Abstract
Preoperative withdrawal of antiplatelet (AP) therapy in secondary prevention multiplies the risk of myocardial infarction, stent thrombosis, stroke, or death, by five to ten times. Aspirin is a lifelong therapy and should never be interrupted. Dual AP therapy with aspirin plus clopidogrel, prasugrel, or ticagrelor is essential for at least 6 weeks after coronary revascularization using bare-metal stents, 12 months after treatment for acute coronary syndrome, and 6–12 months after implanting drug-eluting stents. These time spans might even be prolonged in high-risk cases. Elective surgery should be postponed until after these periods. Vital or urgent operations undertaken earlier must be performed under continued dual AP therapy.
Preoperatively, patients might be on prophylactic or therapeutic doses of anticoagulants. The indication for the anticoagulation therapy must be reevaluated in order to balance the thrombotic risk of interrupting against the risk of bleeding when continuing the treatment. A detailed protocol, comprising the pre-, peri-, and postoperative phases needs then to be established. It should include indications regarding anticoagulation reversal, bridging (when necessary), and postoperative reintroduction of the anticoagulant therapy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Stent Thrombosis
- Anticoagulant Effect
- Dual Therapy
- Prothrombin Complex Concentrate
- Inferior Vena Cava Filter
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Antiplatelet agents
1.1 Introduction
Perioperative management of antiplatelet (AP) drugs is a major challenge. Dual AP therapy (aspirin plus clopidogrel, prasugrel, or ticagrelor) is the key to preventing myocardial infarction (MI) after acute coronary syndrome (ACS) or stent thrombosis (ST) following the implant of bare-metal (BMS) or drug-eluting stents (DES). In this population, platelet inhibition in the perioperative period is particularly important because of the increased platelet activity associated with the postoperative acute inflammatory response. Unfortunately, AP drugs also increase the risk of surgical bleeding. The key question is whether the risk of thrombosis when AP agents are withdrawn is higher than the risk of hemorrhage when they are maintained. Current recommendations are based on the results of highly reliable cardiologic trials (level of evidence A) and on large observational or prospective studies collected in surgery and anesthesiology (level of evidence B). Taken together, these data can be considered as adequate for defining the safest possible strategy.
1.2 Antiplatelet Therapy
The different AP agents are classified according to the type of receptor they inhibit on the platelet (Fig. 8.1). Their pharmacology is described in Tables 8.1 and 8.2. At doses of 50–160 mg/day, aspirin completely inhibits the cyclooxygenase-1 (COX-1) enzyme which converts arachidonic acid to thromboxane A2 (TXA2), the ligand for the homonymous platelet receptor. However, 6–10 % of the population shows a low response to aspirin treatment, resulting in insufficient platelet inhibition. In some patients, this is due to insufficient inhibition of the COX-1 enzyme by aspirin. Yet in others, due to a predominance of alternative activation pathways (e.g., ADP, thrombin), the platelet function remains normal in spite of sufficient COX-1 inhibition. Competitive interaction with nonsteroidal anti-inflammatory drugs (NSAIDs) may also reduce aspirin efficiency (Patrono and Rocca 2010).
Classification of the different AP agents. Blockers of von Willebrand factor/adhesion molecules and thrombin receptor blockers are under investigation (Adapted with permission from www.pac4.ch). ADP adenosine diphosphate, cAMP cyclic adenosine monophosphate, COX-1 cyclooxygenase-1, Fib fibrinogen, inhib inhibitor, NSAID nonsteroidal anti-inflammatory drug, TXA 2 thromboxane A2, vWF von Willebrand factor
Clopidogrel (Plavix™, Iscover™) is a prodrug which is oxidized into an active metabolite in a two-step process by hepatic cytochromes. This metabolite irreversibly blocks the adenosine diphosphate (ADP) receptor (P2Y12) and reduces platelet activity by 50–60 % (Hall and Mazer 2011). Clopidogrel’s efficiency may be lowered because of competition for the same cytochromes by midazolam, fluoxetine, some lipophilic statins (particularly atorvastatin), and some proton pump inhibitors (particularly omeprazole). Although the evidence for an increase in cardiovascular complications is modest, it is safer to avoid the administration of atorvastatin, omeprazole, and clopidogrel simultaneously (Bates et al. 2011). There are no major differences in terms of bleeding between aspirin and clopidogrel monotherapy. After cessation of aspirin or clopidogrel, bleeding time and global platelet activity return to baseline levels in 5 days (Bhatt et al. 2006).
Up to 30 % of patients respond poorly to clopidogrel. One reason is polymorphism in the genes that code the hepatic enzymes involved in the synthesis of the active metabolite. Patients with abnormal alleles are 1.6–3.5 times more likely to experience cardiovascular complications and stent thrombosis when treated with clopidogrel (Mega et al. 2010). Patients who maintain a residual platelet activity after a loading dose of clopidogrel are four to six times more likely to suffer infarction and stent thrombosis than normal responders (Aradi et al. 2010) (Fig. 8.2).
Compared to clopidogrel, prasugrel (Effient™) is faster acting, is more potent, and has a much lower rate of low responders. It is more efficient in diabetics and patients with ST-elevation MI and is twice as efficient in preventing stent thrombosis. However, it does increase the risk of spontaneous hemorrhage 1.5 times and of surgical bleeding up to four times (Wiviott et al. 2007). Considering its potency, prasugrel cessation 7 days before surgery is recommended.
Ticagrelor (Brilinta™, Brilique™, Possia™) is a powerful and reversible ADP receptor blocker. One hour after a loading dose, 80 % of platelet activity is inhibited and after cessation, it takes 3 days for platelet function to recover (Gurbel et al. 2009). Ticagrelor is more efficient than clopidogrel in preventing stent thrombosis, yet does not increase the hemorrhagic risk (Wallentin et al. 2009). Because some patients produce a long-acting metabolite, it is recommended to stop ticagrelor 5 days before an operation.
