Abstract
Cardiovascular disease (CVD) constitutes a major public health problem both in the developed and developing countries. Africa is characterized by a lack of good registries on incidence and mortality of non-communicable diseases (NCDs). Nevertheless, the Global Burden of Disease group, with the data available, showed recently that among the estimated 422 million cases of existing cardiovascular disease in the world in 2015, the age-adjusted higher prevalence of cases were from western and eastern Africa. Specifically, hypertensive heart disease was more prevalent in Africa, and this was accompanied by a higher mortality rate of this condition in this continent compared with other parts of the world.
LMIC are faced with a dual burden of communicable and chronic diseases, which require tertiary care, and a consequent diversion of the limited resources available. In conjunction with the loss of productive years of life, the consequences lead to economic constraints with an impact on both the private and the public sectors. The rising incidence of hypertension in Africa, its high general prevalence and poor control, as well as the premature mortality, makes issues related with hypertension highly relevant for the continent. Various factors have been shown to impact upon the development of left ventricular (LV) hypertrophy (LVH) and LV geometric changes. However, to date, the most consistent explanation for an increased prevalence of LVH and LV geometric remodelling in African populations is a higher pressure load. Bearing in mind the higher prevalence of LVH, especially concentric LVH, in Black Africans, and the higher mortality associated with LVH observed in Black African Americans, it is relevant to discuss issues related with early detection of LVH, intervention for LVH, as well as the consequence of LVH and geometric changes. These issues are paramount in Africa.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Hypertension in Africa
- Left ventricular hypertrophy
- Left ventricular geometric remodelling
- Heart failure in Africa
- Echocardiography
- Electrocardiography
1 Introduction
Cardiovascular disease (CVD) constitutes a major public health problem both in the developed and developing countries. Africa is characterized by a lack of good registries on incidence and mortality of non-communicable diseases (NCDs). Nevertheless, the Global Burden of Disease group [1], with the data available, showed recently that among the estimated 422 million cases of existing cardiovascular disease in the world in 2015, the age-adjusted highest prevalence of cases were from western and eastern Africa. Specifically, hypertensive heart disease was more prevalent in Africa, and this was accompanied by a higher mortality rate of this condition in this continent compared with other parts of the world.
Another important issue is the relative weight of CVD mortality related to the more important infectious diseases in Africa [2]. Of the 58 million deaths from all causes worldwide in 2005, an estimated 17.5 million were due to CVD, three times more deaths than those caused by infectious diseases including HIV/AIDS, tuberculosis and malaria combined.
LMIC are faced with a dual burden of communicable and chronic diseases, which require tertiary care, and a consequent diversion of the limited resources available. In conjunction with the loss of productive years of life, the consequences lead to economic constraints with an impact on both the private and the public sectors.
Sub-Saharan African (SSA) countries are currently experiencing one of the most rapid epidemiological transitions characterized by increasing urbanization and changing lifestyle factors [3], which in turn have raised the incidence of NCDs and CVD including hypertension [4].
The pattern of increasing risk factors with higher rates of urbanization is likely to affect most of SSA [5]. As “civilization” spreads, so does CVD, becoming an increasing health burden that requires skilful and cost-effective management [6].
2 The Epidemiology of Hypertension in Africa
Hypertension is the main risk factor for general morbidity and mortality in the world. With a worldwide distribution, its presence in SSA is relatively recent. A paper published in the 1930s [7] reported that among 1800 patients screened for 2 years, not a single case of high blood pressure was found in a rural community of Kenya. Since then, a great change has occurred. A recent review by Ogah et al. [8] revealed the prevalence of hypertension in the two national studies from SSA was about 31% (35.7% and 37% in men and 37% and 29% in women in Mozambique and Malawi, respectively). They also found that, in rural areas, the prevalence ranged from 16% in rural Rwanda to as high as 46.4% in a rural community in Eastern Nigeria. The values for urban studies ranged from 15.2% in the Democratic Republic of Congo to as high as 47.5% in Cameroon. During the last 40 years while in most of the developed world mean systolic and diastolic blood pressure are decreasing, in SSA, the situation is inverse with a significant increase of both in both sexes [9]. The evolution of the prevalence of hypertension and the mean systolic and diastolic blood pressure shows a constant increase in SSA making this continent the one with the highest prevalence rates of hypertension in the world. Added to this high prevalence, a second major issue is related to its extremely low levels of awareness. In most of these countries the levels of awareness are below 30%. Women and urban populations have a higher level of awareness compared with man and rural populations. Nevertheless in several countries, less than 10% of all hypertensive patients have their blood pressure controlled. In a recent review comparing the levels of awareness, treatment and control in different parts of the world between 2000 and 2010 [10], SSA countries were among the regions with the lowest levels of awareness, treatment and control, which allied with the high prevalence rates are likely to result in an enormous burden of target organ damage mainly stroke and heart failure. The rising incidence of hypertension, its high general prevalence and poor control, as well as the premature mortality, calls for more research into the details of hypertension on the continent.
3 From Hypertension to Hypertrophy to Heart Failure
Left ventricular (LV) hypertrophy (LVH) is defined as an increase in LV mass (LVM) either with or without LV geometric changes. As the current gold standard measurement for LV mass and LV geometric changes is echocardiography, we will primarily focus on the current literature pertaining to echocardiographic data. However, as Africa largely consists of poorly resourced communities with limited access to echocardiography, a section on electrocardiographic (ECG) determined LVH has also been included.
Currently various thresholds and indexations are used to define the presence of an increased echocardiographic LVM and hence LVH. These indexations and thresholds are discussed in detail below. The LV geometric changes depend upon the presence or absence of LV wall thickening. In this regard, concentricity is defined as an LV relative wall thickness (RWT, the ratio of the thickness of the LV wall to the diameter of the LV chamber diameter) of ≥0.42. Concentric LV remodelling refers to those patients in whom there is no LVH, but the RWT is ≥0.42, whereas in concentric LVH, there are both an increased LVM and RWT. Patients in whom LVH is present but the RWT is <0.42 are classified as having eccentric LVH.
