Abstract
Background
Whether routine clinical parameters associated with left ventricular mass (LVM) enhance the performance of electrocardiographic (ECG) criteria for LV hypertrophy (LVH) detection and hence modify overall cardiovascular risk stratification is unknown.
Methods
An approach to echocardiographic LVH detection was identified from ECG criteria and clinical variables [age, body mass index (BMI), systolic blood pressure (SBP) and estimated glomerular filtration rate] associated with LVM in 621 participants of African ancestry. Performance (area under the receiver operating curve) and classification accuracy for LVH detection and the impact on cardiovascular risk stratification were determined.
Results
Compared to Cornell criteria alone, the combined use of Cornell criteria and clinical variables increased the performance (p < 0.001) and sensitivity (p < 0.05 to p < 0.0001) for LVH detection. The use of Cornell product together with additional clinical parameters as compared to Cornell product criteria alone increased the proportion of participants with pre-, grade I or grade II hypertension risk stratified as having a high added cardiovascular risk (56.3–67.9 %, p < 0.05).
Conclusions
In individuals of African ancestry, a combination of Cornell product criteria and age, BMI and SBP improves classification accuracy of Cornell criteria for LVH and increases those identified as having a high added as compared to lower cardiovascular risk scores.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
As left ventricular hypertrophy (LVH) independently predicts outcomes, and electrocardiography (ECG) is the most cost-effective approach to LVH detection [1], ECG identification of LVH for routine risk prediction is recommended by all hypertension guidelines, including the European Society of Hypertension/European Society of Cardiology guidelines [12]. Furthermore, ECG-detected LVH is an independent predictor of cardiac prognosis in chronic heart failure [18]. However, ECG criteria are insensitive to LVH detection [19, 22] and hence a considerable number of patients with LVH are likely to be missed with ECG screening. In this regard, the sensitivity of some ECG criteria may be particularly low for LVH detection in groups of black African ancestry [8, 13, 15], as ECG criteria for LVH have been shown to be less well correlated with LV mass index (LVMI) in African-Americans as compared to Caucasians [4]. These poor correlations may be attributed to increased ECG amplitudes in groups of African descent [3, 10], possibly produced by alterations in skin conductivity [9] or a diminished thoracic diameter reducing the distance from the skin surface to the heart [2, 7, 23]. As universal screening for LVH using transthoracic echocardiography carries a high cost [5], solutions to reducing these costs are required.
As recently suggested, one possible approach to improve the overall performance for LVH detection using ECG criteria is to employ biomarkers of LVH to complement ECG criteria for LVH detection [14]. In this regard, this approach improves overall diagnostic performance in association with an enhanced sensitivity for LVH detection [14]. However, the cost of performing routine measures of biomarkers in all hypertensives is likely to be cost-prohibitive at a primary care level in many countries. The principle of evaluating approaches designed to enhance the sensitivity and overall diagnostic performance of ECG criteria for LVH detection nevertheless offers promise. As a number of readily obtained routine clinical parameters are also closely associated with LV mass index (LVMI), in the present study conducted in a community sample of African ancestry, where we have previously demonstrated a poor performance of ECG criteria [15], we evaluated whether readily obtained routine clinical parameters closely associated with LVMI may be employed to enhance the sensitivity and performance of ECG criteria for LVH detection. We subsequently assessed whether the use of LVH detection determined from ECG criteria together with simple clinical parameters associated with LVH significantly alters the overall level of cardiovascular risk stratification.
Methods
Study group
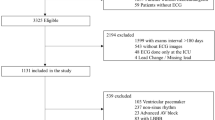
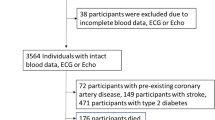
The present study was conducted according to the principles outlined in the Helsinki declaration. The Committee for Research on Human Subjects of the University of the Witwatersrand approved the protocol (approval numbers: M02-04-72 renewed as M07-04-69 and M12-04-108). Participants gave informed, written consent. The study design has previously been described [15, 16, 20, 24]. Briefly, nuclear families of black African descent with siblings older than 16 years were randomly recruited from the South West Township of Johannesburg, South Africa. Of the 1,191 participants recruited, in a substudy consisting of 908 participants of whom 829 (91 %) consented to an echocardiographic procedure [69.6 % males with a body mass index (BMI) = 23.7 ± 3.9 kg/m2, did not consent], high-quality echocardiograms could be obtained in 678 participants and 621 had ECG and eGFR data required for the present analysis. Of the 151 participants with poor-quality echocardiograms, 92.4 % were female (BMI 37.5 ± 7.7 kg/m2).