Rate of major adverse cardiac events (MACE, in blue) after percutaneous coronary intervention and stenting according to the residual platelet activity after a loading dose of aspirin and clopidogrel. Since adverse events cluster in the highest quartile (Q4), there is a larger benefit to decrease platelet activity from Q4 to 50 % than from 50 % to Q1. The curve for hemorrhagic risk (in red) is mirrorlike and varies in the opposite direction. These two curves determine an optimal window with the best combination of minimal risk of bleeding and maximal platelet inhibition (Adapted with permission from Price (2009))
Cangrelor is an intravenous fast onset and offset drug, which will be useful for preoperative substitution of long-acting agents. It abolishes platelet aggregation but allows a complete recovery of platelet activity within 1–3 h of stopping the perfusion (Angiolillo et al. 2012).
Dual AP therapy is essential after ACS or stent implantation because vascular lesions and stents behave like unstable plaques if they are not fully covered by a cellular layer. It takes 6 weeks for the frame of a BMS to become covered by smooth muscle cells and 3 months to be protected by a normal endothelium. DES have a slower endothelialization rate: 20 % at 3 months and 60 % at 1 year (Joner et al. 2006). Thus, the minimal duration of dual AP therapy following implantation is 6 weeks for BMS and 12 months for DES (Table 8.3) (Task Force on Myocardial Revascularization of the European Society of, the European Association for Cardio-Thoracic et al. 2010). These periods can be prolonged beyond 1 year for high-risk stents (DES implanted in dominant, ostial, or bifurcated positions) and high-risk patients (previous ST, diabetes, cardiac or renal failure). Late DES thrombosis is a rare (0.6 %/year) but catastrophic event with a mortality of 9–45 % since it leads to the acute interruption of flow in a previously normal vessel (Dangas et al. 2011). New-generation DES have a faster rate of endothelialization and a lower incidence of ST; depending on the type of stent, the duration of dual AP therapy is 6–12 months.
1.3 Withdrawal of AP Agents
Cessation of AP therapy is associated with an increased mortality and ischemic risk: the shorter the duration, the higher the complication rate. Aspirin withdrawal is associated with an increased risk of cardio- and cerebrovascular complications (Biondi-Zoccai et al. 2006). Cases of acute DES thrombosis following aspirin withdrawal have been reported more than 3 years after stent implantation (Artang and Dieter 2007; Fujimoto et al. 2009). Thrombotic events peak 7 days after interruption, whatever the duration of treatment (Eisenberg et al. 2009). Therefore, aspirin should be a lifelong therapy, never interrupted (Task Force on Myocardial Revascularization of the European Society of, the European Association for Cardio-Thoracic et al. 2010). Stopping clopidogrel is the most significant independent predictor for ST (Gaglia and Waksman 2011). During the first 6 months of therapy, the average delay between clopidogrel cessation and ST is 9 days (Schulz et al. 2009). Although the usefulness of prolonging dual therapy beyond 1 year remains unsettled, there is clear clinical evidence that its cessation during that first year is exceedingly dangerous (Valgimigli et al. 2012).
The interruption of AP drugs is more hazardous in the perioperative period because of the ensuing increased platelet stimulation and the acute systemic inflammatory reaction. Interruption is the major independent factor predicting cardiac complications after noncardiac surgery (Barash and Akhtar 2010). Stopping dual AP therapy to allow major surgery during the first 3 months after angioplasty and stenting (BMS or DES) leads to an average cardiac mortality of 30–50 %, whereas it is ≤5 % when the treatment is maintained perioperatively (Sharma et al. 2004; Schouten et al. 2007; Nuttall et al. 2008; Rabbitts et al. 2008). Mortality is inversely related to the delay between revascularization and surgery (Fig. 8.3).
Schematic illustration of the relationship between mortality for noncardiac surgery and time since revascularization in case of perioperative interruption of dual antiplatelet therapy. During the first 6 weeks after coronary artery bypass graft surgery (CABG), bare-metal stents (BMS), or drug-eluting stents (DES), mortality is around 30 %. After BMS and CABG, it takes 3 months for postoperative mortality to reach the level of patients with no active coronary artery disease, whereas after DES the plateau of the curve is reached only after 12 months
The recommended delays between revascularization and noncardiac surgery are as follows:
-
Angioplasty without stenting: 2–4 weeks (vital surgery only).
-
BMS and coronary artery bypass graft (CABG): 6 weeks for vital surgery and 3 months for elective surgery.
-
DES: >12 months for elective surgery; vital surgery could be performed within 2–12 months under full AP therapy.
1.4 Hemorrhagic Risk Linked to AP Agents
The body of evidence shows that aspirin or clopidogrel taken alone increase average blood loss by 20 % during noncardiac surgery (Chassot et al. 2007). Some operations can show a significant increase in postoperative hemorrhage, such as tonsillectomy or transurethral prostatectomy. Life-threatening hemorrhage has only been reported in intracranial neurosurgery. A meta-analysis including 474 studies comparing surgical bleeding across all kinds of surgery reports no difference in mortality and complication rates between patients who took aspirin and those who did not (Burger et al. 2005).
With aspirin and clopidogrel dual therapy, the relative risk of bleeding increases by up to 50 %, as observed in orthopedic, vascular, abdominal, thoracic, urological, and endoscopic surgery (Moore and Power 2004; Albaladejo et al. 2011; Chernoguz et al. 2011; Taylor et al. 2011). Although hemostasis is difficult and tedious, particularly because of the increased oozing from bones and raw tissues, surgical mortality and long-term morbidity are not increased. In series comparing general surgery with and without dual AP therapy, the transfusion rate is inconsistently affected (relative increase: 4, 12, 16, and 17 %) (Wilson et al. 2003; Schouten et al. 2007; Rabbitts et al. 2008; Chernoguz et al. 2011). Aspirin and clopidogrel do not appear to cause an increase in surgical complications, except for surgery in a closed space (intracranial neurosurgery, surgery of the spinal canal or the posterior ocular chamber) or surgery associated with massive hemorrhage and difficult hemostasis. In these cases, clopidogrel, prasugrel, and ticagrelor should be interrupted or substituted by a short-acting agent (Chassot et al. 2007; Eberli et al. 2010). In cardiac surgery, the situation is more critical due to the full heparinization during heart-lung bypass: blood loss and reoperation for bleeding control are more than doubled; the transfusion rate is increased up to four times; however, mortality remains unchanged (Task Force on Myocardial Revascularization of the European Society of, the European Association for Cardio-Thoracic et al. 2010).
1.5 Recommendations and Guidelines
Current recommendations are based on the safest possible management of the dangers of discontinuing AP agents prematurely (Douketis et al. 2008; American Society of Anesthesiologists Task Force on Neuraxial et al. 2009; Task Force on Myocardial Revascularization of the European Society of, the European Association for Cardio-Thoracic et al. 2010; Korte et al. 2011). They are illustrated as an algorithm in Fig. 8.4 and are summarized in Table 8.4.
Algorithm for the preoperative management of patients under antiplatelet therapy. Low-risk conditions are depicted in yellow, high-risk conditions in red, and decisions in magenta. 1 High-risk stents: multiple stents, long stent, proximal location (left main), and bifurcation lesions; patients with previous stent thrombosis; stent in unique patent vessel. 2 Excessive risk of bleeding: invasive surgery associated with severe bleeding and difficult hemostasis, or bleeding in closed spaces (intracranial neurosurgery, intramedullary canal surgery, posterior eye chamber ophthalmic surgery). 3 The same recommendations apply to prasugrel and ticagrelor. In all cases, restart AP within 24 h postoperative. BMS bare-metal stent, DES drug-eluting stent, ACS acute coronary syndrome, MI myocardial infarction, PCI percutaneous coronary intervention, CABG coronary artery bypass graft surgery (Adapted with permission from www.pac4.ch and form Eberli et al. (2010))
-
Aspirin for primary prevention can be interrupted 5 days before surgery, except in high-risk cases, such as diabetics.
-
Aspirin or clopidogrel monotherapy for secondary prevention after a stroke, ACS, MI, or coronary revascularization should be maintained throughout the perioperative period, whatever the duration of treatment.
-
Aspirin plus dipyridamole dual therapy after stroke should be maintained throughout the perioperative period.
-
Aspirin plus clopidogrel/prasugrel/ticagrelor dual therapy in patients with a low cardiovascular risk: maintain continuous treatment with aspirin; stop clopidogrel 5 days, prasugrel 7 days, and ticagrelor 5 days before surgery; restart clopidogrel/prasugrel/ticagrelor within 24 h after surgery, preferably with a loading dose (if hemorrhagic risk is low).
-
Aspirin plus clopidogrel/prasugrel/ticagrelor dual therapy in patients with high cardiovascular risk: delay elective surgery for 3 months after a stroke, BMS, or CABG, 6 months after acute coronary syndrome or infarction, and 12 months after DES. Beyond these delays: maintain aspirin; if clopidogrel/prasugrel/ticagrelor is still prescribed, discuss with the cardiologist and the surgeon whether to stop or maintain. Delay vital or semi-urgent surgery for at least 6 weeks if possible; maintain both aspirin and dual therapy.
During the first 6 weeks after ACS or revascularization, the operative risk is exceedingly high – even higher than without coronary revascularization. The full benefit of revascularization only manifests itself 3 months after BMS or CABG and 12 months after DES, when mortality returns to the level of noncoronary patients. All elective operations should therefore be postponed beyond these delays. Only vital surgery should be performed on patients still on dual AP therapy; unless the hemorrhagic risk is excessive, dual AP therapy should not be interrupted before surgery. Heparin and LMWHs have no AP activity and are not adequate substitutes for long-acting AP drugs since stent thrombosis is a platelet-mediated phenomenon. A bridge using a 3-day continuous perfusion of a short-acting anti-GP IIb/IIIa agent, such as eptifibatide or tirofiban, is the only effective substitute for clopidogrel or prasugrel, when aspirin is maintained (Savonitto et al. 2010). The perfusion can be stopped 6–8 h before surgery. After the operation, AP therapy should be resumed within the first 24 h.
1.6 Intraoperative Management
Intrathecal and epidural anesthesia are strictly contraindicated in case of dual AP therapy, although they are allowed in patients taking aspirin only, up to 325 mg/day (Gogarten et al. 2010). Although they undoubtedly improve patient comfort, their impact on cardiovascular outcomes is negligible. With a five- to tenfold increase in MI, the risk linked to AP withdrawal is obviously much higher than the benefit expected from neuraxial blockade. Stopping AP drugs in order to perform an intrathecal or epidural anesthesia is therefore clearly unjustified.
Aspirin, clopidogrel, and prasugrel are irreversible blockers. Since they have no antidotes, platelet renewal (10 %/day) is the only way for platelet aggregation to return to normal. As soon as 50 % of platelets have been renewed, blood hemostasis functions normally. Therefore, 5–7 days without AP therapy are required to prevent excessive surgical bleeding. It is commonly accepted that a substance’s plasma level is negligible after 3 half-lives. Therefore, 24 h after the last intake of clopidogrel (half-life: 7.5 h) and 12 h after the last dose of prasugrel (half-life: 3.7 h), there is no residual AP activity in the plasma. Although the patient’s native platelets are still inhibited, the platelets transfused after these delays will function adequately.
After cessation of the reversible AP drug ticagrelor, platelet function recovers more rapidly compared to clopidogrel, since it is not dependent on platelet renewal. Yet, 48 h after interruption of either drug, platelets still show the same degree in inhibition. Only 3 days after cessation, ticagrelor shows a lower degree of inhibition than clopidogrel (Gurbel et al. 2009).
As a reversible drug, ticagrelor will be redistributed from circulating platelet receptors to the receptors of transfused platelets. Platelet transfusion my therefore not be efficient to reverse the AP effect in emergency situations.
Postoperative stent thrombosis – usually manifested as an acute ST-elevation MI leading to cardiogenic shock – is an extreme emergency. It must be treated within 3 h by PCI and angioplasty and has a survival rate of only 65 % (Berger et al. 2001).
2 Anticoagulants
2.1 Introduction
Anticoagulant therapy is an integral part of perioperative management. The mechanisms of action of currently used anticoagulant drugs are described in Fig. 8.5, and their effects on coagulation are listed in Table 8.5.
Anticoagulants and their targets (anticoagulation in the context of heparin-induced thrombocytopenia is presented in Chap. 7). Vitamin K antagonists produce their anticoagulant effect by interfering with the γ-carboxylation of the vitamin K-dependent factors II, VII, IX, and X (in black). Unfractionated heparin (UFH) is an indirect anticoagulant that binds to antithrombin (AT), enhancing its ability to inhibit activated factor X (FXa), thrombin (FIIa), and other coagulation factors. Low-molecular-weight heparins (LMWH) derived from UFH by chemical or enzymatic depolymerization and fondaparinux is a synthetic analog of the AT-binding pentasaccharide found in UFH and LMWH. Fondaparinux, too short to enable bridging between AT and thrombin, selectively potentiates the anti-FXa activity of AT. Similarly LMWHs only have a marginal impact on thrombin. Dabigatran is a direct, selective inhibitor of thrombin, hence independent of AT activity. Rivaroxaban and apixaban are direct, highly selective, factor Xa inhibitors. Clot-based assays comprise the prothrombin time (PT), the activated partial thromboplastin time (aPTT), and the thrombin time (TT). PT is used to assess the extrinsic and common pathways of coagulation. Clotting is initiated by recalcifying citrated plasma in the presence of thromboplastin (a mixture of tissue factor and phospholipids). In order to promote standardization of the PT, the World Health Organization (WHO) developed an international reference thromboplastin and recommends that the PT ratio be expressed as the International Normalized Ratio or INR to evaluate the effect of anti-vitamin K anticoagulants. aPTT is used to assess the integrity of the intrinsic coagulation pathway (prekallikrein, high-molecular-weight kininogen, factors XII, XI, IX, VIII) and final common pathway (factors II, V, X, and fibrinogen). It is performed by recalcifying citrated plasma in the presence of a thromboplastic material that does not have tissue factor activity (hence the term partial thromboplastin) and a negatively charged substance (i.e., celite, kaolin, or silica). TT measures the final step of the clotting pathway, the conversion of fibrinogen to fibrin. The test is performed by recalcifying citrated plasma in the presence of dilute bovine or human thrombin (Adapted with permission from EHM Swiss Medical Publishers Ltd. Gavillet and Angelillo-Scherrer (2012))
Patients can be prescribed prophylactic doses of anticoagulants to prevent venous thromboembolism. They can receive therapeutic doses of anticoagulants to treat or prevent recurrence of a venous thromboembolism or to prevent stroke or systemic arterial embolism in a context of atrial fibrillation, heart failure, or after the placement of prosthetic heart valves.
During the preoperative phase, the indications for anticoagulation therapy have to be confirmed in order to determine, on one hand, the thrombotic risk in case of interruption and, on the other hand, the risk of bleeding when continuing anticoagulation (Kearon et al. 2012).
Following this investigation, a detailed protocol comprising the pre-, peri-, and postoperative phases can be established. The urgency of the surgical procedure must also be taken into account when setting up of the protocol.
In this section, we will review existing anticoagulants and propose strategies for their use in a perioperative context.
2.2 Heparins and Fondaparinux
2.2.1 Introduction
Unfractionated heparin (UFH) and low-molecular-weight heparins (LMWH) are polysaccharides that bind to antithrombin (AT) and potentiate its inhibitory effect on thrombin (FIIa) and activated factor X (FXa) (Fig. 8.5). This effect varies according to the type of heparin molecule used:
-
UFH predominantly potentiates anti-IIa activity.
-
LMWHs predominantly potentiate anti-Xa activity.
Fondaparinux is a synthetic pentasaccharide that selectively binds and activates AT. It is too short a molecule to enable bridging between AT and thrombin; thus, it selectively potentiates the anti-Xa activation of AT without effecting thrombin; see Fig. 8.5 (Garcia et al. 2012).
2.2.2 Monitoring
The anticoagulant response to UFH varies between patients; it is therefore standard practice to monitor UFH and adjust the dose based on the results of coagulation tests. When administered at therapeutic doses, the anticoagulant effect of UFH is usually monitored using the activated partial thromboplastin time (aPTT). Activated clotting time (ACT) allows monitoring of the higher UFH doses given in the context of PCI or cardiac surgery. A therapeutic aPTT range of 1.5–2.5 times the control time is widely accepted (Basu et al. 1972; Garcia et al. 2012). UFH levels can also be monitored using anti-Xa assays. “Heparin resistance” is a term used when patients require unusually high doses of heparin to achieve a therapeutic aPTT (Green et al. 1994; Levine et al. 1994; Anand et al. 1997; Garcia et al. 2012). Several mechanisms explain heparin resistance: AT deficiency (Olson et al. 1998), increased UFH clearance (Hirsh et al. 1976; Green et al. 1994), high levels of heparin-binding proteins (Whitfield et al. 1983; Brey 1992), and elevated levels of FVIII (Edson et al. 1967; Levine et al. 1994) and/or fibrinogen (Edson et al. 1967).
Monitoring LMWH and fondaparinux is unnecessary, except in the contexts of obesity, renal failure, or pregnancy (Garcia et al. 2012). LMWH and fondaparinux monitoring is done by measuring the peak anti-Xa level reached 3–5 h after the subcutaneous injection of the anticoagulant. The anticoagulation is considered to be well adapted if the peak anti-Xa level is within the target range. In the context of renal failure, it is useful to measure the trough level in order to verify that the LMWH level is low enough to perform surgery without an augmented risk of bleeding. To lower the risk of prosthetic valve thrombosis in pregnant women receiving LMWH, the trough and peak anti-Xa levels can be measured to guide dose adjustments. In this context, the trough can be more useful than the peak anti-Xa level for determining an adequate baseline anticoagulant effect.
