Abstract
Purpose
To document the risk of skeletal complications in patients with bone metastases from breast cancer (BC), lung cancer (LC), or prostate cancer (PC) in routine clinical practice.
Methods
We used data from two large US health systems to identify patients aged ≥18 years with primary BC, LC, or PC and newly diagnosed bone metastases between January 1, 1995 and December 31, 2009. Beginning with the date of diagnosis of bone metastasis, we estimated the cumulative incidence of skeletal-related events (SREs) (spinal cord compression, pathologic fracture, radiation to bone, bone surgery), based on review of medical records, accounting for death as a competing risk.
Results
We identified a total of 621 BC, 477 LC, and 721 PC patients with newly diagnosed bone metastases. SREs were present at diagnosis of bone metastasis in 22.4, 22.4, and 10.0 % of BC, LC, and PC patients, respectively. Relatively few LC or PC patients received intravenous bisphosphonates (14.8 and 20.2 %, respectively); use was higher in patients with BC, however (55.8 %). In BC, cumulative incidence of SREs during follow-up was 38.7 % at 6 months, 45.4 % at 12 months, and 54.2 % at 24 months; in LC, it was 41.0, 45.4, and 47.7 %; and in PC, it was 21.5, 30.4, and 41.9 %. More than one half of patients with bone metastases had evidence of SREs (BC: 62.6 %; LC: 58.7 %; PC: 51.7 %), either at diagnosis of bone metastases or subsequently.
Conclusions
SREs are a frequent complication in patients with solid tumors and bone metastases, and are much more common than previously recognized in women with BC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone is among the most common sites of metastasis in patients with lung cancer, and is the most common site in patients with breast and prostate cancer [1, 2]. Patients with bone metastases are at risk of skeletal complications, including spinal cord compression, pathological fracture, surgery to bone, and radiation therapy to alleviate bone pain or prevent fractures. These comorbidities are known collectively as skeletal-related events (SREs). SREs are associated with impaired mobility, reduced quality of life [3], increased mortality [4], and higher healthcare costs [5, 6].
Although estimates of the risk of SREs in patients with bone metastases have been reported in prior studies, their generalizability to clinical practice may be limited. For example, randomized-controlled trials of bone-modifying agents (e.g., bisphosphonates), while a reliable method of evaluating treatment effects, may sacrifice some degree of generalizability (i.e., external validity) to achieve high internal validity [7]. While observational studies do not necessarily suffer from similar problems, their principal shortcoming is their reliability. Studies based on administrative data (e.g., insurance claims) are hampered by the inaccuracy of algorithms that use diagnosis and/or procedure codes (e.g., International Classification of Diseases, 9 th revision: Clinical Modification [ICD-9-CM]) to identify patients with bone metastases as well as those with SREs [6, 8–11]. While medical record review may yield more robust data, the few existing studies either predate widespread use of bisphosphonates or were conducted in settings that may not be generalizable to the United States (US) [12–15]. Some observational studies have additional features, such as atypical definitions of SREs, that may further limit their generalizability to current clinical practice.
To address some of these concerns, we conducted a retrospective study on the risk of SREs in clinical practice in patients with breast, lung, or prostate cancer and newly diagnosed metastases to bone. Our study was based on 15 years of data from two large integrated US health systems.
Methods
Data source
Our study examined data from two large integrated US health systems that serve a combined total of approximately 1.3 million persons annually. Both sites maintain tumor registries that contain information on all newly diagnosed cancers, including primary site, histological type, stage of disease, and first course of treatment. Each site also has a comprehensive electronic medical records (EMR) system that contains information on patient demographics, ambulatory care visits, clinical laboratory and radiology results, inpatient admissions, and a variety of other measures. Information on diagnoses and procedures are captured in administrative data stores using ICD-9-CM and Healthcare Common Procedure Coding System codes. These various data sources are linked through unique system-specific patient identifiers.
To maintain patient confidentiality, all information was extracted and transcribed by medical abstractors onto study case-report forms. We trained the abstractors prior to study initiation, and closely monitored their work while the study was underway to ensure consistency in data collection. We also re-abstracted approximately 30 % of all cases on an ongoing basis, using an independent abstractor who was blinded to the results of the first abstractor. Case-report forms for each pair were compared, and discrepancies were adjudicated by three of the principal investigators (JE, AGG, KER), based on medical record review. During the initial phase of the study, we modified abstractor guidelines as appropriate to clarify data collection procedures.
Study subjects
The source population for the study consisted of all persons, aged ≥18 years, reported in the tumor registry at either study site as having newly diagnosed primary breast, lung, or prostate cancer (“study cancers”) between January 1, 1995 and December 31, 2009 (“study period”). Among these persons, we identified all patients with newly diagnosed metastases to bone, either at initial diagnosis of cancer or at disease progression, based either on (1) notation of metastases to bone in the tumor registry or (2) evidence in administrative data stores of one or more medical encounters with mention of bone metastases (ICD-9-CM 198.5) or primary bone cancer (ICD-9-CM 170.X) on or any time following date of diagnosis of the study cancer.Footnote 1 We reviewed medical records to confirm the diagnosis of bone metastasis; patients without confirmatory evidence were excluded from the study (To ensure that the three cohorts were of approximately equal size, we randomly selected only one third of persons with lung cancer and newly diagnosed bone metastases, as there were approximately three times more patients than those with breast or prostate cancer and bone metastases). After we identified patients with confirmed new diagnoses of bone metastases, we excluded those with evidence of any other invasive primary cancer prior to date of diagnosis of bone metastasis, or in the month immediately thereafter, to minimize the likelihood that another cancer was the source of metastatic disease. We followed all patients for the occurrence of SREs from their date of initial diagnosis of bone metastasis until death, date of last contact (i.e., loss to follow-up), or the end of the study period (i.e., December 31, 2009).
Patient characteristics
Medical record review was used to ascertain age at diagnosis of bone metastasis, gender, and race of all study subjects, whether bone metastases were present at initial diagnosis of cancer, and whether SREs were present at initial diagnosis of bone metastasis. Patients with dates of diagnosis of bone metastasis <60 days following their date of diagnosis of breast, lung, or prostate cancer were considered to have bone metastases at initial diagnosis of cancer; all other patients were designated as having bone metastasis at the date first noted in the medical record.
We used information in administrative data stores and/or the EMR to determine whether patients received intravenous (IV) bisphosphonates (zoledronic acid, pamidronate). We designated such use “primary prophylaxis” if patients had no evidence of an SRE prior to, or up to 7 days following, their first dose of an IV bisphosphonate; all other patients who received IV bisphosphonates were assumed to have received “secondary prophylaxis” (i.e., after an SRE).
Skeletal-related events
The primary measure of interest was the occurrence of SREs any time following initial diagnosis of bone metastasis (“on-study”). SREs comprised spinal cord compression, pathologic fracture, surgery to bone (excluding biopsy only), and radiation to bone. We used findings from conventional x-rays, computerized tomography (CT) scans, magnetic resonance imaging (MRI) scans, myelograms, surgical procedure notes, pathology reports, discharge summaries, and physician progress notes to ascertain history of SREs. Unless confirmed by x-ray, CT scan, or MRI findings, “positive bone scans” were not counted as SREs.
Patients were considered to have experienced spinal cord compression if there was any mention in their medical record of the term “spinal cord compression,” or the terms “spinal cord” or “cord” in conjunction with any of the terms “compression,” “compromise,” “mass-effect,” “impingement,” “displacement,” “effacement,” “indents,” or variants thereof. Patients were considered to have experienced pathologic fracture if there was mention of “pathologic fracture,” “vertebral compression fracture,” or “compression deformity,” provided that these terms were not associated with spinal cord compression, or if the word “vertebrae” or a specific vertebrae (e.g., L1) was used in conjunction with the terms “collapse,” “compression,” “depression,” “wedging,” or variants thereof. Patients were considered to have undergone surgery to bone if there was notation of any operations on bone for repair or palliation of skeletal complications due to bone metastasis, as described in operative/surgical procedure notes and/or hospital discharge summaries (or physician progress notes for procedures done outside the healthcare system). Bone biopsies were not counted as surgery to bone. Patients were considered to have received radiation to bone if a radiation treatment summary described a course of external beam radiation, or a radioactive implant or radioisotope administered for palliation. Receipt of radiation also was established based on notes in the radiation oncology section of the medical record and/or hospital discharge summaries (radiation therapy administered at another facility was ascertained based on physician progress notes or a summary letter in the medical record).
