Abstract
Purpose
Patellar instability is a frequent condition in children and adolescents. The problem can be associated with malalignment resulting from different anatomical abnormalities. Several surgical procedures have been suggested for recurrent patellar dislocation consequent to failed conservative treatment.
Methods
We present an original surgical procedure for reconstructing both the medial patellofemoral (MPFL) and medial patellotibial ligaments (MPTL) by semitendinosus (ST) tendon with gracilis (G) autograft augmentation in skeletally immature patients with recurrent patellar dislocation.
Results
This technique is effective and permits satisfactory patellar congruency documented by static and dynamic CT.
Conclusions
The operation is associated with optimal functional results and is minimally invasive, causing no growth disturbance.
Level of evidence
Expert opinion, Level V.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dislocation of the patella may be congenital or acquired [4]. Different abnormalities can cause this severe degree of instability: flattened or hypoplasic lateral femoral condyle, hypoplasic or high patella, trochlear groove dysplasia (short and shallow), axial (genu valgum) and sagittal (genu recurvatum) deviations or torsional deformities of the legs (excessive femoral anteversion or external tibial torsion), lateral offset of the tibial tuberosity, generalized ligamentous laxity, and contracture dysfunction of vastus lateralis [4, 16, 21, 22]. These combined anatomic and constitutional factors predispose the patella to lateral dislocation, especially in early flexion.
In 1922, Galeazzi described an effective technique for anatomical physeal-sparing medial patellotibial ligament reconstruction. The purpose of the technique is to direct the pull of the quadriceps in line with the intercondylar notch of the femur. The aim was reached reconstructing MPTL that contributes to establish the height of the patella in relation to the femoral condyle and also transmits the force of the quadriceps contraction to the tibia [15, 20]. Moreover, Panagiotopoulos et al. [23] in a recent cadaveric study on static medial patellar stabilizer has evidenced that MPTL also contributes to medial stability for 13%.
Hall et al. [13] reported a 62% good to excellent results, and Baker et al. [4] reported successful outcomes in 81% of their 53% cases treated with their technique, and Letts et al. [17] reported good to excellent results in 88% of cases treated.
The role of MPFL as guy wire for static stabilizer of the patella in the sulcus [24] was better defined.
In fact, biomechanical researches demonstrate that the MPFL accounts for 50–60% of the medial soft tissue restraining force against lateral patellar subluxation or dislocation [6].
In recent years, increasing interest has been observed in literature for surgical reconstruction of MPFL with good results [7]. The author underlined that the indication for MPFL reconstruction has not completely been clarified. In fact, indications may be different due to various predisposing factors because of severe height patella, and severe Q-angle may have a great influence on MPFL reconstruction [19].
When patellar instability, especially in growing age, is sustained by excessive height of the patella, severe Q-angle, malalignment of the lower limbs, trochlear dysplasia, and iperlaxity, the Galeazzi’s procedure lacks of the MPFL reconstruction and the isolated MPFL reconstruction lacks of MPTL to control patellar height.
Therefore, the suggested technique is proposed to combine the reconstruction of both the MPFL and the MPTL and to enhance the strength of the graft to achieve greater stability and thus better results.
The combined use of ST and G, published by Drez et al. [11] for adults, does not add morbidity to the intervention, which provides more strength and durability of the procedure, bearing in mind that adolescent often have a growing patellar instability linked to several factors. Furthermore, the procedure is completely physeal-sparing.
Technical note
All the procedures described in this investigation were approved by the local ethics committee. All the patients and their parents gave written informed consent for inclusion in the present study.
The choice to reconstruct both MPFL and MPTL ligaments is based on the reported importance of MPFL as primary medial patellar stabilizer [1, 8, 10] and of MPTL as accessory stabilizer [14] and patellar height regulator during strong quadriceps contraction [2]. We use combined MPFL/MPTL reconstruction by ST tendon and G autograft augmentation to maintain patellar stability stress occurring during the growth period.
With the patient placed in a supine position on a standard operating table, a pneumatic tourniquet is applied to the proximal thigh. Joint cartilage and menisci conditions are assessed by arthroscopy.
The surgical technique was routinely performed by four mini-incisions, except for the first two cases in which intervention was performed by a longitudinal parapatellar medial incision.
First, a transversal skin incision is made medial to the anterior tibial apophysis to identify the insertion of the pes anserinus tendons. The ST and G tendons are identified and divided from the musculo-tendinous junction, preserving the distal insertion site. The tendons must be at least 12–13 cm long. A second mini-incision is made just medial to the inferior patellar apex. An additional 2 cm incision is made at the supero-medial border of the patella. A longitudinal 2-mm Kirschner nail is driven into the medial third of the patella (Fig. 1). A distal to proximal intraosseus longitudinal tunnel is made with a 4-mm drill and is then expanded to a diameter of 4,5 mm. After division, the tendon grafts are passed through the soft tissue from their distal insertion to the beginning of the patellar tunnel (Fig. 2). ST and G tendons are brought distal to proximal into the tunnel, exiting through the upper tunnel opening. By traction of the proximal portion of the autografts, the distal portion of ST and G tendons is tensioned in full knee extension, drawing the patella medially and downwards to obtain its correct centering in the trochlear. Using a bioabsorbable suture, the distal ST and G autografts are immediately sutured under tension to the periosteum of the distal pole of the patella (Fig. 2). The femoral adductor tubercle is exposed by a 3 cm skin incision made at the middle of its medial aspect, and the proximal portions of the ST and G tendons are tunnelled into the medial parapatellar subfascial soft tissue.
After dissection, the harvested semitendinosus and gracilis tendons are sutured, preserving the distal insertion site. A second mini-incision is made just medial to the inferior patellar apex. An additional 2 cm incision is made at the supero-medial border of the patella. A longitudinal 2-mm Kirschner nail is driven into the medial third of the patella
With the patella well situated in the trochlea, the proximal parts of the ST and G tendons are tensioned maximally at 30°–45° of flexion [18] and fixed at the middle of the edge of adductor tubercle of the medial femoral condyle by a titanium suture anchor (Fig. 3) (Arthrex Corkscrew suture anchor with needles: 5 mm × 12.1 mm with two size 0 fiberwire). The ST and G autografts are secured to the periosteum of the proximal pole of the patella with a bioabsorbable suture. The final stability of the patella is checked in full extension of the knee allowing congruent smooth tracking of the patella. The free movement of the knee is carefully verified, testing the motion in flexion up to 90°. The surgical technique was performed by one senior surgeon (GV). The knee is then positioned in a 20° flexion brace for 3 weeks. CT scan was performed postop to verify that there was no overcorrection, which could lead to a medial patellar subluxation. Isometric quadriceps muscle exercises are started in brace the day after surgery. Once immobilization is stopped, control passive motion of the knee and volitional exercises combined with neuromuscular electrical stimulation are begun, as well as quadriceps and hamstring muscles strengthening exercises. One month after surgery, knee flexion of more than 90° and progressive weight bearing until complete are allowed. Sports activities are restricted for 4–6 months.
A fouth skin incision is made to expose the femoral adductor tubercle. The proximal portions of the ST and G tendons are tunnelled into the medial parapatellar subfascial soft tissue. The ST and G tendons are tensioned at 30°–45° of flexion and fixed at the middle of the edge of adductor tubercle of the medial femoral condyle by a titanium suture anchor
Preoperative assessment includes study of axial and sagittal deviations and torsional deformities of the lower limb. Physical examination determines joint stability, patellar tracking, Q-angle, knee range of motion, and muscular tension.
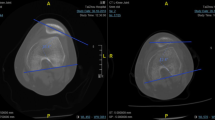
The knee was routinely submitted to radiograph antero-posterior and lateral view at 30° of flexion, and MRI as well as static and dynamic CT scan [12] to assess the patellofemoral relationship (Fig. 4). In the initial stages of an acute phase of recurrent dislocation all clinical evaluations and dynamic CT examination may be difficult to perform.
Female athlete, 12 years old, with severe patellar instability (recurrent dislocation) and generalized ligament laxity. New acute patellar dislocation (third episode). a Preoperative standard X-Ray, lateral view showing a high patella. b The MPFL tear with a minimal osteochondral fragment avulsed from patellar insertion at MRI study. c The TAGT was 1.2 cm on CT scan
In case of recurrent patellar dislocation with excessive patella alta, severe Q-angle (>15°), trochlear dysplasia, TAGT (distance between anterior tuberosity and the deeper part of the groove) >1.2 cm at CT examination, and hyperlaxity the proposed technique is indicated.
Discussion
The most important finding of this technique is that it allows the immediate correction of patellofemoral malalignment followed by clinical stability confirmed by static and dynamic CT examination at 24 months in the first patients operated.
Various procedures have been described for the treatment for recurrent dislocation of the patella [11]. In growing patients, physeal-sparing procedures are recommended [4, 9]. The reconstruction of medial structures is an important factor in stabilization of the knee during flexion and extension. The importance of MPFL in controlling lateral patellar dislocation has been well documented in different biomechanical studies [8, 10]. MPTL also plays an important role, not so much as a secondary medial patellar stabilizer [14] as helping the patellar tendon to limit upward displacement of the patella during strong quadriceps contraction [2]. In case of recurrent patellar dislocation with excessive patella alta, severe Q-angle (>15°), trochlear dysplasia, TAGT > 1.2 cm at CT examination, and iperlaxity, the Galeazzi’s procedure, or its modifications, lacks of the MPFL reconstruction, and the isolated MPFL reconstruction lacks of MPTL to control patellar height.
Recently, various surgical procedures have been proposed for the reconstruction of both MPFL and MPTL using the semitendinosus tendon alone [5, 6, 18]. To our knowledge, to date no surgical procedures have been published, which combine ST autograft with G tendon augmentation in skeletally immature patients. The G tendon augmentation can improve the opposition of the patella to quadriceps contraction and favor patellofemoral stability. This neo-ligament consisting of two tendons is more resistant to ligamentous laxity and to high patella and/or abnormal TAGT that often characterize the recurrent patellar dislocation in skeletally immature patients.
The technique does not require a lateral release and/or medial retinaculum reefing and can be carried out using mini-incisions (Fig. 3), thus reducing the morbidity connected with medial longitudinal parapatellar incision. For female patients, the cosmetic aspect is significant [4].
A wise surgical approach is required for treatment for recurrent lateral patellar dislocation in young patients.
The described technique is a good compromise for restoring a more complete medial patellar restraint with minimal soft tissue exposure. The question of isometry in MPFL and MPTL reconstruction remains open and debatable [3].
The technique should be considered on a large number of cases. It is also indispensable that the results should be reviewed when patients have reached full skeletal maturity. However, the clinical results as well as the static and dynamic CT evaluation at 24-months postsurgery are satisfactory (Fig. 5).
Static and dynamic CT showing the patellafemoral congruency at 6 months (a) and 24 months (b) follow-up. The parapatellar medial hole of semitendinosus and gracilis autografts appears in the medial third of the patella. At 24 months follow-up, (b) the osteochondral avulsed fragment appears to be fused to patellar bone
Another limitation is that the technique could not be definitive because patellar instability in children and adolescent is often supported by different predisposing factors that may require additional procedures if they worsen during growth.
Various techniques were proposed for the treatment for patellar instability with good but not completely satisfactory results. The suggested technique is based on the reinforced reconstruction of two major components for the stability of the patella in the sagittal and coronal views. The clinical relevance of this technique is that it allows patellar stability and has the potential to keep it longer to reach a better functional outcome than other surgical options already proposed in case of recurrent patellar dislocation with excessive patella alta, severe Q-angle (>15°), trochlear dysplasia, TAGT > 1.2 cm at CT examination, and iperlaxity.
Conclusion
The procedure described is original because, to our knowledge, the combined reconstruction of MPFL and MPTL by ST and G tendon augmentation in adolescents has not been reported in literature. This technique is effective and avoids recurrent patellar dislocation, restores patellofemoral congruency in both static and dynamic CT conditions, and can be carried out in a minimally invasive fashion. The procedure is totally physeal-sparing.
