Abstract
Recently Dielectric Barrier Discharge plasma is being explored for its application as an alternative to the conventional sterilization and disinfection techniques in medical sciences. Dielectric barrier discharge plasma torch has been developed to study the interaction of plasma and effect of its treatment on the growth rate of S. aures, Escherichia coli, Bacillus subtilis and E. faecalis. Plasma treated E. faecalis was compared with Chlorhexidine treated cultures and biofilms of E. faecalis. The results are analysed for significance (P < 0.001) using ANOVA and TUCKEY’s test. In-situ optical emission spectroscopy has been employed to identify the plasma species interacting with the bioculture and biofilm. Based on its efficient disinfecting properties dielectric barrier discharge plasma has been proved to be a promising alternative to traditional techniques used for sterilization during the endodontic treatment.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Recently, cold plasma is being explored for its application as an alternative to the conventional sterilization and disinfection techniques in medical field. Amongst the different types of plasmas, studies on Dielectric Barrier Discharge (DBD) plasma has gained importance in the medical field due to its property of being functional at room temperature and atmospheric pressure; unlike low pressure cold plasmas. The antimicrobial property of dielectric barrier discharge plasma has been demonstrated against several bacteria for example Escherichia coli, Candida albicans, Streptococcus mutans, Bacillus subtilis etc. [1].
In the field of dentistry, microorganisms and their by-products are considered to be the major cause of pulp and periradicular pathosis. The objective of endodontic therapy is to [i] remove diseased tissue, [ii] eliminate bacteria present in the canals as well as dentinal tubules and [iii] prevent post endodontic recontamination. Hence, a major objective in root canal treatment is to disinfect the entire root canal system and to eliminate all the possible sources of infection. This can be accomplished by using mechanical instrumentation and chemical agents, in conjunction with medication of the root canal system between treatment sessions. In spite of these treatments, the survival of microorganisms in the apical portion of root filled teeth is still the major cause of endodontic failure. Studies have revealed that this increased resistance is due to the formation of biofilms by the microorganisms. Microorganisms like Enterococcus faecalis, Streptococcus mutans, and Candida albicans can adhere to the root canal walls and form communities organized in biofilm which makes them more resistant to phagocytosis, antibodies, and antimicrobials. This is due to the presence of exopolysaccharides in comparison with non-biofilm producing organisms [2]. Also, due to the presence of dentin tubules; the disinfection of dentin posses special challenges during caries therapy. Conventionally disinfection is achieved by [i] invasive removal, [ii] use of chemicals like chlorhexidine. But these treatments do not disinfect the dental tubules completely. Contact dermatitis is a common adverse reaction to chlorhexidine. Chlorhexidine is also liable to cause desquamative gingivitis, discoloration of tongue and teeth or dysgeusia (distorted taste). Plasma being in the gaseous form would have a better reach in the confined and tortuous root canal system and may prove to be a better adjunct to root canal instrumentation for canal sterilization. Hence, inactivation of microorganisms using plasma has attracted much attention recently.
Numerous in vitro studies have been conducted on the effects of atmospheric plasma on pathogens like Streptococcus mutans, Candida albicans, Chromobacterium violaceum etc. Amongst the various oral pathogens Enterococcus faecalis is one of the primary organisms in patients with post treatment endodontic infection [3]. E. faecalis is known to form intracanal biofilms, periapical biofilms and biomaterial centered infection.
Inspite of being one of the important infection causing organism, relatively few reports are available that describe the efficacy of dielectric DBD plasma against E. faecalis. Hence, this study was aimed at evaluating the inhibitory effect of DBD plasma against E. faecalis culture and biofilms. Initially experiments were carried out with S. aures, Escherichia coli, Bacillus subtilis etc. which was found to be effective for destruction of these bacteria. Later on these bacteria were replaced by E. faecalis for further investigation. The paper reports the use of He (atmospheric pressure) as a plasma generating gas which enables the formation of active reactive species useful for bactericidal properties.
