Abstract
Unassisted coiling is a safe and effective treatment strategy for both ruptured and unruptured aneurysms with favorable anatomy. Those aneurysms best suited for unassisted coiling have straightforward microcatheter access, are small or medium sized, have a narrow neck, and a high dome/neck ratio. Aneurysms with wide necks or incorporate bifurcating branches are less favorable due to the possibility of coil prolapse and thromboembolic complication. A wide selection of different microcatheter shapes and coil conformations is available to tailor the treatment to unique aneurysm anatomy. Operators should prepare for the potential need for additional microcatheters by using an appropriately sized guide catheter (usually 6 French), should dual microcatheter technique or balloon or stent assistance be required. Overall, outcomes with unassisted coiling of appropriate aneurysms are excellent, with retreatment rates approximating 15%. In this chapter, we discuss indications and contraindications for primary coiling, basic principles of catheterization, coil selection, coil deployment, and outcomes associated with unassisted aneurysm coiling.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Aneurysm coil embolization
- Coil embolization
- Endovascular
- Occlusion
- Unassisted aneurysm coil embolization
The invention of the detachable coils by Guglielmi and colleagues in the late 1980s [1, 2] and the period of rapid endovascular technological innovation that followed have revolutionized the way that cerebral aneurysms are being treated. The development of new coil technologies with a wide variety of shapes, sizes, and materials, as well as enhanced detachment mechanisms, more navigable catheters, and refinement of procedural techniques, has further widened the applicability of endovascular coil embolization to a spectrum of aneurysms that traditionally would have been treated only with surgical clipping. Coil-assisted devices, such as self-expanding implantable stents and balloon microcatheters, have allowed neurointerventionists to improve angiographic occlusion and reduce recurrence rates for wide-necked aneurysms or those with challenging morphology. The latest additions to the endovascular armamentarium, flow-diverting stents and intrasaccular devices, provide further options for treating challenging fusiform dissecting aneurysms or challenging bifurcation aneurysms. The success of minimally invasive endovascular techniques has led many centers to now preferentially treat the majority of cerebral aneurysms via endovascular approaches.
Although there is a large assortment of endovascular devices and techniques to choose from, there is a subset of patients where primary coiling remains the preferred treatment option. In many instances, aneurysms have straightforward anatomy and can be treated easily and safely with unassisted coiling. In a recent survey of US physicians that treat brain aneurysms, over 50% of respondents reported that they recommended treatment of most unruptured posterior communicating artery, anterior communicating artery, and vertebral-posterior inferior cerebellar artery aneurysms with primary coiling as opposed to other open or endovascular approaches (unpublished data). This chapter will describe the indications and contraindications to unassisted coiling, basic techniques, coil selection strategies, and outcomes associated with this technique.
Indications for Unassisted Coil Embolization
The decision to pursue endovascular treatment of an aneurysm is based on patient factors, aneurysm location and morphology, and physician preference. Once endovascular management has been decided, the primary factor determining candidacy for unassisted coiling is aneurysm morphology. Cerebral aneurysms are classically divided into two main subtypes based on broad morphology: saccular (berry) and fusiform. Saccular aneurysms are true aneurysms that are outpouchings of arteries, usually at branching points, into the subarachnoid space. Anatomically, a saccular aneurysm is differentiated from the normal parent vessel by the aneurysm neck, which is the segment of the aneurysm separating the dome (or main compartment of the aneurysm) from the underlying parent vessel. The aneurysm neck may be long and clearly delineated or may be very short and wide. In most cases, the aneurysm neck has a relatively well-defined anatomic location that can be drawn as a line separating normal parent vessel from aneurysm. Histologically, the aneurysm dome is composed of thickened intima and muscularis without an internal elastic lamina. The normal muscularis layer and internal elastic lamina of the parent artery stop abruptly at the aneurysm neck. Failure to obliterate the histologically diseased neck during treatment may allow for progressive regrowth and recurrence with continued hemodynamic stresses. Successful coil embolization is therefore dependent upon obliteration of the aneurysm dome, to prevent future hemorrhage; occlusion of the aneurysm-parent vessel interface (the “neck”), to prevent aneurysm recurrence; and sparing of the parent vessel to prevent thromboembolic complications. As such, the aneurysm neck represents an important histologic, anatomic, and angiographic landmark that must be respected when selecting treatment strategies.
Saccular aneurysms come in a variety of shapes and sizes that may differ based on the location of the parent vessels and size and orientation of the bifurcating branches. Aside from standard measurements of aneurysm maximum dome diameter, width, height, and neck size, one very useful means of quantifying aneurysm morphology is by calculating the dome/neck ratio. This ratio is calculated by dividing the maximum width (or length) of the dome by the maximum length of the neck. Most aneurysms have a dome/neck ratio that falls somewhere between 0.5 and 5. A high dome/neck ratio indicates a larger aneurysm dome with a comparatively narrower neck, while a low dome/neck ratio indicates a smaller aneurysm dome with a wider neck.
A high dome/neck ratio is favorable for coil embolization, while a low dome/neck ratio makes endovascular treatment more challenging (Fig. 10.1). Coil technologies are characterized by differing loop sizes, length, and shape, but most coil loops are round in conformation. Larger coil diameters have larger loops, which are less likely to prolapse through a considerably narrower neck into the parent vessel. The larger the disparity between dome width and neck size, the greater the packing density that can be obtained as the larger framing coils are less likely to be forced through the neck during coiling. On the other hand, aneurysms with low dome/neck ratios may be challenging to treat with primary coiling. Coil loops that are smaller than the neck width may very easily prolapse down into the parent vessel, as there is no inferior wall to buttress them into position within the dome. Consequently, satisfactory packing density may not be obtainable as further packing with coils could force loops of coil downward into the parent vessel, increasing the risk of potential thromboembolic complication. In situations where the dome/neck ratio is low, coil-assisted techniques using an adjunctive balloon catheter or self-expanding stent should be considered up front to aid in obtaining adequate packing density and protecting the parent vessel from coil prolapse. While aneurysm morphology is highly variable and the anatomical considerations should be considered on a case-by-case basis, a neck width of more than 4 mm or a dome/neck ratio of less than 2 is considered by many to represent the threshold for a “wide-necked” aneurysm. In cases meeting these criteria, consideration of alternative endovascular strategies or surgical clipping is encouraged, although many wide-necked aneurysms with dome/neck ratios of 1–2 may be treated safely and effectively with primary coiling. Those aneurysms with dome/neck ratios of less than 1 are probably poor candidates for unassisted coiling (Table 10.1). Consequently, fusiform cerebral aneurysms, which have no defined neck and therefore no way to keep coils from intruding upon flow through the parent vessel, should not be treated with unassisted coiling.
Large and giant aneurysms (those with maximum diameters of 15 mm or greater) have historically high recurrence rates with endovascular techniques [3, 4]. Progressive recanalization has been reported in as high as 43–69% of large or giant aneurysms treated with unassisted coiling in some series [5]. Poor angiographic outcomes with primary coiling are largely secondary to progressive coil compaction that occurs in the months that follow coil embolization. With stent-assisted coiling or adjunctive flow diversion, considerably improved success rates are now being achieved. Improved outcomes associated with the use of stents are likely secondary to not only a flow-diverting effect but also enhanced endothelialization across the aneurysm neck from the stent lattice. Similarly, the use of a stent or balloon may improve packing density during coiling, which may help to prevent recurrence. When able, physicians should consider using coil-assisted techniques when treating large or giant aneurysms.
Other important anatomical factors should be considered in determining candidacy for treatment. Bifurcation aneurysms, such as those at the middle cerebral artery (MCA) or basilar apex, may incorporate bifurcating branches into the aneurysm neck. For instance, basilar apex aneurysms often have one or both posterior cerebral artery P1 segments incorporated into a wide neck. Even minor encroachment of coil mass into these bifurcating branches may place the patient at high risk for thromboembolic complication. In these situations, protection of the bifurcating branches with balloon or stent assistance may be preferred. New intrasaccular devices may also be preferred in challenging bifurcation aneurysms. Additionally, MCA aneurysms treated with coiling have historically inferior complete occlusion rates compared to surgical clipping. Therefore physicians should consider adjunctive treatments at the MCA bifurcation if endovascular treatment is chosen.
Finally, there are other important considerations when electing an endovascular strategy. Unassisted coil embolization is often the technique of choice when treating simple aneurysms after acute rupture as it does not require the use of dual antiplatelet agents, which is particularly important if external ventricular drainage or other procedures are necessary. Oftentimes challenging or complex aneurysms may be treated in a staged fashion, with an intentional subtotal unassisted coiling or balloon-assisted coiling procedure to secure the aneurysm but leaving a neck residual, followed by a definitive flow diverter or stent-assisted coiling procedure once dual antiplatelet agents can be safely used [6]. While re-treating aneurysms that have previously been treated with unassisted coiling and have recurred is an option, those that require retreatment should probably be treated definitively with an adjunctive assist technique or with flow diversion, if possible, to promote thrombosis. Lastly, aneurysms that are difficult to catheterize or are prone to catheter prolapse, such as ophthalmic aneurysms with an acute angle between the internal carotid artery and an anterosuperiorly directed dome, can often be successfully treated with flow diversion, which does not require aneurysm catheterization.
Basic Techniques
Preparation and Access
Prior to obtaining vascular access, the interventionalist should develop a procedural plan and evaluate for potential pitfalls. First, patients with severe tortuosity, advanced age, severe peripheral vascular disease, and posterior circulation aneurysms may be good candidates for transradial or transbrachial arterial access, as opposed to transfemoral. Direct carotid puncture is also an option for patients with challenging anterior circulation access as it usually provides robust and stable access for carotid circulation aneurysms but has an inherent risk of carotid dissection. Appropriate guide catheters, sheaths, or intermediate catheters should be selected that provide the proximal support necessary to catheterize the aneurysm. Second, interventionalists should develop a backup plan should unassisted coiling be insufficient or should complication occur. For instance, using a 6-French guide catheter allows for placement of a second microcatheter for balloon or stent assistance or for dual microcatheter technique yet still allows for angiographic runs to be performed through the guide catheter. During the treatment of ruptured aneurysms, it is wise to have a balloon microcatheter preselected and available should aneurysm perforation occur. Alternatively, should coil loops prolapse into the parent vessel, having a backup plan for either balloon-assisted or stent-assisted coiling is wise.