Statistical analyses
We estimated the overall cumulative incidence of on-study SREs in each of the three cohorts, accounting for death as a competing risk because it changes the probability of observing the event of interest (i.e., a skeletal complication) [16–18]. In the presence of a competing risk, the Kaplan–Meier (KM) estimator of cause-specific failure yields biased estimates of the incidence of SREs [19, 20]. We used nonparametric bootstrapping to calculate 95 % confidence intervals for our estimates of cumulative incidence. Cumulative probabilities of survival were estimated using KM methods. We pooled data across both study sites in all of our analyses. All analyses were conducted using SAS Proprietary Software, version 9.2 (SAS Institute Inc., Cary, NC).
Results
Patient characteristics
Across the two study sites, we identified a total of 1,819 patients with newly diagnosed metastases to bone between January 1, 1995 and December 31, 2009, including 621 with breast cancer, 477 with lung cancer, and 721 with prostate cancer (Table 1). Mean (SD) age at diagnosis of bone metastasis was 59.7 (14.0) years for patients with breast cancer, 66.2 (10.3) years for those with lung cancer, and 72.5 (10.4) years for those with prostate cancer (Table 2). Approximately two thirds of study subjects were Caucasian (breast cancer: 66.8 %; lung cancer: 70.4 %; prostate cancer: 60.2 %).
The diagnosis of bone metastasis in patients with breast cancer was most often associated with disease progression (67.0 % of all cases). In patients with bone metastases from lung and prostate cancer, however, it was more often associated with initial diagnosis of cancer (64.4 and 53.5 %, respectively). Approximately one half of all patients in the breast and lung cancer cohorts (47.5 and 50.3 %, respectively) had metastases to other sites at the time of diagnosis of bone metastasis (most commonly, the liver); relatively few patients with prostate cancer (14.7 %), however, had metastases to other sites at initial diagnosis of bone metastasis. Median duration of follow-up from initial diagnosis of bone metastasis was 13.6 months for patients with breast cancer, 3.1 months for those with lung cancer, and 16.6 months for those with prostate cancer.
Use of intravenous bisphosphonates
Approximately one half (55.8 %) of patients with breast cancer received one or more doses of an IV bisphosphonate; rates of use of these agents in patients with lung cancer and prostate cancer were much lower (14.8 and 20.2 %, respectively). In all three groups, initial use of IV bisphosphonates was evenly divided between primary prophylaxis (i.e., prior to an SRE) and secondary prophylaxis (i.e., only after an SRE) (26.3 vs 29.5 %, respectively, for breast cancer; 4.8 vs 9.9 % for lung cancer; 10.6 vs 9.5 % for prostate cancer).
Patients with skeletal-related events
Among 621 patients with bone metastases from breast cancer, 139 (22.4 %) had SREs that were coincident with the diagnosis of bone metastasis (Fig. 1). Among the remaining 482 breast cancer patients without evidence of SREs at study entry, 250 (51.9 %) experienced SREs during follow-up. A total of 389 (62.6 %) patients in the breast cancer cohort therefore had evidence of at least one SRE.
Among 477 patients with bone metastases from lung cancer, 107 (22.4 %) had SREs coincident with the diagnosis of bone metastasis. Among the remaining 370 lung cancer patients without evidence of SRE at study entry, 173 (46.8 %) experienced SREs during follow-up. A total of 280 (58.7 %) patients in the lung cancer cohort therefore had evidence of at least one SRE.
Among 721 patients with bone metastases from prostate cancer, 72 (10.0 %) had SREs coincident with the diagnosis of bone metastasis. Among the remaining 649 prostate cancer patients without evidence of SREs at study entry, 301 (46.4 %) experienced SREs during follow-up. A total of 373 (51.7 %) patients in the prostate cancer cohort therefore had evidence of at least one SRE.
Cumulative incidence of skeletal-related events
Estimates of the cumulative incidence of on-study SREs over 3 years are presented in Fig. 2 and Table 3. In patients with breast cancer, cumulative incidence of SREs was 38.7 % at 6 months, 45.4 % at 12 months, 54.2 % at 24 months, and 57.2 % at 36 months. In patients with lung cancer, the cumulative incidence of SREs was 41.0 % at 6 months, 45.4 % at 12 months, 47.7 % at 24 months, and 48.8 % at 36 months. In patients with prostate cancer, the cumulative incidence of SREs was 21.5 % at 6 months, 30.4 % at 12 months, 41.9 % at 24 months, and 48.9 % at 36 months.