Clinical, demographic, and anthropometric measurements
Demographic and clinical data were obtained using a standardised questionnaire. Height and weight were measured using standard approaches and participants were identified as being overweight if their BMI was ≥25 kg/m2 and obese if their BMI was ≥30 kg/m2. Blood tests of renal function, liver function, blood glucose, lipid profiles, haematological parameters, and percentage glycated haemoglobin (HbA1c) (Roche Diagnostics, Mannheim, Germany) were performed. Diabetes mellitus (DM) or abnormal blood glucose control was defined as the use of insulin or oral hypoglycaemic agents or an HbA1c value greater than 6.5 %. Conventional BP measurements were obtained by a trained nurse-technician using a standard mercury sphygmomanometer as previously described [24].
Electrocardiography
A standard 12-lead ECG was recorded at 25 mm/s and 1.0 mV/cm [15]. R and S wave amplitudes in all leads were measured to the nearest 0.05 mV (0.5 mm). QRS duration was measured to the nearest 4 ms. Cornell, Sokolow–Lyon, Gubner–Ungerleider and Lewis voltage or time–voltage criteria for LVH were calculated using standard formulae which incorporate a gender-specific constant where required [15]. As groups of black African descent show differences in R and S wave amplitudes as compared to other ethnic groups [3, 10], thresholds of ECG criteria for LVH were determined from the upper 95 % confidence intervals derived in 140 participants from the community-based study without clinically significant disease and normal clinical blood parameters who were normotensive, non-diabetic, and had a BMI <30 kg/m2 [15].
Echocardiography
Left ventricular end diastolic internal diameter and septal (anterior wall) and posterior wall thickness were determined from transthoracic two-dimensional targeted M-mode echocardiographic images obtained in the parasternal long-axis as previously described [16, 24]. Variables were analysed according to the American Society of Echocardiography convention [21]. All measurements were recorded and analysed off-line by experienced investigators (CDL and AJW) who were unaware of the clinical data of the participants and whom had a low degree of inter- and intra-observer variability [16, 24]. Only M-mode images of acceptable quality were analysed. In this regard, acceptable quality was considered to exist when appropriate visualisation of both the right and the left septal surfaces occurred and where the endocardial surface of the septal and posterior wall were clearly visible when imaging at the optimal angle of incidence (perpendicular to the posterior wall) and close to the mitral leaflets.
Left ventricular mass (LVM) was determined using a standard formula [6] and indexed (LVMI) to height2.7. Thresholds for LVMI were determined from the upper 95 % confidence intervals derived in 140 participants from the community sample without clinically significant disease and normal clinical blood parameters who were normotensive, non-diabetic, and had a BMI <30 kg/m2. In these participants the upper 95 % confidence interval for LVM indexed to height2.7 (LVMI) was 51.8 g/m2.7 and hence a value of 51 g/m2.7 as previously recommended [17] was employed.
Left ventricular end diastolic and systolic volumes were determined using the Teichholz method. Left ventricular ejection fraction (EF) was calculated as [(LV end diastolic volume-LV end systolic volume)/LV end diastolic volume] × 100. Pulse wave Doppler recordings of transmitral velocity were obtained with the sample volume at the tip of the mitral valve in the apical 4-chamber view. Transmitral velocity measurements were obtained during the early (E) and late (atrial-A) period of left ventricular diastolic inflow and expressed as the E/A ratio.
Renal function
Estimated glomerular filtration rate (eGFR) was determined using the abbreviated Modification of Diet in Renal Disease (MDRD) study group equation: 186.3 × (serum creatinine in mg/decilitre−1.154) × (age in years−0.203) × 1.212 × 0.742 (if female) [11].
