Abstract
The majority of patients undergoing cardiac surgery use antiplatelet agents, such as aspirin, ADP receptor inhibitors, and/or glycoprotein IIb/IIIa receptor inhibitors. An increasing number of patients use dual antiplatelet therapy. Due to the higher bleeding risk in the presence of antiplatelet agents, every individual patient requires a balanced estimation of the bleeding risks in case of continuation and thrombotic risks in case of cessation. This chapter describes different antiplatelet drugs, and the aspects that have to be considered for continuation or discontinuation of these agents before cardiac surgery.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Case VignetteA 64-year-old man recently suffered an ST elevation myocardial infarction and underwent percutaneous coronary angioplasty. During the procedure, multiple lesions in all three main coronary arteries were noted. However, only one drug-eluting stent could be placed in the circumflex artery and the patient was started on aspirin and the thienopyridine prasugrel to prevent stent thrombosis. He was then referred for urgent coronary artery bypass grafting to revascularize the remaining affected coronary arteries. The treating physician discussed whether to continue or discontinue aspirin and prasugrel during a multidisciplinary team consult. The team concluded that prasugrel should be discontinued, but there was no consensus regarding the time of discontinuation and whether bridging therapy is required.
Why Is It Important?
Platelets are a vital component of blood involved in hemostasis. They are activated and mediated by a number of mechanisms. Endothelial damage or rupture of an atherosclerotic plaque activates, adheres, and aggregates platelets to allow hemostasis until tissue repair is completed.
Although these processes are part of normal physiological function, amplification and excessive thrombus formation impede vascular flow. Occlusion of blood at regions narrowed by atherosclerotic plaques can lead to tissue ischemia and damage. Antiplatelet agents are a cornerstone of preventing or reducing such events. However, blocking platelet function during surgery delays hemostasis and increases the risk of bleeding. This chapter focuses on the mechanistic action of antiplatelet drugs, how to manage these in the perioperative setting and whether to bridge patients in case of antiplatelet drug discontinuation.
Platelet Function
Platelet involvement in coagulation is termed primary hemostasis, whereas secondary hemostasis is mediated by the coagulation proteins leading to fibrin formation. Primary hemostasis involves a number of proteins and interactions and occurs very quickly. However, it can be divided into three stages occurring rapidly in succession.
Initial tissue damage exposes the collagen fibers making up the endothelium. Collagen glycoprotein (GP) Ia/IIa surface receptors anchor passing platelets by interacting through von Willebrand factor (vWF) that is secreted by the endothelium and binds to GPIb receptors forming a complex with GPIX and GPV on platelets.
In the absence of tissue damage, platelets are inhibited by endothelial produced nitric oxide, ADPase, and prostacyclin (PGI2). Platelet intracellular calcium is maintained at low levels by a cyclic-AMP mediated calcium pump. Activation of platelets occurs from multiple sources:
-
ADP binding to the purinergic receptors P2Y1 and P2Y12, on the platelet surface.
-
Tissue factor (TF) release from endothelial damage activating factor VII and in turn thrombin, which acts directly on platelets.
This increases the net intracellular calcium, which in turn activates the platelet.
Activated platelets increase the production of thromboxane A2, which activates glycoprotein IIb/IIIa receptors on their own and neighboring platelets, which leads to aggregation. Activated platelets also degranulate, secreting chemotactic agents that attract more platelets to the site of endothelial injury. Activated platelets gather at the site of endothelial injury. The activated glycoproteins IIb/IIIa surface receptors bind to vWF and fibrinogen, thereby anchoring activated platelets to endothelial collagen. The binding to fibrinogen allows platelet cross-linking and hence aggregation.
Mechanisms
Cyclooxygenase Pathway
The enzyme cyclooxygenase (COX) converts arachidonic acid, a fatty acid in cell membranes, to prostaglandins, prostacyclins, and thromboxanes. These are important biological molecules involved in pain, inflammation, and coagulation. There are two forms: COX-1 and COX-2. With COX-1 being a constitutive enzyme that is continuously active and COX-2 being an inducible enzyme that is activated by inflammation or tissue damage (Fig. 6.1).
Aspirin is an irreversible inhibitor of COX-1 and COX-2 . By blocking COX-1, the conversion of arachidonic acid to prostaglandin H2 is blocked, and therefore, its conversion to thromboxane A2 and prostaglandin I2 is also hindered. Thromboxane A2 is the main eicosanoid involved in platelet aggregation as described earlier, while prostaglandin I2 is produced by endothelial cells and has anti-thrombotic actions [1]. As said, the effect of aspirin on platelets is permanent, and the antiplatelet effect wears off after 7 days once new platelets are synthesized. The antiplatelet effect occurs at low doses (75–150 mg) with mostly COX-1 inhibition, while the anti-inflammatory and analgesic effects, mediated mainly by COX-2 inhibition, occur at higher doses (150–325 mg).
Platelet Surface Receptors
The numerous receptors on the platelet surface are mostly involved in activation, anchoring, and maintenance of platelet aggregation, albeit that not all their functions are yet understood. There are multiple antiplatelet drugs produced that specifically target one or two of these receptors. Receptors not yet targeted continue to provide important potential avenues of research in targeted drug development. The most commonly known receptors are the ADP receptors, glycoprotein IIb/IIIa receptors, phosphodiesterase, and protease activated receptors.
ADP receptors are expressed on the platelet surface, and binding results in platelet activation through a conformational change, platelet aggregation, and interaction with other cell surface and plasma receptors and compounds. Blocking ADP binding to the receptor has antiplatelet aggregation effects [2]. ADP receptors are part of the larger purinergic G-protein couple receptor family, and the specific receptors on the platelet surface are termed P2Y1 and P2Y12 receptors. P2Y1 receptors initiate platelet aggregation, whereas P2Y12 receptors amplify and complete aggregation. Therefore, both receptors need to be activated for aggregation to occur. Agents developed to block these receptors have focused on the P2Y12 receptor and are termed ADP receptor inhibitors or P2Y12 receptor antagonists [1]. Drugs currently in clinical use are clopidogrel, prasugrel, ticagrelor, and the more recently approved cangrelor [3].
Glycoprotein IIb/IIIa receptors are the most important receptors on the platelet surface, as they are activated by vWF and fibrinogen. Binding of vWF allows anchorage of platelets to the endothelium and the attraction of other platelets. The binding of fibrinogen allows crosslink formation and platelet aggregation through platelet–fibrin complexes. Activated glycoprotein IIb/IIIa receptors also have effects on thrombin and collagen to continue the prothrombotic effect [4]. Inhibition of these receptors has an antiplatelet effect. The agents currently in use are abciximab, tirofiban, and eptifibatide.
Indications
Antiplatelet drugs are primarily used in the context of prevention of morbidity from coronary artery disease. However, indications for their use differ between agents.
Aspirin
Multiple trials have shown that aspirin as primary prevention taken daily at doses of 75–325 mg reduces the risk of myocardial infarction (MI) by 36–44% [1]. This was questioned from a safety perspective [5], but daily aspirin at low doses (75–150 mg) is still recommended in patients with low risk of gastrointestinal or intracranial hemorrhage.
Aspirin is routinely used after MI and revascularization interventions. Aspirin given within 24 h after a MI reduces the likelihood of reinfarction and mortality. In patients diagnosed with acute coronary syndromes or unstable angina, guidelines recommend that aspirin be given prior to a percutaneous coronary intervention or thrombolysis and continued indefinitely [6]. This reduces the rates of stent thrombosis and mortality. Aspirin is also given as part of a dual antiplatelet therapy (DAPT) regime at low doses. After CABG, the use of aspirin improves graft patency and reduces mortality from MI, stroke, and renal failure [7, 8].
ADP Receptor Inhibitors
In patients presenting with an acute coronary syndrome or unstable angina, ADP receptor inhibitors are recommended by most guidelines. Patients who undergo a percutaneous coronary intervention and have stents are required to take ADP receptor inhibitors in combination with aspirin (DAPT). Recent guidelines have made a number of recommendations in this context [9,10,11,12]. Patients who receive bare-metal stents and are at low risk of bleeding should have DAPT for 4–6 weeks, whereas patients receiving drug-eluting stents should take DAPT for 6 months. Where there is increased risk of stent thrombosis, DAPT treatment should be increased to 12 months.
