Abstract
Introduction: The principles of PEH repair involve primary closure of the hiatus around the esophagus after complete reduction of the hernia sac. However, this repair is associated with a high failure rate, leading surgeons to consider prosthetic materials to reinforce the hiatal closure. In this chapter, we review the literature comparing outcomes of hiatal mesh reinforcement to simple closure during laparoscopic PEH repair.
Synthetic (Nonabsorbable) Mesh: Synthetic mesh reinforcement seems to reduce at least short-term recurrences of PEH compared to primary closure alone. Multiple RCTs comparing synthetic mesh vs primary closure alone showed no long-term benefit of mesh. A report found use of PTFE for hiatal reinforcement increased case costs by $960+/−70 USD. In addition, the risk of bleeding, stricture, and erosion of mesh into the stomach or esophagus is increased with the use of synthetic mesh during PEH repair.
Absorbable Mesh: Multiple RCTs have compared absorbable synthetic or biologic mesh to simple closure of the hiatus. Most notably, a multicenter RCT by Oelschlager et al. in 2006 compared Surgisis® to simple closure of the diaphragmatic pillars and concluded that hiatal reinforcement with Surgisis® resulted in fewer early recurrences at 6 months. However, on long-term re-evaluation, there was no difference in recurrence rates at 5 years. An important consideration is that biologic meshes have been reported to cost up to $1200 USD per case. Absorbable mesh-related complications are far less common compared to those associated with synthetic nonabsorbable materials. Fibrosis and dysphagia are the most reported sequelae of absorbable mesh.
Summary and Conclusion: Based on published RCTs and meta-analyses, there is insufficient evidence to support routine mesh reinforcement of hiatal closure. There is no evidence that they reduce recurrence long-term recurrence of PEH, and they are associated with increased complications and costs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Laparoscopic paraesophageal hernia (PEH) repair has posed a challenge to surgeons ever since Cuschieri reported the first case in 1992 [1]. To this day, it remains a technically demanding procedure that requires advanced training and expertise [2].
The principles of PEH repair, whether laparoscopic or open, involve primary closure of the hiatus around the esophagus after complete reduction of the hernia sac. However, this repair is associated with a high failure rate, which has led surgeons to use prosthetic graft materials to reinforce the hiatal closure. This approach was extrapolated from success with tension-free mesh repairs of other types of hernias, such as abdominal wall defects. Multiple variations to the traditional PEH repair have been tried, with a view to refine the technique and reduce the risk of recurrence.
Attempts at crural reinforcement date back almost 100 years. Hedblom et al. first used autologous fascia lata in 1925 to buttress the crural closure [3, 4]. Later, prosthetic materials such as tantalum [5], polyvinyl formaldehyde sponge [6], and polytetrafluoroethylene (PTFE) [7] were introduced as reinforcement materials for use at the hiatus. Currently, several different types of prosthetics, in a wide range of materials and sizes, are available for this purpose. Regardless of approach, however, the recurrence rate remains between 20–59% at 5 years [8,9,10,11,12]. For the purpose of this report, we will use the term “mesh” to describe these materials used to support the hiatal closure, although some of these products are solid sheets of material with various surfaces designed to promote or discourage ingrowth, while others are truly mesh with various weights and pore sizes.
Despite the high recurrence rate, most recurrences are asymptomatic and infrequently require a repeat operation [13,14,15]. Moreover, reported sequelae of the use of synthetic materials near the esophagus are not inconsequential and include erosion, perforation, obstruction, and increased risk of major complications at revisional surgery. Bioabsorbable and bioprosthetic meshes seem to be safer than synthetic meshes at the hiatus, but are considerably more costly and may be associated with a higher risk for delayed recurrences.
In this chapter, we will review the literature comparing outcomes of hiatal mesh reinforcement to simple closure during laparoscopic paraesophageal hernia repair.
Synthetic (Nonabsorbable) Mesh
Types
Polypropylene, polytetrafluoroethylene (PTFE), and polypropylene with covalently bonded titanized surface (Timesh ®) are types of synthetic mesh that are commonly used for this purpose.
