Abstract
Antioxidants play a vital role in reproductive health and fertility. The local cellular environment influences oocyte development, ovulation, successful fertilization, and maintenance of early pregnancy. An offset of reactive oxygen species (ROS)-induced cellular oxidative stress can adversely affect function of reproductive organs and fertility. ROS and antioxidants have emerged as ubiquitous participants in normal human reproductive processes. Imbalance in the oxidant/antioxidant relationship has been implicated in numerous reproductive disorders and complications, including endometriosis, polycystic ovarian syndrome, oocyte aging, dysmenorrhea and premenstrual syndrome, spontaneous abortion, and infertility. Studies have examined dietary antioxidant supplementation in hopes to prevent and treat reproductive pathologies. Dietary antioxidants, including isoflavones, antioxidant vitamins, and trace elements, which are cofactors of key antioxidant enzymes, have been targeted as nutritional antioxidants for prevention and/or treatment of unexplained infertility and recurrent spontaneous abortions. However, there is a vast knowledge deficit to fill, and targeted studies are needed to elucidate the role of ROS in normal reproductive physiology and fertility, as well as in treatment of reproductive pathologies. This chapter reviews the role played by antioxidants in female reproductive health and fertility and antioxidant interventions for the prevention and treatment of reproductive pathology in association with oxidative stress.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Oxidative stress
- Reproductive disorders and complications
- Antioxidants
- Female reproductive health
- Fertility
5.1 Introduction
Intracellular homeostasis is maintained at least in part by a fine balance between oxidants and antioxidants. Oxidative stress is a state associated with increased damage to cellular structure and function induced by oxygen-derived oxidants commonly known as reactive oxygen species (ROS), which are by-products of aerobic respiration and metabolism. ROS production is tightly controlled by interrelated antioxidant systems that modulate intracellular ROS concentration and set the redox status of the cell. The common ROS that have potential implications in mammalian reproduction and developmental biology are superoxide radicals (•O2 −), hydrogen peroxide (H2O2), hydroxyl radicals (•OH), nitric oxide (NO•), and peroxynitrite anion (ONOO−). ROS and antioxidants have emerged as ubiquitous participants in normal human reproductive processes, and an imbalance in the oxidant/antioxidant relationship has been implicated in numerous reproductive pathologies, including endometriosis, polycystic ovarian syndrome and infertility (Agarwal et al. 2005; Fujii et al. 2005), and prenatal development disorders and complications (Al-Gubory et al. 2010).
Maternal undernutrition or poor nutrition can have long-lasting effects on reproductive potential. Infertility due to ovulation disorders may be preventable by healthy diet and lifestyle behaviors (Chavarro et al. 2007). Substantial evidence suggests that low antioxidant status and oxidative stress may be associated with infertility of both known and idiopathic origin (Ruder et al. 2008). Rats subjected to caloric undernutrition (50% of a standard control diet) during pregnancy and lactation exhibited reduced primary and secondary follicle counts in their offspring (Bernal et al. 2010). These offspring were found to have increased ovarian protein carbonyl groups (biomarkers of oxidative stress), implying decreased antioxidant defenses and increased oxidative damage. It is speculated that oxidative stress accelerates reproductive maturity along with faster decline in ovarian reserve (Bernal et al. 2010). Deficiency in vitamin C, a well-known antioxidant, has been associated with increases in premature births and predisposing newborns to oxidative stress (Negi et al. 2012).
There is a wide array of plant antioxidants, which have a variety of functions but have in common the ability to neutralize ROS in order to maintain homeostasis and protect cells from undue oxidative damage. There is growing interest in the effects of increased consumption of dietary phytoestrogens on the spectra of reproductive processes, including the timing of menarche and menopause. Natural antioxidants have been targeted as nutritional therapies for recurrent spontaneous abortions and unexplained infertility (Sekhon et al. 2010), and some preliminary studies examining antioxidant supplementation in the periconception period have been encouraging (Cetin et al. 2010; Mistry and Williams 2011; