Abstract
Patients with temporomandibular joint (TMJ) pathology and coexisting dentofacial deformities can be corrected with concomitant TMJ and orthognathic surgery (C-TMJ-OS) in one surgical stage or separated into two surgical stages. The two-stage approach requires the patient to undergo two separate operations (one surgery to correct the TMJ pathology and a second operation to perform the orthognathic surgery) and two general anesthetics significantly lengthening the overall treatment time. Performing C-TMJ-OS in a single operation significantly decreases treatment time, provides better outcomes, but requires careful treatment planning and surgical proficiency in the two surgical areas. There are TMJ pathologies that require total joint prostheses for best results. The application of computer technology for TMJ and orthognathic surgical planning and implementation has significantly improved the accuracy and predictability of treatment outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Correctly diagnosing, planning, and accurately producing surgical outcomes for patients with temporomandibular joint (TMJ) and associated dentofacial deformities are very important factors for optimal patient management [1]. Conventional two-dimensional (2D) computer-assisted imaging systems allow the surgeon a quick analysis of the surgical case and to perform treatment planning. However, in some cases, with significant facial deformity and asymmetry, the reliability of these 2D systems is suboptimal. In recent years, the development of 3D software systems (computer-assisted surgery systems—CASS) that integrates cone beam computerized tomography (CBCT) and computerized tomography (CT) images of the facial skeleton, CBCT/CT images of the dental casts or dental model surface scanning, and photographs (2D or 3D) of the patients has improved the methods in which patients can be diagnosed and virtually treatment planned [1,2,3,4,5,6,7]. Three-dimensional computer programs allow the surgeon to visualize the hard and soft tissue structures in 3D to aid and improve the diagnostic and treatment planning accuracy. Through computer-assisted surgical simulation (CASS) technology and virtual surgical planning (VSP) software programs, manipulation of the hard and soft tissue structures, simulating precise surgical movements, can be accomplished. These sophisticated programs allow segmentation of the maxillary and mandibular skeletal structures as determined in the presurgical planning and printing of surgical stabilizing appliances to reposition the jaw into predetermined positions, so accurate duplication of the indicated procedures can be accomplished at surgery. In addition, VSP will identify areas of hard tissue interferences or creation of bony gaps that may need to be addressed in order to meet the treatment goals and provide stability of the surgical results. For instance, if bone gaps are created in the maxilla, this could indicate a bone graft requirement for stability. In the mandible, for example, ramus sagittal split osteotomies used for correcting a posterior yaw may create bony interferences between the proximal and distal segments on the side to which the mandible is rotated toward, requiring additional ostectomies or bone recontouring for the segments to fit together. Predictions of soft tissue changes are also possible that may assist in positioning of the skeletal structures and identify areas that may require hard or soft tissue augmentation or reduction to maximize the esthetic outcomes.
CASS can be used in combination with rapid prototyping (RP) technology, robotics, and image-guidance systems (navigational surgery). Surgical templates fabricated by rapid prototyping (3D printing) technology permit a higher precision and predictability than those obtained with more traditional methods. Surgical cutting guides can also be constructed to mark the osteotomy lines, improving surgical accuracy and decreasing risk of injuries to facial nerves and vessels. Temporary positioning guides can help the surgeon to fix the bony segments in the ideal position previously determined. Finally, custom implants such as TMJ prosthesis, bone reconstruction, mandibular plates or miniplates, maxillary bone plates, custom alloplastic esthetic implants, etc. can be constructed before surgery to fit accurately into the surgical site.
Intraoperative navigation is also possible eliminating the need for surgical guides. Navigation systems can be used for intraoperative guiding as well as for validation of bone position [8,9,10].
Augmented reality tools for maxillary positioning in orthognathic surgery are currently under development and may be a valuable tool in the future for cranio-maxillofacial surgery [11]. The final objective using these techniques is to enhance an accurate diagnosis of the pathology and to improve safety and accuracy of the surgical procedures performed. Although these techniques are expensive and increase the time spent preparing surgery, they may permit less invasive approaches and reduce morbidity. Also, the technology facilitates better communication between the healthcare providers involved in the patient’s treatment plan. Numerous CAD/CAM programs are currently available in oral and maxillofacial surgery (oncologic resection and reconstruction, orthognathic surgery, distraction osteogenesis, and TMJ surgery).
Patients with TMJ pathology, with or without a coexisting dentofacial deformity, can be corrected with only TMJ surgery or may require concomitant TMJ and orthognathic surgery. However, this chapter is directed to patients that have only TMJ pathologies surgically treated without including orthognathic surgical procedures. The combination of TMJ and orthognathic surgery will be presented in a subsequent chapter. Depending on the TMJ pathology and surgeon’s experience and technical skills, TMJ surgery can be performed in one surgical stage or separated into two surgical stages. The two-stage approach requires the patient to undergo two separate operations (one surgery to eliminate the TMJ pathology and a second operation to reconstruct the TMJ) and two general anesthetics significantly lengthening the overall treatment time. Performing TMJ surgery in a single operation significantly decreases treatment time, provides better outcomes, but requires careful treatment planning and surgical proficiency in TMJ surgical techniques. There are TMJ pathologies that require total joint prostheses for best results. The application of computer technology for TMJ reconstruction surgical planning and implementation has significantly improved the accuracy and predictability of treatment outcomes.
This chapter presents the treatment planning and surgical protocols for patients only requiring TMJ reconstruction with the application of computer-assisted surgical simulation (CASS) and virtual surgical planning (VSP) programs for patient-fitted TMJ total joint prostheses. The CASS and VSP protocols decreases the preoperative workup time and increases the accuracy of model preparation fit of the prosthetic components and subsequent surgery [12, 13].
2 Indications for TMJ Total Joint Replacement (TJR)
Temporomandibular joint (TMJ) disorders or pathology without requiring additional orthognathic surgical procedures is common. The TMJ pathology can occur with no effect on the position of the jaws and occlusion or may be the causative factor for malalignment of the mandible in the presence of a normally positioned maxilla. The most common TMJ pathologies that can or cannot adversely affect mandibular position and occlusion, with or without the requirement for concomitant orthognathic surgery, include (1) articular disc dislocation, (2) adolescent internal condylar resorption (AICR), (3) reactive arthritis, (4) condylar hyperplasia, (5) trauma (Case 1, Figs. 7.1, 7.2, 7.3, and 7.4), (6) failed autogenous or alloplastic TMJ reconstruction (Cases 2 and 3, Figs. 7.5, 7.6, 7.7, 7.8, 7.9, 7.10, 7.11, 7.12, and 7.13), (7) heterotopic bone and ankylosis (Case 4, Figs. 7.14, 7.15, 7.16, 7.17, 7.18, 7.19, 7.20, 7.21, and 7.22), (8) congenital deformation or absence of the TMJ, (9) tumors (Case 5, Figs. 7.23, 7.24, 7.25, 7.26, 7.27, 7.28, and 7.29), (10) connective tissue and autoimmune diseases, and (11) other end-stage TMJ pathologies [14, 15]. These TMJ conditions can be associated with dentofacial deformities, malocclusion, TMJ pain, headaches, myofascial pain, TMJ and jaw functional impairment, ear symptoms, sleep apnea, etc. Patients with these conditions may benefit from corrective surgical intervention, including TMJ reconstruction with or without the requirement for orthognathic surgery. Some of the aforementioned TMJ pathologies may have the best outcome prognosis using custom-fitted total joint prostheses for TMJ reconstruction [14, 15].
