Abstract
Disc arthroplasty has opened a new era in spinal surgery and has gained a firm place in the operative portfolio of many surgeons. Many patients beyond the clinical trials were treated successfully with disc arthroplasty. As often in spinal surgery, proper patient selection is more important than selection of implant.
Looking to the future, surgeons must be aware of the interests of the manufacturers, which spent billions of dollars for disc arthroplasty technologies. Nevertheless, the lessons we have learned from the past 30 years should lead us to the development of better implants for our patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Arthroplasty
- Intervertebral disc
- Total disc replacement
- Prosthetic disc nucleus
- Degenerative disc disease
1 Introduction
While the first artificial disk was implanted just 30 years ago, the history of disk arthroplasty is already about 55 years old.
Arthroplasty has been quite successful for joints such as the hip and knee. In contrast, disk arthroplasty is far away from being the standard treatment in spine surgery. Degenerative lesions of the disk consist of a decrease in the hydrophilic properties of the nucleus as well as the appearance of annulus tears. Secondary, osteoarthritis of the facet joints and subchondral bone alterations occur. Thus, the entire functional spinal segment degenerates. While severe hip osteoarthritis can be treated with total hip replacement, successful replacement of a total spinal segment is still not possible.
In the past, surgeons attempted to develop arthroplasty-like implants in order to mimic physiologic motion. The primary purpose was to restore symptom-free biomechanical function. While there is almost no more indication to perform a hip or knee arthrodesis, it is still unclear if spinal arthrodesis will follow this pattern. Today, the increasing demands and expectations from the patients’ side, and the medical desire to avoid fusion with its adverse side effects, have led to the development of multiple implants for disk arthroplasty.
Over the average human lifespan, the spine is exposed to more than 100 million cycles of motion. Per year, the lumbar spine is exposed to 2 million nonsignificant motions and 125.000 significant bends per year. The optimal lifetime for an arthroplasty spinal implant was therefore considered to be approximately 30 million cycles, or 10 million cycles in a fully loaded spine situation [1, 2].
The intervertebral disk is not a simple cartilaginous joint, but rather a complex anatomic structure allowing small movements along and around three main axes. In contrast to peripheral joints, whose stability is mainly achieved by ligaments, the disk on its own provides the major part of its stability. The configuration of nucleus and annulus allows high resistance to external forces.
The biomechanical requirements present quite a challenge for any implanted mechanical device, since the most elastomeric polymers will degrade, metals will wear, each will be exposed to the immune system, and open spaces will lead to tissue ingrowth. Continuous motion and stress will lead to metal fatigue and potentially implant failure. Thus, the implants must be biocompatible and resistant to the stresses of the spine.
The development of disk prostheses was heavily influenced by design and engineering principles previously established for total joint arthroplasty. Strategies for immediate and delayed implant fixation have been taken from lessons learned with hip prostheses. The same is true for the use of cobalt chrome alloys and ultra-high-molecular-weight polyethylene in a majority of devices. Titanium provides excellent biocompatibility and the advantage of MRI compatibility. Knowledge transfer from joint arthroplasty to the spine certainly offers advantages. However, the disk space is a different biomechanical and biologic environment compared to other joints. To complicate matters, the origin of low back pain is not fully understood yet and appears to be more complex than in peripheral joints.
Two key principles can be differentiated for disk arthroplasty [3]:
-
1.
Reproduction of the viscoelastic properties of the disk. Those implants are mostly manufactured from various silicones or polymers. Some rely on springs and/or piston systems and some are injected in monomer form and polymerised in situ. The main field of application is nucleus replacement.
-
2.
Reproduction of the motion characteristics of the disk. Those implants are usually mechanical devices made from metal and/or polyethylene couples. The main field of application is total disk replacement.
Innumerable different designs for both principles have been developed and patented so far. However, only a few of them reached the level of clinical application, and even fewer were implanted in a bigger number of patients. The story began in Europe in the 1950s with preclinical studies and patents. While today the negative aspects of spinal fusion serve as a rationale for disk arthroplasty, the rationale in the last century was restoration of joint biomechanics.