Impact on Recurrence
Synthetic mesh reinforcement seems to reduce at least short-term recurrences of PEH compared to primary closure alone.
During the 1990s, multiple small series were published regarding the use of synthetic mesh reinforcement during paraesophageal hernia repair [16,17,18,19]. These reports were quite heterogeneous, with each group reporting a different technique for reinforcing the hiatus with mesh and each using different materials. These were small case series (n = 1–5), and follow-up was limited to 3–6 months. There were no mesh-related complications reported, possibly due to the small number of patients and short follow-up.
Carlson MA et al. [20] reported the very first randomized controlled trial (RCT) of laparoscopic paraesophageal hernia repair with prosthetic reinforcement [20]. These authors randomized 31 patients to posterior cruroplasty vs cruroplasty with mesh reinforcement using polytetrafluoroethylene (PTFE). The mesh was used as onlay reinforcement in a keyhole fashion to accommodate the esophagus. All patients underwent an esophagogastroduodenoscopy (EGD) and esophagogram at 3 months after surgery and every 6 months thereafter, with a median follow-up ranging between 12 and 36 months. No recurrences were reported in the mesh group; three recurrences (18.8%) were reported in the cruroplasty-alone group. Of these, two underwent repeat operative repair for symptoms. Unfortunately, perioperative symptoms and quality of life were not reported in either group, and the definition of “recurrence” was not described.
Since this study, there have been multiple RCTs comparing laparoscopic hiatal hernia repair with mesh to simple closure of the hiatus (Table 24.1). Many of these reported reduced recurrence rates with synthetic mesh and an increased need for reoperation for symptomatic recurrence in patients repaired without mesh [18, 21]. The follow-up intervals in these studies ranges from 6 to 36 months.
Cost
While very few trials report cost of repair with synthetic mesh versus primary closure, use of mesh is logically more costly than primary closure alone. The mesh itself has an inherent cost, and the additional operating room time needed to place the mesh after primary crural closure must be factored in as well. In one study, an additional cost of $1050 USD was estimated with the use of PTFE when compared to primary closure [20]. Another report found use of PTFE for hiatal reinforcement increased case costs by $960+/−70 USD [22]. The additional cost for the mesh techniques needs to be balanced against the substantial cost of reoperation for a symptomatic recurrence. These data are not available.
Synthetic Nonabsorbable Mesh-Related Complications
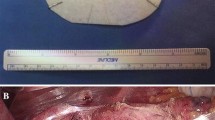
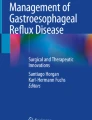
Several types of complications have been described following crural reinforcement with synthetic mesh during paraesophageal hernia repair. Bleeding, stricture, and erosion of mesh into the stomach or esophagus (Figs. 24.1 and 24.2) are the most commonly reported [21, 23, 24].
Esophageal stenosis causing dysphagia is an oft-described sequela of using synthetic nonabsorbable mesh at the hiatus. These cases frequently require either operative or endoscopic intervention to treat the dysphagia. If the mesh can be removed endoscopically, the resulting stricture may be dilated, potentially avoiding operative intervention. If reoperation is necessary, however, the risk of partial esophagectomy or gastrectomy is high [16, 25,26,27,28,29,30,31]. One publication reported 20 cases of mesh-related complications after laparoscopic paraesophageal hernia repair, 8 involving polypropylene and 12 involving PTFE. The complications included mesh erosion in 12 patients and dense fibrosis around the esophagus in the remaining 8, all causing significant dysphagia. Only two of these patients were managed non-operatively [32]. The remaining patients required operations ranging from laparoscopic retrieval of mesh to esophagectomy.
All available RCTs comparing permanent synthetic hiatal mesh to absorbable mesh or no mesh have had short follow-up durations (12–36 months), which may explain the low rate of reported mesh-related complications in these trials. In a recent survey of European surgeons using synthetic mesh for hiatal reinforcement, 523 respondents reported encountering mesh complications at least once in their careers. These complications included mesh erosion (21%), esophageal stenosis (25%), mesh infection (7%), and cardiac tamponade (7%) [33]. The respondents to this survey highlight the very real, and often delayed, risk of serious complications of synthetic mesh for paraesophageal hernia repair.