Once access has been obtained, a 6-French guiding catheter is positioned in the origin of the vessel through which coiling of the aneurysm will be performed. Intra-arterial verapamil may then be administered to prevent or relieve vasospasm. Using road map guidance, the guide catheter is placed as distal as safely possible. The closer the guide catheter is to the aneurysm, the better control the operator will have over the microcatheter. This is particularly important when there are a number of vessel loops between the guide catheter and the aneurysm, such as in anterior communicating artery aneurysms, where the microcatheter must navigate through the carotid siphon and then into the A1 segment. Placing the guiding catheter into the petrous carotid segment may be preferable in such cases. Stability of the guide catheter is necessary for successful microcatheter navigation. If stable purchase cannot be obtained, consideration of a coaxial system or alternate access site is encouraged. Following placement of the guide catheter, administration of intravenous heparin should be considered (if not already administered), depending on the patient’s circumstances. The guide catheter is usually connected to a continuous heparinized saline flush during the entirety of the coiling procedure to prevent stagnation of blood in the catheter, which could result in thromboembolism.
Working Views
Baseline anteroposterior and lateral cerebral angiography should be performed to develop a pretreatment understanding of the patient’s anatomy. This will be helpful when reviewing posttreatment angiography as a comparator when detecting potential procedural complications, such as thromboembolism. Next, angiographic working views should be obtained. These fluoroscopic positions are extremely important for successful aneurysm treatment because they provide visualization of the necessary anatomy and are often the only views used throughout the entirety of the embolization procedure. Failure to obtain adequate working views may result in inadvertent coil placement into the parent or bifurcating vessel, aneurysm perforation, or failure to obtain satisfactory aneurysm occlusion. The most important factors to consider when selecting working views are shown in Table 10.2. Three-dimensional angiography may be performed to assist with understanding aneurysm morphology and selection of an appropriate view. Most importantly, working views should clearly show (1) the relationship between the aneurysm neck, parent vessel, and any bifurcating branch origins and (2) the guide catheter tip and exposed microcatheter on at least one view. The inability to meet the minimum necessary criteria with a given set of working views should prompt consideration of obtaining new views (with three-dimensional angiography assistance) or consideration of alternate treatment strategies, such as flow diversion or the use of balloon or stent assistance. As these views are integral to providing satisfactory aneurysm treatment and avoiding complications, the importance of adequate working views cannot be understated.
Aneurysm Catheterization
Once satisfactory working views have been obtained, a microcatheter and microwire are selected for aneurysm catheterization. The selection of wire and microcatheter is often based on physician preference. Often, a 10, 14, or 17 catheter (inner diameter of 0.014 or 0.017 inches, all capable of housing a 0.014 inch microwire and most coil technologies) is used. Additionally, pre-shaped microcatheters (curved, 45° and 90°) are available that may assist with aneurysm catheterization or coiling based on aneurysm anatomy, though most aneurysms can be accessed with a straight microcatheter. Steam-shaping of straight microcatheter tips may also be performed based on physician preference. Microwire selection is often based on preference, but certain qualities should be strongly considered. Microwires should be steerable (torque applied to the wire reliably results in rotation of the wire in the patient), have an atraumatic tip, and provide adequate support to allow the microcatheter to climb over the wire when advanced without the wire losing its position. Shaping of the microwire is necessary to allow for steering into branches or the aneurysm ostium.
There are multiple techniques for microcatheter and microwire navigation. The technique used is often based on training style but also the number of surgeons present. Single individual procedural techniques include the underhand and overhand techniques, while if two surgeons are present, a dual-surgeon technique can be used. In both single-surgeon techniques, the left hand is placed on the microcatheter just proximal to the guide catheter and is used to advance or withdraw the microcatheter. Synchronously, the right hand is used to spin, advance, or withdraw the microwire either with the palm up (underhand) or palm facing down (overhand). In the dual-surgeon technique, the microcatheter is controlled by one surgeon, while the microwire is controlled by the second.
A major principle of microcatheter and microwire navigation involves the concept of “load” (or “tension”) within the system. In a perfect system, advancement of the microcatheter into the guide catheter by a distance of 1 mm will result in 1 mm of forward motion of the microcatheter on fluoroscopy. This concept is often referred to as “one-to-one movement,” because for every unit of distance, the microcatheter is advanced outside the patient and an equal distance is traveled by the microcatheter tip within the patient. The presence of one-to-one movement is highly favorable for catheter navigation because the operator has complete control over catheter movement. The presence of one-to-one movement also indicates a little forward load or tension within the system. However, in most cases, vascular looping or tortuosity results in a loss of one-to-one movement as the microcatheter interacts with the vessel walls and builds up load within the loops. For instance, as the microcatheter and wire are advanced through the carotid siphon, increased forward load is required to move the catheter distally. This load is reflected in external displacement of the microcatheter between the lesser (short) curve of the vessel to the greater (long) curve and proximal displacement of the guide catheter tip (Fig. 10.2). Excessive load within the system results in a loss of fine control of the microcatheter and wire steering but can also result in sudden release of that potential energy into the catheter tip, resulting in “jumping” of the microcatheter and wire forward. Therefore, failure to recognize the buildup of load in the system when attempting to catheterize the aneurysm can lead to sudden aneurysm perforation by the wire and catheter launching forward unexpectedly. Alternatively, excessive load may cause proximal displacement of the guide catheter, resulting in the system prolapsing into the aorta, or looping of the microcatheter proximally. Load can be removed from the system by withdrawing the microcatheter slowly, which results first in the shifting of the exposed catheter from the greater curves to the lesser curves of the proximal vessels and then second in proximal movement of the catheter tip. Therefore, understanding the load in the system comes not only from appreciating the loss of one-to-one movement but also by constant appreciation of the guide catheter tip and the movement of the exposed microcatheter within the greater and lesser curves of the vessels proximal to the aneurysm. This fact underlies the importance of having the guide catheter tip and microcatheter length viewable on at least one working view and further supports the concept of placing the guide catheter as distally as safely possible.
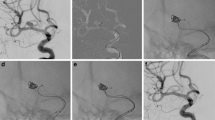
Catheterization of the aneurysm. The short (lesser) and long (greater) curves are shown in green and yellow, respectively (a). The microwire and microcatheter are advanced proximal to the aneurysm. Doing so introduces load into the system, reflected by the microcatheter pushed externally to the greater vessel curves and descent of the guide catheter (b). Load is removed from the system by gently withdrawing the microcatheter, resulting in the guide catheter returning to its previous position and the microcatheter shifting to the lesser curves. The microwire is then advanced into the aneurysm (c). The wire is pinned, and the mirocatheter is advanced over the wire into the aneurysm, just beyond the neck. Note that load is again introduced into the system with this maneuver (d). With the catheter in the desired position, a small amount of load is once again removed (e). Note that the microcatheter tip position does not change but instead the shape of the exposed microcatheter. The wire is then gently removed from the microcatheter (f). A framing coil is then deployed into the aneurysm (g). Oftentimes this may require forward load on the microcatheter if the coil pushes the microcatheter proximally. Coiling is then completed (h)
Under road map guidance using the working view, the microcatheter and microwire are then carefully and slowly navigated to the aneurysm (Fig. 10.2). This is performed by leading with the microwire and gently spinning the wire so that it steers in the direction of interest. Control of the wire is enhanced by having proximal support from the microcatheter, so after the wire is advanced a reasonable distance without the catheter, it is helpful to “pin” the wire by holding it in place and then advancing the microcatheter to a point near the wire tip. The wire is then slowly steered and advanced forward. This process is repeated until the microcatheter and wire are near the aneurysm neck. Attention should be paid toward inadvertent advancement of the wire into tiny perforating branches so that this can be immediately recognized and/or avoided.
Catheterization of the aneurysm is then performed by slowly and carefully advancing the microwire into the aneurysm. Contact with the aneurysm dome wall by the microwire is not necessary or recommended. Next, with appreciation of the load within the system, the microcatheter is slowly advanced over the microwire while pinning the microwire. Often, even with the microwire pinned, the microwire will continue to demonstrate subtle movements while the microcatheter is being advanced. This may necessitate slight withdrawal or advancement of the wire to hold a stable position. This “push and pull” is important for keeping a steady wire position, particularly when the system is under load. If one-to-one movement is absent with microcatheter advancement, extreme care is necessary when supplying forward force on the microcatheter. Often times removing load from the system before delicate microcatheter work will improve control. The microcatheter should then be advanced into the aneurysm over the wire, away from the aneurysm wall. If the catheter is too deep in the aneurysm and in contact with or near the aneurysm dome wall, there is a risk of perforation from the leading segment of the coil when it is deployed. In most cases, position of the microcatheter at, or just beyond, the neck is usually preferred. Once a satisfactory position is reached, the microcatheter is pulled back slightly to remove excess load from the system, which will subtly straighten the microcatheter in the proximal loops but not affect catheter tip position. Care must be taken with this step because if too much load is removed, the microcatheter tip may lose its position and fall into the parent vessel. The microwire is then removed under initial fluoroscopic visualization to ensure the catheter tip does not shift.
Aneurysmography
In complex aneurysms or those with unclear angioarchitecture, aneurysmography is a useful option. This angiographic technique involves the gentle injection of contrast dye through the microcatheter into the aneurysm using a 1 ml syringe. While the volume and force of injection is substantially less than that provided through the guide catheter, aneurysmography may be helpful in visualizing the relationship of the aneurysm neck, parent vessel, bifurcating branches, and dome anatomy. Further, because the injection is distal and localized, aneurysmograms usually provide an unobscured view without overlap from nonrelevant branches. Because of these factors, an aneurysmogram often serves as a superior road map for coiling.
Coil Selection
Since the first use of the Guglielmi detachable coil, coil technology has rapidly evolved with an ever-increasing number of new products from a variety of companies in the market. Most experienced neurointerventionists have their “go-to” coils for their cases which they use based on personal experience. Many physicians have thus developed an algorithm in coil selection that has developed over the years depending on operator experience, availability, cost, and ease of use. There are however practical considerations that can aid the proceduralist in objectively choosing the most appropriate coil for a case.
Basic Coil Design
One of the most important factors in coil design is compatibility with the host. A biocompatible coil should be composed of inert material that allows an effective treatment without the concern for an adverse systemic host response. Metal strength is determined experimentally and is referred to as the shear modulus. The shear modulus is the coefficient of elasticity for a shearing force, defined as the ratio of the shear stress to the shear strain.
A platinum (92%)/tungsten (8%) alloy has become the mainstay material for most current coil designs [7]. This alloy has been shown to be a safe and inert alloy for deployment inside the cerebral vasculature [8]. There are some vendors who offer lines of coils with coating to cause increased fibrosis in aneurysms, such as hydrogel-coated coils. These bioactive coils may promote aneurysm occlusion but have also been associated with hydrocephalus [9].
The intravascular behavior of a coil is the result of an interaction between the primary material, resistance to deformity (stiffness, secondary and tertiary structures), and the mechanism of detachment. All coils start off as a basic platinum alloy wire. The diameter of this wire, which can be highly variable, is thought to be the most impactful factor in determining a coil’s stiffness. Usually, the larger the diameter of the stock wire (D1), the stiffer the coil. This straight stock wire is then wound around a mandrel, a straight metal rod in the case of coils, to give it the “slinky-like” structure. This is referred to as the coil’s primary wind (D2) or secondary structure. The mandrel can also be of variable sizes such that coils can be wound to produce highly variable secondary structure sizes.
This equation describes the relative contributions of the diameter of the stock wire (D1) and the primary wind (D2) to the spring constant or stiffness of the coil. G = shear modulus, n = number of turns per unit distance.
Usually, coils are described as a “10” or an “18” coil, with “10” coil referring to a secondary diameter thickness of 0.010 inch and “18” coil wound to 0.015 inch thickness. The 10 and 18 terminology is based on the old original Tracker 10 and 18 microcatheters. Many of the currently available coils have variable secondary diameters ranging from 0.010 to 0.015 inches. Once a secondary structure is established, a number of tertiary shapes and configurations are available to provide the advertised properties of being three-dimensional, spherical, complex, or helical (Fig. 10.3). The size of the tertiary shape is what the coil manufacturers advertise as the “size” or diameter of the coil. For example, a 5 mm coil will have a majority of coil loops that are 5 mm in diameter, irrespective of the tertiary shape [10].
(a, b) General coil shapes and coiling strategy. Helical coils have a predictable shape, while complex coils acquire unique conformations. Filling coils are designed to seek unfilled spaces within the aneurysm. In general, successful coiling is initiated with large framing coils, followed by smaller coils used to fill the spaces within the framing coils, and then finally very small finishing coils
The coil is attached to a rigid pusher wire that allows for advancement through the microcatheter. The attachment site (interface between coil and pusher) is the location of the detachment zone. A variety of detachment mechanisms are available for different coils including electrolytic, hydraulic, and mechanical. While the original electrolytic detachment system used by the Guglielmi coil notoriously took minutes to detach the coil, nearly all current detachment systems take mere seconds. There is currently no clear clinical advantage of any one system over another.
Coil Shapes
There are various shapes advertised for a plethora of coils with fancy names. There are however three main types of coils: framing coils, filling coils, and finishing coils.
Framing Coils
Framing coils are usually three-dimensional coils (3D), which are designed to form a stiff, peripheral basket (or “frame”) under the aneurysm wall as they exit the microcatheter tip. Therefore these ovalize or form a spherical shape. Usually one or two framing coils are used. Target 3D (Stryker Neurovascular, Fremont, California), Micrusphere 18, and Presidio 10 (Codman Neurovascular, Ratham, Massachusetts, USA) are some examples of commonly used framing coils. The coils are designed so that at least some of the coil loops extend across the aneurysm neck. They are stiff and offer slight centrifugal radial force to allow filling of the inner space of the basket with smaller size 3D coils in a Russian doll technique (onion skinning of progressively decreasing diameters of coils). Alternatively, the scaffold provided by the framing coil can be used to use filling or finishing coil to pack the aneurysm. As framing coils establish an important foundational coil mass boundary within the aneurysm that dictates the success of further coiling, the position of the framing coil when deployed should be an important consideration. Importantly, choosing an appropriately sized framing coil has a significant impact on the long-term outcomes, namely, recanalization and retreatment rates [11]. Therefore it is advisable to withdraw and then redeploy framing coils that fail to acquire the desired frame shape or to select alternate sizes or technologies if the frame that is created is undesirable.
Filling Coils
These coils are designed to occupy space within the frame created by the framing coil. These may be helical and have two-dimensional (2D) or random shapes. The 2D coils were originally designed to be framing coils with the first helical loop smaller than the rest, with the hope that the smaller loops would tumble within the aneurysm without finding the outflow to the parent vessel. These tend be softer coils and are used to pack the aneurysm.
Finishing Coils
When the aneurysm is at the final stages of embolization, these extremely soft coils can find places within the coil mesh and neck of the aneurysm to improve packing density. These are usually very small in diameter and very short in length. Importantly, due to their small size and length, there may be a higher risk of dislodgement from the aneurysm with prolapse into the parent artery.
General Coil Selection Strategy
In general for an unruptured saccular aneurysm, start with a framing 3D coil matched to the size of the diameter of the dome of the aneurysm. Some operators may oversize the coil by 1 mm to ovalize the aneurysm to theoretically narrow the neck and improve the dome/neck ratio. Most operators will match the aneurysm dome diameter to the coil diameter in a ruptured aneurysm. For an irregular nonspherical ruptured aneurysm, a mean measurement of the maximum dimensions may be the best indicator of an appropriate initial coil. Initial coil does not have to be a stiff 3D coil; soft filling coils may sometimes be used in very irregular-shaped ruptured aneurysm as framer or initial coils. Some coil designs have smaller initial loops that confine the first loop(s) to within the aneurysm, have extremely soft loops that can fill very irregularly shaped aneurysms, or simply have no tertiary shape at all, allowing progressive folding and/or filling irrespective of the size or shape of the aneurysm. In general, volume packing density between 25% and 33% usually provides adequate occlusion of the aneurysm with low recanalization rates [12, 13]. As a rule, the first and last coils are the most important to frame and occlude the aneurysm without complication. The first coil should be placed with limited repositioning to minimize the risk of disrupting intra-aneurysmal thrombus, and the final coil should occlude the neck without prolapsing coil into the parent vessel, to prevent a thrombogenic surface that could result in thromboembolism.