In 1955, van Steenbrugghe patented a joint replacement for the disk consisting of two cushions [4]. In the late 1950s, Nachemson injected self-hardening liquid silicone rubber into cadaver disks [5].
However, the virtual clinical pioneer of disk arthroplasty was Fernström. He was the first to implant an “artificial disk” in the late 1950s. In fact, he was using a metal ball in an attempt to reproduce the “ball joint” mechanism of the disk [6].
The Fernström ball seems to have been used in about 250 patients. Because of poor results, the implant was withdrawn [7].
Probably the first attempt of a total disk replacement restoring the motion function was patented by Weber in 1978. The devices consisted of two polyethylene box-like structures anchored in the adjacent vertebrae. In between, a ceramic ovoid core was placed allowing motion. However, the device was never manufactured [8].
The modern history of disk arthroplasty began in the 1980s. Nucleus replacement strategies and total disk replacement were separated and both could reach clinical application in the subsequent course.
2 Nucleus Replacement
Nucleus replacement strategies reflect the earliest attempts to relieve pain and restore function of the degenerated spinal motion segment. The above-mentioned Fernström ball was one of the first replacements. All of those early techniques were neither mechanical nor biological promising.
The history of nucleus replacement suffered from many setbacks. Surgeons and engineers ingenuity lead to numerous devices. The majority of them were either tried and failed or were never tried clinically at all. The early designs were made of virtually any material (metal or polymer) having flexibility, especially elastomeric (rubbery) materials or metal springs and hinges. Literally all of the early designs were mechanical devices. Typical problems of most of the implants were: surgical implanting technique, attachment to the bone, resistance to expulsion, mechanical failure loads, longevity, and tissue compatibility. Despite those problems, nucleus replacements have been used since the late 1990s.
This is probably due to the tremendous efforts of Charles D. Ray, the inventor of the prosthetic disk nucleus (PDN) (Fig. 41.1). He followed the idea to compare the degenerated disk with a flat car tyre. The nucleus loses water and shrinks and consecutively the disk height decreases like a tube of a tyre which deflates. As long as the annulus (respectively, the tyre) maintains its integrity, a restoration of function is possible if the pressure in the disk (respectively, the tube) can be increased again. Coming from this point, he developed a hydrogel which could be hydrated. The first prosthetic disk was patented in 1988 [9].
Ray gave his prosthetic disk nucleus a scientific background. To date, the most often used nucleus replacement is the PDN and PDN-SOLO (Raymedica, Bloomington, USA). The PDN consists of a hydrogel core and an ultra-high-molecular-weight polyethylene jacket. The hydrogel core is a polyacrylonitrile-polyacrylamide multi-block copolymer with memory capability. It can absorb 50–90 % of its dry weight in water to become fully hydrated. The woven jackets provide dimensional control of the swollen pellets. Two PDN devices are usually implanted next to each other after removal of the nucleus [10].
Indications that have been proposed are low back pain due to degenerative disk disease, with or without leg pain [11].
While the theory of nucleus replacement with a swelling implant sounds auspicious, early clinical reports revealed high complication rates. Typical complications were implant dislocations and subsidence into the adjacent vertebral body [12, 13].
Obvious problems led to a new implant design, the PDN-SOLO®. Thus, complication rate dropped to less than 10 %, which is, in our opinion, still too high [14, 15]. Only few data concerning the long-term outcome are available showing persistent favourable clinical results. However, quality and quantity of data are too poor [16].
In the past, many other nucleus replacement strategies have been developed and are currently under investigation. Today, nucleus replacement devices can be functionally categorised as elastomeric and mechanical. The latter are in clinical use but are confronted with many of the same problems encountered with the PDN implant [17]. The surgical approach to the nucleus harms the integrity of the annulus. Thus, implanted nucleus devices can be extruded through the primary approach. The sewing of the annulus as well as lateral approaches to the disk did not eliminate this problem [18].