2 Materials and Methods
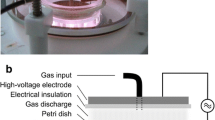
DBD plasma torch is found to be useful for varieties of applications. Its use for dental applications is an emerging field of research. In the present article we report on the development of a small plasma torch with helium as plasma forming gas. Figure 1 shows the schematic of the atmospheric pressure DBD plasma torch which consisted of a tungsten cathode in the form of thin wire axially fitted into a cylindrical glass tube with a fine nozzle. The anode was a stainless steel plate which formed the base below the microtitre plate. The anode is grounded. A 1.5 mm thick glass slab work as the dielectric material to obtain the DBD plasma. Helium was made to flow at a flow rate of 1 lpm through the torch system so as to reach the bacterial culture placed inside the microtitre plate. Pulsed dc voltage of 24 kV was used to operate the torch. The plasma plume 1–2 mm in diameter extended outside the nozzle up to a distance of 2–3 cm and reached the E. faecalis culture. Helium having a low ionization potential serves as a suitable ionizing medium and helps in extracting the plasma plume to larger distances. Compared to other gas plasmas it is easy to obtain plume of few centimeter by using helium gas as plasma forming gas [4]. There are several other advantages of using He as a plasma forming gas like, He gas flow propels radicals and metastables towards the surface to be treated. The flow diameter helps to determine the diameter of the treated portion of the sample and moreover it has a high thermal conductivity and thus acts like a coolant. Also the flow mixes with the atmospheric gases like H2O, N2, and O2 at the downstream from the nozzle [5]; and help in producing reactive atomic oxygen and hydroxide (OH·) species which are well known to be bactericidal.
In order to examine the species responsible and to understand the mechanism of reaction of the bacteria and plasma species; the optical emission spectroscopic studies were carried out. The photon collection was facilitated with an optical fiber which was directed towards the junction between the plasma plume and the upper meniscus of the bio-culture and bio-films. Ocean Optics spectrophotometer (model HR-4000) was employed for the measurements. A collection of species which were produced in the process has been useful to understand the reaction mechanism within the dye due to the plasma.
The glow in the plasma is due to the electron excitation, de-excitation and ionization of the gas atoms, so that it serves as a visual indicator of the presence of energetic electrons and photons. These energetic electrons generate radicals by dissociating gas molecules such as H2O and O2, or by generating metastable He ions that probably dissociate H2O molecules. The air mixed with water molecules help in generating the reactive OH and O radicals which further assist in the killing of the E. faecalis bacteria (Fig. 2) [5].
Enterococcus faecalis (NCIM 5025) was procured from National Collection of Industrial Microorganisms, Pune. The strain was maintained on MRS (de Man, Rogosa and Sharpe) medium (composition per liter: peptone 10 g, meat extract 10 g, yeast extract 5 g, sodium acetate 5 g, dipotassium phosphate 2 g, ammonium citrate 2 g, magnesium sulfate 0.2 g, manganese sulfate 0.05 g, glucose 20 g, between 80 1 g) slants and stored at 4 °C. The effect of atmospheric plasma against E. faecalis culture was monitored as follows. 100 µl of culture was placed in each well of 96 well microtitre plate. The culture was then treated with atmospheric plasma for 2 min. The wells were grouped into 4 groups viz. group A - helium treated, group B, plasma treated and group C - chlorhexidine treated D - control, with a size of 30 wells per group. E. faecalis culture was treated with chlorhexidine for 2 min by adding 100 µl of 0.2 % chlorhexidine solution to the wells and subsequent removal of the solution after 2 min. The viability of the cells was checked by Triphenyl tetrazolium chloride (TTC) assay.
Preparation of the bio-films of E. faecalis was inoculated in MRS broth and incubated at 37 °C at 120 rpm for 24 h. 100 µl of culture (OD 1.0 according to McFarland’s scale, colony forming unit (CFU) 4 × 108/ml) was added in each well of 96-well flat base microtitre plate. The plate was incubated at 37 °C for 1 h in order to allow the organisms to adhere to the surface of the wells. After 1 h, remaining culture from the wells was replaced by 100 µl of fresh MRS broth and the plate was further incubated at 37 °C for 24 h. After incubation, the excess medium from the wells was removed and the biofilms were then treated with DBD plasma for 2 min. The experiment was divided into 4 groups as mentioned above. S. aures, Escherichia coli and Bacillus subtilis were inoculated in Nutrient broth and incubated at 37 °C at 120 rpm for 24 h. The bioculture was treated with DBD plasma for 2 min. All the conditions are same as for E. Faecalis.
