Abstract
Remnant gastric cancer is a type of complicated gastric cancer. Although no consensus definition has been established to date, the most popular definition of remnant gastric cancer is a cancer in the remaining stomach at least 5 years after gastrectomy, regardless of the reason for the primary surgery (i.e., whether it was for benign or malignant disease). In the 1970s and 1980s, gastrectomy was frequently performed for complicated peptic ulcer disease, and most instances of remnant gastric cancer were located in the stomach remaining after surgery for this benign disorder. Nowadays, gastrectomy for benign disease has become less frequent because of the development of effective medical treatment for peptic ulcer disease, which has led to a decrease in the frequency of remnant gastric cancer after surgery for benign disease. By contrast, nationwide mass screening for gastric cancer has increased the proportion of early gastric cancers detected in Korea and Japan, and treatment strategies for gastric cancer have improved, leading to longer survival of patients with gastric cancer. Unlike gastric cancers in Western countries, which generally occur in the upper third of the stomach, 60–70% of gastric cancers in Korea and Japan occur in the distal stomach and are usually treated by distal gastrectomy. Consequently, the incidence of remnant gastric cancer is expected to increase, especially in East Asia.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Introduction
Remnant gastric cancer is a type of complicated gastric cancer. Although no consensus definition has been established to date, the most popular definition of remnant gastric cancer is a cancer in the remaining stomach at least 5 years after gastrectomy, regardless of the reason for the primary surgery (i.e., whether it was for benign or malignant disease). In the 1970s and 1980s, gastrectomy was frequently performed for complicated peptic ulcer disease, and most instances of remnant gastric cancer were located in the stomach remaining after surgery for this benign disorder. Nowadays, gastrectomy for benign disease has become less frequent because of the development of effective medical treatment for peptic ulcer disease, which has led to a decrease in the frequency of remnant gastric cancer after surgery for benign disease. By contrast, nationwide mass screening for gastric cancer has increased the proportion of early gastric cancers detected in Korea and Japan, and treatment strategies for gastric cancer have improved, leading to longer survival of patients with gastric cancer. Unlike gastric cancers in Western countries, which generally occur in the upper third of the stomach, 60–70% of gastric cancers in Korea and Japan occur in the distal stomach and are usually treated by distal gastrectomy. Consequently, the incidence of remnant gastric cancer is expected to increase, especially in East Asia.
Despite the clinical importance of remnant gastric cancer, the molecular carcinogenesis and clinical features of this cancer have not been well characterized; consequently, optimal treatment strategies for remnant gastric cancer have not been established. Reasons for the lack of clinical knowledge about this disease may include its low incidence (follow-up after gastrectomy has demonstrated remnant gastric cancer incidence rates of 1–3% [1,2,3]) and the use of variable definitions of remnant gastric cancer in the available studies (which is especially apparent as we are now in a transition period, with the incidence after surgery for benign disease decreasing and the incidence after surgery for cancer increasing).
Because of the paucity of information regarding treatment options for remnant gastric cancer per se, clinical practice has generally been based on knowledge about primary gastric cancer, especially in terms of staging of the disease [4], extent of surgical resection, and chemotherapy regimens. The available knowledge about remnant gastric cancer, derived from retrospective studies at large-volume hospitals and multiple centers, suggests that the prognosis of this cancer is comparable to that of primary gastric cancer. However, this does not mean that the treatment of remnant gastric cancer does not need to be distinguished from that of primary gastric cancer because the lymphatic structure and molecular carcinogenesis of the two types of cancer could differ [5].
Detailed discussions of the molecular mechanisms of, and perioperative chemotherapy and radiotherapy for, remnant gastric cancer are beyond the scope of the current section. In this chapter, we introduce the clinicopathologic characteristics of remnant gastric cancer and the expected patterns of lymphatic metastases according to the type of previous reconstruction. In addition, we briefly introduce the possibility of endoscopic treatment and minimally invasive surgery (laparoscopic or robotic surgery) for remnant gastric cancer. Finally, the issues surrounding, and the detailed procedures of, gastrectomy and lymph node dissection for remnant gastrectomy will be addressed and related to treatment outcomes of remnant gastric cancer.
Clinicopathologic Characteristics of Remnant Gastric Cancer
Remnant gastric cancer has an incidence of 1–3% and is much more common in males than females (the male/female ratio is 3–5:1). The time interval between primary gastrectomy and the diagnosis of remnant gastric cancer depends on the reason for the initial surgery: the interval is generally shorter after surgery for malignant disease (approximately 10 years) than after gastrectomy for benign disease (approximately 30 years). In addition, remnant gastric cancer is more frequent after gastrojejunostomy than after gastroduodenostomy. Chronic inflammation due to bile reflux is one of the putative mechanisms responsible for the development of remnant gastric cancer, whereas the etiology of other remnant gastric cancers may be similar to that of primary gastric cancer.
Lymph Node Metastases in Remnant Gastric Cancer
Lymphatic flow around the remnant stomach is changed because of the altered anatomy caused by the previous surgery; lymphatic drainage of the remnant stomach after gastroduodenostomy is different from that after gastrojejunostomy. In addition, lymphatic drainage is also affected by the reason for the initial surgery because a more extended lymph node dissection would have been performed for malignant disease, whereas a more limited or no lymph node dissection would have been performed for benign disease. Therefore, the surgical approach should be distinguished according to the type of reconstruction and reason for the initial surgery.
After gastroduodenostomy, cancer in the remnant stomach can spread to the hepatoduodenal ligament, superior mesenteric vein, splenic vessels, and short gastric vessels (Fig. 22.1). After gastrojejunostomy, the lymphatic flow is similar to that observed gastroduodenostomy, so the cancer can spread through the splenic and short gastric vessels. However, lymphatic flow differs after gastrojejunostomy in that metastases can also spread to the mesentery of the jejunum through the anastomosis site (Fig. 22.2). Of course, when the right gastroepiploic, right gastric, and left gastric vessels are retained after the previous surgery (mainly after surgery for benign disease), cancer in the remnant stomach can spread through the lymphatics around these remaining vessels as well. Thus, although there is no definition of D2 for remnant stomach cancer, all D2 lymph nodes for primary gastric cancer should be removed. Furthermore, because lymphatics around the splenic vessels are the main lymphatic flow of the remnant stomach, lymph node dissection in this area should be performed meticulously. Routine splenectomy for lymph node dissection around the splenic vessels is not recommended, which is similar to the situation for primary gastric cancer in the upper third of the stomach; however, complete removal of lymph nodes is a prerequisite for spleen-preserving completion total gastrectomy for remnant gastric cancer.
Minimally Invasive Treatment for Remnant Gastric Cancer
Endoscopic Treatment
Endoscopic resection of gastric cancer, such as by endoscopic mucosal resection and endoscopic submucosal dissection, has become widely used to treat primary gastric cancer in the very early stages. The absence of lymph node metastases is a prerequisite for endoscopic resection of gastric cancer because the procedure only involves removal of the primary cancer, without any lymph node dissection. Selection of which patients can be candidates for this treatment was based on a large-scale review of pathologic results from surgical specimens. Gotoda et al. reviewed the pathologic results of 5265 patients who underwent gastrectomy with lymph node dissection for early gastric cancer and developed a stratification system regarding the risk of lymph node metastasis [6]. Based on these results, patients with a very low risk of lymph node metastases have been treated with endoscopic resection. It is not yet clear whether endoscopic resection is feasible or efficacious for remnant gastric cancer, however, because of the limited number of cases of this type of tumor. In addition, endoscopic resection would be technically challenging because of the narrow space and fibrotic changes around the stapled anastomosis site. Despite these difficulties, recent studies have shown that endoscopic resection for remnant gastric cancer is feasible [7,8,9,10,11,12], and it has been suggested that the same indications for endoscopic resection of primary gastric cancer might be applied to remnant gastric cancer as well [13]. Considering the high degree of difficulty performing completion total gastrectomy for remnant gastric cancer because of fibrosis, adhesions, and changed anatomy, endoscopic resection could be a reasonable treatment option for remnant gastric cancer with a very low risk of lymph node metastases, especially in patients with severe comorbidities.