Elastomeric devices are under clinical investigation with encouraging preliminary results. Most of the actual strategies follow the path of injectable materials that undergo in situ polymerisation.
However, up to now, there is no evidence that nucleus replacement offers any clinical benefit. Furthermore, the indications are not clear yet.
In conclusion, further clinical investigation with prospective, randomised pivotal trials is needed to determine the efficacy of nucleus replacement in the treatment of lumbar degenerative disk disease [19, 20].
3 Total Disk Arthroplasty
The Charité artificial disk was the first available total disk replacement (TDR) system. Three different types have been developed so far. While type I and II Charité artificial disks were manufactured in the former German Democratic Republic (GDR) and, therefore, was never commercially available, the type III Charité disk was distributed by DePuy Spine (Raynham, Massachusetts, USA) until spring 2010.
The Charité type I was developed in East Berlin by Kurt Schellnack and Karin Büttner-Janz in the Charité Hospital in 1982. The idea was based on the biomechanically proven “low friction” principle, which had already been successful in total joint replacement. It consisted of two highly polished metal end plates with teeth for bony anchorage and an ultra-high-molecular-weight polyethylene (UHMWPE) sliding core. The device was intended to imitate the movement of the nucleus pulposus of the intervertebral disk within its annular containment. It is therefore considered to be an unconstrained type of total disk replacement. An unconstrained design incorporates a mobile-bearing core and provides independent rotation and translation about three axes. The so-called SB Charité Artificial Disk Mark I was implanted at the Charité Hospital in the years 1984–1985 [21, 22].
Due to axial plane migrations, the device was modified to the SB Charité II.
It was used between 1985 and 1987. In contrast to type I, end plates were enlarged and exhibited bilateral wings to avoid subsidence. Finally, problems of migration and metal fatigue fractures led to the abandonment of type II also [22].
From 1987 on, the Link SB Charité III was manufactured by Waldemar Link GmbH in Hamburg, West Germany. The end plates were changed to cobalt-chromium-molybdenum alloy (CoCrMo) and received a porous coating of plasma-sprayed titanium and calcium phosphate to enhance osteointegration. The free-floating biconvex sliding core is still made of ultra-high-molecular-weight polyethylene (UHMWPE), encased by a metal wire for radiological marking. Primary stability is achieved by press-fit implantation through the teeth on the end plate which anchor into the subchondral bone. Different sizes and angulations were developed later [21].
After being taken over by DePuy Spine (Johnson & Johnson) in 2003, the SB Charité III was called Charité artificial disk until its abandonment (Fig. 41.2).
One of the earliest and most comprehensive clinical review regarding the Charité III was published by LeMarie in 1997. After 51 months follow-up of 105 patients, he found 79 % excellent results and a return to work rate of 87 % [23].
The American Food and Drug Administration (FDA) approved the Charité artificial disk in October 2004, the first of its kind, for use in treating pain associated with degenerative disk disease (DDD). The device is intended to replace a diseased or damaged intervertebral disk at either the L4–L5 or L5–S1 level.
In a multicenter study, the artificial disk was performed in 205 patients who had been diagnosed with DDD and had failed to have their pain relieved after 6 months of nonsurgical therapy and compared them to 99 patients who received the control device (stand-alone BAK spinal fusion cage using bone graft).
The study showed that 2 years after surgery, patients treated with the artificial disk did no worse than patients treated with intervertebral body fusion. However, patient satisfaction was higher in the artificial disk group. The rates of adverse events from use of the artificial disk were similar to those from treatment with fusion. In addition, the study showed that there was no statistically significant relationship between motion at the level where the disk was implanted and the patient’s relief from pain [24, 25]. To conclude, the patients treated with the Charité artificial disk were as good as the patients treated with a stand-alone cage. However, the latter is considered to be an obsolete treatment in Europe due to unsatisfactory clinical results.
The SB Charité III has the longest clinical follow-up of any TDR. It has been implanted more than 17.000 times worldwide. Following the implantation, most of the authors stated 60–90 % satisfactory to excellent results [26–28].