2.1 Viability Assay
The viability of the organisms was determined using the TTC viability assay described by C E Nwanyanwu with some modifications [6]. 100 µl of 1 % (w/v) solution of TTC prepared in sterile distilled water was added in the wells along with 100 µl of MRS broth following the treatments. The plates were incubated at 37 °C overnight. The color change was measured at 490 nm using Elisa plate reader (Bio Rad model no: IMark).
All the results are analysed for significance (P < 0.001) using ANOVA and TUCKEY’s test. Optical Emission Spectrometer (OES) model HR-4000 (manufactured by Ocean Optics) was employed for the identification of active ionic species present in the plasma. This spectrometer had a linear CCD array detector (model TCD1304AP) and the range of detection extended from 200 nm to 1100 nm with a resolution of ~0.03 nm (FWHM). In addition it has fiber optical input.
3 Results and Discussion
S. aures, B. subtilis, and E. coli cultures were exposed to atmospheric non-thermal helium plasma for 2 min. These organisms were also treated with chlorhexidine and helium. The results of the viability assay were then compared for all three processes as shown in Fig. 3. In all the four groups (Fig. 3), the mean bacterial count for three experiments has been shown. The control group is considered to be 100 % for bacterial survival. The group treated with helium showed same optical density as that of control; indicating that the killing effect of plasma is not due to presence of helium. Significant reduction in optical density was observed in the cultures exposed to chlorhexidine and plasma. In case of S. aures the optical density as compared to that of the control is reduced to be 25 % by chlorhexidine and 58 % after plasma treatment. In case of B. subtilis the optical density reduction was observed to be 2 % by cholorohexidine treatment while 37 % by plasma treatment. However in case of E. coli the reduction in optical density for chlorhexidine treated culture was found to be 9 % while 61 % for plasma treated culture. Effect of atmospheric plasma, helium and chlorhexidine on the culture plates was determined by TTC viability assay.
E. faecalis culture was exposed to DBD helium plasma for 2 min. Similarly, culture was also treated with chlorhexidine and helium for 2 min. The results of the viability assay were then compared for the three processes as shown in Fig. 4. It shows the mean bacterial count in terms of optical density in all the four groups. The wells in the control group and the wells treated with helium exhibited no change in the optical density (OD 1.0) indicating 100 % survival of the culture. However significant reduction in optical density was observed in the wells exposed to chlorhexidine (OD 0.7) and plasma (OD 0.6). Inhibitory effects of DBD plasma have also been reported on E. faecalis culture by Cao et al. [7]. The culture was exposed to helium-oxygen plasma for 5, 10 and 15 min. The post exposure viability was determined by measuring the zone of inhibition. Effects of atmospheric plasma, helium and chlorhexidine on E. faecalis biofilms adhered on wells of the microtitre plates were determined by TTC viability assay. The results were similar to those observed for the culture. Chlorhexidine and plasma treated biofilms showed decrease in optical density.
It was 0.5 for chlorhexidine, 0.47 for plasma as compared to 0.8 of control and helium treated biofilms. This clearly indicated reduction in viability of bacteria in biofilms (Fig. 6).
In order to confirm the presence of the reactive species we have carried out the spectral identification using optical emission spectroscopy. Figure 5 shows the OES spectrum recorded during the plasma exposure of the E. faecalis culture. Optical emission spectrum shows that the species present in the plasma include helium, atomic oxygen (O), Ozone (O3), and OH radicals.