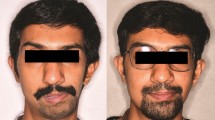
Case 1. (a, b) A 56-year-old female who fell sustaining bilateral subcondylar fractures with resultant anterior open bite and retrusion of the mandible. (c, d) The patient is observed 1 year post-surgery with improvement in facial balance following counterclockwise rotation of the mandible into occlusion to close the open bite with bilateral TMJ Concepts total joint prostheses and bilateral TMJ fat grafts
Case 1. (a–c) Presurgical occlusion demonstrating the anterior open bite. The patient occludes only on the second molars bilaterally. (d–f) One year post bilateral TMJ reconstruction with counterclockwise rotation of the mandible utilizing TMJ Concepts custom-fitted total joint prostheses and bilateral TMJ fat grafts
Case 1. (a, b) The mandibular model was produced with the mandible repositioned into the best occlusal fit using CASS and VSP technology. The mandibular rami were prepared with the red marks indicating areas of bone recontouring to make the lateral aspect of the ramus as flat as possible to accommodate the prostheses. (c, d) TMJ prostheses have been manufactured and are custom fitted to the 3D stereolithic model
Case 2. Records are from a 55-year-old female with failed Christensen metal-on-metal total joint prostheses. (a) Right TMJ Christensen prosthesis with a fractured fossa component but also with heterotopic bone that has grown around the medial posterior and lateral aspect of the prosthesis (red arrow). (b) Left TMJ failed metal prosthesis. Both joints produced metallosis from the metal-on-metal articulation
Case 2. (a) Bone cement spacers were placed bilaterally to fill the osseous defects following removal of the TMJ failed Christensen prostheses. The cement spacer is seen on the left side. (b) Radiographically, the left cement spacer is seen positioned filling the gap between the fossa and left ramus of the mandible. The bone cement spacer serves to maintain the space and stabilize the mandibular position in preparation for the second stage of surgery
Case 2. (a) Residuals of the condylar neck and heterotopic bone in the fossa are seen and require removal in preparation for the custom-fitted total joint prostheses. (b) Mandibular ramus and fossa prepared with removal of heterotopic bone in the fossa and recontouring the ramus in preparation of manufacturing the total joint prosthesis. (c, d) Right side in final preparation with removal of bone from the upper area of the ramus to create 20 mm of space between the fossa and ramus to accommodate the total joint prosthesis. (e, f) Bilateral TMJ Concepts custom-fitted total joint prostheses have been constructed on the 3D stereolithic model
Case 3. Records from a 46-year-old female with a failed Biomet prosthesis. (a, b) Unilateral right Biomet total joint prosthesis with a condyle positioned posterior to the fossa creating severe pain and functional issues. Although the mandibular component is metallic, the fossa component is polyethylene. (c) Clinical picture of the displaced mandibular component of the Biomet prosthesis
Case 4. (a) Surgical view of the right TMJ ankylosis. (b) Ankylotic bone removed to free the right mandible. The gap arthroplasty is observed. (c) The bone and condyles removed from the bilateral TMJ resection to create the gap arthroplasty and the resected coronoid processes are seen. (d) The silicone ball spacer has been inserted into the osseous gap to maintain the space, stabilize the mandibular position, and decrease the risk of reankylosis during the intermediate stage in preparation for the second stage of surgery
Case 4. (a) CT scan, acquisitioned following the first surgical stage that included bilateral remove ankylotic bone, condylectomies, coronoidectomies, and placement of silicone balls into the created bone gap. (b) CASS and VSP technology used to place the mandible into the final surgical position (orange mandible), superimposed on the CT scan in Fig. 7.15a. From this position, it will be determined if additional bone resection and preparation of the fossa and ramus are required
Case 4. (a) 3D CT scan CASS preparation, illustrating the additional bone resection required (orange area at the superior aspect of the rami and in the right fossa) to accommodate the Biomet TMJ prostheses. (b) 3D CT scan CASS technology can provide computer-generated cutting guides to facilitate the accuracy of required bone resection on the ramus. Illustrated is the left ramus cutting surgical template (colored in green) for implementation during surgery
Case 4. Computer design of the Biomet custom-fitted total joint prostheses from numerous views, including the medial view that demonstrates the planned position of the stabilizing screws for the mandibular components in relation to the rami and inferior alveolar nerves, (a) left side, (b) light side
Case 4. (a) Left surgical cutting guide stabilized onto the left mandibular ramus with a bone screw, viewed through the submandibular incision. (b) Superior extent of the surgical cutting guide marks precisely the osteotomy line of the bone at the superior aspect of the ramus that requires resection to accommodate the total joint prosthesis, as viewed through the preauricular incision
Case 4. (a) Postoperative coronal radiograph shows the position of the bilateral Biomet total joint prostheses. The fossa component of polyethylene does not image on the X-ray. (b) Panogram shows the position of the bilateral Biomet TMJ prostheses. (c) Postsurgical maximal interincisal opening achieved was 32 mm
Case 5. (a) Using CASS and VSP technology, the right mandibular condylar tumor was electronically removed, occlusion set, and the Biomet custom-fitted total joint prosthesis designed for a single-stage reconstruction procedure of the right TMJ. (b) Numerous views of the computer design of the right TMJ Biomet prosthesis are observed including screw positioning in relation to the inferior alveolar nerve and ramus
3 TMJ Total Joint Replacement
There are basically two systems on the market for TMJ total joint prosthesis reconstruction: TMJ Concepts (Ventura, CA) and Biomet Microfixation (Jacksonville, FL). These two systems are approved by the Federal Drug Administration (FDA) in the USA and available internationally.
The TMJ Concepts total joint prostheses are patient-fitted devices, originally developed in 1989 by Techmedica (Camarillo, CA) and manufactured until July 1993, when the US Food and Drug Administration (FDA) halted production of all TMJ devices. In 1996, the FDA permitted the new owners, TMJ Concepts (Ventura, CA), to manufacture the device under the 510 K provision and granted full approval of these Class III devices in 1999. The Techmedica and TMJ Concepts devices are computer-assisted designed (CAD) and computer-assisted manufactured (CAM) devices that fit the specific anatomic, functional, and esthetic requirements of each patient.
The TMJ Concepts custom-fitted total joint prostheses use design principles and materials that are proven highly successful and are the gold standard in orthopedic joint reconstruction for hip and knee replacements. The prosthesis consists of a fossa component with a commercially pure titanium framework covered with a mesh and an ultrahigh molecular weight polyethylene functional component fused to the mesh on the bottom side of the framework. The fossa component is attached to the lateral rim of the fossa with four 2-mm-diameter screws, usually 6 mm in length. The mandibular component is composed of a titanium alloy shaft with a cobalt-chromium alloy head with the prosthesis secured to the mandibular ramus with 8–9 2-mm-diameter bicortical screws, usually 8–12 mm in length (Fig. 7.4c, d). The fossa and mandibular components osseointegrate. Cases 1, 2, and 3 demonstrate the use of the TMJ Concepts prostheses.
The Biomet Microfixation TMJ Replacement System is a stock device (off the shelf) with fossa and mandibular components to choose from. Custom-fitted devices are available internationally, but not in the USA. Clinical trials for the stock device were initiated in 1995 and granted FDA approval in 2005. The ramus component is composed of a chromium-cobalt alloy. The ramus side has a titanium coating to help with osseointegration. The ramus component is available in three lengths: 45, 50, and 55 mm. There are three basic styles including standard, offset, and narrow. The fossa is composed of ultrahigh molecular weight polyethylene and does not osseointegrate with the fossa but is stabilized to the lateral rim of the fossa with bone screws. There are three fossa sizes to choose from including small, medium, and large. The prosthesis is metal-on-polyethylene articulation, which is the gold standard in orthopedics. The mandibular component is stabilized to the ramus with 2.7-mm-diameter screws, and the fossa component is secured to the lateral rim of the fossa with 2.0-mm-diameter screws (Fig. 7.11a). Cases 4 and 5 demonstrate the use of the Biomet prostheses.
Treatment planning for cases needing TMJ total joint replacement without the requirement for orthognathic surgery is based on radiographic and MRI imaging, cephalometric analysis, prediction tracing, clinical evaluation, and dental model assessment, which provide the templates for movements of the upper and lower jaws to establish optimal treatment outcome in relation to function, facial harmony, occlusion, and oropharyngeal airway dimensions. For patients who require total joint prostheses, a medical grade computerized tomography (CT) scan with 1 mm overlapping cuts is recommended of the maxillofacial region that includes the TMJs, maxilla, and mandible.
The surgeon has two options for model preparation to aid in the construction of patient-fitted total joint prostheses using the TMJ Concepts system. We have previously published the traditional protocol technique versus the CASS protocol [12, 13]. In this chapter, we will present only the CASS technique for patients requiring TMJ reconstruction without additional orthognathic procedures such as maxillary and mandibular osteotomies.
4 Protocol for TMJ Reconstruction
For TMJ reconstruction cases, the surgery is planned using CASS and VSP technology and moving the mandible into the final position (if malaligned with the maxilla) in a computer-simulated environment (Figs. 7.3 and 7.4).
Using Digital Imaging and Communications in Medicine (DICOM) data, the stereolithic model is produced with the mandible properly aligned with the maxilla in the final position and provided to the surgeon for removal of the condyle(s) and recontouring of the lateral rami and fossae if indicated. For simpler cases, the condylectomies can be done virtually as well as the recontouring of the lateral aspect of the ramus with VSP technology, thus eliminating the step of sending the model to the surgeon for these processes, although the procedures must be approved by the surgeon. The stereolithic model is sent to TMJ Concepts (Ventura, CA) for the design, blueprint, and wax-up of the custom-fitted prostheses. Using the Internet, the design is sent to the surgeon for approval. Then, the prostheses are manufactured (Fig. 7.4). It takes approximately 12 weeks to manufacture the total joint custom-fitted prostheses.
Presurgical orthodontic preparation may or may not be required to obtain the best occlusal outcome and, of course, is case dependent. Usually, a surgical stabilizing splint is not required when the occlusion is good or only the mandible requires repositioning to create a stable occlusion. However, indications for a surgical splint include (1) unstable occlusion with the mandible in the final position; (2) missing posterior teeth; (3) lack of dental units to provide a stable occlusion; (4) significant periodontal issues with unstable dental units; (5) significant changes in the positions of the teeth from the presurgery orthodontics; (6) edentulous patients; and (7) surgeon’s preference. If a splint is required, there are two approaches for providing accurate dental models: (1) provide standard dental models or (2) scan the dentition with an optical scanner and sending either printing models or the scan data to the VSP company. The first option requires that approximately 2 weeks before surgery, final dental models are produced. Equilibration of the teeth on the model is done if indicated. Usually only one set of models is required when the occlusion is good, or only the mandible needs to be repositioned. The second option involves optical scanning of the occlusion, with or without printing of dental models, or scanning of dental models from impressions. The models are either sent to the VSP company or digitally sent for incorporation into the computer model. If a surgical splint is required, the splint is then printed from the computer model. The dental models, splint, and images of the CASS workup are sent to the surgeon for implementation during surgery. For patients with severe decreased incisal opening, such as in TMJ ankylosis cases, where dental models and optical scanning cannot be acquired, the surgical splints can be produced from the computer model, although there could be inaccuracies as compared to dental model acquisition.
The 3D stereolithic model may require preparation of the rami and fossae. In the fossa, heterotopic bone deposition or unusual anatomy may require recontouring so that the custom-fitted fossa component can be precisely adapted to the bony anatomy. The mandibular ramus may need recontouring as well (Fig. 7.9). It is advantageous to modify the ramus to make the contour fairly flat in the area where the prosthesis will be placed. This is to eliminate any depressions, humps, bumps, or curvatures (particularly at the inferior border of the angle). This provides some leeway if the mandible is not perfectly positioned at surgery compared to the stereolithic model. Otherwise, the prosthesis may not fit on the ramus properly with the condyle head seated properly in the fossa, or if the mandibular component is properly seated on the ramus, the head may not be seated in the fossa correctly. Flattening of the lateral aspect of the ramus eliminates potential prosthesis positioning issues.
To follow are the protocols for single-stage or two-stage surgical approaches to TMJ reconstruction with TMJ total joint prostheses. The decision between the protocols is dependent on the TMJ pathology, previous surgical procedures patient has endured, and the surgeon’s skills, experience, and comfort zone.
Indications for two-stage surgery may include (1) significant heterotopic bone deposition in and around the TMJ/fossa area; (2) ankylosis; (3) major altered anatomy requiring significant bony modification, recontouring, or bone grafting; (4) removal of failed alloplastic total joint prosthesis; and (5) removal of failed autogenous graft such as a rib graft or sternoclavicular graft, where the surgeon would prefer to remove the graft and recontour the fossa and ramus prior to CT scan acquisition.
A major potential risk to patients receiving TMJ total joint prosthesis is infection. The occurrence rate is less than 2% with greater risk for patients on immunosuppressant medications such as rheumatoid patients or others with connective tissue/autoimmune diseases. Bacterial or viral contamination of the prosthesis can occur during surgery or develop at a later time from bacterial seeding through a hematological route or localized bacterial sources. As a result, strict adherence to sterile technique for the procedures performed can help prevent or reduce the chance of infection (Table 7.1).
5 Surgical Procedure
The surgical description to follow assumes that if a two-stage procedure was indicated, the first stage has been completed, prostheses manufactured, and the patient is ready to undergo Stage 2. If surgery is a single-stage, the following protocol applies. So, not to duplicate other figures in this book, the following protocol will refer to figures from with the appropriate references.
-
1.
After surgical prepping including the face, neck, mouth, ears, ear canals, nose, endotracheal tube, and abdomen, the abdomen and the face and neck are draped, and the mouth and nose are isolated by application of a Tegaderm film dressing (Fig. 7.15a), and the ear canal is cleaned with chlorhexidine and gently packed with cotton soaked in betadine solution.
-
2.
The TMJs are approached through an endaural (Fig. 7.16) or preauricular incision to perform the condylectomy, discectomy, joint debridement, and also a coronoidectomy when the mandible is significantly advanced or vertically lengthened (Fig. 7.17). The condylectomy and debridement of the joint is performed first. Placing medial retractors and packing Surgicel or similar material medial to the condylar neck will help protect the nerves and vessels medial to the surgical area, while the condylectomy cut is being completed. The fossa is debrided and recontoured if indicated by the preparation on the stereolithic model. There is a requirement of 20 mm space between the fossa and the top of the ramus when the mandible is in its new position to accommodate the prosthesis, or there could be interferences that won’t allow the prosthesis components to be properly seated. Be sure an adequate amount of bone is removed for the superior aspect of the ramus to meet the space requirement. Using cutting guides can improve the accuracy for adequate bone removal.
The coronoidectomy is usually not required with only TMJ reconstruction unless a significant counterclockwise rotation of the mandible is required or the coronoid process is hyperplastic and interfering with mandibular function. If indicated, then the coronoidectomy is preformed through the endaural incision using a reciprocating saw or piezo cutting device, with the cut extending from the anterior aspect of the coronoid into the sigmoid notch (Fig. 7.17). Using a medial retractor or packing Surgicel or Gelfoam medial to the coronoid will protect the vessels and other soft tissue structures, while the cut is made. Risks associated with this part of the surgery include facial nerve injury and bleeding as the facial nerve branches and maxillary artery and branches are in close proximity. Facial nerve involvement can be minimized by understanding the anatomy, employing small incisions, using a nerve stimulator when appropriate, careful surgery, and avoiding heavy-handed inferior retraction toward the earlobe as this can cause damage to the main branch of the facial nerve. Avoid bleeding by using retractors that surround the medial side of the condyle and neck for the condylectomy. When using a reciprocating saw for the condylectomy and coronoidectomy, packing Surgicel or Gelfoam around the medial side of the condylar neck and medial to the ramus, sigmoid notch area, and coronoid will help prevent encountering the major vessels in the area by displacing the vessels more medially and placing a physical barrier between the bone cuts and the vessels. Using piezo technology can also be of benefit.
-
3.
A submandibular incision (Fig. 7.16) is used to access the ramus. A nerve stimulator is used to identify the branches of the facial nerve as the various tissue layers are incised. After cutting through the platysma muscle, blunt dissection to the pterygoid-masseteric sling will reduce the risk of nerve and vascular injury. Cutting through the sling to the inferior aspect of the angle gives access to the ramus for detachment of the masseter muscle. The medial pterygoid muscle is detached only if the mandible is to be vertically lengthened or advanced significantly as in closing an anterior open bite with a counterclockwise rotation of the mandible. The lateral aspect of the ramus is recontoured using a reciprocating bone file to duplicate the alterations made on the stereolithic model to provide a relatively flat contour of the ramus where the mandibular component will be positioned. The mandible is mobilized in a downward and forward direction only if indicated to significantly advance or vertically lengthen the ramus and achieve a passive ideal occlusal relationship. Potential risk factors during this aspect of the surgery include facial nerve damage and bleeding. The use of a nerve stimulator during dissection to the angle area will help identify the nerve branches and help in injury avoidance.
-
4.
The oral cavity is isolated by draping with sterile towels, exposing from commissure to commissure (Fig. 7.15b). The Tegaderm is cut through and the oral cavity is entered. If the case includes bilateral total joint prostheses, the surgical splint is inserted (only if required, as in an unstable bite or multiply missing teeth) and maxillo-mandibular fixation applied. This requires the presence of orthodontic appliances placed prior to surgery or the application of arch bars to the maxillary and mandibular teeth (or other methods of applying stabilizing devices to control the occlusion) that can be placed at the beginning of surgery prior to patient surgical preparation. If the case is a unilateral total joint prosthesis, then go to Step 5. If the case is bilateral total joint prostheses, then go to Step 6.
-
5.
For unilateral total joint prosthesis, when the mandible requires repositioning to obtain a good occlusion, using separate instrumentation, a contralateral mandibular ramus sagittal split osteotomy may be indicated to achieve a good stable occlusion, and the mandible is mobilized on that side. The surgical splint, if required, and maxillo-mandibular fixation are applied. Rigid fixation is placed to secure the mandibular segments and incision closed.
-
6.
The temporary drapes are removed, surgeon changes gloves and gown, the face is re-prepped and redraped, and the mouth and nose are sealed off once again with a Tegaderm film dressing.
-
7.
The total joint prosthesis fossa component is inserted, properly positioned, and fixated usually with four 6-mm-length, 2-mm-diameter bone screws. The mandibular component is inserted through the submandibular incision placing the head into the fossa and against the posterior stop and aligning to the ramus as dictated by the surgical plan. Bone screws (2 mm diameter and usually 8–12 mm in length) are inserted in all of the available holes (usually eight) to stabilize the component to the mandible. Usually it is difficult to reach the top holes in the mandibular component through the submandibular incision. So, a stab incision can be made about 1 cm below the earlobe and a trocar (KLS Martin) inserted to place screws in the holes at the top of the prosthesis that are difficult to access from the submandibular incision (Fig. 7.19).
-
8.
The submandibular surgical areas are thoroughly irrigated with saline and a final rinse using betadine solution. The masseter muscle is reattached to the mandible by placing 3–4 bicortical holes through the inferior border of the mandibular angle area where the muscle was originally attached. 2-0 PDS suture is used to tie the masseter muscle to the bone using the transosseous holes (Fig. 7.20). The submandibular incisions are closed in layers.
-
9.
Fat grafts are harvested from the abdomen through incisions in the suprapubic region (see Fig. 7.21), previous scar line, umbilical area (Fig. 7.22), or buttock with establishment of good hemostasis and closure of the incisions. A small drain and vacuum bulb can be inserted in the donor area if good hemostasis cannot be achieved. An abdominal dressing and abdominal binder are applied at completion of surgery to help prevent hematoma and seroma formation.
-
10.
The articulating area of the prosthesis is thoroughly irrigated with saline through the endaural or preauricular incisions with a final rinse using betadine solution. The fat grafts are packed around the articulating area of the prostheses (Fig. 7.23) and the incisions closed in layers.
-
11.
The oral cavity is then entered, maxillo-mandibular fixation released, and intermediate splint removed unless required for occlusal stability. Surgery is completed.
Since the muscles of mastication including the medial pterygoid and temporalis muscles are not usually detached, vertical support to the mandible and occlusion is usually good. Using elastics post-surgery would only be indicated for occlusion control, patient comfort, or to help control an unstable joint secondary to inadequate placement of the prostheses. If orthodontic appliances are present, postsurgical orthodontics are continued with usual orthodontic mechanics to finalize the occlusion and retain. Postsurgically, light force vertical elastics (recommend 3½ oz., 3/16-in. diameter) can be used to support the mandible for patient comfort and to finalize the occlusion. Postsurgical patient management is the same as routine orthodontics [16, 17].
5.1 Fat Grafts
Early on in the use of total joint prostheses, a common problem encountered in approximately 35% of the patients was postsurgical fibrosis and heterotopic bone formation around the prostheses causing jaw dysfunction, decreased incisal opening, and pain [18, 19]. In 1992, Wolford developed a technique to place fat grafts (harvested from the abdomen or buttock) around the articulating area of the total joint prosthesis to eliminate the dead space. This prevents blood clot formation in the space around the prosthesis that could provide a matrix for fibrous ingrowth and pluripotential cells migrating into the area that could develop heterotopic bone and dense fibrotic tissues. Also, in patients with previous failed alloplastic implants, the fat graft blocks out a large area in which the foreign-body giant cell reaction and reactive bone may otherwise redevelop [18, 19].