Despite the good results published otherwise, Michael Putzier from the Charité Berlin published long-term results after an average follow-up of 17 years. The deflating results revealed spontaneous ankylosis in 60 % and a reoperation rate of 11 % [29].
Interestingly, the last Charité artificial disk was already implanted in the Charité hospital in Berlin in 1989. Despite the fact that the implant carried the name of the biggest university hospital in Germany, it has not been used there since then. In the USA, criticism increased over time, and numerous patients started to sue Johnson & Johnson alleging the pharmaceutical company knew or should have known about the serious complications of the artificial disk surgery. As mentioned above, the Charité artificial disk is not available anymore.
Another early type of artificial disk was the AcroFlex (DePuy Spine), designed by Arthur Steffee. The first implant type consisted of a hexen-based polyolefin rubber cushion attached to two titanium end plates. A pilot study with six patients was published in 1993. Due to concerns regarding potential carcinogenicity of parts of the implant, the clinical trials were suspended. The next generation was proposed by Steffee, Fraser and co-workers. Debris and implant failure were the typical problems of the AcroFlex series [30, 31]. A prospective non-randomised study with almost 10 years follow-up revealed a cumulative survival of only 61 %. The authors concluded that further use of this implant is not justified [32].
Two other types of TDR were developed in the 1990s and showed promising results: the ProDisc and the Maverick artificial disk.
The first ProDisc (Aesculap, Tuttlingen, Germany) was developed by Thierry Marnay in Montpellier in the late 1980s [33].
The ProDisc has two metal (titanium) end plates which are plasma sprayed with titanium and have two vertical fins for fixation to the end plates. The core is made of high-density polyethylene and fits firmly to the inferior end plate. The superior surface of the core is formed convex. The resulting centre of rotation is fixed and located inferior to the disk space. This semiconstrained design includes a fixed axis of rotation that limits translation. This leads to increased stress within the device and at the device-bone interface, resulting in a potentially increased risk of implant loosening.
The first series of 64 patients were operated by Marnay between 1990 and 1993 with promising results. Follow-up ranged between 7 and 11 years with over 75 % excellent or good results. There was no outcome difference between 1 and 2 level implantations. All implants were still intact and functioning without signs of subsidence or migration [34].
The second generation of the ProDisc called ProDisc-L (Fig. 41.3) is distributed by Synthes (Paoli, Pennsylvania, USA). It was introduced to the market in 2000. Different end plate sizes and lordosis angles, different core heights and only one keel per end plate were the main design changes. It has been approved by the American FDA in August 2006 for one- or two-level implantation. The FDA IDE trial compared the ProDisc II with an anteroposterior fusion using femoral ring allografts anteriorly and pedicle screw fixation with autograft posteriorly. The clinical results in the ProDisc group were slightly better than in the fusion group [35].
In uncontrolled clinical series, success rates up to 90 % are reported [27, 36]. Long-term data are sparse. In a prospective, single-centre investigation, 181 patients (90 % follow-up rate) could be examined after a mean follow-up of 7.4 years. Clinical results improved significantly after surgery and 87 % of patients were (highly) satisfied at final follow-up. Complication rate was 14 %, about half of which were device related. Reoperation rate was 16 %. The authors concluded that for a carefully selected cohort of patients, results compare favourably to results achieved with fusion [37]. Similar mid- to long-term results have been published by other authors [38–40].
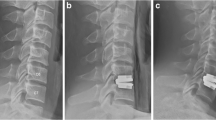
Mathews, Le Huec and co-workers conceived the semiconstrained Maverick artificial disk (Fig. 41.4) (Medtronic Sofamor Danek, Memphis, Tennessee, USA), a metal-on-metal (chrome cobalt) interface implant with a posterior rotation axis [41].