Laparoscopic and Robotic Surgery
Surgery for remnant gastric cancer is technically challenging because of fibrosis, adhesions, and altered anatomy caused by previous surgery. Thus, minimally invasive surgery (such as laparoscopic or robotic surgery) for remnant gastric cancer is difficult to perform, and substantial surgical skills and experience, as well as a comprehensive understanding of the anatomy, are required to perform this procedure. Some surgeons with advanced laparoscopic skills have attempted this seemingly impossible surgery and reported it to be feasible and possible to perform safely, with morbidity and mortality rates comparable to those of open surgery [14,15,16,17,18]. When surgeons try to perform completion total gastrectomy by laparoscopic or robotic methods, there should be no hesitation to convert to open surgery if a problem arises. Detailed results and surgical techniques for minimally invasive surgery of remnant gastric cancer are addressed in another chapter.
Open Surgery for Remnant Gastric Cancer
Difficulties with performing completion total gastrectomy for remnant gastric cancer arise from two distinct characteristics of remnant gastric cancer: (1) the presence of adhesions and fibrosis caused by the previous surgery and (2) changes in the lymphatic drainage. It is generally agreed that there will be more adhesions and fibrosis when the previous surgery was for cancer rather than for benign disease. There will be adhesions around the remnant stomach extending to the wound, other peritoneal surfaces, small bowel, colon, and liver, but the most critical region for completion total gastrectomy will be the supra-pancreatic area. Especially when the reason for previous surgery was cancer, lymph nodes around the celiac axis would have been dissected, which in turn produces more adhesions and fibrosis in the supra-pancreatic area. Consequently, surgeons should be very careful to avoid injuring major vessels, such as the common hepatic artery, portal vein, splenic artery and vein, and even the aorta and inferior vena cava. Dissecting the lymph nodes from the patient’s left to right side rather than right to left side may help identify the appropriate anatomical plane because the anatomy of the left side (around the splenic hilum) may not be affected by the previous surgery. The right gastroepiploic and right gastric vessels would usually have been ligated during the prior surgery, but the left gastroepiploic and left gastric vessels would rarely have been ligated when the reason for previous gastrectomy was benign disease. Although the right gastroepiploic and right gastric vessels would have already been ligated by the previous surgery, careful lymph node dissection around #5 and #6 would be required if the previous surgery was for benign disease. Lymph nodes around the superior mesenteric vein (#14v) are not included in the current D2 lymph node dissection for primary gastric cancer, but if this node remains and the tumor in the remnant stomach is located near the gastroduodenostomy site, dissecting #14v would be helpful for accurate staging and prognosis determination.
After careful dissection between the abdominal wall and intestines, the anatomy around remnant stomach should be identified through adhesiolysis. When the greater omentum remains, total omentectomy is performed in the same manner as during primary gastric cancer surgery. Usually adhesions exist between the liver and the ventral side of the stomach, and gentle dissection of the plane between the liver surface and gastric wall is required. When the tumor is located on the anterior side of the stomach, the surgeon should be careful not to injure the gastric wall during the dissection.
When the previous surgery involved a gastroduodenostomy, the duodenum is transected by stapling, after fully identifying the borders of the duodenum, stomach, and pancreas. Sometimes the gastroduodenostomy was performed by stapling during the previous surgery and is close to the head of the pancreas; if so, resecting the duodenum by stapling will be difficult. In this situation, the duodenum can be transected by a scalpel and the opening repaired by hand suturing (recently, delta anastomosis for laparoscopic gastroduodenostomy has become popular [19], and it would be difficult to secure enough space for duodenectomy with stapling after this type of anastomosis because the previous staple line may extend into the deep part of the duodenum).
Previous gastrojejunostomy would have been performed via an antecolic or retrocolic route. When the previous anastomosis was anterior to the transverse colon, if the cancer does not invade the transverse colon, adhesions between the stomach, jejunum, and transverse colon should be carefully dissected, and both the afferent and efferent jejunum should be divided and transected. Because remnant gastric cancer can spread through the mesentery of the jejunum (Fig. 22.2), the lymph nodes around this mesentery should be removed as appropriate. When the previous gastrojejunostomy was performed by the retrocolic route, the mesocolon should be carefully divided without damaging the vessels supplying the transverse colon. If the cancer invades the transverse colon or vessels of the transverse colon, segmental resection of the transverse colon should be considered.