Assessment of impact of modified LVH evaluation on overall cardiovascular risk
To assess whether LVH as detected using ECG criteria together with routine clinical parameters modifies overall cardiovascular risk, we used the European Society of Hypertension (ESH)/European Society of Cardiology (ESC) guidelines approach to risk assessment [12]. In our assessment of cardiovascular risk we nevertheless excluded costly end-organ damage assessments, including the use of carotid intima-media thickness, aortic pulse wave velocity, or urinary micro-albuminuria. We evaluated the change in proportion of individuals with pre-, grade I or grade II hypertension and a high added rather than average, low or moderate added risk score when using a modified ECG approach to LVH detection (ECG + additional clinical parameters) as compared to when using standard ECG criteria. Normotensives and grade III hypertensives were not included in this assessment as the former could only change to a moderate added risk (which would not qualify for drug treatment) and the latter are already classified as a high added risk (and hence require immediate drug therapy). As ESH/ESC guidelines only advocate the use of Sokolow–Lyon and Cornell time–voltage product criteria for LVH detection [12], and in the present population sample Cornell, but not Sokolow–Lyon criteria showed significant performance for LVH detection, we only assessed the impact of modified Cornell time–voltage product criteria on overall cardiovascular risk.
Data analysis
Database management and statistical analyses were performed with SAS software, version 9.1 (SAS Institute Inc., Cary, NC, USA). Continuous data are reported as mean ± SD or mean ± SEM. Unadjusted means and proportions were compared by the large-sample z test and the χ 2-statistic, respectively. To identify the factors that may complement ECG criteria for LVH detection, all previously described factors normally obtained when risk assessing that have been independently associated with LVMI were included in multivariate models with individual ECG criteria. Those factors providing relationships with LVMI independent of ECG criteria were subsequently evaluated to determine whether the combined effects improved the area under the receiver operating curve (AUC) (which do not depend on thresholds) for LVH detection. To determine sensitivity and specificity, one of a range of values were assigned as determined by a combination of ECG criteria and the factors associated with LVMI independent of ECG criteria. In this regard, values of 1–4 were assigned with a value of 1 given to each of the following: ECG criterion ≥ threshold, age ≥ median (43.6 years), BMI ≥ median (28.3 kg/m2), SBP ≥140 mmHg (or presence of antihypertensive therapy) or eGFR < upper quartile (<97 ml/min/1.73 m2). Either the median of the sample or threshold for upper quartile of the sample was selected depending on the effect on the sensitivity for LVH detection.
Results
Participant characteristics
The demographic and clinical characteristics of the study sample are given in Table 1. A comparison of the characteristics of the participants from the community sample with and without echocardiographic, ECG or eGFR data is given in Supplemental Table S1. No differences were noted in the characteristics. In the study sample, 42 % of participants were obese, and of the 43 % of participants that were hypertensive, only 36 % had controlled BP. In the study sample, 21.7 % of participants had LVH.
Factors associated with LVMI in the same multivariate model as ECG criteria
In the community sample, age, BMI, SBP (but not diastolic BP) and eGFR were consistently associated with LVMI independent of ECG criteria (Table 2). Whilst RaVL, Cornell, Gubner–Ungerleider, and Lewis voltage or time–voltage criteria were associated with LVMI independent of standard demographic and clinical factors, Sokolow–Lyon criteria were not independently associated with LVMI (voltage: partial r = −0.02, p = 0.60, time–voltage product: partial r = −0.001, p = 0.98).
Effect of individual test performances for LVH detection in the community sample
With the exception of Sokolow–Lyon criteria (AUC = 0.51 ± 0.03, p = 0.54), all other ECG criteria for LVH detection showed significant performance (AUC) (Table 3), but a low sensitivity at 85 % specificity (Table 4) for LVH detection. Age (AUC = 0.74 ± 0.02, p < 0.0001), BMI (AUC = 0.71 ± 0.02, p < 0.0001), SBP (AUC = 0.71 ± 0.02, p < 0.0001) and eGFR (AUC = 0.67 ± 0.03, p < 0.0001) all showed significant performance for LVH detection. Using values above the median of the sample for age (≥43.6 years) and BMI (≥28.3 kg/m2), values of SBP ≥140 mmHg (or the use of antihypertensive therapy) and eGFR values less than the highest quartile (<97 ml/min/1.73 m2), age, BMI, SBP and eGFR showed a low specificity (age 59.7 %, BMI 56.0 %, SBP 70.6 %, eGFR 71.4 %) and a high or intermediate sensitivity (age 80.0 %, BMI 73.3 %, SBP 63.0 %, eGFR 50.4 %) for LVH detection.