6 Case Presentations: Figs. 7.14, 7.15, 7.16, and 7.17
Case 1: Bilateral Mandibular Subcondylar Fractures
This 56-year-old female fell, sustaining bilateral mandibular subcondylar fractures (Figs. 7.1a, b, 7.2a–c, and 7.3a–d). The injury created significant displacement of the fractured condyles that were treated initially elsewhere with closed reduction, but without reduction of the displaced segments, resulting in a large anterior open bite (Fig. 7.2a–c). She was subsequently referred for management of her TMJ and jaw deformity at 3 months post injury. At the initial consult, she reported that since her accident, she had developed headaches, myofascial pain, occluded only on the left second molars, snoring, and sleep apnea. Her incisal opening was 40 mm and excursions 2 mm to the right and 4 mm to the left. Her diagnosis included (1) bilateral mandibular subcondylar fractures; (2) mandibular A-P and posterior vertical hypoplasia; (3) anterior open bite of 4 mm; (4) occluding only on the left second molars; and (5) decreased oropharyngeal airway with sleep apnea symptoms. Radiographic evaluation confirmed the significantly displaced subcondylar fractures (Fig. 7.3a–d). A CT scan was obtained and CASS technology used to assess the injury and reposition the mandible into centric occlusion and the 3D stereolithic model produced with the mandible in the corrected position. The surgeon then prepared the model and sent it to TMJ Concepts for manufacturing of the bilateral TMJ custom-fitted total joint prostheses (Fig. 7.4a, b).
Her surgery included (1) bilateral TMJ reconstruction with counterclockwise rotation of the mandible, using TMJ Concepts custom-fitted total joint prostheses (Fig. 7.4c, d); (2) bilateral TMJ fat grafts packed around the articulating area of the prostheses, harvested from the abdomen; (3) application of maxillary and mandibular arch bars; and (4) removal of arch bars at completion of surgery.
The patient was reevaluated at 1-year post-surgery. She was pain free, incisal opening at 47 mm, excursive movements 3 mm to the right and left, stable Class I occlusion, improved facial balance, and elimination of sleep apnea symptoms (Figs. 7.1c, d and 7.2d–f).
Case 2: Failed Bilateral Metal-on-Metal Total Joint Prostheses
This case demonstrates the protocol for patients that have failed metal-on-metal (Christensen System) total joint prostheses or prostheses with a fossa component that contains a metal base with polyethylene attached (TMJ Concepts). The records used here are of a 55-year-old female that presented 18 years post-bilateral TMJ reconstruction with Christensen total joint prostheses with metal-on-metal articulation. She did fairly well for the first 8 years but, during the past 10 years, has suffered from severe pain issues, periodic bleeding from the right ear, and limited jaw function. She developed debilitating headaches, TMJ pain, myofascial pain, and limited jaw function and was on total disability. Her occlusion and facial balance remained stable. Incisal opening was 15 and 0 mm excursions. Radiographic evaluation shows the presence of bilateral Christensen total joint prostheses with the right fossa component fractured and heterotopic bone surrounding the medial, posterior, and lateral aspect of the functional area (Fig. 7.5a, b). The diagnosis for this patient included (1) failed bilateral TMJ Christensen total joint prostheses including metallosis, fractured right fossa component, and right-sided heterotopic bone; (2) severe headaches, TMJ pain, and myofascial pain; and (3) severe limited jaw function.
Because of the presence of the metal-on-metal prosthesis, the patient required two-stage surgery. Although the CASS system can adequately remove the metal from the ramus, it cannot accurately remove the metal from the fossa, so the bony anatomy of the fossa cannot be accurately duplicated. Thus, these cases with metal fossae require a two-stage surgical approach to remove the prosthesis so an accurate CT scan can be acquired to reproduce the bony anatomy accurately, followed by the second surgery stage to reconstruct the TMJ. For this case, the two-stage surgical protocol (Table 7.2) was used. In the first stage, the failed bilateral TMJ Christensen prostheses were removed (Fig. 7.6), bilateral TMJ debridement and placement of bone cement spacers (Fig. 7.7). A CT scan was taken and submitted for CASS, where VSP placed the mandible into the best occlusal fit with the stable maxilla (Fig. 7.8). A stereolithic 3D model was constructed with the maxilla and mandible in the final postsurgical position (Fig. 7.9a–d). The final preparation of the model was completed with recontouring of the fossa and ramus as required, in preparation for the manufacturing of the total joint prostheses (Fig. 7.9a–d). The superior aspect of the ramus was removed to create 20 mm of vertical space between the fossa and ramus to accommodate the TMJ Concepts custom-fitted total joint prostheses. The devices are then designed and manufactured on this model (Fig. 7.9e, f). Surgery Stage 2 included (1) application of maxillary and mandibular arch bars; (2) removal of TMJ spacers; (3) application of maxillo-mandibular fixation; (4) bilateral TMJ reconstruction with TMJ Concepts custom-fitted total joint prostheses; (5) bilateral TMJ fat grafts packed around the articulating area of the prostheses, harvested from the abdomen; and (6) removal of maxillo-mandibular fixation and arch bars for completion of the surgery.
Case 3
This case is to demonstrate the protocol for patients that have failed prosthesis with polyethylene fossa and metal condylar component (Biomet system) total joint prostheses. The records used here are of a 46-year-old female that was referred for consultation 3 years post placement of a right Biomet total joint prostheses with metal-on-polyethylene articulation with the surgery performed at a different institution. She had severe pain since waking up from surgery. At 3 years post-surgery, she had debilitating right-sided headaches, TMJ pain, myofascial pain, and limited jaw function (22 mm incisal opening) and was on total disability and on heavy doses of narcotics. Her occlusion and facial balance remained relatively stable. Radiographic evaluation showed the presence of displaced right mandibular condylar head of the mandibular component total joint prosthesis relative to the fossa component (Figs. 7.10 and 7.11) The diagnosis for this patient included (1) displaced right mandibular component of the Biomet prosthesis; (2) severe headaches, TMJ pain, and myofascial pain; and (3) limited jaw function.
CASS technology was used in preparation of this case. Because of the presence of a polyethylene fossa, these patients can be treated with one-stage surgery protocol (Table 7.3). A CT scan was taken and submitted for CASS. The metal mandibular component and the polyethylene fossa component were electronically removed from the computer model, and VSP placed the mandible into the best occlusal fit with the maxilla (Fig. 7.12). A stereolithic 3D model was constructed, and the final preparation of the model completed by the surgeon with additional recontouring of the ramus and fossa was required, in preparation for the manufacturing of the TMJ Concepts total joint prosthesis (Fig. 7.13a). The prosthesis was then designed and manufactured on this model (Fig. 7.13b). The surgery included (1) orthodontic appliances were already present on the teeth; (2) removal of failed prosthesis; (3) TMJ reconstruction with TMJ Concepts custom-fitted total joint prosthesis; and (4) TMJ fat graft packed around the articulating area of the prosthesis, harvested from the abdomen.