The classification of patients according to the presence or absence of LVH and LV geometric changes is important as both have prognostic implications. In this regard, LVH is an independent predictor of cardiovascular mortality and morbidity [11]. In addition, LV geometric changes are associated with an increased risk of mortality and morbidity [12], with concentric LVH having the highest risk followed by eccentric LVH and then concentric remodelling [12, 13]. As there is a higher prevalence of concentric LVH in African American Blacks compared to Whites [14,15,16], the question arises whether such ethnic differences have been documented in Africa. Currently, no direct Black versus White comparisons are available in Africa; however, a high prevalence of concentricity similar to that in African American Blacks is reported in South African Blacks.
Although the prognostic implications of LVH and geometric remodelling in Africans living in Africa are currently unknown, longitudinal studies in African Americans suggest that LVH contributes more to the risk of cardiovascular mortality in Blacks than it does in Whites [17, 18]. Moreover, in African Americans, for every 100 deaths, 37% were attributable to LVH which is far greater than the percentages attributable to single-vessel disease (1%), LV systolic dysfunction (9%) and multi-vessel disease (22%) [17]. Bearing in mind the higher prevalence of LVH, especially concentric LVH, in Black Africans, and the higher mortality associated with LVH in Black African Americans [19], early detection of and intervention for LVH are paramount in Africa.
4 Indexations of LVM to Define LVH
To define LVH, various indexes of LVM have been used. The indexation of LVM to body surface area (BSA) is largely designed to eliminate the effects of body size, whereas the indexation to allometric signals of body height (e.g. 1.7 and 2.7) eliminates the impact of growth but not obesity on LVM. Consequently, indexation of LVM to allometric signals of height has been recommended in guidelines for the management of hypertension and for the assessment of LVH in the overweight and obese [20]. Indeed, in a large (n = 5004) multiethnic (White, Black, Hispanic and Chinese) community-based study in the USA, when using LVM indexed to BSA, the prevalence of LVH did not differ (p = 0.19) between normal weight (9.1%), overweight (7.5%) and obese (8.5%) participants [21, 22]. However, when using LVM indexed to height1.7, the prevalence of LVH in overweight (17.6%) and obese (40.4%) was markedly higher compared to when using LVM indexed to BSA and indeed differed substantially from the prevalence in normal weight participants (9.2%, p < 0.0001) [21, 22]. Similar differences have been observed when assessing the prevalence of LVH in African populations. Data from a community-based study (n = 793 Blacks) in South Africa showed that the prevalence of LVH in overweight (28.1%) and obese participants (43.2%) when using LVM indexed to height1.7 was higher (p < 0.0001) than that in normal weight participants (10.3%). Similarly, the prevalence of LVH in overweight (25.5%) and obese participants (41.8%) when using LVM indexed to height2.7 was higher (p < 0.0001) than that in normal weight participants (10.3%). However, when using LVM indexed to BSA (overweight = 19.3%; obese = 18.9%), the prevalence of LVH was no different (p = 0.18) from that in normal weight participants (13.9%) [22,23,24].
4.1 Thresholds for Echocardiographic LVH
Thresholds for echocardiographic LVH have largely been derived from White populations. There is limited data from other ethnic groups and particularly from Black Africans. As ethnic groups differ in anthropometric variables which impact on heart size [25], ethnic-specific thresholds may be required. Indeed, the EchoNoRMAL study (see data provided for Europeans, Africans and African Americans in Table 7.1) showed substantial differences in the thresholds between ethnic groups. Nevertheless, to date, only two studies have defined thresholds for echocardiographic LVH in healthy, non-hypertensive, nondiabetic, nonobese Black Africans (Table 7.1) [26, 27]. Data from Woodiwiss and Norton (unpublished) are preliminary reported here [28]. The EchoNoRMAL study included 227 females from seven studies in Africa and 190 males from five studies in Africa. The countries from which these African participants were recruited were not listed. Thresholds were defined for LVM indexed to height1.7 and height2.7, but not BSA. It is clear that within the EchoNoRMAL study, the thresholds for African participants differed from those for Europeans as well as to some degree from those for African Americans. Similarly, the thresholds defined in the South African study [27] differed from those obtained in Europeans/Whites and African Americans, especially when LVM was indexed to height1.7 or BSA. Indeed, the thresholds for LVM indexed to height2.7 appear to show more uniformity across ethnic groups than thresholds for either LVM indexed to height1.7 or BSA. These differences highlight the need to define thresholds specific to Black African populations. In addition, as within ethnic groups thresholds also differed according to gender, gender-specific thresholds are recommended (Table 7.1).
4.2 Prevalence of LVH and LV Geometric Patterns
Large cohort studies have provided evidence that LV mass indexed to height2.7 [14, 15, 30] and the prevalence of LVH [14, 15] is higher in African Americans than in Whites. A higher LVMI (g/m2.7) was evident in a longitudinal study of young adults (the Coronary Artery Disease Risk Development in Young Adults, CARDIA, study) (566 African Americans and 792 Whites) at both baseline [31] and after 5 years of follow-up [30] in both women and men, despite a low prevalence of LVH (<5%). Similarly, in the Hypertension Genetic Epidemiology Network (HyperGEN) study (1060 African Americans and 580 Whites), in multivariate analyses, the African Americans had a 1.8-fold higher prevalence of LVH (defined by indexation to height2.7) and a 2.5-fold higher prevalence of LVH (defined by indexation to BSA) compared to the Whites [15]. In the Dallas Heart Study (1335 African Americans and 858 Whites) (age = 30–65 years), the prevalence of LVH (indexed to height2.7 or BSA) was 2–3 times greater in African Americans compared to Whites [14]. The higher LVM observed in African Americans persisted after adjustments for fat mass, fat-free mass, SBP, age, gender and socioeconomic status [14]. Nevertheless, for a given level of SBP, a higher prevalence of LVH was observed in African Americans compared to Whites [14]. In addition, a greater degree of LV concentricity has been reported among African Americans compared to Whites [14,15,16]. Moreover, after adjusting for covariates, African Americans had a 2.3-fold higher prevalence of concentric geometry (defined by RWT ≥0.43) [15]. It has therefore been suggested that the greater LVM and LV remodelling in African Americans is driven by a greater pressure overload.
