Abstract
Previously considered the hidden lesion of the knee, ramp lesions are longitudinal tears involving the peripheral attachment of the posterior horn of the medial meniscus. More prevalent in association with anterior cruciate ligament (ACL) injuries than previously recognised, ramp lesions are consequently garnering renewed interest. Biomechanical studies suggest that ramp lesions contribute to increased anterior tibial translation and external rotational instability in ACL-deficient knees. ACL reconstruction in isolation does not address these issues, and therefore ramp lesions should be repaired at the time of initial ACL reconstruction. However, ramp lesions are difficult to diagnose preoperatively on magnetic resonance imaging (MRI) and consequently often go undiagnosed. Also, arthroscopic diagnosis of a ramp lesion can be challenging, particularly when viewing through anterior portals alone. To diagnose these lesions accurately, the posterior compartment of the knee has to be examined and evaluated with arthroscopic probing of the posterior horn of the medial meniscus. The use of a posteromedial portal can often facilitate this. Treatment options include nonsurgical management, all-inside meniscal repair, or inside-out meniscal repair. Rehabilitation should follow standard guidelines for either meniscal repair in the case of isolated ramp lesion repair or ACL reconstruction if performed in combination.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
6.1 Introduction
Meniscal lesions occur in association with ACL tears over 60 % of the time [1–5]. In the setting of an acute ACL tear, lateral meniscal tears occur with slightly greater frequency than medial meniscus tears, with a mean distribution of 56–44 %, respectively. However, in the setting of chronic ACL deficiency, medial meniscus tears are much more common [6]. More than 75 % of tears of the medial meniscus in ACL-deficient knees occur in the periphery of the posterior horn [2, 6, 7].
“It saw you but you didn’t see it. Jack Hughston, Orthopaedic Surgeon”
One of the main issues with lesion at the posterior aspect of the meniscus is that they are difficult to visualise from standard anterior portals and are, therefore, frequently missed. The term hidden lesion has quite aptly been used to describe these meniscal tears. In addition, the term ramp lesion has emerged in the orthopaedic vernacular as another descriptive term [3]. The purpose of this chapter is to explain what exactly a ramp lesion is, how can it be diagnosed and how best to treat it.
6.2 What Is a Ramp Lesion?
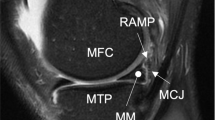
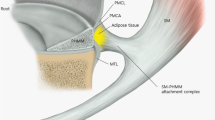
The area on the posterior aspect of the meniscal rim adjoining the meniscocapsular junction is called the meniscal ramp (Fig. 6.1). A ramp lesion, so described by Strobel in 1998 [8], is a longitudinal tear in the ramp area and is typically associated with ACL deficiency. Subsequent authors have extended the definition to a tear less than 2.5 cm in length involving the meniscosynovial or meniscocapsular attachments of the posterior horn of the medial meniscus (red-red zone) [9, 10]. Disruption of the meniscotibial ligaments of the posterior horn of the medial meniscus is most often recognised as a separate entity [2, 11].
(a) Arthroscopic view of the posteromedial aspect of a right knee through the intercondylar notch with a 70° arthroscope; the black arrow marks the ramp lesion, the red arrow the posterior capsule, and the yellow the posterior horn of the medial meniscus.(b) Arthroscopic view of the same patient with a 30° arthroscopic from the posteromedial portal, demonstrating the same ramp lesion with meniscocapsular separation (white arrow) (These photographs are courtesy of Professor Joon Wang, Samsung Medical Centre, Sungkyunkwan University Medical School, Seoul, Korea)
6.3 How Do Ramp Lesions Occur?
The pathogenesis of ramp lesions can be explained by an understanding of the anatomy of the medial meniscus. The medial meniscus is a crescentic fibrocartilage covering approximately 50 % of the medial tibial plateau. It measures roughly 11 mm posteriorly and becomes narrower anteriorly towards the anterior meniscal root [10, 12]. Anatomically, it can be divided into three zones, the anterior horn, the body and the posterior horn (Fig. 6.2).
Sagittal fat-saturated T2-weighted sequence showing medial meniscocapsular separation with thin fluid interposed between the posterior horn of the medial meniscus and capsule (arrow) [28]
The medial meniscus is anchored to the medial tibial plateau by the anterior and posterior roots [13]. The body of the meniscus attaches to the adjacent joint capsule and to the tibia by the meniscotibial ligaments. The meniscus is thick peripherally where it attaches to the joint capsule and tapers to a thin, freely mobile edge centrally [14].This triangular or wedge cross section deepens the tibial articular fossa; enhances load bearing, force distribution and joint stability functions; and influences the stress and strain on the meniscus during activities [15].