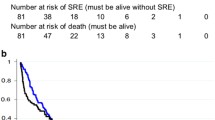
Survival
Cumulative survival in patients with breast cancer was 66.3 % at 1 year and 32.8 % at 3 years; in patients with lung cancer, it was 19.0 and 2.5 %, respectively; and in patients with prostate cancer, it was 73.5 and 43.1 %.
Discussion
Our study sample consisted of more than 1,800 patients with primary breast, lung, or prostate cancer and newly diagnosed metastases to bone—either at initial diagnosis of cancer or at disease progression—in two large integrated US health systems. Almost two thirds (62.6 %) of patients with breast cancer and bone metastases had evidence of SREs, either at study entry or during follow-up. More than one half of all patients with lung cancer and prostate cancer (58.7 and 51.7 %, respectively) had evidence of SREs. When we limited attention to patients without evidence of skeletal complications at study entry, we found that 51.9 % of patients with breast cancer, 46.8 % of those with lung cancer, and 46.4 % of those with prostate cancer developed SREs during follow-up.
It is interesting to compare our estimates of the risk of skeletal complications with those from randomized-controlled trials of bone-modifying agents in similar patient populations. In men with prostate cancer and bone metastases, estimates of SRE risk have ranged from 33 to 59 % [21, 22]. In patients with solid tumors other than breast and prostate (many of whom had non-small cell lung cancer), 43 to 45 % have been reported to develop skeletal complications [23]. These estimates are similar to our own. In women with breast cancer and metastases to bone, however, our estimates of the risk of SREs are substantially higher than those reported in clinical trials of bone-modifying agents (i.e., 40 to 47 %) [24, 25]. The risk of skeletal complications in women with breast cancer and bone metastases in routine clinical practice therefore may be higher than generally recognized.
While these comparisons are interesting, it is important to note that our estimates of SRE risk reflect cumulative incidence, while estimates from clinical trials typically are based on KM methods. The former method treats death as a competing risk, while the KM estimator (specifically, 1 minus the KM estimate of “failure”) censors patients who die. While presentation of data from clinical trials using KM methods is well-established, it overstates the cumulative probability of cause-specific failure (in this instance, SRE) in the presence of a competing risk (e.g., death) in direct proportion to the magnitude of the competing risk(s) [19]. To put this difference into perspective, in Figure 3, we provide KM estimates of the risk of SREs over time among subjects in our study. At 24 months, our KM estimates of SRE risk are 64.8 % for breast cancer, 70.4 % for lung cancer, and 48.2 % for prostate cancer. Although our KM estimate of the risk of skeletal complications in men with prostate cancer is lower than some figures reported from clinical trials [22], this may be because we did not exclude patients who had not failed hormonal therapy, as was done in clinical trials. Our KM estimate of SRE risk in patients with breast cancer is substantially higher than comparable estimates from clinical trials.
Other considerations also should be borne in mind when comparing our findings to those from randomized-controlled trials. First, many patients in our study did not receive anti-resorptive agents, and among those who did, exposure was variable. Our SRE rates therefore would be expected to be higher than those reported from clinical trials in which all patients received such agents. Second, while we began follow-up for all patients at the time of initial diagnosis of bone metastasis, clinical trials had no similar requirement. This may explain why the percentages of patients in our study who had SREs at initial diagnosis of bone metastasis—22.4 % in breast cancer, 22.4 % in lung cancer, 10.0 % in prostate cancer—generally, were lower than the percentages of patients with a history of skeletal complications at study entry in clinical trials of anti-resorptive agents.
Comparison of our findings with those from prior observational studies is also difficult due to differences in the entities considered SREs, different therapeutic eras, different settings of care, and most important, differences in data sources (i.e., chart abstraction vs administrative databases). Nonetheless, our estimates of the total percentage of patients with SREs 24 months following diagnosis of bone metastases (62.6 % for breast cancer, 58.7 % for lung cancer, 51.7 % for prostate cancer) are generally in line with—or higher than—those previously reported [6, 8–15].
