Abstract
Epilepsy is one of the most common complex neurological diseases. It is frequently associated with intellectual and developmental disabilities (ID/DD). In recent years, copy number variation (CNV), especially microdeletion, was proven to be a potential key factor of genetic epilepsy. In this paper, the authors tested the hypothesis that the large de novo rare CNV is an important cause of epilepsy with ID/DD. We performed a custom array comparative genomic hybridization (aCGH) to detect the CNVs of 96 Chinese epileptic patients with ID/DD. The aCGH was designed with a higher density probe coverage of 320 genes known to be involved in epilepsy and ID/DD with lower density whole-genome backbone coverage. We detected 9 large de novo rare microdeletions from 8 patients. These CNVs are located on 2q24.1, 2q33.1-q34, 5q13.2 (2 similar CNVs), 5q33.1-q34, 17p13.2, 22q11.21-q11.22 (2 identical CNVs) and Xp22.31. We also found that only a few genes in the CNVs are known epilepsy related genes. By analysis with systems biology, we found most of the genes are interacting genes known to be epilepsy related genes. We also found a gene motif “BGNADP”, constructed by BTD, GALNT10, NMUR2, AUTS2, DLG2 and PTPRD, would be a key motif in epilepsy and ID/DD. These findings strongly indicate that some large de novo rare microdeletion is an important pathological cause of epilepsy with ID/DD. Our study also found a gene motif “BGNADP” should be a key small network in epilepsy with ID/DD.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
9.1 Introduction
Epilepsy is a disease which arises from largely unknown cellular and genetic mechanisms. It is a common neurological disease that reflects neuronal hyperexcitability induced by many different factors such as trauma, neurotoxicity and genetic variation (Lee and Heo 2014). ID/DD is one of the most common pediatric neurological diseases and is also one of the most important unsolved problems in health care. Studies have shown that the prevalence rate of ID/DD is 1–3% (Chelly et al. 2006). It is estimated that approximately 30% of patients with ID/DD have seizures (Tuchman et al. 2009). These associations indicate that epilepsy shares a similar pathogenic mechanism with those diseases in some situations (Williams et al. 2009; Cooper et al. 2011; Grayton et al. 2012).
Copy number variation (CNV) has been reported to be associated with a group of neuropsychiatric disorders, including epilepsy and ID/DD. Recent studies of CNV in patients with epilepsy have revealed a series of CNV hotspots, such as 1q21.1 (de Kovel et al. 2010; Mefford et al. 2010), 15q11.2 (Zhang et al. 2009; de Kovel et al. 2010; Mefford et al. 2010; Vanlerberghe et al. 2015), 15q13.3 (Mulley et al. 2011; Sisodiya and Mefford 2011; Kogan et al. 2015), 16p11.2 (Mefford et al. 2011; Bassuk et al. 2013; Tiwari et al. 2013), 16p13.11 (Sisodiya and Mefford 2011) and 22q11.2 (Helbig et al. 2013; Kim et al. 2016). At the same time, a group of ID/DD-related CNV hotspots was been found, as 1q21.1 (Harvard et al. 2011), 2q13 (Yu et al. 2012; Riley et al. 2015), 15q11.2 (Derks et al. 2013; Caciotti et al. 2015), 16p11.2 (Bassuk et al. 2013; Derks et al. 2013), 22q11.2 (Mertz et al. 2013; Olszewski et al. 2014). The overlap of those CNV hotpots between epilepsy and ID/DD, indicate these two disease share a similar pathogenic genetic mechanism.
To elucidate whether CNV is a causal factor in epilepsy with ID/DD in Chinese children, we utilized a custom high-density oligonucleotide-based comparative genomic hybridization (CGH) microarrays to detect the CNVs in 96 epilepsy patients with ID/DD.
9.2 Large De Novo Rare Microdeletion Is an Important Pathological Cause of Epilepsy with ID/DD
9.2.1 Ethics and Patients
The study protocol was approved by Medical Ethics Committee of Peking University First Hospital. Informed consent was obtained from the parents. All data of this study were analyzed anonymously. DNA samples were collected from 96 epileptic patients with ID/DD and from their parents. All of the patients were recruited from the Department of Pediatrics, Peking University First Hospital from 2006 to 2014. These samples were prepared from a collection of whole blood samples by DNeasy Blood & Tissue Kit (QIAGEN).
Patient with both epilepsy and ID/DD who fulfilled the following inclusion criteria were assumed to be cryptogenic: (1). no perinatal brain injury (2). no hypoxia, ischemia, trauma or infection of the central nervous system (CNS); (3). no evidence of typical inherited metabolic disorder or specific neurodegenerative disorders, as found by physical examination, cranial neuroimaging and blood/urinary metabolic diseases screening; (4). negative from a gene screen by 300 epilepsy gene panel (Zhang et al. 2015). Finally, according to the inclusion criteria, 96 participating Han ethnicity patients were recruited from Peking University First Hospital.
9.2.2 CNV Detection by Array CGH
To detect the changes of CNVs in the genomic DNA, we applied high-density oligonucleotide-based CGH microarrays, a custom-designed Agilent SurePrint G3 Microarray (4 × 180K) was used to verify CNVs. The high-density areas covered the known epilepsy associated genes or related chromosome loci (including genes and CNVs in epilepsy including early infantile epileptic encephalopathy and idiopathic generalized epilepsy, listed in Supplementary Table 9.1). DNA digestion, Cy5-dUTP or Cy3-dUTP labeling, purification, array hybridization, washing, scanning, and data analysis were conducted by following the Agilent oligonucleotide aCGH protocol (version 6.3).
We performed whole-genome array CGH in a series of 96 patients. All of them had a presenting diagnosis of epilepsy with ID/DD. Our goal was to discover novel CNVs associated with epilepsy and ID/DD. In this study, we gathered data from whole-genome analysis and extended our analysis to other idiopathic epilepsy syndromes, such as infantile spasms and early onset epileptic encephalopathy (EOEE). In total 96 patients, we identified 8 individuals (8.3%) with 9 long rare microdeletions. If the CNV is larger than 500 kb, it will be identified as a long/large one.
9.2.3 The Loci of Microdeletions
In this study, we identified 8 of 96 (8.3%) patients with 1 or 2 large microdeletions (more than 500 kb). The biggest deletion was about 11 Mb, and the smallest was 893 kb. The mean CNV size was 3.5 Mb and the median size was 2.9 Mb. The number of deleted genes in each patient was from 12 to 79 (Table 9.1). Figure 9.1 shows the loci of the CNVs in the genome. There were two identical microdeletions at 22q11.21-q11.22 (Fig. 9.2) and two similar microdeletions at 5q13.2 (Fig. 9.3). The other CNVs were located on 2q33.1-q34, 2q24.1, 5q33.1-q34, 17p13.2, and Xp22.31 (Fig. 9.4). All the CNVs were de novo and heterozygous. Microdeletion of 5q13.2 and 17p13.2 was not found in patients of epilepsy with ID/DD before. The clinical features of the patients with large microdeletion were summarized in Table 9.2. Of the 8 patients with large microdeletions, 5 were male and 3 were female. Besides epilepsy and ID/DD, the phenotypes of the patients were diverse. Six out of 7 patients who had a MRI scan had encephalodysplasia. Of 5 patients who had a psychiatric test, 2 patients suffered from autism. For craniofacial characteristics, 3 patients had facial dysmorphism, 1 patient had cleft lip/palate, and 2 patients had strabismus (Tables 9.2 and 9.3).
The loci of the 9 CNVs of our cohort in the genome. 2 CNVs (2q24.1 of patient 3940 and 2q33.1-q34 of patient 2332) in chromosome 2, 3 CNVs (5q13.2 of patient 1549 and 5332, 5q33.1-q34 of patient 5319), 1 CNV (17p13.3 of 1277) in chromosome 17, 2 CNVs (22q11.21-q11.22 of patient 1583 and 3568) in chromosome 22, 1 CNV (Xp22.31 of patient 1539)
The 2 same CNV in 22q11.21-q11.22. (a) The microdeletion in 22q11.21-q11.22 of patient 3568. Compared with the genome DNA of his father and mother, the CNVs is de novo. From the data of SV database in this area, the CNV is rare. (b) The microdeletion in 22q11.21-q11.22 of patient 1583. Compared with the genome DNA of his father and mother, the CNVs is de novo. From the data of SV database in this area, the CNV is rare
The 2 similar CNV in 5q13.2. (a) The microdeletion in 5q13.2 of patient 5332. Compared with the genome DNA of his father and mother, the CNVs is de novo. From the data of SV database in this area, the CNV is not rare. (b) The microdeletion in 5q13.2 of patient 1549. Compared with the genome DNA of his father and mother, the CNVs is de novo. From the data of SV database in this area, the CNV is not rare
The other CNVs in our cohort. (a) The microdeletion in 2q24.1 of patient 3940. Compared with the genome DNA of his father and mother, the CNVs is de novo. From the data of SV database in this area, the CNV is rare. (b) The microdeletion in 2q33.1-q34 of patient 2332. Compared with the genome DNA of his father and mother, the CNVs is de novo. From the data of SV database in this area, the CNV is rare. (c) The microdeletion in 5q33.1-q34 of patient 5319. Compared with the genome DNA of his father and mother, the CNVs is de novo. From the data of SV database in this area, the CNV is rare. (d) The microdeletion in 17p13.2 of patient 1277. Compared with the genome DNA of his father and mother, the CNVs is de novo. From the data of SV database in this area, the CNV is rare. (e) The microdeletion in Xp22.31 of patient 1549. Compared with the genome DNA of his father and mother, the CNVs is de novo. From the data of SV database in this area, the CNV is rare
From these results, most of patients have only one large microdeletions. Those CNVs should course epilepsy and ID/DD by two different situations, one is the CNVs have both epilepsy-related genes and ID/DD related genes, the other is the CNVs have one or more genes associating both epilepsy and ID/DD. We also found that most of the long rare CNVs in this study were not in the most well-known idiopathic epilepsy CNV hotspots, such as 1q21.1, 15q11.2, 15q13.3, 16p11.2, 16p13.11, 22q11.2 (Table 9.4). The reason for this difference might be that the known CNV hotpots come from studies of idiopathic epilepsy, while our patients suffered from both epilepsy and ID/DD. Most of them are epileptic encephalopathy. The reported CNV regions of epileptic encephalopathy, such as 1q36, 2q32.3, 2q24.3, 3q11, 4q3.1-q3.2, 7q11.23, 14q12, 15q11-13, 16p11.2, Xp22 (Table 9.5) are not in accordance with idiopathic epilepsy.
9.3 Pathogenic Mechanism Analysis
We analyzed the genes in the CNVs and discovered some genes which were candidate pathogenic genes. We screened for candidates by determining whether genes were epilepsy/seizure related, ID/DD related, synapse related, ion channel/receptor related, transmitter related, and neurodevelopment related, or having high expression in the CNS (Table 9.3). We found that 4 out of the 9 CNVs included epilepsy related genes, while 6 out of the 9 CNVs included reported ID/DD related genes. Besides the known epilepsy- or ID/DD-related genes, some novel candidate genes might be involved in epilepsy with ID/DD: NR4A, KCTD18, TRAK2, UNC80, CASP8, NRP2, KLF7, OCLN, SMN1, SMN2, NAIP, ADRA1B, HAND1, SRR, PAFAH1B1, SEPT5, RTN4R, TBX1, ARVCF, RTN4R and CRKL (Table 9.6).
Patient 3940 with a 2q24.1 deletion was suffering from autism with epilepsy and ID/DD. 2q24.1 was reported to be involved in juvenile myoclonic epilepsy (Layouni et al. 2010), ID/DD (Daoud et al. 2009) and schizophrenia (Yamada et al. 2012). Therefore, 2q24.1 should be a potential CNV locus for neuropsychiatric disorders. The pathogenic genes in this patient could be GPD2 and NR4A2. GPD2, which is highly expressed in brain, was reported to be a candidate gene for ID/DD in a female with nonsyndromic ID/DD (Daoud et al. 2009; Barge-Schaapveld et al. 2013). NR4A2 is the gene for Nuclear Receptor Subfamily 4, Group A, Member 2, which is crucial for expression of a set of genes such as SLC6A3, SLC18A2, TH and DRD2 for the development of neurons (Messmer et al. 2007).
The clinical features of patient 2332 with a 2q33.1-q34 deletion were similar to 2q32-q33 deletion syndrome. 2q32-q33 deletion syndrome (OMIM # 612313), first reported at 1989, (Glass et al. 1989) is characterized by severe ID/DD, microcephaly and craniofacial dysmorphism. A STAB2 gene deletion might be the most likely pathogenic gene in the 2q33.1-q34 region. The SATB2 is a candidate brain developmental gene which should be responsible for the 2q32-q33 deletion syndrome (Van Buggenhout et al. 2005; Rosenfeld et al. 2009; Usui et al. 2013). The STAB2 gene encodes a transmembrane receptor which has always been a marker of the upper layer of the normal fetal neocortex (Arai et al. 2012). In the 2q33.1-q34 CNV of our patient, there are both epilepsy-related genes and ID/DD related genes. The reported epilepsy-related genes are ADAM23 (Owuor et al. 2009; Fukata et al. 2010), MAP2 (Chulanova et al. 2001; Jalava et al. 2007). SATB2 (Leoyklang et al. 2007) and CREB1 (Barco et al. 2003) were reported to be ID/DD related gene. Besides those genes, KCTD18 (Pichler et al. 2013), TRAK2 (Grishin et al. 2006), and UNC80 (Gogliotti et al. 2011) are related to ion channels or receptors, and CASP8 (Ma et al. 2007), NRP2 (Maden et al. 2012) and KLF7 (Caiazzo et al. 2011) takes part in neurodevelopment.
There were two patients (1583 and 3568) sharing the identical 48 gene-deleted CNV in 22q11.21-q11.22. Besides epilepsy and ID/DD, they also suffered from encephalodysplasia. Patient 1583 also had an anomalous face. Patient 1583 was a boy born after uneventful term delivery. He was the product of healthy parents without family history of epilepsy and ID/DD. However, this boy had tonic seizures since 5 months. The seizures are intermittent with a frequency of 1.5 times per month. His intellectual and motive developments were delayed. The patient also had an anomalous face with short philtrum, small auricle, high palatal arch, and up-warped upper lip. A brain MRI showed cerebral dysplasia, increased lateral ventricle especially on his left side, wide arachnoid at temporal lobe and frontal lobe. Interictal EEGs found some low to medium amplitude spike wave and spike slow wave in sleep. Patient 3568 was a girl born after uneventful term delivery. There was no history of epilepsy and ID/DD in her family. The girl had complex focal seizures since 2.5 years. The seizures occurred intermittently with a frequency of 2 time per month. Her intellectual development was delayed. The MRI showed that two-side hippocampal sclerosis and abnormal signal at parietal lobe and temporal lobe (especially at the right sides). Besides epilepsy and ID/DD, they also suffered from encephalodysplasia. The reason may be this CNV have some genes of neurodevelopment, such as TBX1, ARVCF, RTN4R, and CRKL (Tables 9.2 and 9.4).
Based on the locus of the deletion and the clinic features, these patients would almost certainly suffer from 22q11.2 deletion syndrome. This syndrome involves a series of syndromes such as DiGeorge syndrome (DGS) (Kelley et al. 1982), velocardiofacial syndrome (VCFS) (Scambler et al. 1991; Driscoll et al. 1992), conotruncal anomaly face syndrome (CTAF) (Matsuoka et al. 1994), some cases of autosomal dominant Opitz G/BBB syndrome (McDonald-McGinn et al. 1995; Fryburg et al. 1996; Lacassie and Arriaza 1996), and Cayler cardiofacial syndrome (asymmetric crying facies) (Giannotti et al. 1994). Among candidate pathogenic genes, COMT is related to both epilepsy (Doyle and Sellinger 1980) and ID/DD (Zhang et al. 2007; Li et al. 2009). SNAP29 (Elfving et al. 2008) and TBX1 (Sedghi et al. 2012) have been proven to related to epilepsy.
In 2006, 5q34 was reported to be a susceptibility locus for idiopathic generalized epilepsy (Hempelmann et al. 2006). A 6.45 Mb deletion in 5q33-q34 and a 713 Kb deletion in 5q33.2 were reported by Mefford in 2010 and 2011 (Mefford et al. 2010, 2011) to be related to epilepsy and ID/DD. Our study found a patient was with a deletion in 5q33.1-q34. Among candidate pathogenic genes, CYFIP2 is highly expressed in the brain and contributes to both epilepsy (Hideyama et al. 2010) and ID/DD (Hoeffer et al. 2012). The other ID/DD gene is GLRA1 (Al-Futaisi et al. 2012), which encodes a subunit of glycine receptor.
In a research in 2013, Speriz reported that 17p13.2 may be an epilepsy and ID/DD related genetic region as a duplication (Spreiz et al. 2014). A deletion of 17p13.2 was also reported to be associated with Miller-Dieker lissencephaly syndrome (Chen et al. 2010). This report, together with our findings, indicates that 17p13.2 may be an important genetic region for gyrus development. Among pathogenic gene candidates, SRR, PAFAH1B1 and MRPL40 should be considered. AFAH1B1 was reported to be associated with lissencephaly (Cardoso et al. 2000; Kerjan and Gleeson 2007). R encodes serine racemase, which catalyzes l-serine to d-serine. d-serine is an important transmitter in brain and may be related to epilepsy (Ryu et al. 2010) and ID/DD (Klatte et al. 2013).
There were two patients (1549 and 5332) sharing the similar gene-deleted CNV in 5q13.2. Patient 1549 was a girl born after uneventful term delivery. She was the product of healthy parents without family history of epilepsy and ID/DD. However, this girl had generalized seizure since 4 years. The seizures are with a most frequency of 9 times per day. Her intellectual and motive developments were delayed. Her brain MRI was normal. Interictal EEGs found some low to medium amplitude spike wave and spike slow wave in sleep. Patient 5332 was a boy born after uneventful term delivery. There was no history of epilepsy and ID/DD in her family. The boy got complex focal seizures since 1 year 4 month. The seizures occurred intermittently with a frequency of 6–30 time per day. His intellectual development was delayed. EEGs found Generalized and multifocal spike wave and spike slow wave. The MRI showed that brain dysplasia with defect of myelination of white matter.
Patient 1549 also has a long deletion in Xp22.31. The patient 5332 also suffered from aphasia and muscle hypotonia. The level of galactose in urine was a little higher than the normal standard. 5q13.2 was not reported to be related to epilepsy or ID/DD. In this CNV, no gene in this CNV have been reported to involve in epilepsy and ID/DD. The candidate pathogenic genes in this deletion were SMN1, SMN2, OCLN, and NAIP. These genes are involved in neurodevelopment. SMN1 and SMN2 are important factor for motor neuron development, and associate with spinal muscular atrophy (Prior 2007). Knocking out SMN2 would increase seizure susceptibility (Gogliotti et al. 2011). OCLN encodes tight junction protein occludin, which is involved in the early stage of neurodevelopment (Virgintino et al. 2004). Occludin was reported to be overexpressed in Alzheimer’s disease and vascular dementia (Romanitan et al. 2007), so it may be related to ID/DD. Neurodevelopment related gene NAIP, which encodes Neuronal Apoptosis Inhibitory Protein (Mercer et al. 2000), was reported to decrease in brains of patients suffering with Down syndrome or Alzheimer’s disease (Seidl et al. 1999). It is indicated that NAIP may be related to ID/DD.
In an infantile spasms related deletion in Xp22 reported by Mefford, CDKL5 was reported as the candidate pathogenic gene (Mefford et al. 2011). In our study, a deletion of Xp22.31 in patient 1594 (who also had a 5q13.2 deletion) contained 4 genes, HDHD1A, STS, VCX, and PNPLA4. PNPLA4 may be involved to epilepsy and ID/DD (Carrascosa-Romero et al. 2012). STS and VCX was proven to take part in X-linked ID/DD (Ben Khelifa et al. 2013). As this patient is a girl, this heterozygous microdeletion in X chromosome may play a less role in the pathogenic mechanism.
9.4 Systems Biological Analysis
Recently, system biology has provided a series of powerful tools for biomedicine studies. As an important analysis method, network reconstruction was used in biomarker detection (Mitra et al. 2013), drug discovery (Zou et al. 2013), and for studying the synaptic plasticity (He et al. 2014) mechanism of learning and memory (Kandel et al. 2014). Network reconstruction is very suitable for studying the pathogenic mechanism of complex disease in CNS, such as autism (Corominas et al. 2014), schizophrenia (Sun et al. 2010), and tumor induced epilepsy (Mittal et al. 2013).
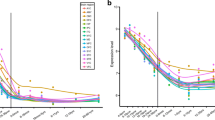
In this study, we also tried to use the analysis tools of systems biology to predict the common pathogenic mechanism for epilepsy and ID/DD as complex diseases. By the Cystoscope 3.1.0 (Shannon et al. 2003), the network of the known epilepsy genes (in Supplementary Table 9.1) and CNV genes was constructed based on genetic interaction, pathway, and physical interaction in GENEMANIA database (Montojo et al. 2010). Form the constructed network, we found 70.5% of the CNV genes (158/224) to be involved in a network, while only 3.5% CNV genes are known epilepsy-related genes (Fig. 9.5a). This result indicated that most of these genes are potential epilepsy related genes. All of the patients in our cohort have suffered from epilepsy and ID/DD, so we believe that there is some common pathogenic mechanism.
The network of epilepsy genes and CNV genes. (a) Systems biology analysis showed 151 CNV genes (151/224, 67.41%) were interacting with the known epilepsy genes. (b) The network of epilepsy genes with CNV genes. The genes in different CNVs was labeled by different colors (2q33.1-q34 in green, 5q33.1-q34 in purple, 22q11.21-q11.22 in orange, 17p13.2 in deep green, 5q13.2 in blue, 2q24.1 in red and Xp22.31 in cyan)
Interestingly, we found the BGNADP motif which was constructed by BTD, GALNT10, NMUR2, AUTS2, DLG2 and PTPRD (Fig. 9.5b). This motif was connected with each of the CNVs in our patients. The BGNADP motif is a small epilepsy and ID/DD related gene network. BTD is the gene of biotinidase. Mutations in BTD caused a disease called biotinidase deficiency, which is characterized by seizures, hypotonia, skin rash, ataxia hearing loss and optic atrophy (Hymes et al. 2001). AUTS2 (autism susceptibility candidate 2) is associated with a series of neurologic disorders, such as autism, attention deficit hyperactivity disorder, dyslexia, ID/DD and epilepsy (Poot et al. 2011; Jolley et al. 2013; Nagamani et al. 2013; Oksenberg et al. 2013). DLG2 encodes a membrane-associated guanylate kinase called PSD-93, which interacts at postsynaptic sites of neurons and forms a scaffold for the clustering receptors and ion channel. DLG2 expression was reported to increase in epilepsy, indicating the role of DLG2 in epilepsy (Liu et al. 2007). PTPRD is a member of the protein tyrosine phosphatase gene family. Deficiency of PTPRD results in ID/DD (Choucair et al. 2015). PTPRD is also an epilepsy candidate gene according to a genome-wide association study (Speed et al. 2014). GALNT10 and NMUR2 are members of the CNVs of our cohort. They have not yet been subjected to serious study, and should be targeted as candidate epilepsy and/or ID/DD genes in a further study. Our study has indicated that this BGNADP motif could be an important component in the common pathogenic mechanism. Further study should be needed to delineate the role of BGNADP in epilepsy and ID/DD.
References
Al-Futaisi AM, Al-Kindi MN, Al-Mawali AM, Koul RL, Al-Adawi S, Al-Yahyaee SA. Novel mutation of GLRA1 in Omani families with hyperekplexia and mild mental retardation. Pediatr Neurol. 2012;46(2):89–93.
Arai A, Saito T, Hanai S, Sukigara S, Nabatame S, Otsuki T, Nakagawa E, Takahashi A, Kaneko Y, Kaido T, Saito Y, Sugai K, Sasaki M, Goto Y, Itoh M. Abnormal maturation and differentiation of neocortical neurons in epileptogenic cortical malformation: unique distribution of layer-specific marker cells of focal cortical dysplasia and hemimegalencephaly. Brain Res. 2012;1470:89–97.
Barco A, Pittenger C, Kandel ER. CREB, memory enhancement and the treatment of memory disorders: promises, pitfalls and prospects. Expert Opin Ther Targets. 2003;7(1):101–14.
Barge-Schaapveld DQ, Ofman R, Knegt AC, Alders M, Hohne W, Kemp S, Hennekam RC. Intellectual disability and hemizygous GPD2 mutation. Am J Med Genet A. 2013;161A(5):1044–50.
Bassuk AG, Geraghty E, Wu S, Mullen SA, Berkovic SF, Scheffer IE, Mefford HC. Deletions of 16p11.2 and 19p13.2 in a family with intellectual disability and generalized epilepsy. Am J Med Genet A. 2013;161A(7):1722–5.
Ben Khelifa H, Soyah N, Ben-Abdallah-Bouhjar I, Gritly R, Sanlaville D, Elghezal H, Saad A, Mougou-Zerelli S. Xp22.3 interstitial deletion: a recognizable chromosomal abnormality encompassing VCX3A and STS genes in a patient with X-linked ichthyosis and mental retardation. Gene. 2013;527(2):578–83.
Caciotti A, Tonin R, Rigoldi M, Ferri L, Catarzi S, Cavicchi C, Procopio E, Donati MA, Ficcadenti A, Fiumara A, Barone R, Garavelli L, Rocco MD, Filocamo M, Antuzzi D, Scarpa M, Mooney SD, Li B, Skouma A, Bianca S, Concolino D, Casalone R, Monti E, Pantaleo M, Giglio S, Guerrini R, Parini R, Morrone A. Optimizing the molecular diagnosis of GALNS: novel methods to define and characterize Morquio-A syndrome-associated mutations. Hum Mutat. 2015;36(3):357–68.
Caiazzo M, Colucci-D’Amato L, Volpicelli F, Speranza L, Petrone C, Pastore L, Stifani S, Ramirez F, Bellenchi GC, di Porzio U. Kruppel-like factor 7 is required for olfactory bulb dopaminergic neuron development. Exp Cell Res. 2011;317(4):464–73.
Cardoso C, Leventer RJ, Matsumoto N, Kuc JA, Ramocki MB, Mewborn SK, Dudlicek LL, May LF, Mills PL, Das S, Pilz DT, Dobyns WB, Ledbetter DH. The location and type of mutation predict malformation severity in isolated lissencephaly caused by abnormalities within the LIS1 gene. Hum Mol Genet. 2000;9(20):3019–28.
Carrascosa-Romero MC, Suela J, Alfaro-Ponce B, Cepillo-Boluda AJ. [X-chromosome-linked ichthyosis associated to epilepsy, hyperactivity, autism and mental retardation, due to the Xp22.31 microdeletion]. Rev Neurol. 2012;54(4): 241–48.
Chelly J, Khelfaoui M, Francis F, Cherif B, Bienvenu T. Genetics and pathophysiology of mental retardation. Eur J Hum Genet. 2006;14(6):701–13.