Effect of combined test performance versus ECG criteria alone for LVH detection
Compared with ECG criteria alone, the combination of individual ECG criteria, age, SBP or BMI showed an improved level of performance (AUC) for all ECG criteria for LVH detection (Table 3). Compared with ECG criteria alone, the combination of Cornell criteria and eGFR also showed an improved level of performance (AUC) for LVH detection (Table 3). However, as compared to ECG criteria alone, the most marked increases in performance were noted when age, BMI, SBP and ECG criteria or age, BMI, eGFR and ECG criteria were combined (Table 3 and Fig. 1). The use of SBP and eGFR used in combination together with age, BMI and ECG criteria did not further enhance the performance (Table 3).
Performance of select electrocardiographic (ECG) criteria for echocardiographic left ventricular hypertrophy detection (left ventricular mass index >51 g/m2.7) before and after the inclusion of age, body mass index and either systolic blood pressure (SBP) or estimated glomerular filtration rate (eGFR) in a model with ECG criteria in a community sample of African ancestry (n = 621). A comparison of the area under the curves is made in Table 3
Compared with Cornell criteria alone, an “LVH value” = 3 based on Cornell criteria + additional clinical parameters showed an increased sensitivity for LVH detection at 85 % specificity (Table 4). An “LVH value” <3 failed to significantly modify the sensitivity for LVH detection of any of the ECG criteria (data not shown). An “LVH value” of 4 provided a low level of sensitivity for LVH detection (data not shown). The improved sensitivity for LVH detection with Cornell criteria together with the alternative clinical measures as compared to Cornell criteria alone translated into a 2–3 times greater decrease (difference) in the probability (chances) of a false-negative finding as compared to the increase (difference) in chances of a false-positive finding for LVH (Table 5).
When assessing the value of using an SBP ≥140 mmHg irrespective of the presence of antihypertensive therapy, incorporated in the “LVH value”, the AUC for LVH detection was similar as compared to when an SBP ≥140 mmHg or the presence of antihypertensive therapy was included (e.g. Cornell time–voltage product: AUC = 0.78 ± 0.02 vs 0.78 ± 0.02). However, the use of an SBP ≥140 mm Hg irrespective of the presence of antihypertensive therapy tended to reduce the sensitivity for LVH detection of the “LVH value” at 85 % specificity as compared to when an SBP ≥140 mmHg or the presence of antihypertensive therapy was included (e.g., Cornell time–voltage product: Sensitivity at 85 % specificity = 48.7 vs 52.7 %).
Effect of combined test performance versus ECG criteria alone on overall cardiovascular risk assessment
The proportion of pre-, grade I and grade II hypertensives with a high added risk increased from 56.3 % (n = 179 of 318) to 67.9 % (216 of 318) (p < 0.05) when LVH was diagnosed using an “LVH value” of 3 derived from the combination of Cornell time–voltage product, age, BMI and SBP, as compared to when using the Cornell time–voltage product alone. The proportion of pre-, grade I and grade II hypertensives with a high added risk increased from 56.3 % (n = 179 of 318) to 60.4 % (192 of 318) (p = 0.08) when LVH was diagnosed using an “LVH value” of 3 derived from the combination of Cornell time–voltage product, age, BMI and eGFR, as compared to when using the Cornell time–voltage product alone.
Relationships between LV function and either ECG criteria alone or ECG combined with other criteria for LV detection
No relationships between ECG criteria alone and EF or ECG combined with other criteria for LVH detection and EF were noted (data not shown). However, ECG criteria for LVH detection were correlated with E/A (r = −0.11 to −0.31, p = 0.007 to <0.0001) and these relationships were strengthened by the use of ECG combined with other criteria for LVH detection (r = −0.45 to −0.51, p < 0.0001, p < 0.0005 for comparison of r values using Z-statistics). However, with adjustments for factors independently associated with E/A (age, sex, BMI, diastolic BP, and heart rate), the use of ECG combined with other criteria for LVH detection did not show stronger relations with E/A than relations noted between ECG criteria alone and E/A (data not shown).