The wedge shape of the anterior horn resists posterior translation of the tibia, and similarly, the posterior horn resists anterior tibial translation. As such, the posterior horn plays a fundamental role as a secondary stabiliser of the knee [9, 16, 17]. In the setting of an ACL-deficient knee, it must assume a more primary role in controlling anterior translation [18]. This results in increased loading of the posterior horn of the medial meniscus, increasing forces here by up to 100 %, which is reflected in the high numbers of peripheral medial meniscus posterior horns associated with chronic ACL tears [19].
Ramp lesions can occur acutely at the time of ACL ruptures or develop in the chronically ACL-deficient knee. Acute ramp lesion tears occur as a result of the high forces, which are transmitted through the posteromedial capsule during valgus strain and internal rotation of the tibial and axial loading of the knee [2].
Hughston’s [20] proposed mechanism for medial meniscus tears in the ACL-deficient knee is that the loss of ACL function results in increased tibial translation, allowing the meniscus to become wedged between the femur and the tibia. At the same time, the semimembranosus muscle contracts along the posterior capsule, focusing a large amount of stress at the peripheral meniscus. If the contraction is intense enough, the medial meniscus will either tear peripherally or tear at the meniscocapsular junction: the ramp area. This may happen at the time of injury or during subsequent instability episodes [9, 21].
Song et al. have recently proposed that an increased medial meniscal slope is an independent risk factor of a concomitant ramp lesion in noncontact ACL injuries [19]. One of the issues with this theory is that the very presence of a tear may have an impact on the tibial slope. Also, the difference in mean medial meniscal slope between those patients with a ramp lesion and those without in noncontact ACL injuries was only 1.5°. Therefore, the clinical utility of this reading is of questionable value.
6.4 How Common Are Ramp Lesions?
Ramp lesions occur most commonly in association with ACL ruptures. Whether acute or chronic, the incidence ranges from 9 to17 % [9, 22]. Other reported risk factors include male sex, younger age and time from ACL injury to surgery [9]. Liu et al. [9] found the prevalence of ramp lesions in the presence of ACL injury in males to be 18.6 %, while the prevalence in female patients was 12.0 %. A significantly higher prevalence of ramp tears was detected in patients younger than 30 years of age, compared to those aged over 30. They also found a significantly higher prevalence of ramp tears in patients with chronic ACL tear (18.8 %) compared to patients with an acute (less than 6 weeks old) ACL tear (12.7 %). The time from injury to ACL reconstruction was reported to be associated with an increased incidence. This assertion was corroborated by Papastergiou et al., who reported that the earliest point of a significantly higher incidence of meniscal tears in an ACL-deficient knee occurred 3 months following injury [23]. Therefore, the authors recommended that ACL reconstruction should ideally be performed within 3 months of injury to mitigate against this risk. However, the prevalence of ramp lesions continues to increase significantly until 24 months post ACL tear where it plateaus [9]. Furthermore, it is likely that the incidence of ramp lesions will increase as a greater awareness of this pathology develops.
6.5 Why Are Ramp Lesions Important?
The posterior horn of the medial meniscus plays a fundamental role in knee stability, particularly in limiting anterior tibial translation. Although the biomechanical consequences of ramp lesions are unknown, longitudinal tears in the posterior horn of the medial meniscus increase anteroposterior tibial translation in the ACL-deficient knee [16]. The potential consequences of ramp lesions are threefold:
-
1.
Failure of the ACL graft:
Papageorgiou et al. [24] demonstrated the biomechanical interdependence between the medial meniscus and the ACL graft. When a medial meniscectomy is performed with an ACL reconstruction, the in situ forces in the ACL graft increase between 33 and 50 % [24] because of the loss of the secondary stabilising forces. Injury to the ACL increases forces in the meniscus by up to 100 % [11, 24]. Failure to recognise or treat a ramp lesion may lead to an increased risk of ACL graft failure.
-
2.
Increased risk of requiring further surgery to address meniscal injury:
If the diagnosis of ramp lesion is not made at the time of ACL reconstruction, secondary meniscal injury may occur in the form of extension of the tear. Extension of the lesion towards the middle third could easily destabilise the entire posterior meniscus or result in a bucket handle tear. This could potentiate in further surgery for meniscal repair, meniscal resection, or meniscectomy.
-
3.