We acknowledge various limitations of our study. First, while our sample size was relatively large, the generalizability of our findings to current clinical practice is uncertain, since our study subjects came only from two health systems, and our data spanned a 15-year period during which available therapies and clinical practice changed substantially. Second, because our study was retrospective and based on medical record review, finding evidence of SREs sometimes entailed sifting through a large amount of data. While our abstractors were experienced, trained prior to study initiation, provided with explicit case-finding criteria, and closely monitored while data collection was underway, errors nonetheless were possible. While we were confident of the sensitivity of our methods of case ascertainment, we were concerned about their specificity (i.e., rate of false-positives). A particular concern was our operational definition of spinal cord compression, which was based on the radiologists’ interpretation and report of imaging studies and thus could have reflected some asymptomatic cases. Three of the authors (JE, AGG, KER) therefore reviewed physician progress notes for every patient we counted as having experienced spinal cord compression. Almost all such patients were found to be symptomatic for this diagnosis. We therefore believe that any bias related to problems of specificity is probably small.
The possibility also exists that our estimate of the risk of skeletal complications in women with breast cancer may reflect the fact that we counted vertebral fractures of any degree as SREs. It is our understanding that some prior studies counted vertebral fractures as SREs only if they were accompanied by a marked (e.g., ≥25 %) decrease in total anterior or posterior height from baseline. To better understand the magnitude of bias that may have resulted from this potential difference in methods, we reviewed the records of all 323 breast cancer patients with on-study SREs during the first 36 months of follow-up. We were reassured to find that the vast majority (93.2 %) of these patients experienced SREs other than vertebral compression fractures (data not presented). We therefore do not believe that our comparatively high SRE rates in patients with breast cancer simply are an artifact of our study design and nonspecific methods of case finding.
In summary, while our estimates of the risk of SREs in patients with lung cancer and prostate cancer generally are in line with those reported by others, our findings suggest that skeletal complications may be more common than previously recognized in women with breast cancer and bone metastases.
Notes
Primary bone cancer was included in the initial scan of administrative data stores, as the authors have found in prior work that metastatic disease to bone is sometimes miscoded as primary bone cancer.
References
Mundy GR (2002) Metastasis to bone: causes, consequences and therapeutic opportunities. Nat Rev Cancer 2:284–293
Coleman RE (2001) Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev 27:165–176
Weinfurt KP, Castel LD, Li Y, Timbie JW, Glendenning GA, Schulman KA (2004) Health-related quality of life among patients with breast cancer receiving zoledronic acid or pamidronate disodium for metastatic bone lesions. Med Care 42:164–175
Oefelein MG, Ricchiuti V, Conrad W, Resnick MI (2002) Skeletal fractures negatively correlate with overall survival in men with prostate cancer. J Urol 168:1005–1007
Lage MJ, Barber BL, Harrison DJ, Jun S (2008) The cost of treating skeletal-related events in patients with prostate cancer. Am J Managed Care 14:317–322
Delea T, Langer C, McKiernan J, Liss M, Edelsberg J, Brandman J, Sung J, Raut M, Oster G (2004) The cost of treatment of skeletal-related events in patients with bone metastases from lung cancer. Oncology 67:390–396
Rothwell PM (2005) External validity of randomised controlled trials: “to whom do the results of this trial apply?”. Lancet 365:82–93
Hatoum HT, Lin S, Smith MR, Barghout V, Lipton A (2008) Zoledronic acid and skeletal complications in patients with solid tumors and bone metastases. Cancer 113:1438–1445
Nørgaard M, Jensen AØ, Jacobsen JB, Cetin K, Fryzek JP, Sørenson HT (2010) Skeletal related events, bone metastasis and survival of prostate cancer: a population based cohort study in Denmark (1999 to 2007). J Urol 184:162–167
Jensen AØ, Jacobsen JB, Nørgaard M, Yong M, Fryzek JP, Sørenson HT (2011) Incidence of bone metastases and skeletal-related events in breast cancer patients: a population-based cohort study in Denmark. BMC Cancer 11:29