2.2.3 Reversal
Protamine sulfate is a basic protein that was originally extracted from salmon testicles. It displaces AT and neutralizes heparin by forming a complex with it, and it has a partial antagonist effect on LMWH. In the absence of heparin, protamine sulfate shows an anticoagulant effect. It is routinely used after cardiopulmonary bypass, but rarely for bleeding resulting from heparin administration. The administration of protamine sulfate can be associated with hemodynamic changes ranging from mild systemic hypotension to severe pulmonary hypertension with hemodynamic collapse. Several mechanisms can contribute to these effects: direct protamine-induced histamine release, anaphylactic reactions (IgE mediated), and anaphylactoid reactions (IgG mediated). The immune-mediated reactions can be based on anti-protamine antibodies or on anti-heparin-protamine complex antibodies. It is generally recommended to slowly administer protamine through a peripheral venous line, since central venous administration could exacerbate the adverse reactions. Three elements need to be specified in order to calculate a correct dosage:
-
1.
Route of heparin administration (subcutaneous half-life > intravenous half-life)
-
2.
Type of heparin (half-life of LMWH > half-life of UFH)
-
3.
Delay between heparin administration and protamine sulfate administration
Dosage is also based on the fact that 1 mg of protamine sulfate inactivates 100 IU of heparin or 100 IU anti-Xa of LMWH.
When the clinical setting requires the neutralization of LMWH’s anticoagulant effect, the following approach is proposed (Garcia et al. 2012):
-
If LMWH was administered within 8 h, protamine sulfate must be given at a dose of 1 mg per 100 IU of anti-Xa activity up to a maximum single dose of 50 mg (1 mg enoxaparin equals approximately 100 IU anti-Xa).
-
A second dose of 0.5 mg protamine sulfate per 100 IU anti-Xa should be provided if bleeding persists.
-
Smaller doses of protamine sulfate can be administered if the time since LMWH administration is longer than 8 h.
It is important to accurately calculate the necessary protamine dose since it has an intrinsic anticoagulant effect, which may lead to increased bleeding in case of an overdose. Fondaparinux does not bind to protamine sulfate. If uncontrollable bleeding occurs with fondaparinux, recombinant activated FVII may be effective (Bijsterveld et al. 2002).
2.3 Vitamin K Antagonists
Vitamin K antagonists (VKA) are classic oral anticoagulation drugs that generate the same effect as a vitamin K deficiency. They include phenprocoumon, warfarin, and acenocoumarol. In elective perioperative settings, these drugs are replaced by UFH, LMWH, or fondaparinux, as these periods are associated with a thromboembolic risk of 0–2 % if VKA are interrupted (Mourelo et al. 2008) and a bleeding risk of 2–25 % if VKA are continued during surgery (Jaffer et al. 2010). There are several ways to reverse the anti-vitamin K effect. For elective surgery, the patient can simply stop taking VKA with overlapping treatment of LMWH. If surgery is more urgent, but not immediate, the patient can receive a vitamin K supplement, for example, 10 mg/day of intravenous vitamin K1. Finally, for same-day urgent surgery, prothrombin complex concentrates (PCC) can be administered. For a 70 kg patient with an estimated plasma volume of 2,500 ml, the substitution dose is calculated as follows:
If the patient’s weight is significantly different, the plasma volume can be estimated according to the following formula:
For a durable reversible effect, vitamin K1 is associated with PCC. The duration of vitamin K1 administration depends on the VKA half-life.
2.4 Novel Oral Anticoagulants
2.4.1 Introduction
Novel oral anticoagulants (NOACs) specifically target either thrombin or FXa (Fig. 8.5). They have a rapid onset of action, few drug interactions, and predictable pharmacokinetics and pharmacodynamics, making routine coagulation monitoring unnecessary. However, there are situations in which assessment of the anticoagulant effect of OACs is important: these include hemorrhage or thrombosis occurring under anticoagulation, emergency surgery, polypharmacy, overdose, renal or liver failure, compliance monitoring, and extreme bodyweights. Moreover, NOACs affect routine coagulation tests (Table 8.5).
Management protocols of NOACs prior to elective surgery exist, but clinical experience is currently insufficient to provide solid guidelines on the management of emergencies including major bleeding in patients receiving NOACs. No specific antidotes are available at present.
2.4.2 Pharmacology Review
Dabigatran is a selective, competitive, reversible, direct thrombin inhibitor. It is not absorbed by the intestine and therefore given as an absorbable prodrug, dabigatran etexilate (Pradaxa™) (Ageno et al. 2012). Its oral bioavailability is low (approximately 6 %) (Stangier et al. 2007). Absorption of dabigatran etexilate is influenced by gastric pH; to optimize intestinal absorption, capsules contain tartaric acid (Connolly et al. 2009). The prodrug is converted into the active compound by plasma esterases. Peak plasma concentration is reached 1–2 h after intake. In healthy volunteers, the terminal half-life is ~9 h following a single dose and 12–17 h after repeated dosing (Stangier et al. 2007; Ageno et al. 2012). A steady-state level is reached in 2–3 days (Ageno et al. 2012). One-third of the circulating drug is bound to plasma proteins, and the drug is mainly cleared by the kidneys. Consequently, it is not recommended to administer the drug to patients with a creatinine clearance <30 ml/min. Similarly, the drug should not be prescribed to patients with severe liver failure and should be avoided in pregnant or lactating women.
Rivaroxaban (Xarelto™) specifically and competitively binds to the active site of FXa and prevents its interaction with prothrombin. Its bioavailability is high (80–100 %). Peak plasma concentrations are reached after 2–4 h after intake, and the terminal half-life is between 5 and 13 h (Kubitza et al. 2005; Weitz 2010; Ageno et al. 2012). Plasma protein binding is high (92–95 %). One-third of the drug is secreted unchanged by the kidneys, and two-thirds undergo hepatic metabolization into inactive metabolites by cytochrome P450 CYP3A4. Rivaroxaban is also a substrate of the transporter protein P-glycoprotein. Therefore, competition with other drugs for either CYP3A4 or P-glycoprotein could lead to clinically significant drug interactions. The drug should not be prescribed to patients with creatinine clearance <30 ml/min (Patel et al. 2011), to patients with severe liver dysfunction, or to pregnant or lactating women.