Increased risk of developing osteoarthritis:
If neglected or misdiagnosed, ramp lesions can lead to instability or injury of the body of the medial meniscus which is a significant precursor to osteoarthritis and general debilitation of the knee. The literature reports that the risk of osteoarthritis in patients with an ACL and without a meniscal tear is between 0 and 13 %, but the risk increases to 21–48 % with meniscal tears. Thus, meniscal injuries that accompany ACL tears are important in the long-term prognosis, especially for OA after ACL reconstruction [4, 13, 25].
6.6 How Do You Diagnose a Ramp Lesion?
“The eyes only see what the mind is prepared to comprehend. Henri Bergson, French Philosopher”
-
(a)
History
Most commonly ramp lesions occur in the ACL-deficient knee. The clinician must therefore have a high index of suspicion for the pathology in the setting of ACL tear. Diagnosis is difficult acutely. The prevalence of ramp lesions increases in patients with a chronically deficient ACL, so one must be highly suspicious for their presence in this setting. In particular, one must enquire about the presence of medial joint line pain, which may point to a ‘hidden lesion’.
-
(b)
Clinical Evaluation
There are no specific clinical tests for ramp lesions. However, there are numerous clinical tests to examine for the presence of a meniscal lesion. A combination of various meniscal tests is recommended, because no single test is conclusive. Negative meniscal tests do not completely exclude a meniscal lesion. The accuracy rate of the tests ranges from 60 to 95 %, depending on the clinical experience of the examiner [12]. Physical examination in the setting of a tear of the posterior horn of the medial meniscus typically reveals posteromedial joint line tenderness and reproduction of posteromedial pain on maximal flexion of the knee [26].
Provocative manoeuvres may cause impingement of the meniscus between the femoral and tibial surfaces. The McMurray test is performed on the medial meniscus by flexing the knee, creating a varus stress by internally rotating the tibia and bringing the knee into full extension while palpating the joint line [26]. Other tests include the Steinmann I sign (tenderness shifting from anterior to posterior with increasing flexion) and the Fouche sign (reversed McMurray sign with internal rotation of the tibia) [12].
-
(c)
Radiological evaluation
Ramp lesions are difficult to diagnose radiologically. MRI, widely used in the evaluation of meniscal injuries, has a low sensitivity for identifying ramp tears. Meniscal lesions are more difficult to detect on MRI in the presence of ACL rupture, and MRI is less specific for medial meniscal tears than for lateral tears [27]. MRI is unreliable in diagnosing ramp tears, presumably because the knee is in near full extension at the time of study, reducing the meniscocapsular separation [9, 22]. It can also be difficult to distinguish meniscocapsular separation from far peripheral vertical longitudinal tears of the posterior horn of the medial meniscus. Hash reported that the most specific sign of a ramp lesion on MRI was the visualisation of a thin fluid signal completely interposed between the posterior horn of the medial meniscus and the posteromedial capsule (Fig. 6.2 – appearance of a ramp lesion on MRI) [28].
It is generally considered that arthroscopic evaluation is necessary to completely rule out or accurately diagnose a ramp lesion [9, 10, 21, 22, 28].
-
(d)
Arthroscopic Evaluation
Ramp lesions are frequently undiagnosed during ACL reconstructive surgery.
Given their high prevalence, they should be routinely looked for [2]. They may go unseen because of poor visualisation from standard anteromedial and anterolateral portals. Obstruction by the medial femoral condyle can make it difficult to visualise the posterior third of the medial meniscus [2]. Various methods have been described to improve visualisation of the posteromedial corner of the knee; however, there are many knees, the so-called tight knees, in which the posteromedial corner is impossible to evaluate via anterior portals only [2].
Sonnery-Cottet et al. [2] demonstrated that 40 % of ramp lesions are not identified without inspection of the posterior compartment via intercondylar view and posteromedial portal access. This is of particular importance, because many of these missed tears are repairable [2, 29].
Given the high prevalence of ramp lesions, some authors have suggested that a posteromedial portal should be used in all cases to enhance the visualisation of the posteromedial aspect of the medial meniscus [2]. Although this approach would certainly enhance diagnosis of the lesion, if it exists, there is still insufficient data to support an improved clinical outcome with repair of these lesions. Therefore, this suggestion remains somewhat controversial.
6.7 How Can I See a Ramp Lesion Arthroscopically?
A number of different arthroscopic techniques have been proposed to visualise ramp lesions properly. Key to any of these is accessing the posteromedial compartment for inspection.