Jensen AØ, Nørgaard M, Yong M, Fryzek JP, Sørensen HT (2009) Validity of the recorded International Classification of Diseases, 10th edition diagnoses codes of bone metastases and skeletal-related events in breast and prostate cancer patients in the Danish National Registry of Patients. Clin Epidemiol 1:101–108
Sun J, Ahn JS, Lee S, Kim JA, Lee J, Park YH, Park HC, Ahn MJ, Ahn YC, Park K (2011) Predictors of skeletal-related events in non-small cell lung cancer patients with bone metastases. Lung Cancer 71:89–93
Yokomizo A, Koga H, Shinohara N, Miyahara T, Machida N, Tsukino H, Uozumi J, Nishiyama K, Satoh F, Sakai H, Naito S (2010) Skeletal-related events in urological cancer patients with bone metastasis: a multicenter study in Japan. Int J Urol 17:332–336
Plunkett TA, Smith P, Rubens RD (2000) Risk of complications from bone metastases in breast cancer: implications for management. Eur J Cancer 36:476–482
Domchek SM, Younger J, Finkelstein DM, Seiden MV (2000) Predictors of skeletal complications in patients with metastatic breast carcinoma. Cancer 89:363–368
Prentice RL, Kalbfleisch JD (1978) The analysis of failure times in the presence of competing risks. Biometrics 34:541–554
Gaynor JJ, Feuer EJ, Tan CC, Wu DH, Little CR, Straus DJ, Clarkson BD, Brennan MF (1993) On the use of cause-specific failure and conditional failure probabilities: examples from clinical oncology data. J Am Statist Assoc 88:400–409
Pepe MS, Mori M (1993) Kaplan–Meier, marginal or conditional probability curves in summarizing competing risks failure time data. Stat Med 12:737–751
Satagopan JM, Ben-Porat L, Berwick M, Robson M, Kutler D, Auerbach AD (2004) A note on competing risks in survival data analysis. Br J Cancer 91:1229–1235
Gooley TA, Leisenring W, Crowley J, Storer BE (1999) Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 18:695–706
Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L, Chin JL, Vinholes JJ, Goas JA, Chen B, Zoledronic Acid Prostate Cancer Study Group (2002) A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst 94:1458–1468
Fizazi K, Carducci M, Smith M, Damião R, Brown J, Karsh L, Milecki P, Shore N, Rader M, Wang H, Jiang Q, Tadros S, Dansey R, Goessl C (2011) Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet 377:813–822
Rosen LS, Gordon D, Tchekmedyian S, Yanagihara R, Hirsh V, Krzakowski M, Pawlicki M, de Souza P, Zheng M, Urbanowitz G, Reitsma D, Seaman JJ (2003) Zoledronic acid versus placebo in the treatment of skeletal metastases in patients with lung cancer and other solid tumors: a phase III, double-blind, randomized trial—the Zoledronic Acid Lung Cancer and Other Solid Tumors Study Group. J Clin Oncol 21:3150–3157
Stopeck AT, Lipton A, Body JJ, Stegar GG, Tonkin K, de Boer RH, Lichinitser M, Fujiwara Y, Yardley DA, Viniegra M, Fan M, Jiang Q, Dansey R, Jun S, Braun A (2010) Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol 28:5132–5139
Rosen LS, Gordon DH, Dugan W Jr, Major P, Eisenberg PD, Provencher L, Kaminski M, Simeone J, Seaman J, Chen BL, Coleman RE (2004) Zoledronic acid is superior to pamidronate for the treatment of bone metastases in breast carcinoma patients with at least one osteolytic lesion. Cancer 100:36–43
Acknowledgment
Dr. Oster, Dr. Edelsberg, and Ms. Lopez are employed by Policy Analysis Inc., Brookline, MA, which received study funding from Amgen Inc., Thousand Oaks, CA. Dr. Lamerato and Mr. Wolff are employed by Henry Ford Health System, Detroit, MI, which received study funding from Amgen Inc. Dr. Glass and Dr. Richert-Boe are employed by Kaiser Permanente Northwest Region, Portland, OR, which received study funding from Amgen Inc.; Ms. Dodge was employed by Kaiser Permanente Northwest Region at the time the study was conducted. Dr. Chung, Dr. Balakumaran, and Ms. Richhariya are employed by Amgen Inc., and may own stock or stock options in the company.
PAI has full control of all primary data and would agree to allow Supportive Care in Cancer to review the data, if requested.
Conflict of Interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oster, G., Lamerato, L., Glass, A.G. et al. Natural history of skeletal-related events in patients with breast, lung, or prostate cancer and metastases to bone: a 15-year study in two large US health systems. Support Care Cancer 21, 3279–3286 (2013). https://doi.org/10.1007/s00520-013-1887-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-013-1887-3