References
Amis AA, Firer P, Mountney J, Senavongse W, Thomas NP (2003) Anatomy and biomechanics of the medial patellofemoral ligament. Knee Sept 10(3):215–220
Arendt EA (2007) Anatomy and biomechanics of the patellar ligaments. Tecniche chirurgiche in ortopedia e traumatologia; 5:13–18
Arendt EA (2009) MPFL recontruction for PT instability. The soft (tissue) approach. Orthop Traumatol Surg Res 95(8 Suppl 1):S97–S100
Baker RH, Carroll N, Dewar FP, Hall JE (1972) The semitendinosus tenodesis for recurrent dislocation of the patella. J Bone Joint Surg Br Feb 54(1):103–109
Balsamo LH, Gerbino PG (2006) Semitendinosus tenodesis to the patella for recurrent lateral subluxation of the patella. In: Micheli LJ, Kocher M (eds) The pediatric and adolescent knee. Patellofemoral dysfunction. Saunders, pp 169–173
Brown GD, Ahmad CS (2008) Combined medial patellofemoral ligament and patellotibial ligament reconstruction in skeletally immature patients. J Knee Surg; 21:328–332
Buckens CF, Salis DB (2010) Reconstruction of the medial patellofemoral ligament for treatment of patellofemoral instability. A systematic review. Am J Sports Med 38:181–188
Conlan T, Garth WP, Lemons JE (1993) Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. May; 75(5):682–693
Cook JL, Micheli LJ (1998) Pediatric lateral retinacular release with medial plication under arthroscopic control. In: Micheli LJ, Kocher M (eds) The pediatric and adolescent knee. Patellofemoral dysfunction. Saunders, pp 163–166
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sport Med; 26:59–65
Drez D Jr, Bradley Edwards T, Williams CS (2001) Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy 17:298–306
Guzzanti V, Gigante A, Di Lazzaro A, Fabbriciani C (1994) Patellofemoral malalignment in adolescents Computerized tomographic assessment with or without quadriceps contraction. Am J Sports Med 22:55–60
Hall JE, Micheli LJ, McManama GB Jr (1979) Semitendinosus tenodesis for recurrent subluxation or dislocation of the patella. Clin Orthop Relat Res 144:31–35
Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM (1998) Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 349:174–182
James SL (1979) Chapter 8 Chondromalacia of the patella in adolescent. In: Kennedy JC (ed) The injured adolescent knee. Williams and Wilkins Company, Baltimore, pp 205–271
Joo SY, Park KB, Kim BRK, Park HW, Kim BR, Park HW (2007) The “four-in-one” procedures for habitual dislocation of the patella in children. J Bone Joint Surg Br 89(12):1645–1649
Letts RM, Davidson D, Beaule P (1999) Semitendinosous tenodesis for repair of recurrent dislocation of the patella in children. J Pediatr Orthop; 19:742–747
Nietosvaara Y, Paukku R, Palmu S, Donnel ST (2009) Acute patellar dislocation in children and adolescent. Surgical technique. J Bone Joint Surg: 91A(Suppl 2):139–145
Nomura E, Inoue M, Kobayashi S (2007) Long term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 35(11):1851–1859
Noyes FR, McGinnis GH, Mooar LA (1984) Functional disability in the anterior cruciate insufficient knee syndrome: review of knee rating systems and projected risk factors in determining treatment. Sports Med; 1:278–302
Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N (2009) The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med 37:1814–1820
Palmu S, Kallio PE, Donnel ST, Helenius I, Nietosvaara Y (2008) Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg 90A:463–470
Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G (2006) Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 14:7–12
Smillie IS (1971) Injured of the knee joint, 4th edn. Williams & Wilkins, Baltimore, pp 205–223
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Giordano, M., Falciglia, F., Aulisa, A.G. et al. Patellar dislocation in skeletally immature patients: semitendinosous and gracilis augmentation for combined medial patellofemoral and medial patellotibial ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 20, 1594–1598 (2012). https://doi.org/10.1007/s00167-011-1784-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-011-1784-6