After resection of the duodenum following gastroduodenostomy or resection of both the afferent and efferent jejunum (and sometimes the transverse colon as well) following gastrojejunostomy, the remnant stomach is lifted upward and retracted by a second assistant. There will be fibrotic adhesions in the supra-pancreatic area if the reason for previous surgery was cancer. Adhesions in the supra-pancreatic area are divided, and any lymph nodes at #12a, #8a, #7, #11p, or #9 remaining from the previous surgery are dissected in the same manner as for primary gastric cancer.
Splenic hilar lymph node dissection is one of the most important parts of surgery for remnant gastric cancer, but relatively fewer adhesions are located here because this area will not have been affected by the previous gastrectomy, regardless of the reason for the surgery. When the left gastroepiploic vessels were not previously dissected, dissecting #4Sb and ligating the short gastric vessels (#4Sa) can expose the hilum of the spleen. If it is technically difficult to dissect the lymph nodes at the splenic hilum, splenectomy must be considered. However, routine splenectomy for completion total gastrectomy is not recommended, which is similar to the situation with total gastrectomy for primary gastric cancer. Note that spleen-preserving completion total gastrectomy is not the same as lymph nodes-around-the-splenic-hilum-preserving gastrectomy.
Figures 22.3 and 22.4 depict the extent of resection of the remnant stomach for remnant gastric cancer according to the type of previous anastomosis. The attached video clip summarizes the procedure of open completion total gastrectomy for remnant gastric cancer. This 71-year-old female patient underwent gastrectomy with gastrojejunostomy (loop, antecolic) for peptic ulcer disease 35 years previously. The order of dissection can be changed according to the surgeon’s preferences.
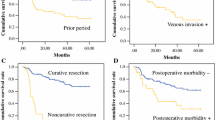
Treatment Outcomes of Remnant Gastric Cancer
Short-term outcomes of completion total gastrectomy for remnant gastric cancer have been reported by several studies. Postoperative morbidity rates have varied from 20% to 40%, and postoperative mortality rates have ranged from 0% to 12.5% [20,21,22,23,24]. Of note, most of these studies were conducted in East Asia, including Korea, Japan, and China. The mortality was relatively high in a study from the West [24]; however, this report was too old (published in 1986) to allow one to conclude that there is difference in mortality after completion total gastrectomy between the East and West. Overall, the morbidity and mortality rates after completion total gastrectomy for remnant gastric cancer seem to be generally similar to those reported after gastrectomy for primary gastric cancer. Few studies have directly compared short-term outcomes after remnant gastric cancer surgery to those after primary gastric cancer surgery; in these reports, outcomes were similar after both types of surgery [21, 25].
Whether the prognosis of remnant gastric cancer is poorer than that of primary gastric cancer in the upper third of the stomach is controversial [3, 26,27,28,29,30,31,32,33,34]. A recent systematic review that conducted pooled analyses examining this issue found that the outcomes among previous studies were significantly heterogeneous [5]. In subgroup analyses, the prognosis of remnant gastric cancer was similar in the early stages (stage I/II according to the current TNM staging system for primary gastric cancer) but poorer in the advanced stages (stage III/IV), compared to the prognosis after primary gastric cancer in the upper third of the stomach. These findings cannot be considered conclusive, and the reason for these results is not yet clear. However, they emphasize the importance of early detection of remnant gastric cancer.
Discussion
Remnant gastric cancers that we encounter clinically are mixtures of cancers that are similar to primary gastric cancers, tumors caused by chronic inflammation secondary to bile reflux, and other cancers caused by mechanisms that are not yet well understood. These varying etiologies of remnant gastric cancer lead to heterogeneous clinical responses to standard treatments, which are generally based on our current knowledge regarding primary gastric cancer. In addition, remnant gastric cancer in recent years primarily involves cancer in the remnant stomach after distal gastrectomy. Recently, function-preserving gastrectomy (e.g., proximal gastrectomy) has become popular to improve the quality of life of patients with early-stage gastric cancer, and survivors who have undergone this type of surgery are becoming more common. If we consider that two-thirds of gastric cancers in Korea and Japan occur in the lower third of the stomach, remnant gastric cancer after proximal gastrectomy for gastric cancer will likely increase in frequency, as the lower third of the stomach remains after this surgery; consequently, the landscape of remnant gastric cancer will change again. However, whether this type of remnant gastric cancer would or would not be similar to primary gastric cancer is another unclear issue.