Case 4
This 53-year-old male was diagnosed with (1) SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, and osteitis) [20], (2) bilateral TMJ arthritis, (3) right TMJ ankylosis, and (4) maximal incisal opening of 5 mm (Fig. 7.14a, b). A-P tomograms and panogram demonstrate the bony morphological changes resultant from the SAPHO syndrome (Fig. 7.14c, d). CT images demonstrated bilateral osseous ankylosis with mandibular bony sclerosis. The patient was treated with two surgical stages that consisted of Surgery Stage 1, resection of bilateral TMJ bony ankylosis, bilateral condylectomies, coronoidectomies (Fig. 7.15a–c), and silicone ball insertion into the bony defect (Fig. 7.15d). The silicone ball spacers were inserted into the osseous gap to maintain the space, stabilize the mandibular position, and decrease the risk of reankylosis during the intermediate stage in preparation for the second stage of surgery.
CT scan of the patient was acquisitioned following the first surgical stage (Fig. 7.16a). CASS and VSP technology were used to place the mandible into the final surgical position (orange mandible), with the best occlusal fit, and are superimposed on the post-surgery CT scan, demonstrating the positional changes (Fig. 7.16b). From this position, it is determined if additional bone resection and preparation of the fossa and ramus are required to accommodate the total joint prostheses.
The CASS- and VSP-corrected CT images show the osseous defects after bilateral condylectomy and coronoidectomy with the silicone balls in place (Fig. 7.17a). The cutting guides (colored green) are manufactured to accurately identify additional bone required for removal from the ramus to accommodate the prostheses (Fig. 7.17b). The Biomet bilateral prostheses were computer designed as custom-fitted total joint prostheses to accommodate to the patients’ specific anatomical requirements (Figs. 7.18 and 7.19). At surgery, the left cutting guide is inserted and secured to the ramus with a bone screw as seen through the submandibular incision (Fig. 7.20a). The top of the cutting guide is seen through the preauricular incision, demonstrating the amount of bone required to be removed to accommodate the TMJ prosthesis (Fig. 7.20b). The prostheses are inserted and stabilized with bone screws. The placement of the right prosthesis is seen through the preauricular incision (Fig. 7.21a), and the left side prosthesis is seen through the submandibular and preauricular incisions (Fig. 7.21b). Postoperative coronal radiograph shows the position of the bilateral Biomet total joint prostheses. The fossa component of polyethylene does not image on the X-ray (Fig. 7.22a). Panogram shows the position of the bilateral Biomet TMJ prostheses (Fig. 7.22b). Postsurgical maximal interincisal opening achieved was 32 mm (Fig. 7.22c).
Case 5
This 42-year-old male was diagnosed with a right preauricular tumor (Fig. 7.23a). CT scan images including 3D imaging demonstrate an expansive osteolytic tumor located in the right mandibular condyle (Fig. 7.23b–d). Biopsy under local anesthesia demonstrated a fibrous benign tumor. Surgery was planned as a single-stage procedure for resection of the tumor and immediate reconstruction of the right TMJ with a Biomet custom-fitted total joint prosthesis using CASS with VSP. The right mandibular condylar tumor is seen, and the level of mandibular osteotomy to remove the tumor is designated in preparation for electronic removal (Fig. 7.24a, b). The tumor is electronically removed, occlusion set, and the Biomet custom-fit total joint prosthesis designed for a single-stage reconstruction procedure of the right TMJ (Fig. 7.25a, b). The Biomet prosthesis was custom-designed on the computer to fit this patient’s specific anatomical requirements. The shape of the mandible and location of the inferior alveolar nerve were identified and figured into the equation for mandibular component design (Fig. 7.25b). A 3D mandibular stereolithic model was produced demonstrating the tumor resection to aid in surgery (Fig. 7.26a). A computer-generated and computer-printed occlusal splint was produced to aid in positioning of the mandible during insertion of the right Biomet total joint prosthesis (Fig. 7.26b). At surgery, the tumor was resected and removed (Fig. 7.27). The right TMJ Biomet fossa component was positioned and stabilized to the lateral rim of the fossa with five bone screws, as viewed through the preauricular incision. The mandibular component was positioned and stabilized to the ramus with seven bone screws, as viewed from the submandibular incision (Fig. 7.28). Pre- and post-surgery panograms demonstrate the original tumor and subsequent removal and right TMJ reconstruction with the Biomet custom-fitted total joint prosthesis (Fig. 7.29).
7 TMJ Ankylosis
TMJ heterotopic bone refers to calcifications that develop in and around areas of the joint that are normally void of bone. The development of heterotopic bone within the confines of a joint or in the surrounding area can cause joint dysfunction, pain, as well as progression to ankylosis. TMJ ankylosis is a condition where the condyle is fused to the fossa by bony or fibrotic tissues creating a debilitating condition that can interfere with jaw function, mastication, speech, oral hygiene, growth and development, breathing, and normal life activities and cause pain. There are numerous surgical techniques that have been proposed to manage heterotopic bone and TMJ ankylosis with varying outcomes reported. The most common post-surgery complications are limited jaw function, pain, and reankylosis.
TMJ ankylosis treatment requires resection of the ankylotic bone creating a gap arthroplasty. In many cases resecting bone formation at the skull base is difficult [12, 13, 21,22,23]. There is a high risk of damaging the internal maxillary artery and nerve injuries or even duramater exposure with secondary cerebrospinal fluid leak. Surgical cutting guides and image-guided navigation are useful tools in these surgical procedures. Reconstruction of the mandibular condyle can be performed with autologous grafts or alloplastic materials, but total joint prostheses have a significantly higher success rate than autogenous tissues [24, 25]. In most adolescent and adult cases, a TMJ total joint prosthesis along with fat grafts packed around the articular area of the prostheses to maximize success and eliminate the risk of reankylosis is the treatment of choice [18, 19, 24,25,26,27]. Surgery can be performed in one or two surgical stages. Custom-made prostheses or stock prostheses can be used to reconstruct the resected mandible and the skull base. In one-stage procedures, the use of custom-made prostheses works well in the hands of the experienced surgeon but, for less experienced surgeons, could be more difficult because the resection must be exactly the same as performed presurgery on the 3D stereolithic model.
In some cases, a stock prosthesis can be adapted to the new anatomic configuration with less accuracy requirements. In the case of two-stage surgical approach, both custom-made and stock prosthesis can be used, but for most cases a custom-made prosthesis is recommended to provide the optimal outcome. In the first surgical stage, only resection of the ankylosed bone is performed, creating a gap between the skull base and the mandibular ascending ramus. To maintain this gap and avoid reankylosis, an acrylic, silicone ball, or orthopedic bone cement spacer can be placed into the gap so as to help maintain the mandibular position and eliminate dead space until the second stage of surgery can be performed. A CBCT or CT is obtained after the first surgical stage to facilitate the manufacture of a custom-made prosthesis. Once the prosthesis is manufactured, the second-stage surgery to place the prosthesis and concomitantly reposition the mandible, if indicated, can be completed along with the fat grafts packed around the articulating area of the prostheses as shown in (Fig. 7.23). The protocol of using custom-fitted total joint prostheses in conjunction with packing fat grafts around the functional aspect of the prostheses in a single-stage or two-stage procedure provides the best prognosis in the management of TMJ ankylosis [24,25,26,27].
8 TMJ Tumors
Tumors of the mandibular condyle are uncommon. Osteochondroma is one of the most common benign tumors of the general skeleton and also the most common tumor to develop in the mandibular condyle [14, 28, 29]. This condylar pathology can develop at any age (although more commonly during the teenage years), with a unilateral vertical overgrowth deformity of the jaws, although a horizontal growth vector can occasionally occur. The growth process can continue indefinitely with progressive worsening of the facial asymmetry. There are two subcategories dependent on the morphology of the tumor. According to Wolford’s classification [28, 29], CH Type 2A indicates a predominant vertical direction of condylar tumor development with relatively normal condylar morphology, although enlarged. CH Type 2B indicates a significant horizontal exophytic tumor mass growing from the condyle in addition to the vertical growth component. CH Type 3 are benign tumors other than osteochondroma (Case 5, Figs. 7.23, 7.24, 7.25, 7.26, 7.27, 7.28, and 7.29), and CH Type 4 are malignant tumors.
Although many surgeons prefer to treat only the TMJ pathology and ignore the associated dentofacial deformity, the definitive surgical protocol recommended to treat this pathology and associated dentofacial deformity has been previously published [28, 29] and includes (1) low condylectomy removing the ipsilateral condyle at the condylar base, preserving the condylar neck; (2) reshaping the condylar neck to function as the new condyle; (3) repositioning the articular disc over the top of the condylar neck and stabilize with a Mitek anchor; (4) repositioning the articular disc on the contralateral side with a Mitek anchor, when displaced; (5) double-jaw orthognathic surgery to correct the associated maxillary and mandibular deformities using VSP; and (6) inferior border ostectomy on the ipsilateral side to reestablish vertical height balance of the mandibular ramus, body, and symphysis if indicated. For the purpose of this chapter, Case 4 represents the treatment of this pathology with removal of a right TMJ tumor and immediate reconstruction with a Biomet total joint prosthesis without orthognathic surgery.
An alternative approach that some surgeons prefer for these types of cases is to treat in two stages where the low condylectomy and disc repositioning are performed at the first stage and the orthognathic surgery is completed at the second stage. In these cases, VSP and guiding surgical templates facilitate the diagnosis of the facial deformity, treatment planning, accurate osteotomies, and contouring of the mandibular border, when indicated [6, 8, 21,22,23, 28, 29].
9 TMJ Arthroscopy
Computer-assisted arthroscopy [6] may help guiding the position of the arthroscope and the instruments used in difficult clinical cases (obese patients, ankylosis, or patients previously treated with severe fibrosis of the TMJ). The main drawback of this technique is that only bony structures can be used as reference points. Also, some authors have described the use of navigation to enhance different TMJ arthroscopic procedures, eliminating the possibility of error in access [23].
10 Treatment Outcomes with TMJ Reconstruction
Most of the studies on treatment outcomes for TMJ total joint prostheses also include concomitant orthognathic surgery procedures. Dela Coleta et al. [30] evaluated 47 female patients for surgical stability following bilateral TMJ reconstruction using TMJ Concepts patient-fitted TMJ total joint prostheses, TMJ fat grafts, and counterclockwise rotation of the maxillo-mandibular complex with Menton advancing an average of 18.4 mm and the occlusal plane decreasing an average of 14.9°. Average follow-up was 40.6 months. Results demonstrated minor maxillary horizontal changes, while the mandibular measurements remained very stable.
Pinto et al. [31] evaluated the same 47 female patients relative to pain and dysfunctional outcomes. Patients were divided into two groups based on the number of previous surgeries: Group 1 had 0–1 previous surgeries, while Group 2 had two or more previous surgeries. Significant improvements (37–52%) were observed for TMJ pain, headaches, jaw function, diet, and disability. MIO increased 14%. Group 1 patients had better pain and jaw function results than Group 2 patients. For patients who did not receive fat grafts around the prostheses and had previous failure of PT-SR TMJ implants, more than half required secondary surgery including TMJ debridement for removal of FBGCR, fibrosis, and/or heterotopic bone formation. Following the secondary surgery consisting of joint debridement and placement of fat grafts, the patients had significant improvement, with no recurrence of the heterotopic bone. These two studies demonstrated that end-stage TMJ patients could be treated in one operation with TMJ Concepts patient-fitted TMJ total joint prostheses, fat grafts, and maxillo-mandibular counterclockwise rotation, for correction of an associated dentofacial deformity with good stability and improvement in pain and TMJ function.
Although the life expectancy of the TMJ Concepts device is unknown, Wolford, et al. [32] published a 20-year follow-up study of 56 patients who had received the Techmedica total joint prostheses between 1989 and 1993. There were statistically significant improvements in all parameters including incisal opening, jaw function, TMJ pain, and diet, with 85.7% of the patients reporting significant improvement in their quality of life. The greater the number of previous TMJ surgeries, patients reported a lower degree of subjective improvement, but they did report increased objective mandibular function and improved quality of life. There were no reports of device removal due to material wear or failure.
Numerous studies have been published in reference to outcome data using patient-fitted TMJ total joint prostheses. A summary of these publications has produced the following facts in reference to the TMJ Concepts total joint prostheses:
-
1.
TMJ Concepts prostheses are superior to autogenous tissues for end-stage TMJ reconstruction relative to subjective and objective outcomes.
-
2.
After two previous TMJ surgeries, autogenous tissues have a very high failure rate, whereas patient-fitted total joint prostheses have a high success rate.
-
3.
No donor site morbidity.
-
4.
Increased number of previous TMJ surgeries produces a lower level of improvement related to pain and function outcomes compared to patients with 0–1 previous TMJ surgeries.
-
5.
Failed TMJ alloplastic reconstruction (i.e., P/T, Silastic, metal-on-metal articulation, etc.) can create a foreign-body giant cell reaction and/or metallosis, best treated by joint debridement and reconstruction with patient-fitted total joint prostheses.
-
6.
Fat grafts packed around the articulating area of the prostheses improves outcomes relative to decreased pain, improved jaw function, and decreased requirement for repeat surgery.
-
7.
Osseointegration of the TMJ Concepts fossa and mandibular components occurs and is important for long-term stability.
-
8.
Posterior stop on the fossa component is important to stabilize the joint, jaw position, and occlusion.
-
9.
Concomitant orthognathic surgery can be performed at the same time as the TMJs are reconstructed.
-
10.
A 20-year follow-up study that demonstrated improvements in pain, jaw function, diet, incisal opening, and quality of life.
During the past 28 years, major advancements have been made in TMJ diagnostics and the development of surgical procedures to treat and rehabilitate the pathological, dysfunctional, and painful TMJ. Research has clearly demonstrated that TMJ and orthognathic surgery can be safely and predictably performed at the same operation, but it does necessitate the correct diagnosis and treatment plan, as well as requires the surgeon to have expertise in both TMJ and orthognathic surgery. The surgical procedures can be separated into two or more surgical stages, but the TMJ surgery should be done first. With the correct diagnosis and treatment plan, combined TMJ and orthognathic surgical approaches provide complete and comprehensive management of patients with coexisting TMJ pathology and dentofacial deformities. The application of computer-assisted surgical simulation (CASS) with virtual surgical planning (VSP) for C-TJR-OS cases requiring TMJ reconstruction with patient-fitted total joint prostheses and orthognathic surgery has significantly improved treatment quality by decreasing the preoperative workup time and increasing the accuracy of surgical preparation and subsequent surgery.
References
Edwards SP. Computer-assisted craniomaxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2010;22(1):117–34.
Bell RB. Computer planning and intraoperative navigation in cranio-maxillofacial surgery. Oral Maxillofac Surg Clin North Am. 2010;22(1):135–56.