Discussion
The main findings of the present study are as follows: In a community sample of African ancestry with a high prevalence of obesity, we evaluated whether incorporating Cornell criteria for LVH detection together with an age ≥43.6 years (median), a BMI ≥28.3 kg/m2 (median), and an SBP ≥140 mmHg (median) (or antihypertensive therapy) on the ability to detect echocardiographic LVH and subsequently risk predict. As compared to Cornell criteria alone, the use of age, BMI and SBP (or antihypertensive therapy) to complement Cornell criteria increased the overall performance (AUC) and sensitivity for echocardiographic LVH detection. Moreover, using a combination of Cornell product, age, BMI and SBP resulted in a greater proportion of pre-, grade I and grade II hypertensives correctly stratified as having a high added, rather than average, low or moderate added overall cardiovascular risk as compared to when using the Cornell product alone for LVH detection and risk evaluation.
A recent study [14] has similarly evaluated an approach to enhance the ability of ECG criteria to identify LVH, but in this study thresholds for LVM indexed to body surface area were considered. In this regard, biomarkers of LVH, including circulating brain-natriuretic peptide and troponin T concentrations, were assessed, an approach which in contrast to our study, where only readily available clinical measures were evaluated, would incur costs beyond normal risk assessment [14]. Moreover, in that study [14], the effect on the ability of Sokolow–Lyon voltages [the criterion with the highest overall performance (AUC)] for LVH detection was determined. Biomarkers were noted to increase the sensitivity (26–44 %), decrease the specificity (96–90 %) and improve the overall performance (AUC increased from 0.760 to 0.798) of Sokolow–Lyon criteria for LVH detection [14]. As the community sample studied by us has a high prevalence of obesity-associated LVH, we evaluated the performance of ECG criteria for the detection of an increased LVM indexed to height2.7. As previously described [15] using this approach we noted negligible performance of Sokolow–Lyon criteria. We therefore evaluated whether we could enhance the ability of alternative ECG criteria to detect LVH. In this regard, using simple clinical measures to complement Cornell criteria, the combined approach increased the AUC for LVH detection of the Cornell time–voltage product criteria from 0.65 to 0.78 and the sensitivity for LVH detection from 34.9 to 52.7 % at 85 % specificity. Importantly, the present data show that the use of a combined approach to LVH detection will considerably improve the false-negative rate from values as high as 89.6 to 51.1 % (Cornell time–voltage product) in the population studied, whilst maintaining a false-positive rate of only 16.7 %. Thus, whilst a markedly greater proportion of individuals with LVH whom would have otherwise been missed would be referred for echocardiography or other imaging modalities for LVH detection, few additional individuals without LVH would be referred.
The clinical implications of the present study warrant consideration. To reduce the high costs of universal screening for LVH using transthoracic echocardiography, one possibility is that those with ECG evidence of LVH are referred for echocardiographic or other assessments. However, the low sensitivity for LVH detection using ECG criteria alone would exclude a significant number of those with echocardiographic LVH from referral for further imaging. Nevertheless, in the present study using Cornell criteria plus additional clinical parameters for LVH detection, significantly more individuals with LVH would have been referred for echocardiographic LVH detection. The consequence in the present community is that an additional 37 of 318 participants (12 %) with pre-, grade I or grade II hypertension were risk stratified using a combined Cornell criteria plus additional clinical parameters for LVH detection as being at high added rather than average, low added or moderate added risk for a cardiovascular event. Confirmation of LVH in these individuals with echocardiography or other imaging modalities would, according to the ESH/ESC guidelines [12], require drug therapy in addition to lifestyle modification, rather than lifestyle modification and observation alone. Hence, combining Cornell criteria and additional clinical parameters for LVH detection enhances the sensitivity to detect LVH, and subsequently identifies significantly more individuals with LVH and a higher overall cardiovascular risk requiring markedly different management approaches.
There are several limitations to the present study which should be underscored. First, the present study was conducted in a community sample of black African descent in Africa. In this regard, the sensitivity of some ECG criteria may be particularly low for LVH detection in groups of black African ancestry [8, 13, 15]. Whether similar results apply to other communities requires further evaluation. Second, more women than men volunteered for the present study and we were not statistically powered to examine the use of a combination of Cornell criteria, age, BMI, and SBP on the performance and sensitivity for LVH detection in sex-specific groups. Hence, the present results may apply to women only. Third, we employed echocardiography to detect LVH which is limited by the use of imaging in a single rather than multiple LV planes, and is hindered by the extent of the acoustic window and possible poor image quality. Further studies are therefore required to confirm the present approach to LVH detection using magnetic resonance imaging.