Apixaban (Eliquis™) is a selective, reversible, direct FXa inhibitor. This active drug has a mean bioavailability of 52 %. Plasma concentration peaks 3–4 h after intake and elimination half-life is 9–14 h (Kubitza et al. 2005; Weitz 2010; Ageno et al. 2012). Plasma protein binding is high (about 87 %). Apixaban is eliminated by oxidative metabolism and renal (27 %) and intestinal routes (Zhang et al. 2009). Similarly to rivaroxaban, any drug interfering with either CYP3A4 or P-glycoprotein could lead to a clinically significant drug interaction. Apixaban should not be prescribed to patients with severe renal (creatinine clearance <15 ml/min) or hepatic failure. It should be avoided in pregnant or lactating women.
2.4.3 Reversal Prior to Elective Surgery
The reversal strategy for dabigatran should take into account renal function. Creatinine needs to be checked – and the creatinine clearance calculated – several days before elective surgery. The interruption protocol for dabigatran further takes into account bleeding risk and type of surgery (Table 8.6). Thrombin time should be measured 6–12 h before surgery in patients at high risk of bleeding or if major surgery is planned (van Ryn et al. 2010). A normal result would exclude any residual anticoagulant effect of dabigatran. If the thrombin time is prolonged, specific tests should be performed to assess dabigatran concentration (Stangier et al. 2007). Hemodialysis might be considered in patients with severe renal impairment and persistently elevated dabigatran plasma concentrations (van Ryn et al. 2010).
For the direct FXa inhibitors, considering their short half-life, cessation of medication may be sufficient to reverse the anticoagulant effect. However, we suggest checking renal function and slightly modify the reversal protocol in case of renal failure (Table 8.6). Reversal can be monitored by measuring anti-FXa activity (specific assays) (Barrett et al. 2010; Samama et al. 2012).
2.4.4 Reversal in an Emergency
There is no evidence-based strategy for emergency reversal of NOACs (Pengo et al. 2011; Ageno et al. 2012). In case of major bleeding, general measures comprise the following: the discontinuation of the NOAC; the initiation of appropriate clinical support, including mechanical compression and local as well as surgical hemostasis; blood product transfusion; volume substitution; inotropic drugs; and maintenance of adequate diuresis (Table 8.7). Transfusion of platelet concentrates might be proposed if thrombocytopenia is present or in case antiplatelet drugs have been administered. If the initial support described above is insufficient, PCCs, recombinant FVIIa, or FEIBA™ (factor eight inhibitor bypass activity) might be infused empirically in cases of life-threatening bleeding or emergency surgery (Table 8.7). The decision to administrate these products should be based upon the clinical situation and not on laboratory tests. It is important to realize that these products are highly prothrombotic and that their administration might be complicated by thrombotic events. Their use should therefore be limited to life-threatening situations. For dabigatran, reversal can be monitored by measuring the thrombin time (see Sect. 8.2.4.3). However, because this test is highly sensitive to dabigatran, an assessment of its concentration by specific tests would be more accurate (Stangier et al. 2007). For anti-Xa drugs, reversal can be monitored by measuring anti-Xa activity (Barrett et al. 2010; Samama et al. 2012). Hemodialysis could complete the reversal strategy for dabigatran (Warkentin et al. 2012).
2.5 Vena Cava Filters
The use of inferior vena cava filter is recommended in patients with acute proximal deep vein thrombosis and/or pulmonary embolism who have a contraindication to anticoagulants, i.e., an unacceptable risk of bleeding (Garcia et al. 2012). If the contraindication to anticoagulation is temporary (e.g., during active bleeding), it is possible to insert a temporary retrievable filter and remove it when anticoagulation treatment can be safely restarted. However, it is worth noting that most retrievable filters are not removed (Mismetti et al. 2007; Dabbagh et al. 2010; Jaff et al. 2011; Garcia et al. 2012). Furthermore, retrievable filters that do not get removed might display a higher complication rate than permanent filters (Mismetti et al. 2007, p 223; Dabbagh et al. 2010, p 493; Nicholson et al. 2010, p 1827).
Insertion of an inferior vena cava filter does not eliminate the risk of pulmonary embolism and does increase the risk of deep vein thrombosis. Consequently, it is suggested that patients who have an inferior vena cava filter inserted should receive a conventional course of anticoagulants when the contraindication to anticoagulation is withdrawn (Garcia et al. 2012). Venous thrombosis at the site of filter insertion occurs in about 10 % of patients (Streiff 2000).