ADP receptor inhibitors tend to be used with low dose aspirin. The CURE trial found that aspirin with clopidogrel is superior to aspirin alone in patients with an acute coronary syndrome. This reduces major cardiac events and also reduces hemorrhagic side effects from higher dose aspirin [13].
ADP receptor inhibitors are also used in peripheral arterial disease to prevent thrombotic events and improve flow. They are also used as alternatives in ischemic strokes associated with carotid or vertebral artery dissections. ADP receptor inhibitors are also used as alternatives to warfarin in atrial fibrillation where warfarin is contraindicated.
Glycoprotein IIb/IIIa Receptor Inhibitors
Glycoprotein IIb/IIIa receptor inhibitors agents are given intravenously to have a quick onset of effect. Therefore, their use is mainly in the context of percutaneous coronary interventions or acute MI. A meta-analysis of 21 studies has shown that the use of glycoprotein IIb/IIIa receptor inhibitors in patients undergoing coronary interventions reduces the combined endpoint of death, non-fatal MI, or urgent revascularization at 30 days [14]. It is therefore recommended to use glycoprotein IIb/IIIa inhibitors in combination with aspirin and heparin for those medically managed or undergoing intervention for acute MI [15]. Specifically, for patients undergoing coronary interventions, initiation of therapy with heparin and abciximab, high-dose tirofiban/eptifibatide [15], or cangrelor, an intravenous and ultra-short acting ADP-receptor blocker is recommended [16].
Risks
Aspirin
Evidence shows that the antiplatelet effect increases up to 75–81 mg dosage, with higher doses increasing the gastrointestinal or intracranial bleeding risk without increasing benefit [17]. In particular, a review of 22 trials found that low-dose aspirin doubles the risk of gastrointestinal and intracranial bleeding compared to placebo [18]. A meta-analysis of 16 trials showed that aspirin increases the risk of hemorrhagic stroke despite favorable effects on ischemic stroke and MI [19]. In patients undergoing a non-cardiac surgical intervention, aspirin use is not associated with major bleeding events [20]. However, in cardiac surgery, there is increased postoperative bleeding that however does not require reoperation when aspirin is continued [21].
ADP Receptor Inhibitors
ADP receptor inhibitors are associated with an increased bleeding risk, but compared with aspirin the gastrointestinal-related side effects are lower. The addition of clopidogrel to aspirin therapy in patients with coronary syndromes increases the risk of bleeding, but fatal bleeding rates remain similar [13]. More importantly, in patients undergoing CABG surgery, a meta-analysis found that clopidogrel use within 7 days preceding the intervention was associated with an increased risk of major bleeding and related complications, requiring re-exploration and transfusions [22]. In patients with an acute coronary syndrome, ticagrelor reduced the rate of death from prothrombotic causes compared to clopidogrel without an increase in the rate of overall major bleeding but with an increase in the rate of non-procedure-related bleeding [23]. However, patients on aspirin with ticagrelor have a stronger trend towards bleeding when ticagrelor is stopped only 1 day prior to surgery than patients on aspirin with clopidogrel [24].
Glycoprotein IIb/IIIa Receptor Inhibitors
Glycoprotein IIb/IIIa receptor inhibitors significantly increase the risk of bleeding compared with placebo [25]. However, the risk of bleeding is comparable to the use of heparin, in particular with respect to the rates of intracranial hemorrhage when used as single antiplatelet therapy [26].
Perioperative Use and Management
The use of antiplatelet drugs during cardiac and non-cardiac surgery increases the risk of perioperative bleeding, as previously indicated. However, the cessation of antiplatelet agents before surgery increases the risk of perioperative MI, stroke, stent occlusion, and even death from rebound pro-inflammatory effects. To ensure minimal risk for bleeding or life-threatening thrombosis, a risk evaluation and interdisciplinary management plan needs to be agreed upon before surgery.
Bleeding Risk
The bleeding risk varies according to the antiplatelet agents used, and whether dual antiplatelet therapy is being used. In a review it was stated that the risk of bleeding with continued use of antiplatelets is 30–50% compared with 2.5–20% in patients without antiplatelet drugs, and a 30% higher transfusion rate [4]. Given these risks, one should outweigh whether it is safe to plan surgery, or to delay surgery such that antiplatelet drugs can be discontinued. Moreover, in case of urgent surgery, the risk of bleeding due to antiplatelet therapy should be quantified. Surgeries are classed as low, intermediate, or high risk of bleeding depending on the vasculature involved and the transfusion requirements.
Cardiac surgery is classified as an intermediate risk of bleeding, but most patients will be on at least aspirin for primary prevention of cardiac ischemia. A sizeable portion of patients will be taking dual antiplatelet agents for secondary prevention after a previous cardiac event or intervention. Other factors that increase the bleeding risk are described in a previous chapter [27].
Recent European guidelines provided multiple recommendations on antiplatelet drug use in cardiac surgery [12, 28]. They recommend continuing aspirin unless the patient is at particularly high risk of bleeding, in which case, aspirin should be stopped at least 5 days before surgery. For patients on DAPT, ticagrelor, clopidogrel, and prasugrel should be stopped 3, 5, and 7 days prior to surgery, respectively. GPIIb/IIIa inhibitors should be discontinued at least 4 h prior to surgery. Obviously, in emergency surgery you should proceed to surgery and anticipate the higher risk of bleeding.
Thrombotic Risk
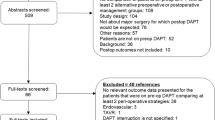
The thrombotic risk of cessation of antiplatelet therapy before cardiac surgery depends on the initial indication for antiplatelet use and the current cardiovascular status of the patient. Most patients will be taking antiplatelet agents for either primary or secondary prevention of cardiovascular disease, or cerebrovascular disease or peripheral vascular disease. However, patients that will present the greatest challenge will be those taking DAPT for secondary prevention of further ischemic cardiac events, especially following coronary stent implantation. Discontinuing these agents before surgery increases the risk for thrombosis from rebound platelet activation. In the context of coronary stents, thrombosis may occur within stents, leading to potential stent failure and myocardial ischemia. Figure 6.2 shows the considerations that need to be made before DAPT discontinuation. The thrombotic risk of cessation of aspirin is lower than for DAPT.
These factors then need to be considered in those undergoing cardiac surgery. If a stent has not been inserted, surgery will address coronary ischemia. However, if the stented vessels are not being addressed, then the risk of thrombosis from discontinuing DAPT needs to be considered. DAPT has also been shown to improve graft patency in patients undergoing coronary artery bypass surgery. Therefore, the ACC/AHA guidelines recommend DAPT postoperatively for 12 months [9].
European guidelines recommend bridging therapy for patients at high risk of thrombosis, including patients with mechanical heart valves, atrial fibrillation with rheumatic heart disease, an acute thrombotic event in the previous 4 weeks, and/or atrial fibrillation with a CHA2DS2Vasc score of >4. Most of these patients will be on other anticoagulants, and bridging therapy will therefore consist of unfractionated or low-molecular weight heparins, cangrelor, or glycoprotein IIb/IIIa inhibitors.
Implications for Daily Practice
Antiplatelet drug use is common given the number of indications and the benefit of their use. However, their use perioperatively carries the risk of bleeding if continued intra-operatively and thrombosis if discontinued before surgery. These risks are amplified during dual antiplatelet therapy.
Bridging therapy can include short-acting antiplatelet agents, such as tirofiban and eptifibatide. Antiplatelet agents have transformed the treatment of acute coronary syndromes and the postoperative management of coronary artery bypass graft patients. Appropriate use must be balanced by the risk of thrombosis versus hemorrhage and side effects. Devices such as platelet aggregometry exist to measure platelet inhibition levels, and might be used to assess the risk of individual patients. The correct timing for when to stop and restart therapy is discussed in the next chapters.
References
Oprea AD, Popescu WM. Perioperative management of antiplatelet therapy. Br J Anaesth. 2013;111:i3–i17.
Davì G, Patrono C. Platelet activation and atherothrombosis. N Engl J Med. 2007;357:2482–94.
Kubica J, Kozinski M, Navarese EP, et al. Cangrelor: an emerging therapeutic option for patients with coronary artery disease. Curr Med Res Opin. 2014;30:813–28.
Koenig-Oberhuber V, Filipovic M. New antiplatelet drugs and new oral anticoagulants. Br J Anaesth. 2016;117:ii74–84.
Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373:1849–60.
O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:485–510.