Firstly, a thorough assessment of the knee should be made using standard anterolateral and anteromedial portals and a classic 30° arthroscope [9, 21, 30]. ACL rupture should be confirmed, followed by routine assessment of the posterior horn of the medial meniscus with the knee in extension and a valgus force applied. The meniscus should be inspected and probed to determine the presence of a tear and the stability of the meniscus [9, 29]. The ramp area should then be inspected and can be done so by two main approaches:
-
(a)
Intercondylar approach
Strobel [12] proposed the ramp area of the medial meniscus be inspected by passing the arthroscope through the intercondylar notch and under the posterior cruciate ligament (PCL) into the posteromedial recess. The knee should be flexed to 90° and a valgus stress applied. A 2.7 mm diameter 70° arthroscope may be used to obtain a wider view of the posteromedial compartment [30]; however, this may not be required [2]. The use of a blunt trocar may facilitate passing the camera [2]. Once the cannula has been passed into the compartment, the blunt trocar is exchanged for the 30° or 70° scope. The optical lens is rotated to allow good visualisation of the posteromedial compartment and especially the meniscocapsular junction. Internal rotation applied to the tibia can help visualisation because this causes the posterior tibial plateau to sublux leading to posterior translation of the middle third of the medial meniscus [31] (Fig. 6.3).
Position of the arthroscope (A) for the intercondylar view. The arthroscope is advanced between the medial femoral condyle (MC) and posterior cruciate ligament (PCL). The arthroscope is then rotated to view the posteromedial recess (arrows) (F, femur; T, tibia) [29]
Vision may be obscured by synovitis in the posteromedial recess or by osteophytes. If a ramp lesion is strongly suspected but cannot be confirmed or excluded by viewing via an anterolateral portal, inspection can be aided by needling. A needle is inserted into the posteromedial recess percutaneously to help evaluate the ramp area [9, 12]. With the knee in 90° of flexion and the use of transillumination, a needle is inserted from the posteromedial aspect of the knee, proximal to the medial femoral condyle. The needle is passed into the posterior part of the meniscal attachment or the posterior part of the tear. Moving the needle posteriorly will open up the tear and more clearly define its location and extent [12]. Once the presence of a ramp lesion has been confirmed, it should be repaired [9, 10, 12].
-
(b)
Posteromedial approach
Some authors advocate the use of a posteromedial portal [9, 12, 29]. Strobel advocates the use of a low posteromedial portal, placed at the level of the joint space, which provides relatively tangential access to the posterior horn and ramp area of the medial meniscus. This is the portal placement of choice for all-inside repairs [12]. A posteromedial portal is established under direct visualisation using a localising 18-gauge needle. Once the localising needle is in optimal position, a superficial incision is made through the skin only to decrease the risk of injury to the saphenous nerve and vein, and the portal is completed with the use of a straight artery forceps to penetrate the joint capsule and expand the portal. The established posteromedial portal can be used for both visualisation and as a working portal. The probe is first introduced through the posteromedial portal to manipulate the posterior horn of the meniscus. The arthroscope can then be inserted to view the posterior horn, with probing through the anterior portals [29]. It is also possible to create two posteromedial portals, one superiorly and one inferiorly, with an adequate skin bridge, to visualise and work exclusively posteromedially.
Sonnery-Cottet et al. [2] propose a four-step systematic arthroscopic exploration to ensure ramp lesions are not missed: (1) standard arthroscopic exploration via anterolateral portal and probing of the meniscal tissue, (2) exploration of the posteromedial compartment by introducing the arthroscope through the anterolateral portal and advancing it deeply into the notch and under the PCL, (3) creating a posteromedial portal and probing the posterior horn of the medial meniscus and (4) medial meniscal repair. In their study they found 42 % of ramp lesions at step 3. In true hidden lesions, the tears were not revealed until the area was evaluated with an arthroscopic probe, and superficial soft tissue was minimally debrided with a motorised shaver [2].
6.8 If I See a Ramp Lesion, How Should I Treat It?
No clear consensus exists on the appropriate management of ramp lesions [10]. Despite being in the red-red zone, an area with a rich vascular supply, questions have been raised on whether ramp lesions can heal without repair. Ahn et al. [32] showed that during knee flexion and extension, the hypermobility of the detached meniscocapsular structure disturbs the ramp area, preventing spontaneous healing. The rates of poor healing for medial meniscus remains high when nonoperative treatment is used, even though nonoperative treatment is reportedly more effective for lateral meniscus tears [33–35].