References
Ageno W, Gallus AS et al (2012) Oral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e44S–e88S
Albaladejo P, Marret E et al (2011) Non-cardiac surgery in patients with coronary stents: the RECO study. Heart 97(19):1566–1572
American Society of Anesthesiologists Task Force on Neuraxial Opioids, Horlocker TT et al (2009) Practice guidelines for the prevention, detection, and management of respiratory depression associated with neuraxial opioid administration. Anesthesiology 110(2):218–230
Anand SS, Brimble S et al (1997) Management of iliofemoral thrombosis in a pregnant patient with heparin resistance. Arch Intern Med 157(7):815–816
Angiolillo DJ, Firstenberg MS et al (2012) Bridging antiplatelet therapy with cangrelor in patients undergoing cardiac surgery: a randomized controlled trial. JAMA 307(3):265–274
Aradi D, Komocsi A et al (2010) Prognostic significance of high on-clopidogrel platelet reactivity after percutaneous coronary intervention: systematic review and meta-analysis. Am Heart J 160(3):543–551
Artang R, Dieter RS (2007) Analysis of 36 reported cases of late thrombosis in drug-eluting stents placed in coronary arteries. Am J Cardiol 99(8):1039–1043
Asmis LM, Alberio L et al (2012) Rivaroxaban: Quantification by anti-FXa assay and influence on coagulation tests: a study in 9 Swiss laboratories. Thromb Res 129(4):492–498
Barash P, Akhtar S (2010) Coronary stents: factors contributing to perioperative major adverse cardiovascular events. Br J Anaesth 105(Suppl 1):i3–i15
Barrett YC, Wang Z et al (2010) Clinical laboratory measurement of direct factor Xa inhibitors: anti-Xa assay is preferable to prothrombin time assay. Thromb Haemost 104(6):1263–1271
Basu D, Gallus A et al (1972) A prospective study of the value of monitoring heparin treatment with the activated partial thromboplastin time. N Engl J Med 287(7):324–327
Bates ER, Lau WC et al (2011) Clopidogrel-drug interactions. J Am Coll Cardiol 57(11):1251–1263
Berger PB, Bellot V et al (2001) An immediate invasive strategy for the treatment of acute myocardial infarction early after noncardiac surgery. Am J Cardiol 87(9):1100–1102, A1106, A1109
Bhatt DL, Fox KA et al (2006) Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med 354(16):1706–1717
Bijsterveld NR, Moons AH et al (2002) Ability of recombinant factor VIIa to reverse the anticoagulant effect of the pentasaccharide fondaparinux in healthy volunteers. Circulation 106(20):2550–2554
Biondi-Zoccai GG, Lotrionte M et al (2006) A systematic review and meta-analysis on the hazards of discontinuing or not adhering to aspirin among 50,279 patients at risk for coronary artery disease. Eur Heart J 27(22):2667–2674
Brey RL (1992) Antiphospholipid antibodies and ischemic stroke. Heart Dis Stroke 1(6):379–382
Burger W, Chemnitius JM et al (2005) Low-dose aspirin for secondary cardiovascular prevention – cardiovascular risks after its perioperative withdrawal versus bleeding risks with its continuation – review and meta-analysis. J Intern Med 257(5):399–414
Chassot PG, Delabays A et al (2007) Perioperative antiplatelet therapy: the case for continuing therapy in patients at risk of myocardial infarction. Br J Anaesth 99(3):316–328
Chassot PG, Marcucci C et al (2010) Perioperative antiplatelet therapy. Am Fam Physician 82(12):1484–1489
Chernoguz A, Telem DA et al (2011) Cessation of clopidogrel before major abdominal procedures. Arch Surg 146(3):334–339
Connolly SJ, Ezekowitz MD et al (2009) Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 361(12):1139–1151
Dabbagh O, Nagam N et al (2010) Retrievable inferior vena cava filters are not getting retrieved: where is the gap? Thromb Res 126(6):493–497
Dangas GD, Caixeta A et al (2011) Frequency and predictors of stent thrombosis after percutaneous coronary intervention in acute myocardial infarction. Circulation 123(16):1745–1756
Douketis JD, Berger PB et al (2008) The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133(6 Suppl):299S–339S
Eberli D, Chassot PG et al (2010) Urological surgery and antiplatelet drugs after cardiac and cerebrovascular accidents. J Urol 183(6):2128–2136
Edson JR, Krivit W et al (1967) Kaolin partial thromboplastin time: high levels of procoagulants producing short clotting times or masking deficiencies of other procoagulants or low concentrations of anticoagulants. J Lab Clin Med 70(3):463–470
Eerenberg ES, Kamphuisen PW et al (2011) Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation 124(14):1573–1579
Eisenberg MJ, Richard PR et al (2009) Safety of short-term discontinuation of antiplatelet therapy in patients with drug-eluting stents. Circulation 119(12):1634–1642
Fujimoto H, Ishimura R et al (2009) Two cases of acute coronary syndrome that occurred by preoperative discontinuation of antiplatelet therapy in the chronic phase after stent implantation. J Cardiol 54(3):470–474
Gaglia MA Jr, Waksman R (2011) Systematic review of thienopyridine discontinuation and its impact upon clinical outcomes. Eur Heart J 32(19):2358–2364
Garcia DA, Baglin TP et al (2012) Parenteral anticoagulants: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e24S–e43S
Gavillet M, Angelillo-Scherrer A (2012) Quantification of the anticoagulatory effect of novel anticoagulants and management of emergencies. Cardiovasc Med 15(5):170–179
Gogarten W, Vandermeulen E et al (2010) Regional anaesthesia and antithrombotic agents: recommendations of the European Society of Anaesthesiology. Eur J Anaesthesiol 27(12):999–1015
Green D, Hirsh J et al (1994) Low molecular weight heparin: a critical analysis of clinical trials. Pharmacol Rev 46(1):89–109
Gurbel PA, Bliden KP et al (2009) Randomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: the ONSET/OFFSET study. Circulation 120(25):2577–2585
Hall R, Mazer CD (2011) Antiplatelet drugs: a review of their pharmacology and management in the perioperative period. Anesth Analg 112(2):292–318
Hirsh J, van Aken WG et al (1976) Heparin kinetics in venous thrombosis and pulmonary embolism. Circulation 53(4):691–695
Jaff MR, McMurtry MS et al (2011) Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation 123(16):1788–1830
Jaffer AK, Brotman DJ et al (2010) Variations in perioperative warfarin management: outcomes and practice patterns at nine hospitals. Am J Med 123(2):141–150
Joner M, Finn AV et al (2006) Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J Am Coll Cardiol 48(1):193–202
Kearon C, Akl EA et al (2012) Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e419S–e494S