Mangano DT, Multicenter Study of Perioperative Ischemia Research Group. Aspirin and mortality from coronary bypass surgery. N Engl J Med. 2002;347:1309–17.
Goldman S, Copeland J, Moritz T, et al. Improvement in early saphenous vein graft patency after coronary artery bypass surgery with antiplatelet therapy: results of a Veterans Administration Cooperative Study. Circulation. 1988;77:1324–32.
Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Thorac Cardiovasc Surg. 2016;152:1243–75.
Douketis JD, Spyropoulos AC, Spencer FA, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e326–50.
Wijns W, Kolh P, Danchin N, et al. Guidelines on myocardial revascularization. Eur Heart J. 2010;31:2501–55.
Boer C, Meesters MI, Milojevic M, et al. 2017 EACTS/EACTA guidelines on patient blood management for adult cardiac surgery. J Cardiothorac Vasc Anesth. 2017;25:1–34.
Yusuf S, Zhao F, Mehta SR, Chrolavicius S, Tognoni G, Fox KK, Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001;345:494–502.
Sabatine MS, Jang IK. The use of glycoprotein IIb/IIIa inhibitors in patients with coronary artery disease. Am J Med. 2000;109:224–37.
Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery: executive summary: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Anesth Analg. 2012;114:11–72.
Bhatt DL, Stone GW, Mahaffey KW, et al. Effect of platelet inhibition with cangrelor during PCI on ischemic events. N Engl J Med. 2013;368:1303–13.
Campbell CL, Smyth S, Montalescot G, Steinhubl SR. Aspirin dose for the prevention of cardiovascular disease: a systematic review. J Am Med Assoc. 2007;297:2018–24.
McQuaid KR, Laine L. Systematic review and meta-analysis of adverse events of low-dose aspirin and clopidogrel in randomized controlled trials. Am J Med. 2006;119:624–38.
He J, Whelton PK, Vu B, Klag MJ. Aspirin and risk of hemorrhagic stroke: a meta-analysis of randomized controlled trials. J Am Med Assoc. 1998;280:1930–5.
Mantz J, Samama CM, Tubach F, et al. Impact of preoperative maintenance or interruption of aspirin on thrombotic and bleeding events after elective non-cardiac surgery: the multicentre, randomized, blinded, placebo-controlled, STRATAGEM trial. Br J Anaesth. 2011;107:899–910.
Alghamdi AA, Moussa F, Fremes SE. Does the use of preoperative aspirin increase the risk of bleeding in patients undergoing coronary artery bypass grafting surgery? Systematic review and meta-analysis. J Card Surg. 2007;22:247–56.
Pickard AS, Becker RC, Schumock GT, Frye CB. Clopidogrel-associated bleeding and related complications in patients undergoing coronary artery bypass grafting. Pharmacotherapy. 2008;28:376–92.
Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045–57.
Hansson EC, Jidéus L, Åberg B, et al. Coronary artery bypass grafting-related bleeding complications in patients treated with ticagrelor or clopidogrel: a nationwide study. Eur Heart J. 2016;37:189–97.
PURSUIT Trial Investigators. Platelet glycoprotein IIb/IIIa in unstable angina: receptor suppression using integrilin therapy. N Engl J Med. 1998;339:436–43.
Memon MA, Blankenship JC, Wood GC, Frey CM, Menapace FJ. Incidence of intracranial hemorrhage complicating treatment with glycoprotein IIb/IIIa receptor inhibitors: a pooled analysis of major clinical trials. Am J Med. 2000;109:213–7.
Stawiarski K, Kataria R, Bravo CA, et al. Dual-antiplatelet therapy guidelines and implications for perioperative management. J Cardiothorac Vasc Anesth. 2018;32:1072–80.
Kozek-Langenecker SA, Ahmed AB, Afshari A, et al. Management of severe perioperative bleeding: guidelines from the European Society of Anaesthesiology: first update 2016. Eur J Anaesthesiol. 2017;34:332–95.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ahmed, A., Majeed, A. (2019). Antiplatelet Drug Management. In: von Heymann, C., Boer, C. (eds) Patient Blood Management in Cardiac Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-15342-7_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-15342-7_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-15341-0
Online ISBN: 978-3-030-15342-7
eBook Packages: MedicineMedicine (R0)