There are currently no direct evaluations of the prevalence of LVH and/or LV geometric patterns in Blacks versus Whites living in Africa. Data are therefore provided from a large cross-sectional community-based study in Blacks living in South Africa [28], for informal comparisons with data from the literature in Whites and African Americans (Table 7.2). It is clearly evident from this table that the prevalence of LVH is strongly influenced by the type of indexation of LVM. When LVM is indexed to BSA, the prevalence is much lower than when LVM is indexed to height2.7. This is largely because indexation to BSA eliminates the effects of obesity on LVM. With respect to ethnic differences, the prevalence of LVH in Black South Africans more closely represents that in African Americans, with both being higher than in Whites. Similarly, as reported for African Americans versus Whites, there is a higher frequency of concentricity in the Black South Africans.
4.3 Detection of LVH: Electrocardiography (ECG) Versus Echocardiography and Challenges with Accuracy of ECG
Although the current gold standard for the detection of LVH is echocardiography, access to echocardiography proves to be problematic in Africa with vast areas of the continent being largely underdeveloped. Hence, in many settings, the detection of LVH relies on electrocardiography (ECG) as a more accessible and cost-effective option. However, it is well recognized that ECG criteria have a poor sensitivity in detecting LVH in comparison to imaging techniques [34]. In addition to comparisons between modalities used to detect LVH, ethnic differences in the ability of ECG to detect LVH have been reported [11]. Indeed, ECG criteria for LVH have been shown to be less well correlated with echocardiographic LV mass index in African Americans as compared to Caucasians [35]. These poor correlations may be attributed to increased ECG amplitudes in groups of African descent [36, 37], possibly produced by alterations in skin conductivity [38], or a diminished thoracic diameter reducing the distance from the skin surface to the heart [39]. In addition, an excess adiposity attenuates the utility of all ECG voltage criteria for LVH detection [40]. Consequently, the sensitivity of some ECG criteria may be particularly low for the detection of LVH in groups of Black African ancestry [40,41,42]. Hence, the value of ECG criteria for the detection of LVH in individuals of Black African ancestry has been questioned [41, 43]. Moreover, none of the current ECG voltage criteria can be recommended for the use in obese people of Black African ancestry [40]. However, as universal screening for LVH using echocardiography carries a high cost [44], solutions to reducing these costs are required. Moreover, bearing in mind the limited access to alternative measures, especially in Africa, various options to try and improve on the accuracy of ECG in detecting LVH have therefore been proposed.
A composite of Cornell product with Sokolow voltage or Sokolow product increases the diagnostic ability of ECG [45]. In addition, the composite of these voltages was associated with increased LVM index and a greater prevalence of echocardiographic LVH than either criterion alone. Moreover, in the LIFE study (only 5.8% Blacks), a combination of Cornell product and Sokolow-Lyon voltage was associated with a higher rate of myocardial infarction, stroke, cardiovascular death and all-cause mortality (4.8 year follow-up in hypertensive patients) in comparison to either criterion alone or neither [46]. These data from predominantly non-African communities suggest that in resource-limited settings (such as in Africa), ECG is still a useful tool especially when combined with other clinical criteria and when ECG criteria are combined in preference to being used alone. However, are there data in African communities indicating possibilities for improving the accuracy of ECG criteria in detecting LVH?
In a study of 182 Cameroonian patients (69% with echocardiographic LVH), adjusting Sokolow-Lyon voltage to BSA or body mass index (BMI) improved the sensitivity from 26.5% to 55.8% and 58.4%, respectively [47]. However, these improved sensitivities were associated with reductions in specificity from 84.1% (unadjusted) to 46.4% (BSA adjusted) and 40.6% (BMI adjusted). Hence there was limited improvement in accuracy (unadjusted = 48.4%, BSA adjusted = 52.2%, BMI adjusted = 51.7%). Adjustments of Cornell voltage to BSA or BMI proved more promising with improvements in sensitivity from 37.2% to 68.1% and 69.0%, respectively, associated with increases in accuracy from 56.0% to 62.1% and 61.5%, respectively [47].
In 621 participants of African ancestry (South African), the accuracy of a combination of ECG criteria with readily available clinical variables [age, BMI, systolic blood pressure (SBP) or estimated glomerular filtration rate (eGFR)] was compared to the accuracy of ECG criteria alone [48]. Compared with ECG criteria alone, the combination of individual ECG criteria with age, BMI and SBP showed an improved level of performance [area under the receiver operator characteristic (ROC) curve, AUC] for all ECG criteria for LVH detection (ECG alone = 0.65–0.71; ECG plus age, BMI, SBP = 0.78–0.79, p < 0.005; ECG plus age, BMI, eGFR = 0.78, p < 0.005). In addition, the sensitivity at 85% specificity was increased (ECG alone = 32.6%–37.2%; ECG plus age, BMI, SBP = 46.5%–52.7%, p < 0.005; ECG plus age, BMI, eGFR = 42.6%–48.8%, p < 0.005). However, the use of both SBP and eGFR in combination with age, BMI and ECG criteria did not further enhance the performance of ECG criteria. Another approach to improve the ability of ECG criteria to detect LVH in a group of African descent (South African) was to correct ECG QRS voltages for the attenuating effect of BMI [27]. In 661 randomly selected participants (43.0% obese) of Black African ancestry in South Africa, correcting RaVL and Lewis voltages by the difference in the slope of BMI-voltage relations in those with BMI < 29 kg/m2 versus those with BMI ≥ 29 kg/m2 showed the greatest performance (AUC) for LVH detection (uncorrected RaVL = 0.69, corrected RaVL = 0.73, p < 0.0001) and also increased the sensitivity (uncorrected RaVL = 30.6%, corrected RaVL = 42.4%, p < 0.0005) with no change in specificity (uncorrected RaVL = 86.3%, corrected RaVL = 83.0%; p = 0.28). These novel approaches [27, 48] offer practically useful alternatives to improve the performance and sensitivity for LVH detection in individuals of African ancestry.