Even amidst the aforementioned complexity, it is clear that radical surgery for remnant gastric cancer is the only treatment strategy available to provide a true cure. Nevertheless, radical surgery for remnant gastric cancer is technically difficult and challenging because of adhesions and fibrosis due to the previous surgery and because of alterations in the anatomy, including changes in the lymphatic drainage. Therefore, surgeons should refine their surgical skills and experience to conquer the present and upcoming complex disease, remnant gastric cancer. In addition, it cannot be overemphasized that following oncologic principles for cancer surgery is important for all operations involving remnant gastric cancer.
References
Kodera Y, Yamamura Y, Torii A, Uesaka K, Hirai T, Yasui K, et al. Incidence, diagnosis and significance of multiple gastric cancer. Br J Surg. 1995;82(11):1540–3.. Epub 1995/11/01. PubMed PMID: 8535813
Viste A, Bjornestad E, Opheim P, Skarstein A, Thunold J, Hartveit F, et al. Risk of carcinoma following gastric operations for benign disease. A historical cohort study of 3470 patients. Lancet. 1986;2(8505):502–5. PubMed PMID: 2875248
Kaneko K, Kondo H, Saito D, Shirao K, Yamaguchi H, Yokota T, et al. Early gastric stump cancer following distal gastrectomy. Gut. 1998;43(3):342–4. PubMed PMID: 9863478; PubMed Central PMCID: PMC1727245
Nakagawa M, Choi YY, An JY, Hong JH, Kim JW, Kim HI, et al. Staging for remnant gastric cancer: the metastatic lymph node ratio vs. the UICC 7th edition system. Ann Surg Oncol. 2016; https://doi.org/10.1245/s10434-016-5390-1. PubMed PMID: 27370654
Shimada H, Fukagawa T, Haga Y, Oba K. Does remnant gastric cancer really differ from primary gastric cancer? A systematic review of the literature by the Task Force of Japanese Gastric Cancer Association. Gastric Cancer. 2015; https://doi.org/10.1007/s10120-015-0582-0. Epub 2015/12/17. PubMed PMID: 26667370
Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3(4):219–25. PubMed PMID: 11984739
Ojima T, Takifuji K, Nakamura M, Nakamori M, Katsuda M, Iida T, et al. Endoscopic submucosal dissection for gastric tumors in various types of remnant stomach. Endoscopy. 2014;46(8):645–9. https://doi.org/10.1055/s-0034-1365454. PubMed PMID: 24777426
Takenaka R, Kawahara Y, Okada H, Tsuzuki T, Yagi S, Kato J, et al. Endoscopic submucosal dissection for cancers of the remnant stomach after distal gastrectomy. Gastrointest Endosc. 2008;67(2):359–63. https://doi.org/10.1016/j.gie.2007.10.021. Epub 2008/01/30. PubMed PMID: 18226704
Hirasaki S, Kanzaki H, Matsubara M, Fujita K, Matsumura S, Suzuki S. Treatment of gastric remnant cancer post distal gastrectomy by endoscopic submucosal dissection using an insulation-tipped diathermic knife. World J Gastroenterol. 2008;14(16):2550–5. Epub 2008/04/30. PubMed PMID: 18442204; PubMed Central PMCID: PMCPMC2708368
Nonaka S, Oda I, Makazu M, Haruyama S, Abe S, Suzuki H, et al. Endoscopic submucosal dissection for early gastric cancer in the remnant stomach after gastrectomy. Gastrointest Endosc. 2013;78(1):63–72. https://doi.org/10.1016/j.gie.2013.02.006. Epub 2013/04/10PubMed PMID: 23566640
Tanaka S, Toyonaga T, Morita Y, Fujita T, Yoshizaki T, Kawara F, et al. Endoscopic submucosal dissection for early gastric cancer in anastomosis site after distal gastrectomy. Gastric Cancer. 2014;17(2):371–6. https://doi.org/10.1007/s10120-013-0283-5. Epub 2013/07/23. PubMed PMID: 23868403
