Abstract
To better understand the patellofemoral joint’s complex anatomy, and perhaps improve surgical outcomes, focus on the distal medial patellar restraints (medial patellotibial ligament (MPTL) and patellomeniscal ligament (MPML)) has been recently scrutinized for their (potential) role in injury and surgery [3, 9, 11–13, 19, 24, 25, 32, 33, 35, 37]. The anatomy of the medial patellar restraints has been previously detailed [24, 34], and described in a companion chapter in this publication. Therefore, it is not included in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
19.1 Introduction
To better understand the patellofemoral joint’s complex anatomy, and perhaps improve surgical outcomes, focus on the distal medial patellar restraints (medial patellotibial ligament (MPTL) and patellomeniscal ligament (MPML)) has been recently scrutinized for their (potential) role in injury and surgery [3, 9, 11,12,13, 19, 24, 25, 32, 34, 36, 38]. The anatomy of the medial patellar restraints has been previously detailed [24, 35], and described in a companion chapter in this publication. Therefore, it is not included in this chapter.
19.2 Biomechanics
A brief review of biomechanics of the distal medial patellar restraints is helpful in understanding possible surgical applications.
The first biomechanical study of medial sided patellar ligaments was by Conlan et al. [6], followed by Desio et al. [7], Hautamaa et al. [16], and Panagiotopoulos et al. [31]. These investigations involved in vitro cutting studies, looking at the difference in lateral patellar translation before and after cutting various medial sided structures. All used a straight lateral force with the knee near full extension. There was agreement by all authors that the MPFL was the primary stabilizer to lateral translation, contributing to 50–60% of restraint. The contribution of the secondary stabilizers was variable, ranging from 0 to 24% (MPTL) and 8 to 38% (MPML), and combined MPTL and MPML 20 to 40% [6, 7, 16, 31].
In 2012, Philippot et al. evaluated patellar tracking in a cadaver model from full extension to 90° of flexion [32]. Acquisitions were made sequentially on a healthy knee, with individual sectioning of the MPFL, and MPTL along with the MPML. The contributions of the MPTL and MPML as a unit against lateral translation increased from 26% in extension to 46% at 90° of flexion. Additionally, the MPTL and MPML at 90° of flexion were responsible for 72% of patellar tilt and 92% of patellar rotation. Isolated contribution of the MPTL and MPML was not evaluated. A comparative description found on these studies is summarized in Table 19.1.
Translating these in vitro studies to the clinical arena, one can surmise that the distal medial patellar complex augments the proximal medial patellar complex in resisting lateral patellar translation in early flexion (Fig. 19.1), and is the main soft-tissue restraint in deeper flexion, where typically the bony walls of a normal trochlear are the main constraint against lateral patellar translation. Trochlea dysplasia can change those contributions, and is possible that in that setting, ligamentous stability becomes more important in the whole arc of motion, including in deeper flexion when the patella should be engaged in the trochlea.
19.3 Clinical
Clinical correlation for MPTL is derived from articles discussing patella motion parameters associated with injury site [11], imaging correlation with injury [37], and reconstruction of the MPTL ligaments [1, 5, 8, 9, 12, 13, 15, 17, 22, 28, 34, 38].
Isolated clinical reports of MPTL reconstructions and their indications have been previously published. In 1922 Galeazzi [10] described a semitendinosus (ST)-patellar tenodesis for treating patellar instability and, in 1998, Rillmann et al. [33] described a transfer of the medial portion of the patellar tendon (PT) when persistent objective instability despite conservative treatment of at least 6 months was present. Both techniques were analogous to MPTL reconstruction. Myers et al. [28] perform MPTL reconstruction in skeletally mature patients with Q < 25° or skeletally immature patients with any Q value. Marcacci et al. [27] showed MPTL reconstruction to be a good option in case of objective habitual patella dislocation or chronic lateral instability; Zaffagnini et al. [38] (2014) used the same technique in case of dislocation, traumatic or atraumatic, with no resolution of symptoms after at least 3 months of conservative treatment. These reported clinical series were without a MPFL reconstruction.
Hinckel et al. [17] proposed augmenting MPFL reconstruction with MPTL reconstruction if the patient presents lateral patellar subluxation in extension, dislocation in flexion, and knee hyperextension associated with generalized ligamentous hyperlaxity, and in select cases of skeletal immaturity when a bony procedure is precluded.
Individual techniques and their results have been summarized in a recent systematic review and were found to have favorable results for the outcome of no recurrence of lateral patellar dislocations [3].