Studies have consistently demonstrated the improved healing capacity of the meniscus when associated with a concomitant ACL reconstruction, and conversely, multiple authors have demonstrated an increased failure rate of meniscal repairs in ACL-deficient knees [36].
When surgical repair is the treatment of choice, the anatomic location of a meniscal ramp lesion creates a surgical challenge. The posteromedial portal places the saphenous neurovascular bundle at risk [37]. Techniques that allow for direct visualisation of the posterior capsule to avoid iatrogenic injury to the saphenous nerve are recommended. While outside-in repairs can be useful for repairs of the anterior and middle thirds of the meniscus, this technique should be undertaken with caution in the setting of repair of the posterior horn of the medial meniscus [37, 38].
All-inside techniques and inside-out techniques have been shown to have success in treating ramp lesions [31]. The meniscus should be prepared for repair. The lesion is debrided with a meniscal rasp, and the edges of the tear trimmed with a shaver [31].
The major advantages of the inside-out meniscal repair technique are its versatility, ease of use, relatively short learning curve and reliability. Excellent healing rates have been widely reported in the literature [36, 39].
-
(a)
Inside-out technique
For an inside-out repair, a posteromedial approach is required. With the knee in flexion, an oblique vertical incision is made at the posteromedial border of the tibia just below the joint line [2]. The sartorius fascia is incised as proximal as possible while preserving the pes anserine tendons. An anatomic triangle is formed by the posteromedial joint capsule anteriorly, the medial gastrocnemius posteriorly and the direct arm of the semimembranosus inferiorly [40]. A retractor is placed in this interval to protect the posterior neurovascular structures during the repair procedure [40]. Zone-specific cannulas are used to place sutures into the medial meniscus from the anterolateral portal. Single or double lumen cannulas can be used depending on the surgeon’s preference [39]. Ten-inch flexible needles with preloaded non-absorbable or absorbable sutures are typically used. While applying a valgus force to the joint, the cannula is directed towards the tear. The tip of the needle is passed just beyond the end of the cannula to visualise its precise entry into the meniscus. The tear should be anatomically reduced, and the needle is passed through the meniscus. The second needle is then passed adjacent to the first in a horizontal, vertical or oblique mattress. The assistant retrieves the needles through the posteromedial incision, and the needles are cut from the sutures and clamped with a hemostat. The process is repeated every 3–5 mm. The sutures are tied with the knee at 90°, being careful not to overtighten the posteromedial structures [10, 39–41]. Inside-out repair offers a success rate of 60–80 % for isolated meniscal repairs and 85–90 % when performed at the time of ACL reconstruction [39].
-
(b)
All-inside technique
All-inside meniscal repairs are performed entirely through arthroscopic portals. This technique avoids the need for accessory incisions and decreases the risk of neurovascular injury. Various meniscal repair devices are available. They may be rigid or self-adjusting suture-based implants [38].
-
(i)
Suture hook: Morgan [42] described an all-inside suturing technique, which although technically demanding allows for placement of vertically oriented sutures [43]. The tear is repaired using a curved suture hook angled approximately 90° at the tip (angled to the right for the left knee, to the left for the right knee). The arthroscope is placed from the anterolateral portal into the posteromedial compartment through the intercondylar notch. A posteromedial portal is made and the tear is debrided to enhance healing [44]. The suture hook is passed through the meniscal peripheral rim tissue (meniscocapsular tissue first) from superior to inferior and then through the mobile central meniscal fragment from inferior to superior. This allows the sagging posterior tissues to be lifted to the level of the meniscal posterior horn [12]. It is postulated that this lifting manoeuvre is essential and cannot be replicated with the standard anterior-to-posterior all-inside technique [12, 29, 32]. A probe can be used to keep the central meniscal fragment in place [45]. The suture hook is advanced and rotated until the tip of the hook appears on the upper meniscal surface. The suture is advanced and retrieved with an arthroscopic grasper [12]. The suture is tied with an arthroscopic knot pusher. Sutures are placed every 5 mm along the length of the tear [2].
-
(ii)
Meniscal suture anchor: Proprietary meniscal suture devices can also be used for ramp lesion repair – the following description uses a FasT-Fix device (Smith & Nephew, Andover, MA, USA). With the arthroscope in the anterolateral portal, the device is advanced to the ramp lesion through the anteromedial portal. Using the intercondylar approach to gain direct vision of the posteromedial compartment, the first implant is inserted under the meniscus and obliquely into the joint capsule. The second implant is inserted into the peripheral edge of the meniscus. The pre-tied self-sliding knot is tensioned to achieve secure fixation. The curve of the FasT-Fix may be increased to allow for easier access below the meniscus and to avoid damage to the chondral surface of the femoral condyle. The knee may be flexed or extended while applying a valgus force to bring the capsular synovium as far as possible to the attachment. The anchors are inserted every 3–5 mm along the tear [30]. This technique does not use an accessory posteromedial portal, and one can postulate this may result in decreased accuracy of blind passage (Fig. 6.4).