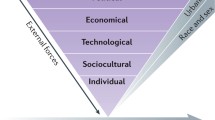
4.4 Factors That Contribute Towards Ethnic Differences in the Prevalence of LVH and Concentric Geometry
Various factors have been shown to impact upon the development of LVH and LV geometric changes. Importantly, increased LVM and LV remodelling among different ethnic groups could be influenced by socioeconomic factors, as well as dietary and lifestyle risk factors for cardiovascular disease. However, to date, the most consistent explanation for an increased prevalence of LVH and LV geometric remodelling in African populations is a higher pressure load. A recent ECG study comparing Black Nigerians to White Flemish reported a threefold steeper relationship between SBP and ECG voltages in the Blacks versus the Whites [49]. The higher prevalence of ECG LVH in the Blacks (54.4%) versus the Whites (36.0%) was in part attributed to this steeper relationship. These data confirm previous reports of a steeper relationship between BP and LVM in African American Blacks compared to Whites [14, 30, 50]. Moreover, in a cross-sectional study of 430 hypertensive Black South Africans, blood pressure was the strongest determinant of ECG-LVH, independent of age, BMI, antihypertensive use and markers of a poor lifestyle (smoking drinking, cholesterol, diabetes) [51]. Similarly, in a study of stroke patients in Ghana and Nigeria, blood pressure was the major modifiable risk factor which independently predicted LVH [52]. In a cross-sectional community-based study of Blacks in South Africa, pulse pressure (the difference between SBP and DBP) was associated with an increased LVM index as well as LVH [33]. In addition, aortic stiffness (pulse wave velocity) was associated with an increased LVM index as well as LVH, independent of pulse pressure [33]. Although augmentation index (a marker of aortic function) is increased in Blacks in South Africa compared to Whites [53], whether the ethnic differences in aortic stiffness contribute towards ethnic differences in LVM and LVH is not known.
Obesity is also an important determinant of LVH and LV geometric changes. Independent of age and blood pressure, BMI was a strong predictor of LVM [54, 55] and RWT [55]. Even among healthy young adults, BMI is associated with increases in LVM and changes in LV geometry (increased RWT) [30]. The relationship between BMI and LVM was stronger in African Americans than Whites [30]. In Blacks in South Africa, an interactive effect between blood pressure and obesity has been noted for LVM [56], whereby adiposity-induced increases in LVM reflect an enhanced effect of blood pressure on LV growth. As consequence of this interactive effect (which may be mediated by leptin), increased blood pressure (never treated hypertension) impacts on LVM in centrally obese but not lean people of African descent in South Africa [56]. In addition, in a population sample of Blacks in South Africa with a high prevalence of obesity, excess adiposity promoted concentric rather than eccentric LV geometric changes. These effects of obesity on LV geometric changes were independent of conventional, central artery and 24-hour blood pressures [57]. Indeed, the greater clustering of insulin resistance and obesity with high blood pressure in African Americans compared to Whites may play a role in ethnic differences [58]. In addition, in the MESA study acculturation due to the adoption of poor lifestyle behaviours (such as poor diet, smoking and drinking) may explain ethnic differences in the prevalence of LVH [59]. However, formal comparative studies are required to determine whether these factors account for the high prevalence of LVH and concentric remodelling in Blacks in Africa versus other ethnic groups.
Similarly, although genetic factors play a role in the development of LVM and LV geometric changes, whether genetic factors explain ethnic differences is unknown. In a large family-based study (181 nuclear families) of Blacks in South Africa, both LVM (independent of confounders including blood pressure) and LV geometric remodelling (independent of confounders including blood pressure and LVM) showed significant intrafamilial aggregation and heritability [60]. However, familial clustering of LVH and LV concentricity (independent of confounders including blood pressure) was also shown in a large family-based study of Whites [61]. Whether inheritance of these traits is stronger in Black Africans than Whites (and hence explains the higher prevalence of LVH and LV concentricity in Blacks than Whites) is not known.
4.5 Consequences of LVH and Geometric Changes
Bearing in mind the high prevalence of LVH, LV geometric changes and hypertension (one of the main determinants of LVH and LV geometric changes) in African communities, it is relevant to discuss the consequence of LVH and geometric changes. As LVH is associated with the development of decreased LV ejection fraction [62], heart failure [63] and mortality [11], it is speculated that the higher prevalence of LVH in African Americans would translate into a higher burden of systolic dysfunction and heart failure. However, to date there is no convincing data showing that LV dysfunction is more common in African Americans than it is in Whites. Indeed, in the CARDIA study, LV ejection fraction was comparable between African American and Whites [64]. Although, in multivariate analysis in the HyperGEN study, African Americans had a lower LV ejection fraction than in Whites, this did not translate into a higher prevalence of a decreased ejection fraction [65]. It is also unclear whether heart failure is more prevalent in African Americans than in Whites. Data from NHANES indicate that this is the case [66]; however, data from the National Health Interview Survey indicated a similar prevalence of heart failure in these two ethnic groups [67]. Importantly, in most studies, Black race was no longer a predictor of new heart failure after adjusting for potential risk factors [68, 69]. Nevertheless, in African American patients with hypertension, the risk of incident heart failure (4.7-year follow-up) was greater than in White patients with hypertension. Although this increased risk was independent of ECG LVH, in a cohort with echocardiographic LVH, increased LVM and RWT in African Americans compared to Whites were associated with decreases in systolic function (LV midwall shortening) [19].