Korte W, Cattaneo M et al (2011) Peri-operative management of antiplatelet therapy in patients with coronary artery disease: joint position paper by members of the working group on Perioperative Haemostasis of the Society on Thrombosis and Haemostasis Research (GTH), the working group on Perioperative Coagulation of the Austrian Society for Anesthesiology, Resuscitation and Intensive Care (OGARI) and the Working Group Thrombosis of the European Society for Cardiology (ESC). Thromb Haemost 105(5):743–749
Kubitza D, Becka M et al (2005) Safety, pharmacodynamics, and pharmacokinetics of single doses of BAY 59-7939, an oral, direct factor Xa inhibitor. Clin Pharmacol Ther 78(4):412–421
Levine MN, Hirsh J et al (1994) A randomized trial comparing activated thromboplastin time with heparin assay in patients with acute venous thromboembolism requiring large daily doses of heparin. Arch Intern Med 154(1):49–56
Mega JL, Simon T et al (2010) Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis. JAMA 304(16):1821–1830
Mismetti P, Rivron-Guillot K et al (2007) A prospective long-term study of 220 patients with a retrievable vena cava filter for secondary prevention of venous thromboembolism. Chest 131(1):223–229
Moore M, Power M (2004) Perioperative hemorrhage and combined clopidogrel and aspirin therapy. Anesthesiology 101(3):792–794
Mourelo R, Kaidar-Person O et al (2008) Hemorrhagic and thromboembolic complications after bariatric surgery in patients receiving chronic anticoagulation therapy. Obes Surg 18(2):167–170
Nicholson W, Nicholson WJ et al (2010) Prevalence of fracture and fragment embolization of Bard retrievable vena cava filters and clinical implications including cardiac perforation and tamponade. Arch Intern Med 170(20):1827–1831
Nuttall GA, Brown MJ et al (2008) Time and cardiac risk of surgery after bare-metal stent percutaneous coronary intervention. Anesthesiology 109(4):588–595
Olson JD, Arkin CF et al (1998) College of American Pathologists Conference XXXI on laboratory monitoring of anticoagulant therapy: laboratory monitoring of unfractionated heparin therapy. Arch Pathol Lab Med 122(9):782–798
Patel MR, Mahaffey KW et al (2011) Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med 365(10):883–891
Patrono C, Rocca B (2010) The future of antiplatelet therapy in cardiovascular disease. Annu Rev Med 61:49–61
Pengo V, Crippa L et al (2011) Questions and answers on the use of dabigatran and perspectives on the use of other new oral anticoagulants in patients with atrial fibrillation. A consensus document of the Italian Federation of Thrombosis Centers (FCSA). Thromb Haemost 106(5):868–876
Pharma BS (2009) Xarelto. Summary of product characteristics. www.xarelto.com/html/downloads/Xarelto_Summary_of_Product_Characteristics_May2009.pdf. Accessed Mar 2011
Price MJ (2009) Bedside evaluation of thienopyridine antiplatelet therapy. Circulation 119(19):2625–2632
Rabbitts JA, Nuttall GA et al (2008) Cardiac risk of noncardiac surgery after percutaneous coronary intervention with drug-eluting stents. Anesthesiology 109(4):596–604
Samama MM, Contant G et al (2012) Evaluation of the anti-factor Xa chromogenic assay for the measurement of rivaroxaban plasma concentrations using calibrators and controls. Thromb Haemost 107(2):379–387
Savonitto S, D’Urbano M et al (2010) Urgent surgery in patients with a recently implanted coronary drug-eluting stent: a phase II study of ‘bridging’ antiplatelet therapy with tirofiban during temporary withdrawal of clopidogrel. Br J Anaesth 104(3):285–291
Schouten O, van Domburg RT et al (2007) Noncardiac surgery after coronary stenting: early surgery and interruption of antiplatelet therapy are associated with an increase in major adverse cardiac events. J Am Coll Cardiol 49(1):122–124
Schulz S, Schuster T et al (2009) Stent thrombosis after drug-eluting stent implantation: incidence, timing, and relation to discontinuation of clopidogrel therapy over a 4-year period. Eur Heart J 30(22):2714–2721
Sharma AK, Ajani AE et al (2004) Major noncardiac surgery following coronary stenting: when is it safe to operate? Catheter Cardiovasc Interv 63(2):141–145
Stangier J, Rathgen K et al (2007) The pharmacokinetics, pharmacodynamics and tolerability of dabigatran etexilate, a new oral direct thrombin inhibitor, in healthy male subjects. Br J Clin Pharmacol 64(3):292–303
Streiff MB (2000) Vena caval filters: a comprehensive review. Blood 95(12):3669–3677
Task Force on Myocardial Revascularization of the European Society of, Cardiology; The European Association for Cardio-Thoracic Surgery; et al (2010) Guidelines on myocardial revascularization. Eur Heart J 31(20):2501–2555
Taylor K, Filgate R et al (2011) A retrospective study to assess the morbidity associated with transurethral prostatectomy in patients on antiplatelet or anticoagulant drugs. BJU Int 108(Suppl 2):45–50
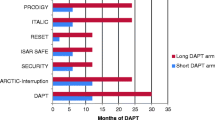
Valgimigli M, Campo G et al (2012) Short- versus long-term duration of dual-antiplatelet therapy after coronary stenting: a randomized multicenter trial. Circulation 125(16):2015–2026
van Ryn J, Stangier J et al (2010) Dabigatran etexilate–a novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity. Thromb Haemost 103(6):1116–1127
Wallentin L, Becker RC et al (2009) Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 361(11):1045–1057
Warkentin TE, Margetts P et al (2012) Recombinant factor VIIa (rFVIIa) and hemodialysis to manage massive dabigatran-associated postcardiac surgery bleeding. Blood 119(9):2172–2174
Weitz JI (2010) New oral anticoagulants in development. Thromb Haemost 103(1):62–70
Whitfield LR, Lele AS et al (1983) Effect of pregnancy on the relationship between concentration and anticoagulant action of heparin. Clin Pharmacol Ther 34(1):23–28
Wilson SH, Fasseas P et al (2003) Clinical outcome of patients undergoing non-cardiac surgery in the two months following coronary stenting. J Am Coll Cardiol 42(2):234–240
Wiviott SD, Braunwald E et al (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357(20):2001–2015
Zhang D, He K et al (2009) Comparative metabolism of 14C-labeled apixaban in mice, rats, rabbits, dogs, and humans. Drug Metab Dispos 37(8):1738–1748
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Chassot, PG., Barelli, S., Blum, S., Angelillo-Scherrer, A., Marcucci, C.E. (2015). Antiplatelet Therapy and Anticoagulation. In: Marcucci, C., Schoettker, P. (eds) Perioperative Hemostasis. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-55004-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-642-55004-1_8
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-55003-4
Online ISBN: 978-3-642-55004-1
eBook Packages: MedicineMedicine (R0)