Dual Microcatheter Technique
The double or dual microcatheter technique to treat wide-necked intracranial aneurysms was originally described by Baxter et al. in 1998 [14]. In this technique, two microcatheters are navigated one after the other into the aneurysm such that they lie side by side within the neck or dome. A framing coil is initially deployed through one microcatheter but is not detached. Sequential placement of coils is then performed within the lattice of the initially deployed but not detached coil through the second microcatheter. This is performed until satisfactory occlusion of the aneurysm is seen. The initial coil is then detached. This technique is very useful in wide-necked aneurysms with incorporation of branch vessel origins in the aneurysm base. A common example would be a wide-necked basilar tip aneurysm with incorporation of bilateral posterior cerebral arteries. This technique results in stabilization of the tumbling of the initial coil with narrowing of the neck, preventing any coil prolapse into the parent artery, and can be very useful to prevent the need for stent assistance in the case of a ruptured aneurysm. The technique also theoretically would reduce thromboembolic events that can be associated with using a balloon remodeling technique.
Outcomes
Outcomes of coil embolization can be divided into four areas: clinical outcomes, rates of occlusion, durability, and rebleeding. There are caveats when looking at the literature, however. With inherent differences between ruptured and unruptured aneurysms, clinical outcomes and durability can differ between these groups. Additionally, with the technologic advancements in coils, balloon remodeling, and stent-assisted coiling, current outcomes of modern primary coiling alone are difficult to isolate; however, the following provides a synopsis of the historical and current literature.
Clinical outcome should be the cornerstone of the decision-making process, and outcomes are often compared to microsurgical clipping. To date, there have been three randomized, prospective studies comparing clipping and coiling of ruptured aneurysms [15,16,17,18]. The International Subarachnoid Aneurysm Trial (ISAT) demonstrated clinical superiority of coiling over clipping in 2143 patients (1594 available for a 12-month follow-up) who had aneurysms demonstrating clinical equipoise, namely, small- and medium-sized saccular Acom and Pcom aneurysms, with 23.7% (coiling) vs 30.6% (clipping) dead or dependent at 1 year [15]. This was again demonstrated in the Barrow Ruptured Aneurysm Trial (BRAT), which randomized all ruptured aneurysms and allowed for 38% crossover for optimal treatment, resulting in a 23.2% (coiling) vs 33.7% (clipping) rate of death or dependence at 1 year [16]. At 3 and 6 years, there was no benefit except in posterior circulation aneurysms [17]. In the Finnish randomized trial, MRI showed equal number of ischemic deficits in both groups at 1 year [18].
Outcomes in unruptured aneurysms have been less rigorously studied, but in a recent meta-analysis, database registry studies of unruptured aneurysms favored coiling over clipping with regard to independent outcome and lower mortality (OR = 0.34, CI 0.29–0.41, and OR = 1.74, CI 1.52–1.98, respectively) [19]. In the Matrix and Platinum Science (MAPS) trial, at 1 year 95.8% of patients with unruptured aneurysms (N = 398) and 90.4% (N = 228) of those with ruptured aneurysms were independent (mRS ≤ 2), though this included stent-assisted coiling in addition to primary coiling [20].
Safety is certainly paramount to any surgical technique. Reported rates of complications occurring during Guglielmi detachable coil embolization vary widely, with estimates ranging from 2.5% to 28% [21]. Murayama et al. reviewed 916 aneurysms undergoing coil embolization, with only 49 utilizing balloon assistance [22]. While the coil technology has since improved, this likely gives us the best assessment of pure risk of primary coil embolization. Patients were divided into an early (1990–1995) and late (1995–2002) cohort, due to improved experience and technology. Technical complications occurred in 69 patients (8.4%) [22]. Thromboembolic complications occurred in 4.4% of patients, including distal emboli and parent artery occlusion, of which 1% developed a permanent neurologic deficit with 0.6% mortality. Aneurysm perforation occurred in 2.3% with 1.4% neurologic morbidity and 0.7% mortality. Less frequent complications included arterial dissection (0.7%), coil migration (0.5%), coil rupture (0.4%), and new mass effect (0.1%). The later cohort (1995–2002) had an overall lower rate of intraprocedural complications (7.3 vs 11.3%) [22]. While advances in technology have created softer and more stable coils that may mitigate some of these complications, increasing case complexity, such as stent assistance and the concomitant use of dual antiplatelet agents, increases the risk for intraprocedural complications and new diffusion abnormalities on MRI [23].
Aneurysm occlusion is classically graded by the Raymond-Roy Occlusion Classification, where Class I indicates complete occlusion, Class II indicates residual neck, and Class III residual aneurysm filling [24]. In ruptured aneurysms, ISAT demonstrated a complete occlusion rate of 66%, as compared to 82% in clipped aneurysms [15]. BRAT showed an even lower occlusion rate with 48% Raymond-Roy Class I occlusion vs 96% complete obliteration with clipping [16]. Similarly, the MAPS, Cerecyte, and HELPS trials showed complete occlusion rates of 42–76%, including aneurysms treated with adjuvant balloon or stent remodeling [20, 25, 26]. Murayama et al. demonstrated a complete occlusion rate of 57% in the latter group of aneurysms undergoing primary coiling [22].