Chen CP, Liu YP, Lin SP, Chen M, Tsai FJ, Chen YT, Chen LF, Hwang JK, Wang W. Ventriculomegaly, intrauterine growth restriction, and congenital heart defects as salient prenatal sonographic findings of Miller-Dieker lissencephaly syndrome associated with monosomy 17p (17p13.2 --> pter) in a fetus. Taiwan J Obstet Gynecol. 2010;49(1):81–6.
Choucair N, Mignon-Ravix C, Cacciagli P, Abou Ghoch J, Fawaz A, Megarbane A, Villard L, Chouery E. Evidence that homozygous PTPRD gene microdeletion causes trigonocephaly, hearing loss, and intellectual disability. Mol Cytogenet. 2015;8:39.
Chulanova TA, Echikov SN, Sadovnikov VB, Shchipakina TG. Functional peculiarities of MAP2 in DBA/2J inbred mice as a component of genetic predisposition to seizures. Bull Exp Biol Med. 2001;132(5):1058–61.
Cooper GM, Coe BP, Girirajan S, Rosenfeld JA, Vu TH, Baker C, Williams C, Stalker H, Hamid R, Hannig V, Abdel-Hamid H, Bader P, McCracken E, Niyazov D, Leppig K, Thiese H, Hummel M, Alexander N, Gorski J, Kussmann J, Shashi V, Johnson K, Rehder C, Ballif BC, Shaffer LG, Eichler EE. A copy number variation morbidity map of developmental delay. Nat Genet. 2011;43(9):838–46.
Corominas R, Yang X, Lin GN, Kang S, Shen Y, Ghamsari L, Broly M, Rodriguez M, Tam S, Trigg SA, Fan C, Yi S, Tasan M, Lemmens I, Kuang X, Zhao N, Malhotra D, Michaelson JJ, Vacic V, Calderwood MA, Roth FP, Tavernier J, Horvath S, Salehi-Ashtiani K, Korkin D, Sebat J, Hill DE, Hao T, Vidal M, Iakoucheva LM. Protein interaction network of alternatively spliced isoforms from brain links genetic risk factors for autism. Nat Commun. 2014;5:3650.
Daoud H, Gruchy N, Constans JM, Moussaoui E, Saumureau S, Bayou N, Amy M, Vedrine S, Vu PY, Rotig A, Laumonnier F, Vourc’h P, Andres CR, Leporrier N, Briault S. Haploinsufficiency of the GPD2 gene in a patient with nonsyndromic mental retardation. Hum Genet. 2009;124(6):649–58.
Derks EM, Ayub M, Chambert K, Del Favero J, Johnstone M, MacGregor S, Maclean A, McKechanie AG, McRae AF, Moran JL, Pickard BS, Purcell S, Sklar P, StClair DM, Wray NR, Visscher PM, Blackwood DH. A genome wide survey supports the involvement of large copy number variants in schizophrenia with and without intellectual disability. Am J Med Genet B Neuropsychiatr Genet. 2013;162B(8):847–54.
Dibbens LM, Mullen S, Helbig I, Mefford HC, Bayly MA, Bellows S, Leu C, Trucks H, Obermeier T, Wittig M, Franke A, Caglayan H, Yapici Z, Sander T, Eichler EE, Scheffer IE, Mulley JC, Berkovic SF. Familial and sporadic 15q13.3 microdeletions in idiopathic generalized epilepsy: precedent for disorders with complex inheritance. Hum Mol Genet. 2009;18(19):3626–31.
Doyle RL, Sellinger OZ. Differences in activity in cerebral methyltransferases and monoamine oxidases between audiogenic seizure susceptible and resistant mice and deermice. Pharmacol Biochem Behav. 1980;13(4):589–91.
Driscoll DA, Budarf ML, Emanuel BS. A genetic etiology for DiGeorge syndrome: consistent deletions and microdeletions of 22q11. Am J Hum Genet. 1992;50(5):924–33.
Elfving B, Bonefeld BE, Rosenberg R, Wegener G. Differential expression of synaptic vesicle proteins after repeated electroconvulsive seizures in rat frontal cortex and hippocampus. Synapse. 2008;62(9):662–70.
Fryburg JS, Lin KY, Golden WL. Chromosome 22q11.2 deletion in a boy with Opitz (G/BBB) syndrome. Am J Med Genet. 1996;62(3):274–5.
Fukata Y, Lovero KL, Iwanaga T, Watanabe A, Yokoi N, Tabuchi K, Shigemoto R, Nicoll RA, Fukata M. Disruption of LGI1-linked synaptic complex causes abnormal synaptic transmission and epilepsy. Proc Natl Acad Sci U S A. 2010;107(8):3799–804.
Giannotti A, Digilio MC, Marino B, Mingarelli R, Dallapiccola B. Cayler cardiofacial syndrome and del 22q11: part of the CATCH22 phenotype. Am J Med Genet. 1994;53(3):303–4.
Glass IA, Swindlehurst CA, Aitken DA, McCrea W, Boyd E. Interstitial deletion of the long arm of chromosome 2 with normal levels of isocitrate dehydrogenase. J Med Genet. 1989;26(2):127–30.
Gogliotti RG, Lutz C, Jorgensen M, Huebsch K, Koh S, Didonato CJ. Characterization of a commonly used mouse model of SMA reveals increased seizure susceptibility and heightened fear response in FVB/N mice. Neurobiol Dis. 2011;43(1):142–51.
Grayton HM, Fernandes C, Rujescu D, Collier DA. Copy number variations in neurodevelopmental disorders. Prog Neurobiol. 2012;99(1):81–91.
Grishin A, Li H, Levitan ES, Zaks-Makhina E. Identification of gamma-aminobutyric acid receptor-interacting factor 1 (TRAK2) as a trafficking factor for the K+ channel Kir2.1. J Biol Chem. 2006;281(40):30104–11.
Harvard C, Strong E, Mercier E, Colnaghi R, Alcantara D, Chow E, Martell S, Tyson C, Hrynchak M, McGillivray B, Hamilton S, Marles S, Mhanni A, Dawson AJ, Pavlidis P, Qiao Y, Holden JJ, Lewis SM, O’Driscoll M, Rajcan-Separovic E. Understanding the impact of 1q21.1 copy number variant. Orphanet J Rare Dis. 2011;6:54.
He Y, Kulasiri D, Samarasinghe S. Systems biology of synaptic plasticity: a review on N-methyl-D-aspartate receptor mediated biochemical pathways and related mathematical models. Biosystems. 2014;122:7–18.
Helbig I, Hartmann C, Mefford HC. Clarifying the role of the 22q11.2 microdeletion in juvenile myoclonic epilepsy. Epilepsy Behav. 2013;29(3):589–90.
Helbig I, Mefford HC, Sharp AJ, Guipponi M, Fichera M, Franke A, Muhle H, de Kovel C, Baker C, von Spiczak S, Kron KL, Steinich I, Kleefuss-Lie AA, Leu C, Gaus V, Schmitz B, Klein KM, Reif PS, Rosenow F, Weber Y, Lerche H, Zimprich F, Urak L, Fuchs K, Feucht M, Genton P, Thomas P, Visscher F, de Haan GJ, Moller RS, Hjalgrim H, Luciano D, Wittig M, Nothnagel M, Elger CE, Nurnberg P, Romano C, Malafosse A, Koeleman BP, Lindhout D, Stephani U, Schreiber S, Eichler EE, Sander T. 15q13.3 microdeletions increase risk of idiopathic generalized epilepsy. Nat Genet. 2009;41(2):160–2.
Hempelmann A, Taylor KP, Heils A, Lorenz S, Prud’homme JF, Nabbout R, Dulac O, Rudolf G, Zara F, Bianchi A, Robinson R, Gardiner RM, Covanis A, Lindhout D, Stephani U, Elger CE, Weber YG, Lerche H, Nurnberg P, Kron KL, Scheffer IE, Mulley JC, Berkovic SF, Sander T. Exploration of the genetic architecture of idiopathic generalized epilepsies. Epilepsia. 2006;47(10):1682–90.
Hideyama T, Yamashita T, Nishimoto Y, Suzuki T, Kwak S. Novel etiological and therapeutic strategies for neurodiseases: RNA editing enzyme abnormality in sporadic amyotrophic lateral sclerosis. J Pharmacol Sci. 2010;113(1):9–13.
Hoeffer CA, Sanchez E, Hagerman RJ, Mu Y, Nguyen DV, Wong H, Whelan AM, Zukin RS, Klann E, Tassone F. Altered mTOR signaling and enhanced CYFIP2 expression levels in subjects with fragile X syndrome. Genes Brain Behav. 2012;11(3):332–41.
Hymes J, Stanley CM, Wolf B. Mutations in BTD causing biotinidase deficiency. Hum Mutat. 2001;18(5):375–81.
Jalava NS, Lopez-Picon FR, Kukko-Lukjanov TK, Holopainen IE. Changes in microtubule-associated protein-2 (MAP2) expression during development and after status epilepticus in the immature rat hippocampus. Int J Dev Neurosci. 2007;25(2):121–31.
Jolley A, Corbett M, McGregor L, Waters W, Brown S, Nicholl J, Yu S. De novo intragenic deletion of the autism susceptibility candidate 2 (AUTS2) gene in a patient with developmental delay: a case report and literature review. Am J Med Genet A. 2013;161A(6):1508–12.
Kandel ER, Dudai Y, Mayford MR. The molecular and systems biology of memory. Cell. 2014;157(1):163–86.
Kelley RI, Zackai EH, Emanuel BS, Kistenmacher M, Greenberg F, Punnett HH. The association of the DiGeorge anomalad with partial monosomy of chromosome 22. J Pediatr. 1982;101(2):197–200.
Kerjan G, Gleeson JG. Genetic mechanisms underlying abnormal neuronal migration in classical lissencephaly. Trends Genet. 2007;23(12):623–30.
Kim EH, Yum MS, Lee BH, Kim HW, Lee HJ, Kim GH, Lee YJ, Yoo HW, Ko TS. Epilepsy and other neuropsychiatric manifestations in children and adolescents with 22q11.2 deletion syndrome. J Clin Neurol. 2016;12(1):85–92.
Klatte K, Kirschstein T, Otte D, Pothmann L, Muller L, Tokay T, Kober M, Uebachs M, Zimmer A, Beck H. Impaired D-serine-mediated cotransmission mediates cognitive dysfunction in epilepsy. J Neurosci. 2013;33(32):13066–80.
Kogan JH, Gross AK, Featherstone RE, Shin R, Chen Q, Heusner CL, Adachi M, Lin A, Walton NM, Miyoshi S, Miyake S, Tajinda K, Ito H, Siegel SJ, Matsumoto M. Mouse model of chromosome 15q13.3 microdeletion syndrome demonstrates features related to autism spectrum disorder. J Neurosci. 2015;35(49):16282–94.
de Kovel CG, Trucks H, Helbig I, Mefford HC, Baker C, Leu C, Kluck C, Muhle H, von Spiczak S, Ostertag P, Obermeier T, Kleefuss-Lie AA, Hallmann K, Steffens M, Gaus V, Klein KM, Hamer HM, Rosenow F, Brilstra EH, Trenite DK, Swinkels ME, Weber YG, Unterberger I, Zimprich F, Urak L, Feucht M, Fuchs K, Moller RS, Hjalgrim H, De Jonghe P, Suls A, Ruckert IM, Wichmann HE, Franke A, Schreiber S, Nurnberg P, Elger CE, Lerche H, Stephani U, Koeleman BP, Lindhout D, Eichler EE, Sander T. Recurrent microdeletions at 15q11.2 and 16p13.11 predispose to idiopathic generalized epilepsies. Brain. 2010;133(Pt 1):23–32.
Lacassie Y, Arriaza MI. Opitz GBBB syndrome and the 22q11.2 deletion. Am J Med Genet. 1996;62(3):318.
Layouni S, Salzmann A, Guipponi M, Mouthon D, Chouchane L, Dogui M, Malafosse A. Genetic linkage study of an autosomal recessive form of juvenile myoclonic epilepsy in a consanguineous Tunisian family. Epilepsy Res. 2010;90(1-2):33–8.
Lee BI, Heo K. Epilepsy: new genes, new technologies, new insights. Lancet Neurol. 2014;13(1):7–9.
Leoyklang P, Suphapeetiporn K, Siriwan P, Desudchit T, Chaowanapanja P, Gahl WA, Shotelersuk V. Heterozygous nonsense mutation SATB2 associated with cleft palate, osteoporosis, and cognitive defects. Hum Mutat. 2007;28(7):732–8.
Li J, Yu C, Li Y, Liu B, Liu Y, Shu N, Song M, Zhou Y, Zhu W, Li K, Jiang T. COMT val158met modulates association between brain white matter architecture and IQ. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(3):375–80.
Lin WD, Chang KP, Wang CH, Chen SJ, Fan PC, Weng WC, Lin WC, Tsai Y, Tsai CH, Chou IC, Tsai FJ. Molecular aspects of Dravet syndrome patients in Taiwan. Clin Chim Acta. 2013;421:34–40.
Liu FY, Wang XF, Li MW, Li JM, Xi ZQ, Luan GM, Zhang JG, Wang YP, Sun JJ, Li YL. Upregulated expression of postsynaptic density-93 and N-methyl-D-aspartate receptors subunits 2B mRNA in temporal lobe tissue of epilepsy. Biochem Biophys Res Commun. 2007;358(3):825–30.
Ma D, Williamson P, Januszewski A, Nogaro MC, Hossain M, Ong LP, Shu Y, Franks NP, Maze M. Xenon mitigates isoflurane-induced neuronal apoptosis in the developing rodent brain. Anesthesiology. 2007;106(4):746–53.