The use of Teflon pledgets has also been associated with complications. In one retrospective review of 1175 cases of laparoscopic paraesophageal hernia repair, 11 patients developed symptoms from Teflon pledgets erosion that occurred more than 2 months after surgery [34]. These patients presented with dysphagia, recurrent symptoms of reflux, and melena.
Absorbable Mesh
Types
Surgisis®, Strattice ™, Alloderm®, and Gore’s BioA® are the more commonly reported absorbable products used for hiatal hernia repair.
Impact on Recurrence
Similarly to synthetic nonabsorbable mesh, multiple RCTs and systematic reviews have been conducted comparing absorbable or biologic mesh to simple closure of the hiatus. The well-known RCT by Oelschlager et al., in 2006 [35], compared Surgisis® to simple closure of the diaphragmatic pillars. In the Surgisis® group, a piece of Surgisis® was prepared and cut in a U configuration. The mesh was then placed with the base of the U overlying the posterior hiatal closure and sutured in place with interrupted sutures. A total of 108 patients were randomized and followed for 6 months. Recurrence was defined as a hiatal hernia >2 cm diagnosed on upper gastrointestinal imaging or the need for reoperation secondary due to wrap disruption, migration, or herniation at any time during the study period. Initial results showed a significantly lower recurrence rate in the mesh group versus the simple closure group (9 vs 24%, p = 0.04). Based on these early results, the authors concluded that hiatal reinforcement with Surgisis® resulted in fewer recurrences when compared to simple closure of the hiatus [35]. This trial stimulated enthusiasm for the use of biologic material to supplement crural closure. However, a follow-up study of these same patients examining recurrence rates at 5 years showed no difference between groups [10].
Two RCTs compared synthetic mesh, biologic mesh, and simple closure after PEH repair. These studies found no difference in recurrence rates among all three groups at 12 months [36] and 24 months [11], with recurrence rates ranging from 12% to 30%.
No reports could be found specifically examining the efficacy of bioprosthetic absorbable mesh for crural reinforcement. A retrospective review of a single institution database found no significant difference in hernia recurrence rates or complications with BioA® and biologic meshes [37]. Another retrospective series of 114 patients undergoing both sliding and PEH repair with BioA® mesh reported a recurrence rate of 0.9% with a median follow-up of 1 year. While this low recurrence rate is highly encouraging, this study has several significant limitations, including its retrospective nature, lack of long-term follow-up, and inclusion of small (sliding) hiatal hernias [38]. No mesh-related complications were reported in either series. As prospective data are lacking, no meaningful conclusions can be drawn regarding the efficacy of bioprosthetic mesh for prevention of hiatal hernia recurrence.
Cost
No trials have directly compared cost differences between various mesh repairs versus primary closure alone. However, use of these meshes is clearly more costly than simple primary closure. While costs of materials vary somewhat by region, biologic meshes have been reported to cost up to $1202 USD per case and other materials up to $483 USD [39].
Absorbable Mesh-Related Complications
Mesh-related complications are in general far less common or devastating for absorbable meshes compared to permanent synthetic crural reinforcements. Fibrosis and dysphagia seem to be the most common sequelae of absorbable mesh placed next to the esophagus. One series described four patients who developed dysphagia and pain after paraesophageal hernia repair with absorbable mesh reinforcement. Of these, one required reoperation to remove the mesh as it was determined to be the cause of his dysphagia, and another required multiple endoscopic dilatations [34]. Another series described 6 patients who developed dysphagia due to extensive fibrosis around the gastroesophageal junction after absorbable mesh use [32].
As with randomized controlled trials of permanent mesh for hiatal reinforcement, most RCTs examining outcomes with absorbable mesh report only short-term outcomes. In the Oelschlager 5-year follow-up study of 108 patients randomized to no mesh versus Surgisis reinforcement, no significant mesh-related complications were reported [10]. In general, it seems complications of absorbable mesh occur less frequently, and are less devastating, than those encountered when permanent mesh is used at the hiatus.
Meta-analyses of Randomized Controlled Trials
Since the results of individual RCTs regarding the value of mesh reinforcement at the hiatus have been conflicting, numerous systematic reviews and meta-analyses (SR&MAs) have been conducted [2, 9, 40,41,42,43]. Most of these grouped synthetic and biologic meshes together in their analysis of outcomes, and the majority have concluded there is insufficient evidence to support routine mesh reinforcement of any type at the hiatus.
In 2016 alone, there were two such systematic reviews and meta-analyses published [2, 9]. Memon et al. reviewed four randomized controlled trials (406 patients) comparing mesh repair to simple closure during laparoscopic hernia repair [9]. The median follow-up was 6 months. They concluded that all included RCTs suffered from poor methodological quality and that there is presently no evidence to support the routine use of mesh. The report by Tam et al. (2016) analyzed 26 studies comparing mesh repair to simple closure in laparoscopic paraesophageal hernia repair with recurrence as the primary outcome [2]. They found the odds of hernia recurrence in the mesh repair group were 49% less (OR 0.51, 95% CI 0.30 to 0.87; p = 0.014) relative to the baseline group of simple repair. However, there was no significant difference in the need for reoperation between mesh and non-mesh groups (odds ratio 0.42, 95% CI 0.13 to 1.37; p = 0.149). Furthermore, the included studies were highly variable with respect to type of mesh used, definition of recurrence, and time to objective follow-up, which ranged between 6 and 117 months, such that a favorable conclusion toward mesh repair could not be made. Of the studies included in the same meta-analysis, three studies reported six mesh-related complications including five mesh erosion into the esophagus and one unspecified complication requiring mesh removal [2].
Significance of Hiatal Hernia Recurrence After Paraesophageal Hernia Repair
Recurrence has classically been used as a metric of quality after paraesophageal hernia repair. As such, the goal of paraesophageal hernia repair historically has been to avoid recurrences of any size, even small type I hernias. As described above, the majority of RCTs and other studies examining mesh reinforcement after hiatal closure report follow-up of only ~6–24 months; few of these report on pre- vs postoperative quality of life or symptoms (Table 24.1). The one trial which did report on these outcomes at 5 years in patients receiving biologic vs no mesh found no differences in symptoms, quality of life, or need for reoperation between groups, regardless of hernia recurrence [10].
In the absence of direct data, need for reoperation may be used as a surrogate for poor quality of life or intolerable symptoms. In large series reporting on 5–10 years of follow-up, the rate of reoperation appears to be quite low (0–4.8%) [8, 10]. Furthermore, in studies that have reported long-term quality of life and symptoms scores, these appear to improve and remain stable over time irrespective of hernia recurrence [8, 44,45,46]. In light of these results, it seems that anatomical recurrence alone is not a sufficient indicator of operative “failure” after PEH repair.
Summary
Despite numerous RCTs and other clinical reports, the available data do not presently support the routine use of mesh for crural reinforcement over primary cruroplasty alone. While synthetic nonabsorbable mesh use has been shown to result in lower anatomic recurrence rates, most recurrences are of little clinical significance and do not warrant the risk of catastrophic complications from permanent mesh placed at the hiatus. Absorbable materials might lessen the risk of serious complications but result in similar long-term recurrence rates to primary closure with considerable additional cost.
As such, it is our opinion, based on the available evidence at this time, that routine mesh reinforcement after primary hiatal hernia repair is of little clinical value and associated with elevated risk of complications and cost. We recommend against the use of permanent mesh entirely and suggest that bioabsorbable meshes be used only selectively.
References
Cuschieri A, Shimi S, Nathanson LK. Laparoscopic reduction, crural repair, and fundoplication of large hiatal hernia. Am J Surg. 1992;163(4):425–30.
Tam V, Winger DG, Nason KS. A systematic review and meta-analysis of mesh vs suture cruroplasty in laparoscopic large hiatal hernia repair. Am J Surg. 2016;211(1):226–38.
Hedblom CA. The selective surgical treatment of diaphragmatic hernia. Ann Surg. 1931;94(4):776–85.
Hedblom CA. Diaphragmatic hernia: a study of three hundred and seventy eight cases in which operation was performed. JAMA. 1925;85:947.
Fusco EM. The repair of hiatus hernia with tantalum mesh. Mil Med. 1960;125:189–90.
Friedman MH, Mackenzie WC. The clinical use of polyvinyl sponge (ivalon) in the repair of oesophageal hiatus hernia. Can J Surg. 1961;4:176–82.
Merendino KA, Dillard DH. Permanent fixation by teflon mesh of the size of the esophageal diaphragmatic aperture in hiatus herniplasty; a concept in repair. Am J Surg. 1965;110:416–20.
Le Page PA, et al. Durability of giant hiatus hernia repair in 455 patients over 20 years. Ann R Coll Surg Engl. 2015;97(3):188–93.
Memon MA, et al. Suture cruroplasty versus prosthetic hiatal herniorrhaphy for large hiatal hernia: a meta-analysis and systematic review of randomized controlled trials. Ann Surg. 2016;263(2):258–66.
Oelschlager BK, et al. Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg. 2011;213(4):461–8.
Koetje JH, et al. Quality of life following repair of large hiatal hernia is improved but not influenced by use of mesh: results from a randomized controlled trial. World J Surg. 2015;39(6):1465–73.
Mattar SG, et al. Long-term outcome of laparoscopic repair of paraesophageal hernia. Surg Endosc. 2002;16(5):745–9.
Allison PR. Hiatus hernia: (a 20-year retrospective survey). Ann Surg. 1973;178(3):273–6.
Lebenthal A, Waterford SD, Fisichella PM. Treatment and controversies in paraesophageal hernia repair. Front Surg. 2015;2:13.
Smith GS, et al. Symptomatic and radiological follow-up after para-esophageal hernia repair. Dis Esophagus. 2004;17(4):279–84.
Edelman DS. Laparoscopic paraesophageal hernia repair with mesh. Surg Laparosc Endosc. 1995;5(1):32–7.
Paul MG, et al. Laparoscopic tension-free repair of large paraesophageal hernias. Surg Endosc. 1997;11(3):303–7.
Frantzides CT, Carlson MA. Prosthetic reinforcement of posterior cruroplasty during laparoscopic hiatal herniorrhaphy. Surg Endosc. 1997;11(7):769–71.
Watanabe G, et al. Laparoscopic repair of a paraesophageal hiatus hernia without fundoplication. Surg Today. 1997;27(11):1093–6.
Carlson MA, Richards CG, Frantzides CT. Laparoscopic prosthetic reinforcement of hiatal herniorrhaphy. Dig Surg. 1999;16(5):407–10.
Granderath FA, et al. Impact of laparoscopic nissen fundoplication with prosthetic hiatal closure on esophageal body motility: results of a prospective randomized trial. Arch Surg. 2006;141(7):625–32.
Frantzides CT, et al. A prospective, randomized trial of laparoscopic polytetrafluoroethylene (PTFE) patch repair vs simple cruroplasty for large hiatal hernia. Arch Surg. 2002;137(6):649–52.
Arendt T, et al. Dysphagia due to transmural migration of surgical material into the esophagus nine years after Nissen fundoplication. Gastrointest Endosc. 2000;51(5):607–10.
Trus TL, et al. Complications of laparoscopic paraesophageal hernia repair. J Gastrointest Surg. 1997;1(3):221–7. discussion 228
Carlson MA, et al. Management of intrathoracic stomach with polypropylene mesh prosthesis reinforced transabdominal hiatus hernia repair. J Am Coll Surg. 1998;187(3):227–30.
Schauer PR, et al. Comparison of laparoscopic versus open repair of paraesophageal hernia. Am J Surg. 1998;176(6):659–65.
Coluccio G, et al. Dislocation into the cardial lumen of a PTFE prosthesis used in the treatment of voluminous hiatal sliding hernia, a case report. Minerva Chir. 2000;55(5):341–5.
van der Peet DL, et al. Laparoscopic treatment of large paraesophageal hernias: both excision of the sac and gastropexy are imperative for adequate surgical treatment. Surg Endosc. 2000;14(11):1015–8.
Rumstadt B, et al. Gastric mesh erosion after hiatoplasty for recurrent paraesophageal hernia. Endoscopy. 2008;40(Suppl 2):E70.
Griffith PS, et al. Rejection of goretex mesh used in prosthetic cruroplasty: a case series. Int J Surg. 2008;6(2):106–9.
Tatum RP, et al. Complications of PTFE mesh at the diaphragmatic hiatus. J Gastrointest Surg. 2008;12(5):953–7.
Stadlhuber RJ, et al. Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc. 2009;23(6):1219–26.
Huddy JR, et al. Laparoscopic repair of hiatus hernia: does mesh type influence outcome? A meta-analysis and European survey study. Surg Endosc. 2016;30(12):5209–21.
Antonakis F, Kockerling F, Kallinowski F. Functional results after repair of large hiatal hernia by use of a biologic mesh. Front Surg. 2016;3:16.
Oelschlager BK, et al. Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg. 2006;244(4):481–90.
Watson DI, et al. Laparoscopic repair of very large hiatus hernia with sutures versus absorbable mesh versus nonabsorbable mesh: a randomized controlled trial. Ann Surg. 2015;261(2):282–9.
Jones R, et al. Long-term outcomes of radiologic recurrence after paraesophageal hernia repair with mesh. Surg Endosc. 2015;29(2):425–30.
Alicuben ET, Worrell SG, DeMeester SR. Resorbable biosynthetic mesh for crural reinforcement during hiatal hernia repair. Am Surg. 2014;80(10):1030–3.
Chiruvella A, Lomelin D, Oleynikov D. A cost-comparison of mesh usage in laparoscopic paraesophageal hernia repair. In: Sages. Boston: Sages Archives; 2016.
Antoniou SA, et al. Lower recurrence rates after mesh-reinforced versus simple hiatal hernia repair: a meta-analysis of randomized trials. Surg Laparosc Endosc Percutan Tech. 2012;22(6):498–502.
Antoniou SA, et al. Laparoscopic augmentation of the diaphragmatic hiatus with biologic mesh versus suture repair: a systematic review and meta-analysis. Langenbeck's Arch Surg. 2015;400(5):577–83.
Rathore MA, et al. Metaanalysis of recurrence after laparoscopic repair of paraesophageal hernia. JSLS. 2007;11(4):456–60.
Furnee E, Hazebroek E. Mesh in laparoscopic large hiatal hernia repair: a systematic review of the literature. Surg Endosc. 2013;27(11):3998–4008.
Lidor AO, et al. Long-term quality of life and risk factors for recurrence after laparoscopic repair of paraesophageal hernia. JAMA Surg. 2015;150(5):424–31.
Targarona EM, et al. Long-term outcome and quality of life after laparoscopic treatment of large paraesophageal hernia. World J Surg. 2013;37(8):1878–82.
Mittal SK, et al. Outcomes after repair of the intrathoracic stomach: objective follow-up of up to 5 years. Surg Endosc. 2011;25(2):556–66.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 SAGES
About this chapter
Cite this chapter
Al Mahroos, M., Mueller, C.L., Fried, G.M. (2019). Expert Commentary: Mesh Reinforcement of Hiatal Closure. In: Grams, J., Perry, K., Tavakkoli, A. (eds) The SAGES Manual of Foregut Surgery . Springer, Cham. https://doi.org/10.1007/978-3-319-96122-4_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-96122-4_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-96121-7
Online ISBN: 978-3-319-96122-4
eBook Packages: MedicineMedicine (R0)