Metal-on-metal disk prostheses have been developed to eliminate polyethylene wear and its potential risks. Although polyethylene debris and osteolysis have not been proven to be significant clinical issues with TDR, the long-term effects remain unclear. As known from hip surgery, metal-on-metal surfaces produce far lesser debris than polyethylene-on-metal surfaces [27].
The Maverick artificial disk is fixated to the end plates with a midline sagittal fin like the ProDisc. The end plates are hydroxyapatite coated. The overall biomechanical profile is similar to the ProDisc. However, the convex caudal component has a slightly smaller radius of curvature compared with the concave superior component.
Like in the other TDR, different sizes, heights and angles are available.
The first implantation was performed in 2002 and a randomised FDA clinical trial was begun in 2003, comparing the Maverick artificial disk to a fusion using cage combined with BMP. LeHuec and co-workers published a prospective study reporting the outcome of 64 Maverick devices implanted between January 2002 and November 2003. The Oswestry score improved for 75 % of patients [42]. Published midterm data 4 years after surgery showed 85 % of patients were again working and 79 % took up their normal sports activities [43].
In the last 6 years, a variety of new implants and techniques have been developed so that nowadays nearly all companies offer implants for disk arthroplasty. Despite extensive biomechanical studies, it currently remains unclear which type of constraint offers the most advantages in total disk replacement. Constrained implants offer stability but lead to high stress on fixation, while unconstrained implants are sensitive to surgical positioning. The normal axis of rotation of the lumbar spine is not fixed but varies. Although a constrained device in good position may provide more controlled motion and consecutive preservation of the facet joints, an unconstrained device may provide greater range of motion and be more forgiving in terms of surgical positioning.
In the recent past, results from multicenter and prospective randomised studies without any potential conflict of interest have been published. Data from 240 patients from a Swiss registry including different types of TDR showed significant, clinically relevant and lasting reduction of pain until 5 years after surgery. Adjacent segment degeneration occurred in 10 % of patients. Revision rate was 4.4 %. Almost 87 % of operated segments remained mobile despite the fact that heterotopic ossifications could be detected in 44 % of patients [44].
In a Swedish prospective randomised controlled trial, 152 patients were either fused posteriorly or received TDR of different types. After 5 years, both groups still showed significant clinical benefit from surgery. However, all parameters were significantly better in the TDR group. No differences were found concerning complications and reoperations [45].
In a recent meta-analysis looking at results after 2-year follow-up, seven relevant RCTs with a total of 1,584 patients could be included. TDR was significantly more effective in ODI, VAS score, shorter duration of hospitalisation and a greater proportion of willing to choose the same operation again. All other parameters showed no significant difference [46].
Nevertheless, the authors of a Cochrane review judged the results slightly different: “Although statistically significant, the differences in clinical improvement were not beyond generally accepted boundaries for clinical relevance. Prevention of adjacent level disease and/or facet joint degeneration was not properly assessed. Therefore, because we think that harm and complications may occur after some years, the spine surgery community should be prudent to adopt this technology on a large scale, despite the fact that total disk replacement seems to be effective in treating low back pain in selected patients, and in the short term is at least equivalent to fusion surgery” [47].
Complications have been reported with all types of TDR and can be divided into two groups: those related to the surgical approach and those related to the prosthesis.
Access to the anterior lumbar spine includes potential injury to major vascular and visceral structures. Total complication rates range from 10 % to 23 %. Complications related directly to device implantation occur in 2.9–6.5 % of patients [26, 37, 44, 46].
Implant-related complications are design specific and appear as subsidence, dislocation and breakage of the prosthesis. Overall complication rates range from 2 % to 26 % of patients [26, 27, 37, 46, 48].
4 Conclusion
Thirty years of clinical application has not revealed a clear advantage of disk arthroplasty over fusion techniques. Even the prospective randomised FDA studies are arguable since the methods used in the control groups are considered to be arguably substandard treatment in some parts of the world. Conflicting results, increasing number of lawsuits and inconsistent demeanour of companies have lead to an increasing mistrust of both surgeons and patients in TDR. During the last decade, in the USA, surgical treatment for lumbar DDD has increased 2.4-fold. Although all fusion procedures significantly increased, TDR did not increase [49].