While the occlusion rate is significantly lower in coiled aneurysms than those clipped, it is the rate of rehemorrhage and retreatment that is clinically most important. Prevention of hemorrhage, or rebleeding, is the overarching benchmark of successful treatment. Raymond et al. demonstrated that recurrent aneurysms have a low incidence of rebleeding [27]. In 501 aneurysms, they showed a recurrence rate of 33.6% at 1 year, but a hemorrhage rate of only 0.8% over a mean clinical follow-up period of almost 3 years. ISAT had a relatively high rehemorrhage rate of 4.1% during the first year (3.6% in the clipping group), which then approached 0% in the 10 years of follow-up [15]. BRAT [16] and HELPS [26] demonstrated a 0% rehemorrhage rate, with CARAT [28], MAPS (1.3%) [20], and Cerecyte (0.2%) [25] also demonstrating very low rebleeding rates.
Durability includes the rates of recanalization as well as the rates of retreatment, perhaps and more clinically a relevant benchmark. As previously stated, volume packing density between 25% and 33% usually provides adequate occlusion of the aneurysm with low recanalization rates [12, 13]. Initial angiographic occlusion class is a predictor of aneurysm recurrence and rehemorrhage [27, 28]. Mascitelli et al. found that among Raymond-Roy Class III aneurysms, the subgroup with residual contrast opacification within the coil interstices (Class IIIa) was likely to improve to Class I or II on follow-up angiography, compared to aneurysms with contrast opacification along the aneurysm wall, outside of the coil mass (83.3 vs 15%, p < 0.01) [29]. Similar to the 33.6% recanalization rate in Raymond’s study [28], Murayama et al. demonstrated a 21% recanalization rate of aneurysms undergoing primary coiling [22]. Though recanalization rates have decreased with adjuvant treatment such as neck remodeling (BRAT showed a 10% recanalization rate over 6 years) [ 17], rates of retreatment are not insignificant. ISAT showed a 15% retreatment rate in the coil embolization group as compared to 4.1% in the clipping group [15]. BRAT showed a similar rate (16.4% (coil) vs 4.6% (clip)) [17].
In summary, when discussing treatment options with our patients, we counsel that the literature demonstrates that clinical outcome after coil embolization, especially within a year in those with ruptured aneurysms, is superior to microsurgical clipping. However, there is a significant chance of residual aneurysm and recanalization, resulting in a retreatment rate around 15%, but with good angiographic follow-up, the risk of rehemorrhage is exceedingly low.
Conclusions
Unassisted coiling is a safe and effective treatment strategy for both ruptured and unruptured aneurysms with favorable anatomy. Those aneurysms best suited for unassisted coiling have straightforward microcatheter access, are small or medium sized, and have a narrow neck and a high dome/neck ratio. Aneurysms with wide necks or incorporate bifurcating branches are less favorable due to the possibility of coil prolapse and thromboembolic complication. A wide selection of different microcatheter shapes and coil conformations is available to tailor the treatment to unique aneurysm anatomy. Operators should prepare for the potential need for additional microcatheters by using an appropriately sized guide catheter (usually 6 French), should dual microcatheter technique or balloon or stent assistance be required. Overall, outcomes with unassisted coiling of appropriate aneurysms are excellent, with retreatment rates approximating 15%.
References
Guglielmi G, Vinuela F, Sepetka I, Macellari V. Electrothrombosis of saccular aneurysms via endovascular approach. Part 1: electrochemical basis, technique, and experimental results. J Neurosurg. 1991;75(1):1–7.
Guglielmi G, Vinuela F, Dion J, Duckwiler G. Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: preliminary clinical experience. J Neurosurg. 1991;75(1):8–14.
Gruber A, Killer M, Bavinzski G, Richling B. Clinical and angiographic results of endosaccular coiling treatment of giant and very large intracranial aneurysms: a 7-year, single-center experience. Neurosurgery. 1999;45(4):793–803. discussion 803-794
van Rooij WJ, Sluzewski M. Coiling of very large and giant basilar tip aneurysms: midterm clinical and angiographic results. AJNR Am J Neuroradiol. 2007;28(7):1405–8.
Sluzewski M, Menovsky T, van Rooij WJ, Wijnalda D. Coiling of very large or giant cerebral aneurysms: long-term clinical and serial angiographic results. AJNR Am J Neuroradiol. 2003;24(2):257–62.
Brinjikji W, Piano M, Fang S, et al. Treatment of ruptured complex and large/giant ruptured cerebral aneurysms by acute coiling followed by staged flow diversion. J Neurosurg. 2016;125(1):120–7.
White JB, Ken CG, Cloft HJ, Kallmes DF. Coils in a nutshell: a review of coil physical properties. AJNR Am J Neuroradiol. 2008;29(7):1242–6.
Marks MP, Tsai C, Chee H. In vitro evaluation of coils for endovascular therapy. AJNR Am J Neuroradiol. 1996;17(1):29–34.
Meyers PM, Lavine SD, Fitzsimmons BF, et al. Chemical meningitis after cerebral aneurysm treatment using two second-generation aneurysm coils: report of two cases. Neurosurgery. 2004;55(5):1222.
Eddleman CS, Welch BG, Vance AZ, et al. Endovascular coils: properties, technical complications and salvage techniques. J Neurointerv Surg. 2013;5(2):104–9.
Ishida W, Sato M, Amano T, Matsumaru Y. The significant impact of framing coils on long-term outcomes in endovascular coiling for intracranial aneurysms: how to select an appropriate framing coil. J Neurosurg. 2016;125(3):705–12.