Gateno J, Xia JJ, Teichgraeber JF, Christensen AM, Lemoine JJ, Liebschner MA, et al. Clinical feasibility of computer-aided surgical simulation (CASS) in the treatment of complex cranio-maxillofacial deformities. J Oral Maxillofac Surg. 2007;65(4):728–34.
Stokbro K, Aagaard E, Torkov P, Bell RB, Thygesen T. Virtual planning in orthognathic surgery. Int J Oral Maxillofac Surg. 2014;43(8):957–65.
Uribe F, Janakiraman N, Shafer D, Nanda R. Three-dimensional cone-beam computed tomography-based virtual treatment planning and fabrication of a surgical splint for asymmetric patients: surgery first approach. Am J Orthod Dentofacial Orthop. 2013;144(5):748–58.
Wolf J, Weiss A, Dym H. Technological advances in minimally invasive TMJ surgery. Dent Clin North Am. 2011;55(3):635–40, xi.
Zweifel DF, Simon C, Hoarau R, Pasche P, Broome M. Are virtual planning and guided surgery for head and neck reconstruction economically viable? J Oral Maxillofac Surg. 2015;73(1):170–5.
Li Y, Jiang Y, Ye B, Hu J, Chen Q, Zhu S. Treatment of dentofacial deformities secondary to osteochondroma of the mandibular condyle using virtual surgical planning and 3-dimensional printed surgical templates. J Oral Maxillofac Surg. 2016;74(2):349–68.
Chang HW, Lin HH, Chortrakarnkij P, Kim SG, Lo LJ. Intraoperative navigation for single-splint two-jaw orthognathic surgery: from model to actual surgery. J Craniomaxillofac Surg. 2015;43(7):1119–26.
Yeung RW, Xia JJ, Samman N. Image-guided minimally invasive surgical access to the temporomandibular joint: a preliminary report. J Oral Maxillofac Surg. 2006;64(10):1546–52.
Mischkowski RA, Zinser MJ, Kubler AC, Krug B, Seifert U, Zoller JE. Application of an augmented reality tool for maxillary positioning in orthognathic surgery—a feasibility study. J Craniomaxillofac Surg. 2006;34(8):478–83.
Movahed R, Teschke M, Wolford LM. Protocol for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery utilizing computer-assisted surgical simulation. J Oral Maxillofac Surg. 2013;71(12):2123–9.
Movahed R, Wolford LM. Protocol for concomitant temporomandibular joint custom-fitted total joint reconstruction and orthognathic surgery using computer-assisted surgical simulation. Oral Maxillofac Surg Clin North Am. 2015;27(1):37–45.
Wolford LM, Cassano DS, Goncalves JR. Common TMJ disorders: orthodontic and surgical management. In: McNamara JA, Kapila SD, editors. Temporomandibular disorders and orofacial pain: separating controversy from consensus, Craniofacial growth series, vol. 46. Ann Arbor: The University of Michigan; 2009. p. 159–98.
Wolford LM, Dhameja A. Planning for combined TMJ arthroplasty and orthognathic surgery. Atlas Oral Maxillofac Surg Clin North Am. 2011;19(2):243–70.
Wolford LM. Postsurgical patient management. In: Fonseca R, Marciani R, Turvey T, editors. Chapter 19: Oral and maxillofacial surgery, vol. III. 2nd ed. St. Louis: Saunders; 2008. p. 396–418.
Wolford LM, Rodrigues DB, Limoeiro E. Orthognathic and TMJ surgery: postsurgical patient management. J Oral Maxillofac Surg. 2011;69(11):2893–903.
Wolford LM, Karras SC. Autologous fat transplantation around temporomandibular joint total joint prostheses: preliminary treatment outcomes. J Oral Maxillofac Surg. 1997;55(3):245–51; discussion 251–2.
Mercuri LG, Ali FA, Woolson R. Outcomes of total alloplastic replacement with periarticular autogenous fat grafting for management of reankylosis of the temporomandibular joint. J Oral Maxillofac Surg. 2008;66(9):1794–803.
McPhillips A, Wolford LM, Rodrigues DB. SAPHO syndrome with TMJ involvement: review of the literature and case presentation. Int J Oral Maxillofac Surg. 2010;39:1160–7.
Malis DD, Xia JJ, Gateno J, Donovan DT, Teichgraeber JF. New protocol for 1-stage treatment of temporomandibular joint ankylosis using surgical navigation. J Oral Maxillofac Surg. 2007;65(9):1843–8.
Yu HB, Shen GF, Zhang SL, Wang XD, Wang CT, Lin YP. Navigation-guided gap arthroplasty in the treatment of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2009;38(10):1030–5.
Wagner A, Undt G, Watzinger F, Wanschitz F, Schicho K, Yerit K, et al. Principles of computer-assisted arthroscopy of the temporomandibular joint with optoelectronic tracking technology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(1):30–7.
Wolford L, Movahed R, Teschke M, Fimmers R, Havard D, Schneiderman E. Temporomandibular joint ankylosis can be successfully treated with TMJ concepts patient-fitted total joint prosthesis and autogenous fat grafts. J Oral Maxillofac Surg. 2016;74:1215–27.
Wolford L. Diagnosis and management of TMJ heterotopic bone and ankylosis. In: Bouloux GF, editor. Complications of temporomandibular joint surgery. Cham: Springer; 2017. p. 111–33.
Wolford LM, Morales-Ryan CA, Garcia-Morales P, Cassano DS. Autologous fat grafts placed around temporomandibular joint (TMJ) total joint prostheses to prevent heterotopic bone. Baylor Univ Med Center Proc. 2008;21:248–54.
Wolford LM, Cassano DS. Autologous fat grafts around temporomandibular joint (TMJ) total joint prostheses to prevent heterotopic bone. In: Shiffman MA, editor. Autologous fat transfer. Berlin: Springer; 2010. p. 361–82.
Wolford LM, Movahed R, Perez D. A classification system for conditions causing condylar hyperplasia. J Oral Maxillofac Surg. 2014;72:567–95.
Wolford LM, Movahed R, Dhameja A, Allen WR. Low condylectomy and orthognathic surgery to treat mandibular condylar osteochondroma: retrospective review of 37 cases. J Oral Maxillofac Surg. 2014;72:1704–28. https://doi.org/10.1016/j.joms.2014.03.009.
Dela Coleta KE, Wolford LM, Goncalves JR, Pinto Ados S, Pinto LP, Cassano DS. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ concepts total joint prostheses: part I–skeletal and dental stability. Int J Oral Maxillofac Surg. 2009;38(2):126–38.
Pinto LP, Wolford LM, Buschang PH, Bernardi FH, Goncalves JR, Cassano DS. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ concepts total joint prostheses: part III–pain and dysfunction outcomes. Int J Oral Maxillofac Surg. 2009;38(4):326–31.
Wolford LM, Mercuri LG, Schneiderman ED, Movahed R, Allen W. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ concepts device. J Oral Maxillofac Surg. 2015;73(5):952–60.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Wolford, L., Sanroman, J.F. (2019). Surgery of the Temporomandibular Joint: Virtual Planning. In: Connelly, S.T., Tartaglia, G.M., Silva, R.G. (eds) Contemporary Management of Temporomandibular Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-99909-8_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-99909-8_7
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99908-1
Online ISBN: 978-3-319-99909-8
eBook Packages: MedicineMedicine (R0)