Lee JY, Choi IJ, Cho SJ, Kim CG, Kook MC, Lee JH, et al. Endoscopic submucosal dissection for metachronous tumor in the remnant stomach after distal gastrectomy. Surg Endosc. 2010;24(6):1360–6. https://doi.org/10.1007/s00464-009-0779-6.. PubMed PMID: 19997930
Choi YY, Kwon IG, Lee SK, Kim HK, An JY, Kim HI, et al. Can we apply the same indication of endoscopic submucosal dissection for primary gastric cancer to remnant gastric cancer? Gastric Cancer. 2014;17(2):310–5. https://doi.org/10.1007/s10120-013-0265-7.. Epub 2013/05/23. PubMed PMID: 23695167
Kwon IG, Cho I, Guner A, Choi YY, Shin HB, Kim HI, et al. Minimally invasive surgery for remnant gastric cancer: a comparison with open surgery. Surg Endosc. 2014;28(8):2452–8. https://doi.org/10.1007/s00464-014-3496-8. Epub 2014/03/14. PubMed PMID: 24622766
Tsunoda S, Okabe H, Tanaka E, Hisamori S, Harigai M, Murakami K, et al. Laparoscopic gastrectomy for remnant gastric cancer: a comprehensive review and case series. Gastric Cancer. 2016;19(1):287–92. https://doi.org/10.1007/s10120-014-0451-2. Epub 2014/12/17. PubMed PMID: 25503677
Nagai E, Nakata K, Ohuchida K, Miyasaka Y, Shimizu S, Tanaka M. Laparoscopic total gastrectomy for remnant gastric cancer: feasibility study. Surg Endosc. 2014;28(1):289–96. https://doi.org/10.1007/s00464-013-3186-y. Epub 2013/09/10. PubMed PMID: 24013469
Son SY, Lee CM, Jung DH, Lee JH, Ahn SH. Park do J, et al. laparoscopic completion total gastrectomy for remnant gastric cancer: a single-institution experience. Gastric Cancer. 2015;18(1):177–82. https://doi.org/10.1007/s10120-014-0339-1. Epub 2014/01/31. PubMed PMID: 24477417
Kim HS, Kim BS, Lee IS, Lee S, Yook JH, Kim BS. Laparoscopic gastrectomy in patients with previous gastrectomy for gastric cancer: a report of 17 cases. Surg Laparosc Endosc Percutan Tech. 2014;24(2):177–82. https://doi.org/10.1097/SLE.0b013e31828f6bfb. Epub 2014/04/02. PubMed PMID: 24686356
Kanaya S, Kawamura Y, Kawada H, Iwasaki H, Gomi T, Satoh S, et al. The delta-shaped anastomosis in laparoscopic distal gastrectomy: analysis of the initial 100 consecutive procedures of intracorporeal gastroduodenostomy. Gastric Cancer. 2011;14(4):365–71. https://doi.org/10.1007/s10120-011-0054-0. Epub 2011/05/17. PubMed PMID: 21573920
Kodera Y, Yamamura Y, Torii A, Uesaka K, Hirai T, Yasui K, et al. Gastric stump carcinoma after partial gastrectomy for benign gastric lesion: what is feasible as standard surgical treatment? J Surg Oncol. 1996;63(2):119–24. https://doi.org/10.1002/(SICI)1096-9098(199610)63:2<119::AID-JSO9>3.0.CO;2-H. PubMed PMID: 8888805
Imada T, Rino Y, Takahashi M, Shiozawa M, Hatori S, Noguchi Y, et al. Clinicopathologic differences between gastric remnant cancer and primary cancer in the upper third of the stomach. Anticancer Res. 1998;18(1A):231–5. Epub 1998/05/06. PubMed PMID: 9568082
Wang Y, Huang CM, Wang JB, Zheng CH, Li P, Xie JW, et al. Survival and surgical outcomes of cardiac cancer of the remnant stomach in comparison with primary cardiac cancer. World J Surg Oncol. 2014;12:21. https://doi.org/10.1186/1477-7819-12-21. PubMed PMID: 24468299; PubMed Central PMCID: PMC3906884
Kwon IG, Cho I, Choi YY, Hyung WJ, Kim CB, Noh SH. Risk factors for complications during surgical treatment of remnant gastric cancer. Gastric Cancer. 2015;18(2):390–6. https://doi.org/10.1007/s10120-014-0369-8. Epub 2014/04/08. PubMed PMID: 24705942