In conclusion, in the present study we show that in a community of African ancestry the use of a combination of Cornell voltage or time–voltage product, age, BMI and SBP, markedly improved the overall performance and sensitivity for LVH detection as compared to Cornell criteria alone. This approach, by reducing the proportion with false-negative Cornell-LVH, increased the proportion who, once LVH is confirmed, would be correctly stratified as having a high added rather than average, low or moderate added cardiovascular risk.
References
Agabiti-Rosei E, Muiesan ML, Salvetti M (2007) New approaches to the assessment of left ventricular hypertrophy. Therap Adv Cardio Dis 1:119–128. doi:10.1177/1753944707086350
Ashcroft MT (1972) Cardiac enlargement in Jamaicans. BMJ 2:655. doi:10.1136/bmj.2.5814.655-b
Chapman JN, Mayet J, Chang CL, Foale RA, Thom SA, Poulter NR (1999) Ethnic differences in the identification of left ventricular hypertrophy in the hypertensive patient. Am J Hypertens 12:437–442. doi:10.1016/S0895-7061(99)00027-8
Crow RS, Pineas RJ, Rautaharju P, Hannan P, Liebson PR (1995) Relations between electrocardiography and echocardiography for left ventricular mass in mild systemic hypertension (results from Treatment of Mild Hypertension Study). Am J Cardiol 75:1233–1238. doi:10.1016/S0002-9149(99)80769-3
Cuspidi C, Meani S, Valerio C, Fusi V, Sala C, Zanchetti A (2006) Left ventricular hypertrophy and cardiovascular risk stratification: impact and cost-effectiveness of echocardiography in recently diagnosed essential hypertensives. J Hypertens 24:1671–1677. doi:10.1097/01.hjh.0000239305.01496.ca
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N (1986) Echocardiograph assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458. doi:10.1016/0002-9149(86)90771-X
Horton JD, Sherber HS, Lakatta EG (1977) Distance correction for precordial electrocardiographic voltage in estimating left ventricular mass: an echocardiographic study. Circulation 55:509–512. doi:10.1161/01.CIR.55.3.509
Jaggy C, Perret F, Bovet P, van Melle G, Zerkiebel N, Madeleine G, Kappenberger L, Paccaud F (2000) Performance of classic electrocardiographic criteria for left ventricular hypertrophy in an African population. Hypertension 36:54–61. doi:10.1161/01.HYP.36.1.54
Krovetz LJ (1994) Racial differences of apparent electrocardiographic left ventricular hypertrophy in the hypertensive patient. Am J Cardiol 74:418. doi:10.1016/0002-9149(94)90423-5
Lee DK, Marantz PR, Devereux RB, Kligfield P, Alderman MH (1992) Left ventricular hypertrophy in black and white hypertensives: standard elctrocardiographic criteria overestimate racial differences in prevalence. JAMA 267:3294–3299. doi:10.1001/jama.267.24.3294
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation: Modification of Diet in Renal Disease Study Group. Ann Intern Med 130:461–470. doi:10.7326/0003-4819-130-6-199903160-00002
Mancia G, De Backer G, Dominiczak A et al (2007) 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 28:1462–1536. doi:10.1093/eurheartj/ehm236
Martin TC, Bhaskar YG, Umesh KV (2007) Sensitivity and specificity of the electrocardiogram in predicting the presence of increased left ventricular mass index on the echocardiogram in Afro-Caribbean hypertensive patients. West Indian Med J 56:134–138. doi:10.1590/S0043-31442007000200006
Martinez-Rumayor AA, de Lemos JA, Rohatgi AK, Ayers CR, Powell-Wiley TM, Lakoski SG, Berry JD, Khera A, Das SR (2013) Addition of highly sensitive troponin T and N-terminal pro-B-type natriuretic peptide to electrocardiography for detection of left ventricular hypertrophy. Results from the Dallas Heart Study. Hypertension 61:105–111. doi:10.1161/HYPERTENSIONAHA.112.195289