As LV concentricity is more closely associated with heart failure with a preserved ejection fraction than heart failure with a reduced ejection fraction, it could be speculated that African populations are more prone to the development of heart failure with a reduced ejection fraction. Although there are currently limited data, one study failed to show a high proportion of African Americans among patients with heart failure with preserved ejection fraction [70]. However, in the Anglo-Scandinavian Cardiac Outcomes Trial, African-Caribbean hypertensive patients had greater diastolic dysfunction than Whites after adjusting for confounders including LVM [71]. There are currently no outcome data in Africans compared to other race groups; however, blood pressure [72], obesity [73], insulin resistance and concentric remodelling [74] are all independent determinants of diastolic dysfunction in a community study of Black South Africans. Whether increases in LVM and concentricity in Africans translate into an increased prevalence of heart failure independent of other cardiovascular risk factors remains unclear. Future studies are clearly required in order to address these issues in Black Africans.
5 Heart Failure in Africa and the Contribution of Hypertension
5.1 Epidemiology
Heart failure (HF), the end stage of all diseases of the heart, is one of the most important causes of morbidity and mortality both in the developed and the developing nations. It was estimated that there were 37.7 million cases of prevalent heart failure recorded globally in 2010, leading to 4.2 years lived with disability (YDLs). Heart failure was distributed across a number of causes. More than two-thirds (68.7%) of heart failure globally was attributable to four underlying causes: hypertensive heart disease, rheumatic heart disease, cardiomyopathies and ischaemic heart disease [75].
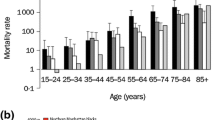
HF has been shown to have a significant impact on health-related quality of life [76] and appears to impose a huge economic burden to all nations [77]. It is associated with shorter life expectancy, greater morbidity and impaired quality of life than most common diseases. About 30% of people die within 3 months of HF diagnosis. Those with severe HF have an annual mortality of >50% [78, 79].
The sub-Saharan African survey on heart failure (THESUS-HF) [80] revealed that there are major differences in the epidemiology of acute heart failure (AHF) in sub-Saharan Africa, compared to North America, Europe and Asia. Table 7.3 compares the characteristic from patients with AHF from the USA, Europe, Asia and sub-Saharan Africa [81].
In sub-Saharan Africa, AHF affects relatively younger people (mean age 52 years). In Western countries, acute decompensated heart failure is a disease of the elderly with a mean age of 70–72 years [82, 83]. AHF therefore strikes the generation of breadwinners and caregivers in African patients, thereby having major economic implications. The younger African patients with AHF also have a lower frequency of ischaemic heart disease, diabetes mellitus, atrial fibrillation and renal insufficiency, compared to elderly heart failure sufferers in developed countries.
Compared to a summary of the causes of heart failure in sub-Saharan Africa, based on the case series published between 1957 and 2005 [84], THESUS-HF shows a changing trend in the epidemiology of acute heart failure in sub-Saharan Africa [80]. There was a rise in the contribution of hypertension as a cause of heart failure (from 23 to 45%), a reduction in the role of rheumatic heart disease (from 22 to 14%) and an apparent increase in recognition of ischaemic heart disease as a cause of heart failure (from 2% to nearly 8%). The high prevalence of hypertension and relatively low rate of coronary artery disease have also been observed in other single-centre studies, such as the Heart of Soweto study, where <10% of cases of heart failure were attributed to coronary artery disease [85].
Ojji and colleagues [86] compared 1515 consecutive HF patients with 4626 patients from the Heart of Soweto project [87]. They showed that hypertension contributed 60% of all cases presented with HF in Abuja versus 33% in Soweto. On an age- and sex-adjusted basis, compared with the Soweto cohort, the Abuja cohort were more likely to present with a primary diagnosis of hypertension (adjusted OR 2.10, 95% CI 1.85–2.42) or hypertension heart disease/hypertension heart failure (HHD/HHF) (OR 2.48, 95% CI 2.18–2.83); P < 0.001 for both. In the Heart of Soweto study, HHF (682/1196–57%, mean age 60 ± 14 years) was the most common manifestation of HHD among African women with diagnosis of hypertension [88].
In the Abeokuta HF registry, over 90% of the patients were known hypertensives. Most patients present in the fourth decade of life with severe heart failure and secondary functional valvular dysfunction and significant in-hospital mortality [89]. In a study of 52 Gambians and 55 Nigerians between ages 16 and 69 years with hypertensive heart failure, the mean duration of diagnosis of systemic hypertension among the previously known hypertensives was 4.3 years [90]. The overall 1-year survival rate was 71%, although it was unclear whether this was largely systolic or diastolic heart failure and whether the cases were primarily essential hypertension or included large numbers with secondary hypertension. The prognosis of hypertensive heart failure among this population is poor, with the first 3 months from onset of heart failure being critical for survival [90]. In a Nigerian study, acute left ventricular failure from hypertensive heart disease was the commonest cause of sudden cardiac death, while acute myocardial infarction was rare [91].
There are few reports on heart failure with preserved systolic function from SSA. This is commonly seen due to hypertensive heart disease either alone or in addition to systolic heart failure [92]. This needs to be addressed in future studies as it is likely that the profile of heart failure will also change in those regions due to shifts in population demographics, prevalence of specific risk factors, and influenced by the evolution and access to therapeutic options.
5.2 Pathophysiology
Hypertensive heart disease (HHD) is the cardiac damage related to chronic systemic arterial hypertension. It has been documented that some genes are implicated in the development of the cardiomyocyte hypertrophy in patients with hypertension which affect intracellular signalling, degradation of normal extracellular collagens and contractile dysfunction among other functions ultimately leading to left ventricular hypertrophy and HF [93]. There is also the possibility that these genes interact with environment as seen in Black Americans whereby weight gain, high salt intake and psychosocial factors may facilitate the rapid development of hypertension and hypertensive heart disease in susceptible individuals [94]. The presence of LVH adversely affects the prognosis of patients with arterial hypertension. In the Framingham Study, cardiovascular mortality among patients with arterial hypertension and increased left ventricular mass measured by echocardiography was double in comparison with patients with normal mass [11].