Maden CH, Gomes J, Schwarz Q, Davidson K, Tinker A, Ruhrberg C. NRP1 and NRP2 cooperate to regulate gangliogenesis, axon guidance and target innervation in the sympathetic nervous system. Dev Biol. 2012;369(2):277–85.
Matsuoka R, Takao A, Kimura M, Imamura S, Kondo C, Joh-o K, Ikeda K, Nishibatake M, Ando M, Momma K. Confirmation that the conotruncal anomaly face syndrome is associated with a deletion within 22q11.2. Am J Med Genet. 1994;53(3):285–9.
McDonald-McGinn DM, Driscoll DA, Bason L, Christensen K, Lynch D, Sullivan K, Canning D, Zavod W, Quinn N, Rome J. Autosomal dominant “Opitz” GBBB syndrome due to a 22q11.2 deletion. Am J Med Genet. 1995;59(1):103–13.
Mefford HC, Muhle H, Ostertag P, von Spiczak S, Buysse K, Baker C, Franke A, Malafosse A, Genton P, Thomas P, Gurnett CA, Schreiber S, Bassuk AG, Guipponi M, Stephani U, Helbig I, Eichler EE. Genome-wide copy number variation in epilepsy: novel susceptibility loci in idiopathic generalized and focal epilepsies. PLoS Genet. 2010;6(5):e1000962.
Mefford HC, Yendle SC, Hsu C, Cook J, Geraghty E, McMahon JM, Eeg-Olofsson O, Sadleir LG, Gill D, Ben-Zeev B, Lerman-Sagie T, Mackay M, Freeman JL, Andermann E, Pelakanos JT, Andrews I, Wallace G, Eichler EE, Berkovic SF, Scheffer IE. Rare copy number variants are an important cause of epileptic encephalopathies. Ann Neurol. 2011;70(6):974–85.
Mercer EA, Korhonen L, Skoglosa Y, Olsson PA, Kukkonen JP, Lindholm D. NAIP interacts with hippocalcin and protects neurons against calcium-induced cell death through caspase-3-dependent and -independent pathways. EMBO J. 2000;19(14):3597–607.
Mertz LG, Christensen R, Vogel I, Hertz JM, Nielsen KB, Gronskov K, Ostergaard JR. Angelman syndrome in Denmark. Birth incidence, genetic findings, and age at diagnosis. Am J Med Genet A. 2013;161A(9):2197–203.
Messmer K, Remington MP, Skidmore F, Fishman PS. Induction of tyrosine hydroxylase expression by the transcription factor Pitx3. Int J Dev Neurosci. 2007;25(1):29–37.
Mitra S, Das S, Chakrabarti J. Systems biology of cancer biomarker detection. Cancer Biomark. 2013;13(4):201–13.
Mittal S, Shah AK, Barkmeier DT, Loeb JA. Systems biology of human epilepsy applied to patients with brain tumors. Epilepsia. 2013;54(Suppl 9):35–9.
Montojo J, Zuberi K, Rodriguez H, Kazi F, Wright G, Donaldson SL, Morris Q, Bader GD. GeneMANIA Cytoscape plugin: fast gene function predictions on the desktop. Bioinformatics. 2010;26(22):2927–8.
Mulley JC, Scheffer IE, Desai T, Bayly MA, Grinton BE, Vears DF, Berkovic SF, Dibbens LM. Investigation of the 15q13.3 CNV as a genetic modifier for familial epilepsies with variable phenotypes. Epilepsia. 2011;52(10):e139–42.
Nagamani SC, Erez A, Ben-Zeev B, Frydman M, Winter S, Zeller R, El-Khechen D, Escobar L, Stankiewicz P, Patel A, Cheung SW. Detection of copy-number variation in AUTS2 gene by targeted exonic array CGH in patients with developmental delay and autistic spectrum disorders. Eur J Hum Genet. 2013;21(3):343–6.
Oksenberg N, Stevison L, Wall JD, Ahituv N. Function and regulation of AUTS2, a gene implicated in autism and human evolution. PLoS Genet. 2013;9(1):e1003221.
Olszewski AK, Radoeva PD, Fremont W, Kates WR, Antshel KM. Is child intelligence associated with parent and sibling intelligence in individuals with developmental disorders? An investigation in youth with 22q11.2 deletion (velo-cardio-facial) syndrome. Res Dev Disabil. 2014;35(12):3582–90.
Owuor K, Harel NY, Englot DJ, Hisama F, Blumenfeld H, Strittmatter SM. LGI1-associated epilepsy through altered ADAM23-dependent neuronal morphology. Mol Cell Neurosci. 2009;42(4):448–57.
Paciorkowski AR, Thio LL, Rosenfeld JA, Gajecka M, Gurnett CA, Kulkarni S, Chung WK, Marsh ED, Gentile M, Reggin JD, Wheless JW, Balasubramanian S, Kumar R, Christian SL, Marini C, Guerrini R, Maltsev N, Shaffer LG, Dobyns WB. Copy number variants and infantile spasms: evidence for abnormalities in ventral forebrain development and pathways of synaptic function. Eur J Hum Genet. 2011;19(12):1238–45.
Pichler I, Schwienbacher C, Zanon A, Fuchsberger C, Serafin A, Facheris MF, Marroni F, Pattaro C, Shen Y, Tellgren-Roth C, Gyllensten U, Gusella JF, Hicks AA, Pramstaller PP. Fine-mapping of restless legs locus 4 (RLS4) identifies a haplotype over the SPATS2L and KCTD18 genes. J Mol Neurosci. 2013;49(3):600–5.
Poot M, van der Smagt JJ, Brilstra EH, Bourgeron T. Disentangling the myriad genomics of complex disorders, specifically focusing on autism, epilepsy, and schizophrenia. Cytogenet Genome Res. 2011;135(3-4):228–40.
Prior TW. Spinal muscular atrophy diagnostics. J Child Neurol. 2007;22(8):952–6.
Riley KN, Catalano LM, Bernat JA, Adams SD, Martin DM, Lalani SR, Patel A, Burnside RD, Innis JW, Rudd MK. Recurrent deletions and duplications of chromosome 2q11.2 and 2q13 are associated with variable outcomes. Am J Med Genet A. 2015;167A(11):2664–73.
Romanitan MO, Popescu BO, Winblad B, Bajenaru OA, Bogdanovic N. Occludin is overexpressed in Alzheimer’s disease and vascular dementia. J Cell Mol Med. 2007;11(3):569–79.
Rosenfeld JA, Ballif BC, Lucas A, Spence EJ, Powell C, Aylsworth AS, Torchia BA, Shaffer LG. Small deletions of SATB2 cause some of the clinical features of the 2q33.1 microdeletion syndrome. PLoS One. 2009;4(8):e6568.
Ryu HJ, Kim JE, Yeo SI, Kim DS, Kwon OS, Choi SY, Kang TC. Potential roles of D-serine and serine racemase in experimental temporal lobe epilepsy. J Neurosci Res. 2010;88(11):2469–82.