(a–d) Arthroscopic view of posteromedial compartment of the left knee viewed through the intercondylar notch with a 70° arthroscope; (a) red arrow demonstrates the ramp lesion tear; (b) yellow arrow shows a curved suture hook used for an all-inside repair technique; (c) white arrow demonstrates a suture in situ with an arthroscopic knot; (d) the completed repair with approximation of the posteromedial capsule to the meniscus (These photographs are courtesy of Professor Joon Wang, Samsung Medical Centre, Sungkyunkwan University Medical School, Seoul, Korea)
Rates of structural healing and complications are comparable for inside-out and all-inside repair techniques. Complications are associated with both techniques. More nerve symptoms are associated with the inside-out repair, and more implant-related complications are associated with the all-inside technique [31, 32, 36].
All-inside repair using meniscal suture anchors has increased in popularity because of its easy application. Biomechanically, the horizontal sutures of these devices have inferior strength compared with vertical mattress sutures. Also, meniscal fixators cannot provide sufficient fixation strength at the repair site in the case of ramp lesions [44].
6.9 How Do I Rehabilitate Ramp Lesion Repairs?
Post-operative rehabilitation programmes following meniscus repairs are highly variable, and currently there is no general consensus [2, 9, 10, 30, 38]. There are a number of variables to consider including the range of motion and weight-bearing status. Most surgeons agree that early knee motion is beneficial. Prolonged immobilisation can lead to stiffness, atrophy and decreased collagen content and impaired healing of the meniscus repair site [38]. However, maximal knee flexion is associated with considerable anterior tibial translation and can increase the stresses within the posterior horn of the meniscus, especially with weight bearing. Weight bearing can help reduce and stabilise longitudinal meniscus tears. Therefore, weight bearing in full extension theoretically poses less risk to ramp lesion repairs and may aid healing [38].
At present there is no clinical evidence that there is any need to slow or modify the ACL rehabilitation protocol when there is an associated meniscal repair.
Rehabilitation after a ramp lesion repair should follow usual protocols for ACL reconstruction when performed in combination or a meniscal repair when done in isolation [5].
6.10 What Do I Tell My Patients About the Outcome of Ramp Lesion Repairs?
It is still unknown at present what the natural history of a ramp lesion is and whether it will heal spontaneously once the knee has been stabilised by an ACL reconstruction or whether suture repair is mandatory to prevent it from extending to a larger tear [9]. There are no reported outcomes studies for nonsurgical management of ramp tears. There are only a small number of outcome studies for the diagnosis and management of ramp lesions in the literature [10]. Repair of the peripheral meniscus in conjunction with ACL reconstruction has been reported to produce favourable meniscal healing; therefore, the ramp area has high healing capacity. A systematic review by Grant et al. [36] in 2012 looked at inside-out versus all-inside meniscal repair in isolated, peripheral longitudinal unstable meniscal tears. They found no clear benefit of one technique over the other with regard to structural healing or perioperative complications.
The integrity of the ACL is a critical factor that affects the overall success of a meniscal repair. Studies have consistently demonstrated the improved healing capacity of the meniscus when associated with a concomitant ACL reconstruction [36, 38]. It is hypothesised this is related to the biological augmentation of the repair from factors in the bone marrow released within the joint [46]. Conversely, multiple authors have demonstrated an increased failure rate of meniscal repairs in ACL-deficient knees [47].
Take-Home Message
Ramp lesions are longitudinal tears at the meniscocapsular junction of the posterior horn of the medial meniscus. They are commonly associated with the ACL-deficient knee, both in the acute and chronic setting, with their incidence increasing in time from injury. Ramp lesions are difficult to diagnose preoperatively, and one must have a high index of suspicion in the setting of a chronic ACL tear. The key to diagnosing ramp lesions is to thoroughly evaluate the medial meniscus during arthroscopy, particularly the posteromedial aspect. This can be achieved through intercondylar access or via a posteromedial portal. Ramp lesions may be hidden under a superficial layer of tissue, and so probing with a needle or debridement with a shaver may reveal the tear. Once diagnosed, meniscal ramp lesions should be repaired to reinstate the biomechanical stabilising force of the medial meniscus. Options for repair include all-inside or inside-out techniques. Rehabilitation should follow standard protocols for isolated meniscal repair or ACL reconstruction.