The role of biomarkers in diagnosing hypertensive HF is still being defined and does not yet impact treatment decisions [95]. However, it has recently been shown that the novel serum biomarker soluble ST2 differentiates hypertensive patients without LVH from those with LVH and those from hypertensive patients with heart failure [96]. The same author showed that in hypertensive patients with heart failure, there was a strong correlation between the levels of soluble ST2 and right ventricular diameters, right ventricle systolic pressure and right atrium area evaluated by echocardiography [96]. This suggests that serum soluble ST2 may have the potential of predicting who develops HF among hypertensive patients. It is therefore important to note that although markers for early detection remain a challenge, efforts should be made to explore combinations of genotypic, biochemical and physiological approaches to define and stratify the population at risk.
Conclusions
Hypertension is an increasing health problem in Africa. Although some research on left ventricular function on hypertensive patients have recently been developed, most of the data are still extrapolated from studies done in the USA with African Americans. Several studies, coming mainly from HHF in Africans, occur among individuals in their productive age group with attendant high economic loss and disability-adjusted life-years. The disease is often severe as a result of late presentation. Efforts should be made at the community level to ensure primordial prevention, early detection, treatment and control of hypertension on the continent. There is currently an unmet critical need in HHF research in Africa. It is essential that cohort studies of hypertensive patients are established to better understand this heterogeneous patient population, inform public policy decisions and guide basic, translational and clinical research. This kind of studies should capture comprehensive and longitudinal data including hospital course and post-discharge outcomes over long period of time. Future studies should also incorporate quality improvement initiatives focusing on continuity of care from initial presentation to the early post-discharge vulnerable period. In addition to traditional endpoints (i.e. hospitalization and mortality), patient-centred outcomes should be designed that comprehensively and longitudinally capture the burden of worsening HF (i.e. quality of life impairments and functional limitations).
References
Roth GA, et al. Global, regional, and National Burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1–25.
World Health Organization. Global status report on noncommunicable diseases, 2010. 2011. p. 176.
Fezeu L, et al. Association between socioeconomic status and adiposity in urban Cameroon. Int J Epidemiol. 2006;35(1):105–11.
Kadiri S, Salako BL. Cardiovascular risk factors in middle aged Nigerians. East Afr Med J. 1997;74(5):303–6.
Yusuf S, et al. Global burden of cardiovascular diseases: part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001;104(23):2855–64.
Gaziano TA. Cardiovascular disease in the developing world and its cost-effective management. Circulation. 2005;112(23):3547–53.
Donnison CP. Blood pressure in the African natives: its bearing upon aetiology of hyperpiesa and arteriosclerosis. Lancet. 1929;1:6–7.
Ogah OS, Rayner BL. Recent advances in hypertension in sub-Saharan Africa. Heart. 2013;99(19):1390–7.
Collaboration, N.C.D.R.F. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389(10064):37–55.
Mills KT, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–50.
Levy D, et al. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322(22):1561–6.
Krumholz HM, Larson M, Levy D. Prognosis of left ventricular geometric patterns in the Framingham Heart Study. J Am Coll Cardiol. 1995;25(4):879–84.
Koren MJ, et al. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991;114(5):345–52.
Drazner MH, et al. Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: the Dallas Heart Study. Hypertension. 2005;46(1):124–9.
Kizer JR, et al. Differences in left ventricular structure between black and white hypertensive adults: the Hypertension Genetic Epidemiology Network Study. Hypertension. 2004;43(6):1182–8.
Rodriguez CJ, et al. Left ventricular mass and ventricular remodeling among Hispanic subgroups compared with non-Hispanic blacks and whites: MESA (multi-ethnic study of atherosclerosis). J Am Coll Cardiol. 2010;55(3):234–42.
Liao Y, et al. The relative effects of left ventricular hypertrophy, coronary artery disease, and ventricular dysfunction on survival among black adults. JAMA. 1995;273(20):1592–7.
Havranek EP, et al. Left ventricular hypertrophy and cardiovascular mortality by race and ethnicity. Am J Med. 2008;121(10):870–5.
Okin PM, et al. Racial differences in incident heart failure during antihypertensive therapy. Circ Cardiovasc Qual Outcomes. 2011;4(2):157–64.
Mancia G, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34(28):2159–219.
Chirinos JA, et al. Left ventricular mass: allometric scaling, normative values, effect of obesity, and prognostic performance. Hypertension. 2010;56(1):91–8.
Woodiwiss AJ, Norton GR. Obesity and left ventricular hypertrophy: the hypertension connection. Curr Hypertens Rep. 2015;17(4):539.
Booysen HL, et al. Indexes of aortic pressure augmentation markedly underestimate the contribution of reflected waves toward variations in aortic pressure and left ventricular mass. Hypertension. 2015;65(3):540–6.
Sibiya MJ, et al. Gender-specific contribution of aortic augmentation index to variations in left ventricular mass index in a community sample of African ancestry. Hypertens Res. 2014;37(11):1021–7.
Wagner DR, Heyward VH. Measures of body composition in blacks and whites: a comparative review. Am J Clin Nutr. 2000;71(6):1392–402.
Echocardiographic Normal Ranges Meta-Analysis of the Left Heart Collaboration. Ethnic-specific normative reference values for echocardiographic LA and LV size, LV mass, and systolic function: the EchoNoRMAL study. JACC Cardiovasc Imaging. 2015;8(6):656–65.
Robinson C, et al. Novel approach to the detection of left ventricular hypertrophy using body mass index-corrected electrocardiographic voltage criteria in a Group of African Ancestry. Clin Cardiol. 2016;39(9):524–30.
Woodiwiss and Norton. Thresholds for echocardiographic LVH in healthy, non-hypertensive, non-diabetic, non-obese Black Africans (personal Communication).
Nunez E, et al. Optimal threshold value for left ventricular hypertrophy in blacks: the atherosclerosis risk in communities study. Hypertension. 2005;45(1):58–63.
Lorber R, et al. Influence of systolic blood pressure and body mass index on left ventricular structure in healthy African-American and white young adults: the CARDIA study. J Am Coll Cardiol. 2003;41(6):955–60.