Scambler PJ, Carey AH, Wyse RK, Roach S, Dumanski JP, Nordenskjold M, Williamson R. Microdeletions within 22q11 associated with sporadic and familial DiGeorge syndrome. Genomics. 1991;10(1):201–6.
Sedghi M, Nouri N, Abdali H, Memarzadeh M, Nouri N. A case report of 22q11 deletion syndrome confirmed by array-CGH method. J Res Med Sci. 2012;17(3):310–2.
Seidl R, Bajo M, Bohm K, LaCasse EC, MacKenzie AE, Cairns N, Lubec G. Neuronal apoptosis inhibitory protein (NAIP)-like immunoreactivity in brains of adult patients with Down syndrome. J Neural Transm Suppl. 1999;57:283–91.
Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, Amin N, Schwikowski B, Ideker T. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13(11):2498–504.
Sisodiya SM, Mefford HC. Genetic contribution to common epilepsies. Curr Opin Neurol. 2011;24(2):140–5.
Speed D, Hoggart C, Petrovski S, Tachmazidou I, Coffey A, Jorgensen A, Eleftherohorinou H, De Iorio M, Todaro M, De T, Smith D, Smith PE, Jackson M, Cooper P, Kellett M, Howell S, Newton M, Yerra R, Tan M, French C, Reuber M, Sills GE, Chadwick D, Pirmohamed M, Bentley D, Scheffer I, Berkovic S, Balding D, Palotie A, Marson A, O’Brien TJ, Johnson MR. A genome-wide association study and biological pathway analysis of epilepsy prognosis in a prospective cohort of newly treated epilepsy. Hum Mol Genet. 2014;23(1):247–58.
Spreiz A, Haberlandt E, Baumann M, Baumgartner Sigl S, Fauth C, Gautsch K, Karall D, Janetschek C, Rostasy K, Scholl-Burgi S, Zotter S, Utermann G, Zschocke J, Kotzot D. Chromosomal microaberrations in patients with epilepsy, intellectual disability, and congenital anomalies. Clin Genet. 2014;86(4):361–6.
Sun J, Jia P, Fanous AH, van den Oord E, Chen X, Riley BP, Amdur RL, Kendler KS, Zhao Z. Schizophrenia gene networks and pathways and their applications for novel candidate gene selection. PLoS One. 2010;5(6):e11351.
Tiwari VN, Sundaram SK, Chugani HT, Huq AH. Infantile spasms are associated with abnormal copy number variations. J Child Neurol. 2013;28(10):1191–6.
Tuchman R, Moshe SL, Rapin I. Convulsing toward the pathophysiology of autism. Brain Dev. 2009;31(2):95–103.
Usui D, Shimada S, Shimojima K, Sugawara M, Kawasaki H, Shigematu H, Takahashi Y, Inoue Y, Imai K, Yamamoto T. Interstitial duplication of 2q32.1-q33.3 in a patient with epilepsy, developmental delay, and autistic behavior. Am J Med Genet A. 2013;161A(5):1078–84.
Van Buggenhout G, Van Ravenswaaij-Arts C, Mc Maas N, Thoelen R, Vogels A, Smeets D, Salden I, Matthijs G, Fryns JP, Vermeesch JR. The del(2)(q32.2q33) deletion syndrome defined by clinical and molecular characterization of four patients. Eur J Med Genet. 2005;48(3):276–89.
Vanlerberghe C, Petit F, Malan V, Vincent-Delorme C, Bouquillon S, Boute O, Holder-Espinasse M, Delobel B, Duban B, Vallee L, Cuisset JM, Lemaitre MP, Vantyghem MC, Pigeyre M, Lanco-Dosen S, Plessis G, Gerard M, Decamp M, Mathieu M, Morin G, Jedraszak G, Bilan F, Gilbert-Dussardier B, Fauvert D, Roume J, Cormier-Daire V, Caumes R, Puechberty J, Genevieve D, Sarda P, Pinson L, Blanchet P, Lemeur N, Sheth F, Manouvrier-Hanu S, Andrieux J. 15q11.2 microdeletion (BP1-BP2) and developmental delay, behaviour issues, epilepsy and congenital heart disease: a series of 52 patients. Eur J Med Genet. 2015;58(3):140–7.
Virgintino D, Errede M, Robertson D, Capobianco C, Girolamo F, Vimercati A, Bertossi M, Roncali L. Immunolocalization of tight junction proteins in the adult and developing human brain. Histochem Cell Biol. 2004;122(1):51–9.
Wang JW, Shi XY, Kurahashi H, Hwang SK, Ishii A, Higurashi N, Kaneko S, Hirose S. Prevalence of SCN1A mutations in children with suspected Dravet syndrome and intractable childhood epilepsy. Epilepsy Res. 2012;102(3):195–200.
Williams HJ, Owen MJ, O’Donovan MC. Schizophrenia genetics: new insights from new approaches. Br Med Bull. 2009;91:61–74.
Yamada K, Iwayama Y, Toyota T, Ohnishi T, Ohba H, Maekawa M, Yoshikawa T. Association study of the KCNJ3 gene as a susceptibility candidate for schizophrenia in the Chinese population. Hum Genet. 2012;131(3):443–51.
Yu HE, Hawash K, Picker J, Stoler J, Urion D, Wu BL, Shen Y. A recurrent 1.71 Mb genomic imbalance at 2q13 increases the risk of developmental delay and dysmorphism. Clin Genet. 2012;81(3):257–64.
Zhang F, Gu W, Hurles ME, Lupski JR. Copy number variation in human health, disease, and evolution. Annu Rev Genomics Hum Genet. 2009;10:451–81.
Zhang K, Gao J, An C, Gao X, Zheng Z, Li R, Huang S, Zhang F. An association study between cathechol-O-methyltransferase gene and mental retardation in the Chinese Han population. Neurosci Lett. 2007;419(1):83–7.
Zhang Y, Kong W, Gao Y, Liu X, Gao K, Xie H, Wu Y, Zhang Y, Wang J, Gao F, Wu X, Jiang Y. Gene mutation analysis in 253 Chinese children with unexplained epilepsy and intellectual/developmental disabilities. PLoS One. 2015;10(11):e0141782.
Zou J, Zheng MW, Li G, Su ZG. Advanced systems biology methods in drug discovery and translational biomedicine. Biomed Res Int. 2013;2013:742835.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
9.1 Electronic Supplementary Material
Supplementary Table 9.1
(XLS 34 kb)
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Gao, K. et al. (2018). Large De Novo Microdeletion in Epilepsy with Intellectual and Developmental Disabilities, with a Systems Biology Analysis. In: Cheung-Hoi Yu, A., Li, L. (eds) Systems Neuroscience. Advances in Neurobiology, vol 21. Springer, Cham. https://doi.org/10.1007/978-3-319-94593-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-94593-4_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-94591-0
Online ISBN: 978-3-319-94593-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)