Therefore, some authors still consider total disk replacement as an experimental procedure [50].
On the other hand, much knowledge has been gained on TDR, and extensive database exist from numerous randomised and non-randomised studies. The results are as good as with fusion. Complications and reoperations are similar with both techniques. Disk arthroplasty has opened a new era in spinal surgery and has gained a firm place in the operative portfolio of many surgeons. Many patients beyond the clinical trials were treated successfully with disk arthroplasty. As often in spinal surgery, proper patient selection is more important than selection of implant.
Looking to the future, surgeons must be aware of the interests of the manufacturers, which spent billions of dollars for disk arthroplasty technologies. Nevertheless, the lessons we have learned from the past 30 years should lead us to the development of better implants for our patients.
References
White AA, Panjabi MM. The basic kinematic of the lumbar spine. Spine. 1978;3:12–20.
Hedman TP, Kostuik JP, Fernie GR, Hellier WG. Design of an intervertebral disk prosthesis. Spine. 1991;16(6 Suppl):S256–60.
Szpalski M, Gunzburg M, Mayer M. Spine arthroplasty: a historical review. Eur Spine J. 2002;11 Suppl 2:S65–84.
Van Steenbrugghe MH. Perfectionnements aux prothèses articulaires. French Patent 1.122.634, 28 May 1956
Nachemson A. Some mechanical properties of the lumbar intervertebral disc. Bull Hosp Joint Dis. 1962;23:130–2.
Fernström U. Arthroplasty with intercorporal endoprosthesis in herniated disc and in painful disc. Acta Orthop Scand. 1966;10(Suppl):287–9.
Fernström U. Der Bandscheibenersatz mit Erhaltung der Beweglichkeit. In: Herdman H, editor. Zukunftaufgaben für die Erforschung und Behandlung von Wirbelsäulenleiden. Die Wirbelsäule in Forschung und Praxis. Stuttgart: Hippokrates; 1972.
Weber G. Zwischenwirbel Prothese. Swiss Patent 624573, February 1, 1978
Ray CD, CorbinT. Prosthetic disc and method of implanting. US Patent 4,772,287; 20 Sept 1988
Ray CD. The Raymedica prosthetic disc nucleus. an update. In: Kaech DL, Jinkins JR, editors. Spinal restabilization procedures. New York: Elsevier Science B.V; 2002. p. 273–82.
Klara PM, Ray CD. Artificial nucleus replacement. Clinical experience. Spine. 2002;12:1374–7.
Schönmayr R, Busch C, Lotz C, Lotz-Metz G. Prosthetic disc nucleus implants: the Wiesbaden feasibility study. 2 years follow-up in ten patients. Riv Neuroradiol. 1999;12:S163–70.
Shim CS, Lee SH, Park CW, Choi WC, Choi G, Choi WG, Lim SR, Lee HY. Partial disc replacement with the PDN prosthetic disc nucleus device. J Spinal Disord Tech. 2003;16:324–30.
Bertagnoli R, Karg A, Voigt S. Lumbar partial disc replacement. Orthop Clin N Am. 2005;36:341–7.
Schnake KJ, Weigert F, Kandziora F, Haas NP. Local vertebral body destruction after migration of a nucleus replacement. Z Orthop Unfall. 2007;145:649–51.
Selviaridis P, Foroglou N, Tsitlakidis A, Hatzisotiriou A, Magras I, Patsalas I. Long-term outcome after implantation of prosthetic disc nucleus device (PDN) in lumbar disc disease. Hippokratia. 2010;14(3):176–84.
Balsano M, Zachos A, Ruggiu A, Barca F, Tranquilli-Leali P, Doria C. Nucleus disc arthroplasty with the NUBAC™ device: 2-year clinical experience. Eur Spine J. 2011;20 Suppl 1:S36–40.