Gardin JM, et al. Relationship of cardiovascular risk factors to echocardiographic left ventricular mass in healthy young black and white adult men and women. The CARDIA study. Coronary artery risk development in young adults. Circulation. 1995;92(3):380–7.
Abdalla M, et al. Hypertension and alterations in left ventricular structure and geometry in African Americans: the Jackson Heart Study. J Am Soc Hypertens. 2016;10(7):550–8.
Bello H, et al. Contributions of aortic pulse wave velocity and backward wave pressure to variations in left ventricular mass are independent of each other. J Am Soc Hypertens. 2017;11(5):265–274 e2.
Bacharova L, et al. Determinants of discrepancies in detection and comparison of the prognostic significance of left ventricular hypertrophy by electrocardiogram and cardiac magnetic resonance imaging. Am J Cardiol. 2015;115(4):515–22.
Crow RS, et al. Relation between electrocardiography and echocardiography for left ventricular mass in mild systemic hypertension (results from treatment of mild hypertension study). Am J Cardiol. 1995;75(17):1233–8.
Chapman JN, et al. Ethnic differences in the identification of left ventricular hypertrophy in the hypertensive patient. Am J Hypertens. 1999;12(5):437–42.
Lee DK, et al. Left ventricular hypertrophy in black and white hypertensives. Standard electrocardiographic criteria overestimate racial differences in prevalence. JAMA. 1992;267(24):3294–9.
Krovetz LJ. Racial differences of apparent electrocardiographic left ventricular hypertrophy. Am J Cardiol. 1994;74(4):418.
Walker AR, et al. Cardio-thoracic ratio in Negroes in Southern Africa. Postgrad Med J. 1972;48(564):584–9.
Maunganidze F, et al. Obesity markedly attenuates the validity and performance of all electrocardiographic criteria for left ventricular hypertrophy detection in a group of black African ancestry. J Hypertens. 2013;31(2):377–83.
Jaggy C, et al. Performance of classic electrocardiographic criteria for left ventricular hypertrophy in an African population. Hypertension. 2000;36(1):54–61.
Martin TC, Bhaskar YG, Umesh KV. Sensitivity and specificity of the electrocardiogram in predicting the presence of increased left ventricular mass index on the echocardiogram in Afro-Caribbean hypertensive patients. West Indian Med J. 2007;56(2):134–8.
Vanezis AP, Bhopal R. Validity of electrocardiographic classification of left ventricular hypertrophy across adult ethnic groups with echocardiography as a standard. J Electrocardiol. 2008;41(5):404–12.
Cuspidi C, et al. Left ventricular hypertrophy and cardiovascular risk stratification: impact and cost-effectiveness of echocardiography in recently diagnosed essential hypertensives. J Hypertens. 2006;24(8):1671–7.
Calderon A, et al. Detection of left ventricular hypertrophy by different electrocardiographic criteria in clinical practice. Findings from the Sara study. Clin Exp Hypertens. 2010;32(3):145–53.
Okin PM, et al. Combining ECG criteria for left ventricular hypertrophy improves risk prediction in patients with hypertension. J Am Heart Assoc. 2017;6(11):e007564.
Jingi AM, et al. Determinants and improvement of electrocardiographic diagnosis of left ventricular hypertrophy in a black African population. PLoS One. 2014;9(5):e96783.
Maunganidze F, et al. Left ventricular hypertrophy detection from simple clinical measures combined with electrocardiographic criteria in a group of African ancestry. Clin Res Cardiol. 2014;103(11):921–9.
Odili AN, et al. Office and home blood pressures as determinants of electrocardiographic left ventricular hypertrophy among black Nigerians compared with white Flemish. Am J Hypertens. 2017;30(11):1083–92.
Arnett DK, et al. Black-white differences in electrocardiographic left ventricular mass and its association with blood pressure (the ARIC study). Atherosclerosis risk in communities. Am J Cardiol. 1994;74(3):247–52.
Peer N, et al. Determinants of target organ damage in black hypertensive patients attending primary health care services in Cape Town: the Hi-Hi study. Am J Hypertens. 2008;21(8):896–902.
Adeoye AM, et al. Exploring overlaps between the genomic and environmental determinants of LVH and stroke: a multicenter study in West Africa. Glob Heart. 2017;12(2):107–113 e5.
Chirinos JA, et al. Ethnic differences in arterial wave reflections and normative equations for augmentation index. Hypertension. 2011;57(6):1108–16.
de Simone G, et al. Relation of obesity and gender to left ventricular hypertrophy in normotensive and hypertensive adults. Hypertension. 1994;23(5):600–6.
Lauer MS, et al. The impact of obesity on left ventricular mass and geometry. The Framingham Heart Study. JAMA. 1991;266(2):231–6.
Norton GR, et al. The relationship between blood pressure and left ventricular mass index depends on an excess adiposity. J Hypertens. 2009;27(9):1873–83.
Woodiwiss AJ, et al. Obesity promotes left ventricular concentric rather than eccentric geometric remodeling and hypertrophy independent of blood pressure. Am J Hypertens. 2008;21(10):1144–51.
Haffner SM, et al. LDL size in African Americans, Hispanics, and non-Hispanic whites : the insulin resistance atherosclerosis study. Arterioscler Thromb Vasc Biol. 1999;19(9):2234–40.
Effoe VS, et al. Acculturation is associated with left ventricular mass in a multiethnic sample: the multi-ethnic study of atherosclerosis. BMC Cardiovasc Disord. 2015;15:161.
Peterson VR, et al. Intrafamilial aggregation and heritability of left ventricular geometric remodeling is independent of cardiac mass in families of African ancestry. Am J Hypertens. 2015;28(5):657–63.
Niiranen TJ, et al. Familial clustering of hypertensive target organ damage in the community. In: J Hypertens, vol. 36; 2018. p. 1086.