Figure 6 shows that helium gas alone did not show any inhibitory effect on biofilms. Inhibitory effects of DBD plasma have also been examined on Chromobacterium violaceum [8] and on Streptococcus mutans biofilms [9]. Du et al. [10] have also reported the reduction in viability of E. faecalis biofilms after treatment with DBD plasma. The authors also determined the viability using confocal laser scanning microscopy. Cao et al. [7] have reported antibacterial effects of atmospheric plasma on E. faecalis biofilms prepared on nitrocellulose membrane using SEM. Our results of 2 min exposure, leading to a significant reduction in the viability, suggest that this technique can be used as an adjunct for endodontic therapy in dentistry. Further research in this line could prove its potential as an alternative for traditional procedures of disinfection. However it has been obvious that the oxygen and OH radicals which are known to be bactericidal, most probably, react with the cell walls of the bacteria causing the rupture of the cell walls. As an effect the cytoplasm leaks out, causing the death of the bacteria.
4 Conclusions
Dielectric Barrier Discharge plasma proves to be a promising alternative to the traditional disinfectants for disinfection during endodontic treatment. Using plasma will be beneficial mainly due to its gaseous nature, improved dispersion of disinfectant in the dentinal tubules, better reach in the tortuous canals and no dysgeusia (distorted taste). Hence, application of DBD plasma can be a quick method since post disinfection clean-up procedures can be minimized during endodontic treatments.
References
Hong, Y.F., Kang, J.G., Lee, H.Y., Uhm, H.S., Moon, E., Park, Y.H.: Sterilization effect of atmospheric plasma on Escherichia coli and Bacillus subtilis endospores. Lett. Appl. Microbiol. 48, 33–37 (2009)
Sabeena, M., Boopathi, T.: Enterococcus faecalis - an endodontic challenge. J. Ind. Acad. Dent. Spec. 1(4), 46–50 (2010)
Mohammadi, Z., Abbott, P.V.: The properties and applications of chlorhexidine in endodontics. Int. Endod. J. 42, 288–302 (2009)
Sladek, R.E.J., Stoffels, E., Walraven, R., Tielbeek, P.J.A., Koolhoven, R.A.: Plasma treatment of dental cavities: a feasibility study. IEEE Trans. Plasma Sci. 32(4), 1540–1543 (2004)
Goree, J., Liu, B., Drake, D., Stoffels, E.: Killing of S. mutans bacteria using a plasma needle at atmospheric pressure. IEEE Trans. Plasma Sci. 34(4), 1317–1323 (2006)
Nwanyanwu, C.E., Abu, G.O.: Influence of pH and inoculum size on phenol utilization by bacterial strains isolated from oil refinery effluent. Int. J. Nat. Appl. Sci. 7(1), 8–15 (2011)
Cao, Y., et al.: Efficacy of atmospheric pressure plasma as an antibacterial agent against Enterococcus faecalis in vitro. Plasma Sci. Technol. 13(1), 93–98 (2011)
Jonathan, C.J., Kwan, C., Abramzon, N., Vandervoort, K., Brelles-Marin, G.: Is gas-discharge plasma a new solution to the old problem of biofilm inactivation? Microbiology 155, 724–732 (2009)
Sladek, R.E.J., Filoche, S.K., Sissons, C.H., Stoffels, E.: Treatment of Streptococcus mutans biofilms with a nonthermal atmospheric plasma. Lett. Appl. Microbiol. 45(3), 318–323 (2007)
Du, T., Ma, J., Yang, P., Xiong, Z., Lu, X., Cao, Y.: Evaluation of antibacterial effects by atmospheric pressure non-equilibrium plasmas against Enterococcus faecalis biofilms in vitro. J. Endod. 38(4), 545–549 (2011)
Acknowledgements
ASB is thankful to UGC for the award of Ph.D. fellowship. SVB is thankful to DST and CSIR, New Delhi for the financial support and award of ES fellowship.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this paper
Cite this paper
Bansode, A.S. et al. (2014). Dielectric Barrier Discharge Plasma for Endodontic Treatment. In: Fernández-Chimeno, M., et al. Biomedical Engineering Systems and Technologies. BIOSTEC 2013. Communications in Computer and Information Science, vol 452. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-662-44485-6_7
Download citation
DOI: https://doi.org/10.1007/978-3-662-44485-6_7
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-662-44484-9
Online ISBN: 978-3-662-44485-6
eBook Packages: Computer ScienceComputer Science (R0)