Key Points
Incidence | The presence of a ramp lesion must be considered in the setting of acute ACL rupture, and the index of suspicion should be high in a chronically ACL-deficient knee (>3 months) The prevalence of ramp lesions is significantly increased with time from injury The interval between ACL injury and surgery is an important predictor of secondary meniscal injury |
Significance | Ramp lesions appear to play a significant role in knee stability given the posterior horn of the medial meniscus is a secondary restraint to anterior tibial translation and external rotation Diagnosis is important because missed lesions contribute to meniscal instability and subsequent failure of the meniscus Failure to recognise or treat a ramp lesion may lead to an increased risk of ACL graft failure |
Diagnosis | Ramp lesions are difficult to diagnose preoperatively as there may be no specific findings on examination, and the sensitivity of MRI is low The posterior compartment of the knee must be inspected arthroscopically to accurately diagnose ramp lesions The posterior compartment of the knee may be examined by intercondylar access or additional posteromedial portal |
Management | Despite being in the vascular red-red zone, it is thought that ramp lesions may have low potential to heal spontaneously given the ramp area is likely to be disturbed during flexion and extension of the knee Therefore, repair of the meniscus should be performed Options for repair include inside-out and all-inside techniques Rates of structural healing and complications are comparable for inside-out and all-inside repair techniques. Complications are associated with both techniques. More nerve symptoms are associated with the inside-out repair, and more implant-related complications are associated with the all-inside technique |
Rehabilitation | Rehabilitation should follow standard guidelines for isolated meniscal repair or ACL reconstruction when performed in combination |
References
Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230–5.
Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42(4):921–6.
Keene GC, Bickerstaff D, Rae PJ, Paterson RS. The natural history of meniscal tears in anterior cruciate ligament insufficiency. Am J Sports Med. 1993;21(5):672–9.
Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW, et al. Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39(9):1889–93.
Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM. A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med. 2013;41(8):1801–7.
Smith 3rd JP, Barrett GR. Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am J Sports Med. 2001;29(4):415–9.
Noyes FR, Chen RC, Barber-Westin SD, Potter HG. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med. 2011;39(5):1008–17.
Strobel MJ. Menisci. In: Fett HM, editor. Manual of arthroscopic surgery. New York: Springer; 1998. p. 171–8.
Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39(4):832–7.
Chahla J, Dean CS, Moatshe G, Mitchell JJ, Cram TR, Yacuzzi C, et al. Meniscal ramp lesions: anatomy, incidence, diagnosis, and treatment. Orthop J Sports Med. 2016;4(7):2325967116657815.
Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2967–73.
Strobel MJ. Manual of arthroscopic surgery. Berlin Heidelberg: Springer; 2002. p. 171–8.
Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40(10):2342–7.
Rath E, Richmond JC. The menisci: basic science and advances in treatment. Br J Sports Med. 2000;34(4):252–7.
Englund M. Meniscal tear – a feature of osteoarthritis. Acta Orthop Scand Suppl. 2004;75(312):1–45. backcover
Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH. Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med. 2011;39(10):2187–93.
Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res. 2000;18(1):109–15.
Thompson WO, Fu FH. The meniscus in the cruciate-deficient knee. Clin Sports Med. 1993;12(4):771–96.
Song GY, Liu X, Zhang H, Wang QQ, Zhang J, Li Y, et al. Increased medial meniscal slope is associated with greater risk of ramp lesion in noncontact anterior cruciate ligament injury. Am J Sports Med. 2016;44(8):2039–46.
Hughston J. Functional anatomy. injury and repair: knee ligaments. St Louis: Mosby-Year Book; 1993. p. 50–66.
Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44(2):400–8.
Bollen SR. Posteromedial meniscocapsular injury associated with rupture of the anterior cruciate ligament: a previously unrecognised association. J Bone Joint Surg Br. 2010;92(2):222–3.
Papastergiou SG, Koukoulias NE, Mikalef P, Ziogas E, Voulgaropoulos H. Meniscal tears in the ACL-deficient knee: correlation between meniscal tears and the timing of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2007;15(12):1438–44.
Papageorgiou CD, Gil JE, Kanamori A, Fenwick JA, Woo SL, Fu FH. The biomechanical interdependence between the anterior cruciate ligament replacement graft and the medial meniscus. Am J Sports Med. 2001;29(2):226–31.
Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–43.