Sluzewski M, van Rooij WJ, Slob MJ, Bescos JO, Slump CH, Wijnalda D. Relation between aneurysm volume, packing, and compaction in 145 cerebral aneurysms treated with coils. Radiology. 2004;231(3):653–8.
Uchiyama N, Kida S, Nomura M, et al. Significance of volume embolization ratio as a predictor of recanalization on endovascular treatment of cerebral aneurysms with guglielmi detachable coils. Interv Neuroradiol. 2000;6(Suppl 1):59–63.
Baxter BW, Rosso D, Lownie SP. Double microcatheter technique for detachable coil treatment of large, wide-necked intracranial aneurysms. AJNR Am J Neuroradiol. 1998;19(6):1176–8.
Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, Sandercock P, International Subarachnoid Aneurysm Trial (ISAT) Collaborative Group. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366(9488):809–17.
Spetzler RF, McDougall CG, Zabramski JM, Albuquerque FC, Hills NK, Russin JJ, Partovi S, Nakaji P, Wallace RC. The barrow ruptured aneurysm trial: 6-year results. J Neurosurg. 2015;123(3):609–17.
McDougall CG, Spetzler RF, Zabramski JM, Partovi S, Hills NK, Nakaji P, Albuquerque FC. The barrow ruptured aneurysm trial. J Neurosurg. 2012;116(1):135–44.
Koivisto T, Vanninen E, Vanninen R, Kuikka J, Hernesniemi J, Vapalahti M. Cerebral perfusion before and after endovascular or surgical treatment of acutely ruptured cerebral aneurysms: a 1-year prospective follow-up study. Neurosurgery. 2002;51:312–25.
Delgado FA, Andersson T, Delgado FA. Clinical outcome after surgical clipping or endovascular coiling for cerebral aneurysms: a pragmatic meta-analysis of randomized and non-randomized trials with short- and long-term follow-up. J Neurointerv Surg. 2016;6
McDougall CG, Johnston SC, Gholkar A, Barnwell SL, Vazquez Suarez JC, Massó Romero J, Chaloupka JC, Bonafe A, Wakhloo AK, Tampieri D, Dowd CF, Fox AJ, Imm SJ, Carroll K, Turk AS, MAPS Investigators. Bioactive versus bare platinum coils in the treatment of intracranial aneurysms: the MAPS (Matrix and Platinum Science) trial. AJNR Am J Neuroradiol. 2014;35(5):935–42.
Koebbe CJ, Veznedaroglu E, Jabbour P, Rosenwasser RH. Endovascular management of intracranial aneurysms: current experience and future advances. Neurosurgery. 2006;59(5 Suppl 3):S93–102.
Murayama Y, Nien YL, Duckwiler G, Gobin YP, Jahan R, Frazee J, Martin N, Vinuela F. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years’ experience. J Neurosurg. 2003;98:959–66.
Takigawa T, Suzuki K, Sugiura Y, Suzuki R, Takano I, Shimizu N, Tanaka Y, Hyodo A. Thromboembolic events associated with single balloon-, double balloon-, and stent-assisted coil embolization of asymptomatic unruptured cerebral aneurysms: evaluation with diffusion-weighted MR imaging. Neuroradiology. 2014;56(12):1079–86.
Raymond J, Roy D. Safety and efficacy of endovascular treatment of acutely ruptured aneurysms. Neurosurgery. 1997;41:1235–46.
Molyneux AJ, Clarke A, Sneade M, Mehta Z, Coley S, Roy D, Kallmes DF, Fox AJ. Cerecyte coil trial: angiographic outcomes of a prospective randomized trial comparing endovascular coiling of cerebral aneurysms with either cerecyte or bare platinum coils. Stroke. 2012;43(10):2544–50.
White PM, Lewis SC, Gholkar A, Sellar RJ, Nahser H, Cognard C, Forrester L, Wardlaw JM, HELPS trial collaborators. Hydrogel-coated coils versus bare platinum coils for the endovascular treatment of intracranial aneurysms (HELPS): a randomised controlled trial. Lancet. 2011;377(9778):1655–62.
Raymond J, Guilbert F, Weill A, Georganos SA, Juravsky L, Lambert A, Lamoureux J, Chagnon M, Roy D. Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke. 2003;34:1398–403.
Johnston SC, Dowd CF, Higashida RT, Lawton MT, Duckwiler GR, Gress DR, CARAT Investigators. Predictors of rehemorrhage after treatment of ruptured intracranial aneurysms: the cerebral aneurysm Rerupture after treatment (CARAT) study. Stroke. 2008;39(1):120–5.
Mascitelli JR, Moyle H, Oermann EK, Polykarpou MF, Patel AA, Doshi AH, Gologorsky Y, Bederson JB, Patel AB. An update to the Raymond-Roy Occlusion Classification of intracranial aneurysms treated with coil embolization. J Neurointerv Surg. 2015;7(7):496–502.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Fargen, K.M., Singh, J., Wilson, J.A., Wolfe, S.Q. (2019). Unassisted Aneurysm Coil Embolization. In: Spiotta, A., Turner, R., Chaudry, M., Turk, A. (eds) Management of Cerebrovascular Disorders. Springer, Cham. https://doi.org/10.1007/978-3-319-99016-3_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-99016-3_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-99015-6
Online ISBN: 978-3-319-99016-3
eBook Packages: MedicineMedicine (R0)