Bertagnoli R, Vazquez RJ. The Anterolateral TransPsoaticApproach (ALPA): a new technique for implanting prosthetic disc-nucleus devices. J Spinal Disord Tech. 2003;36:398–404.
Di Martino A, Vaccaro AJ, Lee JY, Denaro V, Lim MR. Nucleus pulposus replacement: basic science and indications for clinical use. Spine. 2005;30:S16–22.
Coric D, Mummaneni PV. Nucleus replacement technologies. J Neurosurg Spine. 2008;8:115–20.
Link HD. History, design and biomechanics of the LINK SB Charité artificial disc. Eur Spine J. 2002;11 Suppl 2:S98–105.
Büttner-Janz K, Schnellnack K, Zippel H. Eine alternative Behandlungsstrategie beim lumbalen Bandscheibenschaden mit der Bandscheibenendoprothese Modulartyp SB Charité. Z Orthop. 1987;125:1–6.
LeMaire JP, Skalli W, Lavaste F, Templier A, Mendes F, Diop A, Sauty V, Laloux E. Intervertebral disc prosthesis. Results and prospects for the year 2000. Clin Orthop Res. 1997;337:64–76.
Blumenthal S, McAfee PC, Guyer RD, Hochschuler SH, Geisler FH, Holt RT, Garcia Jr R, Regan JJ, Ohnmeiss DD. A prospective, randomized, multicenter Food and Drug Administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine. 2005;30:1565–75.
McAfee PC, Cunningham B, Holsapple G, Adams K, Blumenthal S, Guyer RD, Dmietriev A, Maxwell JH, Regan JJ, Isaza J. Prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part II: evaluation of radiographic outcomes and correlation of surgical technique accuracy with clinical outcomes. Spine. 2005;30:1576–83.
Petersilge CA. Lumbar disc replacement. Semin Musculoskelet Radiol. 2006;10:22–9.
Mayer HM. Total lumbar disc replacement. J Bone Joint Surg Brit. 2005;87:1029–37.
Guyer RD, McAfee PC, Banco RJ, Bitan FD, Cappuccino A, Geisler FH, Hochschuler SH, Holt RT, Jenis LG, Majd ME, Regan JJ, Tromanhauser SG, Wong DC, Blumenthal SL. Prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: five-year follow-up. Spine J. 2009;9(5):374–86. doi: 10.1016/j.spinee.2008.08.007. Epub 2008 Sep 19.
Putzier M, Funk JF, Schneider SV, Gross C, Tothz SW, Khodadadyan-Klostermann C, Perka C, Kandziora F. Charité total disc replacement – clinical and radiographical results after an average follow-up of 17 years. Eur Spine J. 2006;15:183–95.
Steffee AD. The Steffee artificial disc. In: Weinstein JN, editor. Clinical efficacy and outcome in the diagnosis and treatment of low back pain. New York: Raven; 1992.
Fraser RD, Ross ER, Lowery GL, Steffee AD. Spinal disc, United States Patent 6139579, 31 Oct 2000
Meir AR, Freeman BJ, Fraser RD, Fowler SM. Ten-year survival and clinical outcome of the AcroFlex lumbar disc replacement for the treatment of symptomatic disc degeneration. Spine J. 2013;13(1):13–21.
Marnay T. Prosthesis for intervertebral discs and instruments for implanting it. United States Patent 5314477, 24 May 1994
Marnay T. The ProDisc™: clinical analysis of an intervertebral disc implant. In: Kaech DL, Jinkins JR, editors. Spinal restabilization procedures. New York: Elsevier Science B.V; 2002. p. 317–31.
Zigler J, Delamarter R, Spivak JM, Linovitz RJ, Danielson 3rd GO, Haider TT, Cammisa F, Zuchermann J, Balderston R, Kitchel S, Foley K, Watkins R, Bradford D, Yue J, Yuan H, Herkowitz H, Geiger D, Bendo J, Peppers T, Sachs B, Girardi F, Kropf M, Goldstein J. Results of the prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine. 2007;32:1155–62.
