Chow LC, Cockrell DC et al. Predicting bone scan positivity in non-metastatic castration-resistant prostate cancer. Prostate Cancer Prostatic Dis 2015; 18: 333–337.
Scher HI, Morris MJ, Basch E, Heller G . End points and outcomes in castration-resistant prostate cancer: from clinical trials to clinical practice. J Clin Oncol 2011; 29: 3695–3704.
Hamilton RJ, Aronson WJ, Terris MK, Kane CJ, Presti JC Jr, Amling CL et al. Limitations of prostate specific antigen doubling time following biochemical recurrence after radical prostatectomy: results from the SEARCH database. J Urol 2008; 179: 1785–1790.
Freedland SJ, Humphreys EB, Mangold LA, Eisenberger M, Dorey FJ, Walsh PC et al. Risk of prostate cancer-specific mortality following biochemical recurrence after radical prostatectomy. JAMA 2005; 294: 433–439.
Aly A, Onukwugha E, Woods C, Mullins CD, Kwok Y, Qian Y et al. Measurement of skeletal related events in SEER-Medicare: a comparison of claims-based methods. BMC Med Res Methodol 2015; 15: 65.
Fizazi K, Carducci M, Smith M, Damiao R, Brown J, Karsh L et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet 2011; 377: 813–822.
James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet 2015; 387: 1163–1177.
Oudard S, Banu E, Medioni J, Scotte F, Banu A, Levy E et al. What is the real impact of bone pain on survival in patients with metastatic hormone-refractory prostate cancer treated with docetaxel? BJU Int 2009; 103: 1641–1646.
Acknowledgements
This study was funded by Bayer HealthCare and supported by the NIH/NCI under Award Number P50CA09231.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Howard, L., De Hoedt, A., Aronson, W. et al. Do skeletal-related events predict overall survival in men with metastatic castration-resistant prostate cancer?. Prostate Cancer Prostatic Dis 19, 380–384 (2016). https://doi.org/10.1038/pcan.2016.26
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2016.26
- Springer Nature Limited
This article is cited by
-
Real-world safety and effectiveness of radium-223 in Japanese patients with castration-resistant prostate cancer (CRPC) and bone metastasis: exploratory analysis, based on the results of post-marketing surveillance, according to prior chemotherapy status and in patients without concomitant use of second-generation androgen-receptor axis-targeted agents
International Journal of Clinical Oncology (2021)
-
Management of bone health in patients with cancer: a survey of specialist nurses
Supportive Care in Cancer (2020)
-
Optimizing antiresorptive treatment in patients with bone metastases: time to initiation, switching strategies, and treatment duration
Supportive Care in Cancer (2019)
-
Harnessing the potential of therapeutic agents to safeguard bone health in prostate cancer
Prostate Cancer and Prostatic Diseases (2018)
-
Skeletal-related events significantly impact health-related quality of life in metastatic castration-resistant prostate cancer: data from PREVAIL and AFFIRM trials
Prostate Cancer and Prostatic Diseases (2017)