Maak TG, Fabricant PD, Wickiewicz TL. Indications for meniscus repair. Clin Sports Med. 2012;31(1):1–14.
De Smet AA, Graf BK. Meniscal tears missed on MR imaging: relationship to meniscal tear patterns and anterior cruciate ligament tears. AJR Am J Roentgenol. 1994;162(4):905–11.
Hash TW, 2nd. Magnetic resonance imaging of the knee. Sports Health 2013;5(1):78-107.
Peltier A, Lording TD, Lustig S, Servien E, Maubisson L, Neyret P. Posteromedial meniscal tears may be missed during anterior cruciate ligament reconstruction. Arthroscopy. 2015;31(4):691–8.
Li WP, Chen Z, Song B, Yang R, Tan W. The fast-fix repair technique for ramp lesion of the medial meniscus. Knee Surg Relat Res. 2015;27(1):56–60.
Thaunat M, Jan N, Fayard JM, Kajetanek C, Murphy CG, Pupim B, et al. Repair of meniscal ramp lesions through a posteromedial portal during anterior cruciate ligament reconstruction: outcome study with a minimum 2-year follow-up. Arthroscopy. 2016;37(4):776–85.
Ahn JH, Wang JH, Yoo JC. Arthroscopic all-inside suture repair of medial meniscus lesion in anterior cruciate ligament – deficient knees: results of second-look arthroscopies in 39 cases. Arthroscopy. 2004;20(9):936–45.
Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17(4):396–401.
Yagishita K, Muneta T, Ogiuchi T, Sekiya I, Shinomiya K. Healing potential of meniscal tears without repair in knees with anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(8):1953–61.
Ahn JH, Lee YS, Yoo JC, Chang MJ, Koh KH, Kim MH. Clinical and second-look arthroscopic evaluation of repaired medial meniscus in anterior cruciate ligament-reconstructed knees. Am J Sports Med. 2010;38(3):472–7.
Grant JA, Wilde J, Miller BS, Bedi A. Comparison of inside-out and all-inside techniques for the repair of isolated meniscal tears: a systematic review. Am J Sports Med. 2012;40(2):459–68.
Rodeo SA. Arthroscopic meniscal repair with use of the outside-in technique. Instr Course Lect. 2000;49:195–206.
Bava ED, Barber FA. Meniscal repair with the newest fixators: which are best? Clin Sports Med. 2012;31(1):49–63.
Nelson CG, Bonner KF. Inside-out meniscus repair. Arthrosc Tech. 2013;2(4):e453–60.
Chahla J, Serra Cruz R, Cram TR, Dean CS, LaPrade RF. Inside-out meniscal repair: medial and lateral approach. Arthrosc Tech. 2016;5(1):e163–8.
Johnson D, Weiss WM. Meniscal repair using the inside-out suture technique. Clin Sports Med. 2012;31(1):15–31.
Morgan CD. The “all-inside” meniscus repair. Arthroscopy. 1991;7(1):120–5.
Rimmer MG, Nawana NS, Keene GC, Pearcy MJ. Failure strengths of different meniscal suturing techniques. Arthroscopy. 1995;11(2):146–50.
Choi NH, Kim TH, Victoroff BN. Comparison of arthroscopic medial meniscal suture repair techniques: inside-out versus all-inside repair. Am J Sports Med. 2009;37(11):2144–50.
Ahn JH, Kim SH, Yoo JC, Wang JH. All-inside suture technique using two posteromedial portals in a medial meniscus posterior horn tear. Arthroscopy. 2004;20(1):101–8.
Hutchinson ID, Moran CJ, Potter HG, Warren RF, Rodeo SA. Restoration of the meniscus: form and function. Am J Sports Med. 2014;42(4):987–98.
Duchman KR, Westermann RW, Spindler KP, Reinke EK, Huston LJ, Amendola A, et al. The fate of meniscus tears left in situ at the time of anterior cruciate ligament reconstruction: a 6-year follow-up study from the MOON cohort. Am J Sports Med. 2015;43(11):2688–95.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 ISAKOS
About this chapter
Cite this chapter
Young, R., Devitt, B.M., Whitehead, T. (2017). Meniscal Ramp Lesions: Diagnosis and Treatment Strategies. In: LaPrade, R., Arendt, E., Getgood, A., Faucett, S. (eds) The Menisci. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-53792-3_6
Download citation
DOI: https://doi.org/10.1007/978-3-662-53792-3_6
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-53791-6
Online ISBN: 978-3-662-53792-3
eBook Packages: MedicineMedicine (R0)