Maunganidze F, Norton GR, Maseko MJ, Libhaber CD, Majane OHI, Woodiwiss AJ (2013) Obesity markedly attenuates the validity and performance of all electrocardiographic criteria for left ventricular hypertrophy detection in a group of African ancestry. J Hypertens 31:377–383. doi:10.1097/HJH.0b013e32835b8daa
Norton GR, Majane OH, Maseko MJ, Libhaber C, Redelinghuys M, Kruger D, Veller M, Sareli P, Woodiwiss AJ (2012) Brachial blood pressure-independent relations between radial late systolic shoulder-derived aortic pressures and target organ changes. Hypertension 59:885–892. doi:10.1161/HYPERTENSIONAHA.111.187062
Nunez E, Arnett DK, Benjamin EJ, Liebson PR, Skelton TN, Taylor H, Andrew M (2005) Optimal threshold value for left ventricular hypertrophy in blacks in the Atherosclerosis Risk in Communities study. Hypertension 45:58–63. doi:10.1161/01.HYP.0000149951.70491.4c
Otaki Y, Takahashi H, Watanabe T, Kadowaki S, Narumi T, Honda Y, Hasegawa H, Honda S, Funayama A, Nishiyama S, Arimoto T, Shishido T, Miyashita T, Miyamoto T, Kubota I (2014) Electrocardiographic left ventricular hypertrophy Cornell product is a feasible predictor of cardiac prognosis in patients with chronic heart failure. Clin Res Cardiol 103:275–284. doi:10.1007/s00392-013-0646-2
Pewsner D, Juni P, Egger M, Battaglia M, Sundström J, Bachmann LM (2007) Accuracy of electrocardiography in diagnosis of left ventricular hypertrophy in arterial hypertension: a systematic review. BMJ 335:711–717. doi:10.1136/bmj.39276.636354.AE
Redelinghuys M, Norton GR, Scott L, Maseko MJ, Brooksbank R, Majane OHI, Sareli P, Woodiwiss AJ (2010) Relationship between urinary salt excretion and pulse pressure and central aortic hemodynamics independent of steady state pressure in the general population. Hypertension 56:584–590. doi:10.1161/HYPERTENSIONAHA.110.156323
Sahn DJ, De Maria A, Kisslo J, Weyman A (1978) Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurement. Circulation 58:1072–1083. doi:10.1161/01.CIR.58.6.1072
Schillaci G, Battista F, Pucci G (2012) A review of the role of electrocardiography in the diagnosis of left ventricular hypertrophy in hypertension. J Electrocardiol 45:617–623. doi:10.1016/j.jelectrocard.2012.08.051
Walker ARP, Richardson BD, Wadvalla M, Walker BF (1972) Cardio-thoracic ratio in Negroes in Southern Africa. Postgrad Med J 48:584–589. doi:10.1136/pgmj.48.564.584
Woodiwiss AJ, Molebatsi N, Maseko MJ, Libhaber E, Libhaber C, Majane OH, Paiker J, Dessein P, Brooksbank R, Sareli P, Norton GR (2009) Nurse-recorded auscultatory blood pressure at a single visit predicts target organ changes as well as ambulatory blood pressure. J Hypertens 27:287–297. doi:10.1097/HJH.0b013e328317a78f
Acknowledgments
This study would not have been possible without the voluntary collaboration of the participants and the excellent technical assistance of Mthuthuzeli Kiviet, Nomonde Molebatsi, and Nkele Maseko. This study was supported by the Medical Research Council of South Africa, the University Research Council of the University of the Witwatersrand, the National Research Foundation (Women in Research and the Thuthuka Program), the Circulatory Disorders Research Trust, and the Carnegie Programme.
Conflict of interest
None of the authors have any conflicts of interests to declare.
Author information
Authors and Affiliations
Corresponding authors
Additional information
F. Maunganidze, A.J. Woodiwiss and G.R. Norton contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Maunganidze, F., Woodiwiss, A.J., Libhaber, C.D. et al. Left ventricular hypertrophy detection from simple clinical measures combined with electrocardiographic criteria in a group of African ancestry. Clin Res Cardiol 103, 921–929 (2014). https://doi.org/10.1007/s00392-014-0730-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-014-0730-2