Drazner MH, et al. Increased left ventricular mass is a risk factor for the development of a depressed left ventricular ejection fraction within five years: the Cardiovascular Health Study. J Am Coll Cardiol. 2004;43(12):2207–15.
Gottdiener JS, et al. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol. 2000;35(6):1628–37.
Wong ND, et al. Echocardiographic left ventricular systolic function and volumes in young adults: distribution and factors influencing variability. Am Heart J. 1995;129(3):571–7.
Devereux RB, et al. Left ventricular systolic dysfunction in a biracial sample of hypertensive adults: the Hypertension Genetic Epidemiology Network (HyperGEN) Study. Hypertension. 2001;38(3):417–23.
Thom T, et al. Heart disease and stroke statistics—2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113(6):e85–151.
Ni H. Prevalence of self-reported heart failure among US adults: results from the 1999 National Health Interview Survey. Am Heart J. 2003;146(1):121–8.
Bahrami H, et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med. 2008;168(19):2138–45.
He J, et al. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up study. Arch Intern Med. 2001;161(7):996–1002.
Yancy CW, et al. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the acute decompensated heart failure National Registry (ADHERE) database. J Am Coll Cardiol. 2006;47(1):76–84.
Sharp A, et al. Ethnicity and left ventricular diastolic function in hypertension an ASCOT (Anglo-Scandinavian cardiac outcomes trial) substudy. J Am Coll Cardiol. 2008;52(12):1015–21.
Libhaber CD, et al. Differential relationships of systolic and diastolic blood pressure with components of left ventricular diastolic dysfunction. J Hypertens. 2014;32(4):912–20.
Millen AM, et al. Relative impact of blood pressure as compared to an excess adiposity on left ventricular diastolic dysfunction in a community sample with a high prevalence of obesity. J Hypertens. 2014;32(12):2457–64. discussion 2464.
Peterson V, et al. Insulin resistance-associated decreases in left ventricular diastolic function are strongly modified by the extent of concentric remodeling in a community sample. Int J Cardiol. 2016;220:349–55.
Sliwa K, Stewart S. Heart failure in the developing world. In: Michael Felker G, Mann D, editors. Heart failure: a companion to Braunwald’s heart disease; 2016. p. 410–9.
Faller H, et al. Impact of depression on quality of life assessment in heart failure. Int J Cardiol. 2010;142(2):133–7.
Fagnani F, et al. Management, cost and mortality of a cohort of patients with advanced heart failure (the EPICAL study). Therapie. 2001;56(1):5–10.
Thomas S, Rich MW. Epidemiology, pathophysiology, and prognosis of heart failure in the elderly. Heart Fail Clin. 2007;3(4):381–7.
Aronow WS. Epidemiology, pathophysiology, prognosis, and treatment of systolic and diastolic heart failure. Cardiol Rev. 2006;14(3):108–24.
Damasceno A, et al. The causes, treatment, and outcome of acute heart failure in 1006 Africans from 9 countries. Arch Intern Med. 2012;172(18):1386–94.
Sliwa K. Is all heart failure the same around the globe? Eur Heart J. 2013;34(40):3091–2.
Adams KF Jr, et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE). Am Heart J. 2005;149(2):209–16.
Nieminen MS, et al. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27(22):2725–36.
Mayosi BM. Contemporary trends in the epidemiology and management of cardiomyopathy and pericarditis in sub-Saharan Africa. Heart. 2007;93(10):1176–83.
Stewart S, et al. Predominance of heart failure in the Heart of Soweto Study cohort: emerging challenges for urban African communities. Circulation. 2008;118(23):2360–7.
Ojji D, et al. A predominance of hypertensive heart failure in the Abuja Heart Study cohort of urban Nigerians: a prospective clinical registry of 1515 de novo cases. Eur J Heart Fail. 2013;15(8):835–42.
Sliwa K, et al. Spectrum of heart disease and risk factors in a black urban population in South Africa (the Heart of Soweto Study): a cohort study. Lancet. 2008;371(9616):915–22.
Stewart S, et al. Standing at the crossroads between new and historically prevalent heart disease: effects of migration and socio-economic factors in the Heart of Soweto cohort study. Eur Heart J. 2011;32(4):492–9.
Ogah OS, et al. Contemporary profile of acute heart failure in southern Nigeria: data from the Abeokuta Heart Failure Clinical Registry. JACC Heart Fail. 2014;2(3):250–9.
Isezuo AS, ABO O, Gaye A, Corrah T, Araoye MA. One year survival among sub-Saharan Africans with hypertensive heart failure. Cardiologie Tropicale. 2000;26(103):57–60.
Rotimi O, Ajayi AA, Odesanmi WO. Sudden unexpected death from cardiac causes in Nigerians: a review of 50 autopsied cases. Int J Cardiol. 1998;63(2):111–5.
Bloomfield GS, et al. Heart failure in sub-Saharan Africa. Curr Cardiol Rev. 2013;9(2):157–73.
Frohlich ED. State of the art lecture. Risk mechanisms in hypertensive heart disease. Hypertension. 1999;34(4 Pt 2):782–9.
Fuchs FD. Why do black Americans have higher prevalence of hypertension?: an enigma still unsolved. Hypertension. 2011;57(3):379–80.
Gluba A, et al. An update on biomarkers of heart failure in hypertensive patients. J Hypertens. 2012;30(9):1681–9.
Ojji DB, et al. Relationship between left ventricular geometry and soluble ST2 in a cohort of hypertensive patients. J Clin Hypertens (Greenwich). 2013;15(12):899–904.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this chapter
Cite this chapter
Damasceno, A., Woodiwiss, A., Sani, M. (2018). Hypertension and the Heart in Africa. In: Modesti, P., Cappuccio, F., Parati, G. (eds) Ethnic Diversities, Hypertension and Global Cardiovascular Risk. Updates in Hypertension and Cardiovascular Protection. Springer, Cham. https://doi.org/10.1007/978-3-319-93148-7_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-93148-7_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-93147-0
Online ISBN: 978-3-319-93148-7
eBook Packages: MedicineMedicine (R0)