Viste A, Eide GE, Glattre E, Soreide O. Cancer of the gastric stump: analyses of 819 patients and comparison with other stomach cancer patients. World J Surg. 1986;10(3):454–61. PubMed PMID: 3727608
Thorban S, Bottcher K, Etter M, Roder JD, Busch R, Siewert JR. Prognostic factors in gastric stump carcinoma. Ann Surg. 2000;231(2):188–94.. PubMed PMID: 10674609; PubMed Central PMCID: PMC1420985
Sasako M, Maruyama K, Kinoshita T, Okabayashi K. Surgical treatment of carcinoma of the gastric stump. Br J Surg. 1991;78(7):822–4. PubMed PMID: 1873711
Pointner R, Wetscher GJ, Gadenstatter M, Bodner E, Hinder RA. Gastric remnant cancer has a better prognosis than primary gastric cancer. Arch Surg. 1994;129(6):615–9.. Epub 1994/06/01. PubMed PMID: 8204036
Newman E, Brennan MF, Hochwald SN, Harrison LE, Karpeh MS Jr. Gastric remnant carcinoma: just another proximal gastric cancer or a unique entity? Am J Surg. 1997;173(4):292–7. https://doi.org/10.1016/s0002-9610(96)00403-5. Epub 1997/04/01. PubMed PMID: 9136783
Bruno L, Nesi G, Montinaro F, Carassale G, Lassig R, Boddi V, et al. Clinicopathologic findings and results of surgical treatment in cardiac adenocarcinoma. J Surg Oncol. 2000;74(1):33–5. PubMed PMID: 10861606
An JY, Choi MG, Noh JH, Sohn TS, Kim S. The outcome of patients with remnant primary gastric cancer compared with those having upper one-third gastric cancer. Am J Surg. 2007;194(2):143–7. https://doi.org/10.1016/j.amjsurg.2006.10.034. Epub 2007/07/10. PubMed PMID: 17618792
Schaefer N, Sinning C, Standop J, Overhaus M, Hirner A, Wolff M. Treatment and prognosis of gastric stump carcinoma in comparison with primary proximal gastric cancer. Am J Surg. 2007;194(1):63–7. https://doi.org/10.1016/j.amjsurg.2006.12.037. PubMed PMID: 17560911
Mezhir JJ, Gonen M, Ammori JB, Strong VE, Brennan MF, Coit DG. Treatment and outcome of patients with gastric remnant cancer after resection for peptic ulcer disease. Ann Surg Oncol. 2011;18(3):670–6. https://doi.org/10.1245/s10434-010-1425-1. Epub 2010/11/11. PubMed PMID: 21063791
Li F, Zhang R, Liang H, Zhao J, Liu H, Quan J, et al. A retrospective clinicopathologic study of remnant gastric cancer after distal gastrectomy. Am J Clin Oncol. 2013;36(3):244–9. https://doi.org/10.1097/COC.0b013e3182467ebd. Epub 2012/04/13. PubMed PMID: 22495457
Tokunaga M, Sano T, Ohyama S, Hiki N, Fukunaga T, Yamada K, et al. Clinicopathological characteristics and survival difference between gastric stump carcinoma and primary upper third gastric cancer. J Gastrointest Surg. 2013;17(2):313–8. https://doi.org/10.1007/s11605-012-2114-0. PubMed PMID: 23233273
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Electronic Supplementary Material
(MP4 512284 kb)
Rights and permissions
Copyright information
© 2019 Springer-Verlag GmbH Germany, part of Springer Nature
About this chapter
Cite this chapter
Choi, Y.Y., Noh, S.H. (2019). Surgery for Remnant Gastric Cancer: Open Surgery. In: Noh, S., Hyung, W. (eds) Surgery for Gastric Cancer. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-45583-8_22
Download citation
DOI: https://doi.org/10.1007/978-3-662-45583-8_22
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-45582-1
Online ISBN: 978-3-662-45583-8
eBook Packages: MedicineMedicine (R0)