Current use of MPTL reconstructions can be summarized as:
-
1.
Reconstruction of MPTL as the sole soft-tissue restraint for stabilization of the patella against lateral translation. This is most often accomplished by use of the semitendinosus (ST) or utilization of the medial third of the patella tendon.
-
(a)
Semitendinosus: From a historical perspective, Galeazzi in 1922 first described a patellar tenodesis (mimicking the MPTL) for treating lateral patellar instability [10]; some authors use a modification of the Galeazzi ST-patellar tenodesis by passing the tendon through a tunnel drilled in the patella (Fig. 19.2) [1, 2, 13, 26]. Most frequent indication was recurrent lateral patellar dislocation in children, with recurrent rate of continued patellar instability ranging from 0% to 82% [1, 2, 13, 15, 26].
-
(b)
The medial transfer of the medial third of the patellar tendon, which can be likened to a reconstruction of the MPTL.
Many of the published series were before the widespread use of MPFL reconstruction as a surgical option.
-
(a)
-
2.
For patellar stabilization in obligate patellar dislocation in flexion (habitual lateral patellar dislocation): To date, there is only one report in the literature to include a type of MPTL reconstruction (Galeazzi procedure), in addition to lateral release, proximal “tube” realignment of the patella, and transfer of the patellar tendon, into the surgical procedure for habitual patella dislocation. This was a small cohort of children <7 years old with severe generalized laxity and trochlear dysplasia [22]. No patients had recurrence of patellar instability.
-
3.
More recently, outcomes of combined MPFL and MPTL reconstruction have been reported by six authors for treatment of recurrent lateral patellar dislocations with varying techniques:
-
(a)
Use semitendinosus (ST) or gracilis (G) autografts, maintaining their tibial insertion (simulating the MPTL tibial insertion) with extension of the graft proximally to reconstruct the MPFL [5, 9, 12, 34] (Fig. 19.2).
-
(b)
Independent fixation of the auto- or allografts on the patella, one for the MPTL reconstruction and one for the MPFL reconstruction: This allows better positioning of the two grafts on the patella, as well as independent graft tension at different degrees of knee flexion [34].
-
(c)
Use of quadriceps (MPFL) and patellar tendon (MPTL) grafts, with retained patella attachments with independent fixation on the femur (MPFL) and tibia (MPTL) (Fig. 19.3) [17, 18]: This also allows better positioning of the two grafts on the patella, as well as independent graft tension at different degrees of knee flexion.
-
(a)
Reconstruction of the medial patellofemoral ligament and the medial patellotibial ligament with the hamstrings (with permission, Giordano M, Falciglia F, Aulisa AG, Guzzanti V (2012) Patellar dislocation in skeletally immature patients: semitendinosus and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20:1594–1598)
Reconstruction of the medial patellofemoral ligament with a medial slip of the quadriceps tendon, and of the medial patellotibial ligament with the medial third of the patellar tendon (with permission, Hinckel BB, Gobbi RG, Bonadio MB, Demange MK, Pécora JR, Camanho GL. Reconstrução do ligamento patelofemoral medial com tendão quadricipital combinada com patelotibial medial com tendão patelar: experiência inicial. Revista Brasileira de Ortopedia. 2016;51(1):75–82)
19.4 Surgical Considerations
Based on anatomy and biomechanical studies, the distal medial patellar complex (MPTL and MPML) is important in two knee motions: active terminal extension of the knee, where it directly counteracts quadriceps contraction [9, 11] (Fig. 19.1), and deeper knee flexion, when the ligament complex tightens increasing its contribution to lateral patella translation [32] (Fig. 19.4). It also improves kinematics of patellar tilt and rotation throughout range of motion, especially in deep knee flexion [32]. The alignment of the MPML in both extension and flexion helps resist the superior/lateral pull of the patella.
Schematic depiction of the vectors of the MPTL counteracting on the vectors of quadriceps and vastus lateralis at 90° of knee flexion. Note the near-parallel nature of the MPFL and the MPTL (MPFL medial patellofemoral ligament, MPTL medial patellotibial ligament) (Copyright © Regents of the University of Minnesota. All rights reserved)
Current reconstructions of the distal medial restraints are called MPTL reconstructions due to its osseous tibial fixation, but its orientation to the patella tendon may be better directed to mimic the direction of the MPML. Recent anatomic studies suggest that our current use of MPTL reconstruction is more in line with the MPML (approx. 25° angled from the patella tendon) than the MPTL (approx. 10° angled from the patella tendon) [23, 24]. Knowledge to date suggests that MPTL and MPML have similar biomechanical roles and act complementarily. The MPML is more horizontal (oblique) opposing more lateral translation while the MPTL is more vertical, opposing more proximal translation (Fig. 19.5 a, b) [19, 24]. The MPTL and MPML shared a common patellar insertion in many cases [19, 23, 24]. The MPTL inserts on a bony ridge, which was located 5.0 mm distal to the joint line measured on radiographs [24]. By anatomic dissection, the insertion distance from the joint line is 13–14 mm [19, 23].
A cadaveric dissection from the frontal (a) and lateral (b) views depicting the MPML more horizontal (oblique) opposing more lateral translation while the MPTL is more vertical, opposing more proximal translation (Kruckeberg BM, Chahla J, Moatshe G, et al. Quantitative and Qualitative Analysis of the Medial Patellar Ligaments: An Anatomic and Radiographic Study. Am J Sports Med. 2018;46(1):153–162)
Biomechanical studies show the MPML and MPTL to have similar strength, with the MPTL being stiffer than the MPML and the MPFL [19, 25].
Recognizing the tibia insertion site is especially important in children, as the graft should ideally be fixed just above the tibial physis, on the proximal epiphysis of the tibia, so tension can be maintained during growth; this is an agreement with MPFL surgical principles of fixation distal to the femoral growth plate [29].
The closer the tibial insertion is to the joint line the more parallel the MPML is to the MPFL in deeper knee flexion, increasing its contribution to the restraint of lateral translation [20]. Future studies are needed to assess the ideal orientation of a distal patellar pulley to help resist proximal-lateral patellar dislocation, and may differ depending on its use (to help augment the patella near extension or in deep flexion).
For MPTL reconstructions that maintain the hamstrings of tibial insertion, one must note that it is not an anatomic reconstruction, with hamstring insertion more distal and more midline than the MPTL. The tibial insertion of the hamstrings is 41 ± 6.6 mm distal from the tibial plateau and 6.88 ± 1 mm medial to the patellar tendon [14], while the MPTL’s bony attachment is 5.0 to 10 mm distal to the joint line (measured on radiographs) [19, 24].
Clinical and biomechanical data suggests that the MPTL should be tightened at 90o, which makes it easier to achieve similar tension to the patellar tendon. This permits its normal behavior during flexion, without overtensioning and overloading the patellofemoral joint in extension, which could lead to pain and/or elongation [4].
Graft choices vary depending on the technique chosen. As with MPFL reconstruction, surgical principles are more important than graft choice.
The advantages and disadvantages of the different graft choices and techniques are itemized in Table 19.2.
Due to the heterogeneity among case series, lack of comparative studies, and emerging focused anatomic and biomechanical studies, the indications for the clinical use in patellar stabilization do not allow for authoritative statements on the indication for their role, either isolated or combined, in patellar surgical stabilization. Based on the reviewed literature and on the authors’ collective experience, suggested indications for this considering adding MPTL to MPFL procedure are as follows:
-
Active extension subluxation (defined by patellar lateral translation during active quadriceps contraction with the knee fully extended): MPTL is combined with MPFL to restrain lateral and superolateral translation, specifically opposing proximal and lateral quadriceps muscle pull [11].
-
Flexion instability (obligatory patellar dislocation and lateral glide during flexion): To contribute restraint to lateral translation in higher knee flexion angles, as the MPTL tightens with increasing knee flexion [22, 27, 32].
-
Children with excessive number anatomic risk factors (trochlear dysplasia, large quadriceps vector, and patella alta): To add additional support during extension and flexion when there is the risk of complications when doing bony procedures due to open physes [12, 22, 28, 30].
-
Knee hyperextension associated with generalized laxity: To add additional support to functional patella alta and large quadriceps vector during hyperextension [21, 22].
19.4.1 Surgical Technique of MPTL Reconstruction Using Medial Third of PT
The patient is positioned supine on the table, with an applied tourniquet. A midline incision with the knee in 20° of flexion is performed exposing the entire length of the extensor apparatus (Fig. 19.6). It is possible to perform a lateral release when a tight lateral retinaculum is observed with abnormal patellar tilt. Also, a dissection of the vastus medialis oblique is performed, with the aim of making a clearer evaluation of the patellar tracking in the trochlear groove and checking the status of articular cartilage. Then the tibial tuberosity is isolated and the medial third of the patellar tendon is detached from its distal insertion (Fig. 19.7) and prepared with nonabsorbable suture (Fig. 19.8). The graft is medialized and put under tension trying to find a medial insertion location close to the anterior edge of medial collateral ligament. The tourniquet is normally released to avoid any influence on this functional evaluation of patella tracking. Repeated dynamic analysis of patella tracking is carried out to find the precise location where the graft must be fixed with a metal staple (Fig. 19.9). The fixation must lead to patellar stability without creating excessive tension on the ligament band in case of flexed knee. In this position, the patella stability is tested using a finger that tries to pull the patella laterally in the first degrees of flexion. The patella must be stable in every degree of the ROM, without any joint limitation and avoiding any stretching of the ligament structure. It is fundamental to avoid excessive medialization of the patella with the aim of preventing clinical failure. Associated procedures such as tibial tuberosity transfer or trochleoplasty are usually performed before MPTL reconstruction when anatomical abnormalities are present.
19.4.2 Surgical Technique of MPTL Reconstruction Using Free Hamstring Graft
Typically, the MPTL reconstruction is an adjunct to patella stabilization with MPFL. The surgical procedure of MPFL is done in the surgeon’s usual practice. If using an auto hamstring, oftentimes the length is enough to accommodate a single-strand MPFL and MPTL. Using allograft, a peroneal allograft often offers the width needed to divide the graft into two parts, one longer one for the MPFL and one shorter one for the MPTL. The length of the graft can be estimated by the length of the patella tendon.
Fluoroscopy is already in the surgical theater for visualizing MPFL insertion sites.
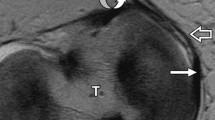
Keeping the C-arm in the lateral position, one identifies the inferior-medial border of the patella, at the distal end of the cartilage border. Patella fixation can be a bony fixation using a 4 mm tunnel, entering on the medial patellar border and exiting on the dorsal surface. If the patella is small or there are concerns of bone quality, one can undermine the periosteum starting just underneath the patella tendon and periosteum, and exiting on the dorsal patella surface. A leader suture is placed in the tunnel for later use. Turning the C-arm to an AP position, one identifies a place on the anteromedial tibia approx. 5–10 mm from the joint line visualized on imaging, angled 25° from the medial patellar tendon border. One marks this spot for later use of the tibial attachment of the MPTL. Fluoroscopy is no longer needed.
Under separate cover, a peroneal allograft is brought into the room typically 8 mm wide and >200 mm in length. The graft is divided into two grafts, each approximately 4 mm in diameter. We put leader sutures on both ends of the graft, trimming the graft as needed to fit a 4 mm tunnel.
The graft is brought to the surgical table. Using the previously placed suture as a passing guide, we threaded the graft into the patellar tunnel (bony or soft tissue). The graft is then sutured into the soft tissue on the dorsal surface of the patella or on itself (Fig. 19.10).
Once the patella insertion is secured, the knee is flexed to 90°. In the pre-designated spot on the anterior tibia (located), a 5.0 mm drill is made in the tibia for a depth of 20 mm. The graft is placed under the patellar retinaculum, and placed over drilled bony tunnel, with the graft secured to the tibia using a 4.75 PEEK “forked-topped” swivelock anchor (Arthrex™) (Fig. 19.11 a, b).
During fixation, the tension in the MPTL should be similar to the one in the patellar tendon to prevent excessive medial pressure.
Full passive range of motion of the knee and medial and lateral patella translation are checked.
References
Aulisa AG, Falciglia F, Giordano M, Savignoni P, Guzzanti V. Galeazzi’s modified technique for recurrent patella dislocation in skeletally immature patients. J Orthop Sci. 2012;17:148–55. https://doi.org/10.1007/s00776-011-0189-1.
Baker RH, Carroll N, Dewar FP, Hall JE. The semitendinosus tenodesis for recurrent dislocation of the patella. J Bone Joint Surg. 1972;54:103–9.
Baumann CA, Pratte EL, Sherman SL, Arendt EA, Hinckel BB. Reconstruction of the medial patellotibial ligament results in favorable clinical outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26:2920–33. https://doi.org/10.1007/s00167-018-4833-6.
Beck P, Brown NAT, Greis PE, Burks RT. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:1557–63. https://doi.org/10.1177/0363546507300872.
Brown GD, Ahmad CS. Combined medial patellofemoral ligament and medial patellotibial ligament reconstruction in skeletally immature patients. J Knee Surg. 2008;21:328–32.
Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75:682–93.
Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59–65.
Drez D Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298–306. https://doi.org/10.1053/jars.2001.21490.
Ebied AM, El-Kholy W. Reconstruction of the medial patello-femoral and patello-tibial ligaments for treatment of patellar instability. Knee Surg Sports Traumatol Arthrosc. 2012;20:926–32. https://doi.org/10.1007/s00167-011-1659-x.
Galeazzi R. New applications of muscle and tendon transplant. Arch Ortop. 1922;38:315–23.
Garth WP Jr, Connor GS, Futch L, Belarmino H. Patellar subluxation at terminal knee extension: isolated deficiency of the medial patellomeniscal ligament. J Bone Joint Surg Am. 2011;93:954–62. https://doi.org/10.2106/JBJS.H.00103.
Giordano M, Falciglia F, Aulisa AG, Guzzanti V. Patellar dislocation in skeletally immature patients: Semitendinosus and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20:1594–8. https://doi.org/10.1007/s00167-011-1784-6.
Grannatt K, Heyworth BE, Ogunwole O, Micheli LJ, Kocher MS. Galeazzi semitendinosus tenodesis for patellofemoral instability in skeletally immature patients. J Pediatr Orthop. 2012;32:621–5. https://doi.org/10.1097/BPO.0b013e318263a230.
Grassi CA, Fruheling VM, Abdo JC, de Moura MFA, Namba M, da Silva JLV, da Cunha LAM, de Oliveira Franco APG, Costa IZ, Filho ES. Estudo anatômico da inserção dos tendões flexores do joelho/[Hamstring tendons insertion—an anatomical study]. Rev Bras Ortop. 2013;48:417–20. https://doi.org/10.1016/j.rbo.2012.07.011.
Hall JE, Micheli LJ, McManama GB Jr. Semitendinosus tenodesis for recurrent subluxation or dislocation of the patella. Clin Orthopaed Relat Res. 1979;144:31–5.
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthopaed Relat Res. 1998;349:174–82.
Hinckel BB, Gobbi RG, Bonadio MB, Demange MK, Pécora JR, Camanho GL. Reconstruction of medial patellofemoral ligament using quadriceps tendon combined with reconstruction of medial patellotibial ligament using patellar tendon: initial experience. Rev Bras Ortop. 2016;51:75–82. https://doi.org/10.1016/j.rbo.2015.03.003.
Hinckel BB, Gobbi RG, Demange MK, Bonadio MB, Pecora JR, Camanho GL. Combined reconstruction of the medial patellofemoral ligament with quadricipital tendon and the medial patellotibial ligament with patellar tendon. Arthrosc Tech. 2016;5:e79–84. https://doi.org/10.1016/j.eats.2015.10.004.
Hinckel BB, Gobbi RG, Demange MK, Pereira CAM, Pecora JR, Natalino RJM, Miyahira L, Kubota BS, Camanho GL. Medial patellofemoral ligament, medial patellotibial ligament, and medial patellomeniscal ligament: anatomic, histologic, radiographic, and biomechanical study. Arthroscopy. 2017;33:1862–73. https://doi.org/10.1016/j.arthro.2017.04.020.
Hinckel BB, Gobbi RG, Kaleka CC, Camanho GL, Arendt EA. Medial patellotibial ligament and medial patellomeniscal ligament: anatomy, imaging, biomechanics, and clinical review. Knee Surg Sports Traumatol Arthrosc. 2018;26:685–96. https://doi.org/10.1007/s00167-017-4469-y.
Howells NR, Eldridge JD. Medial patellofemoral ligament reconstruction for patellar instability in patients with hypermobility: a case control study. J Bone Joint Surg. 2012;94:1655–9. https://doi.org/10.1302/0301-620X.94B12.29562.
Joo SY, Park KB, Kim BR, Park HW, Kim HW. The ‘four-in-one’ procedure for habitual dislocation of the patella in children: early results in patients with severe generalised ligamentous laxity and aplasis of the trochlear groove. J Bone Joint Surg. 2007;89:1645–9. https://doi.org/10.1302/0301-620X.89B12.19398.
Kaleka CC, Aihara LJ, Rodrigues A, de Medeiros SF, de Oliveira VM, de Paula Leite Cury R. Cadaveric study of the secondary medial patellar restraints: patellotibial and patellomeniscal ligaments. Knee Surg Sports Traumatol Arthrosc. 2017;25:144–51. https://doi.org/10.1007/s00167-016-4322-8.
Kruckeberg BM, Chahla J, Moatshe G, Cinque ME, Muckenhirn KJ, Godin JA, Ridley TJ, Brady AW, Arendt EA, LaPrade RF. Quantitative and qualitative analysis of the medial patellar ligaments: an anatomic and radiographic study. Am J Sports Med. 2018;46:153–62. https://doi.org/10.1177/0363546517729818.
LaPrade MD, Kallenbach SL, Aman ZS, Moatshe G, Storaci HW, Turnbull TL, Arendt EA, Chahla J,LaPrade RF. Biomechanical evaluation of the medial stabilizers of the patella. Am J Sports Med. 2018;46:1575–82. https://doi.org/10.1177/0363546518758654.
Letts RM, Davidson D, Beaule P. Semitendinosus tenodesis for repair of recurrent dislocation of the patella in children. J Pediatr Orthop. 1999;19:742–7.
Marcacci M, Zaffagnini S, Lo Presti M, Vascellari A, Iacono F, Russo A. Treatment of chronic patellar dislocation with a modified Elmslie-Trillat procedure. Arch Orthop Trauma Surg. 2004;124:250–7. https://doi.org/10.1007/s00402-003-0511-2.
Myers P, Williams A, Dodds R, Bulow J. The three-in-one proximal and distal soft tissue patellar realignment procedure. Results, and its place in the management of patellofemoral instability. Am J Sports Med. 1999;27:575–9.
Nelitz M, Reichel H, Dornacher D, Lippacher S. Anatomical reconstruction of the medial patellofemoral ligament in children with open growth-plates. Arch Orthop Trauma Surg. 2012;132:1647–51. https://doi.org/10.1007/s00402-012-1593-5.
Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N. The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med. 2009;37:1814–20. https://doi.org/10.1177/0363546509333480.
Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14:7–12. https://doi.org/10.1007/s00167-005-0631-z.
Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20:331–6. https://doi.org/10.1007/s00167-011-1598-6.
Rillmann P, Dutly A, Kieser C, Berbig R. Modified Elmslie-Trillat procedure for instability of the patella. Knee Surg Sports Traumatol Arthrosc. 1998;6:31–5. https://doi.org/10.1007/s001670050069.
Sobhy MH, Mahran MA, Kamel EM. Midterm results of combined patellofemoral and patellotibial ligaments reconstruction in recurrent patellar dislocation. Eur J Orthop Surg Traumatol. 2013;23:465–70. https://doi.org/10.1007/s00590-012-0999-7.
Tanaka MJ, Chahla J, Farr J 2nd, LaPrade RF, Arendt EA, Sanchis-Alfonso V, Post WR, Fulkerson JP. Recognition of evolving medial patellofemoral anatomy provides insight for reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;27(8):2537–50. https://doi.org/10.1007/s00167-018-5266-y.
Thawait SK, Soldatos T, Thawait GK, Cosgarea AJ, Carrino JA, Chhabra A. High resolution magnetic resonance imaging of the patellar retinaculum: Normal anatomy, common injury patterns, and pathologies. Skelet Radiol. 2012;41:137–48. https://doi.org/10.1007/s00256-011-1291-3.
Tompkins MA, Rohr SR, Agel J, Arendt EA. Anatomic patellar instability risk factors in primary lateral patellar dislocations do not predict injury patterns: an MRI-based study. Knee Surg Sports Traumatol Arthrosc. 2018;26:677–84. https://doi.org/10.1007/s00167-017-4464-3.
Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A, Marcacci M. Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2491–8. https://doi.org/10.1007/s00167-013-2751-1.
Acknowledgment
We thanks Mrs. Silvia Bassini for iconographic material.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 ESSKA
About this chapter
Cite this chapter
Hinckel, B.B., Zaffagnini, S., Arendt, E.A. (2020). Medial Patellotibial Ligament: Clinical Application and Surgical Reconstruction for Patellar Stabilization. In: Dejour, D., Zaffagnini, S., Arendt, E., Sillanpää, P., Dirisamer, F. (eds) Patellofemoral Pain, Instability, and Arthritis. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-61097-8_19
Download citation
DOI: https://doi.org/10.1007/978-3-662-61097-8_19
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-61096-1
Online ISBN: 978-3-662-61097-8
eBook Packages: MedicineMedicine (R0)