Bertagnoli R, Yue JJ, Shah RV, Nanieva R, Pfeiffer F, Fenk-Mayer A, Kershaw T, Husted DS. The treatment of disabling multilevel lumbar discogenic low back pain with total disc arthroplasty utilizing the ProDisc prosthesis: a prospective study with 2-year minimum follow-up. Spine. 2005;30:2192–9.
Siepe CJ, Heider F, Wiechert K, Hitzl W, Ishak B, Mayer MM. Mid- to long-term results of total lumbar disc replacement: a prospective analysis with 5- to 10-year follow-up. Spine J. 2014;14(8):1417–31.
Zigler JE, Delamarter RB. Five-year results of the prospective, randomized, multicenter, Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential arthrodesis for the treatment of single-level degenerative disc disease. J Neurosurg Spine. 2012;17(6):493–501.
Park CK, Ryu KS, Lee KY, Lee HJ. Clinical outcome of lumbar total disc replacement using ProDisc-L in degenerative disc disease: minimum 5-year follow-up results at a single institute. Spine. 2012;37:672–7.
Tropiano P, Huang RC, Girardi FP, Cammisa Jr FP, Marnay T. Lumbar total disc replacement. Seven to eleven-year follow-up. J Bone Joint Surg Am. 2005;87-A:490–6.
Mathews H, Le Huec JC, Bertagnoli R, Friesem T, Eisermann L. Design rationale and early multicenter evaluation of Maverick total disk arthroplasty. International meeting on Advanced Spine Technologies, 2002, Montreux
Le Huec JC, Mathews H, Basso Y, Aunoble S, Hoste D, Bley B, Friesem T. Clinical results of Maverick lumbar total disc replacement: two-year prospective follow-up. Orthop Clin North Am. 2005;36:315–22.
Van de Kelft E, Verguts L. Clinical outcome of monosegmental total disc replacement for lumbar disc disease with ball-and-socket prosthesis (Maverick): prospective study with four-year follow-up. World Neurosurg. 2012;78(3–4):355–63.
Aghayev E, Bärlocher C, Sgier F, Hasdemir M, Steinsiepe KF, Wernli F, Porchet F, Hausmann O, Ramadan A, Maestretti G, Ebeling U, Neukamp M, Röder C. Five-year results of lumbar disc prostheses in the SWISSspine registry. Eur Spine J. 2014;23:2114–26.
Sköld C, Tropp H, Berg S. Five-year follow-up of total disc replacement compared to fusion: a randomized controlled trial. Eur Spine J. 2013;22(10):2288–95.
Rao MJ, Cao SS. Artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg. 2014;134(2):149–58.
Jacobs WC, van der Gaag NA, Kruyt MC, Tuschel A, de Kleuver M, Peul WC, Verbout AJ, Oner FC. Total disc replacement for chronic discogenic low back pain: a Cochrane review. Spine (Phila Pa 1976). 2013;38(1):24–36.
Cinotti G, David T, Postacchini F. Results of disc prosthesis after a minimum follow-up period of 2 years. Spine. 1996;21:995–1000.
Yoshihara H, Yoneoka D. National trends in the surgical treatment for lumbar degenerative disc disease: US, 2000–2009. Spine J. 2014. pii: S1529-9430(14)01544-7. doi: 10.1016/j.spinee.2014.09.026. [Epub ahead of print].
De Kleuver M, Oner FC, Jacobs WCH. Total disc replacement for chronic low back pain: background and a systematic review of the literature. Eur Spine J. 2003;12:108–16.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Schnake, K.J., Kandziora, F. (2016). Disk Arthroplasty: A 30-Year History. In: Pinheiro-Franco, J., Vaccaro, A., Benzel, E., Mayer, H. (eds) Advanced Concepts in Lumbar Degenerative Disk Disease. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-47756-4_41
Download citation
DOI: https://doi.org/10.1007/978-3-662-47756-4_41
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-47755-7
Online ISBN: 978-3-662-47756-4
eBook Packages: MedicineMedicine (R0)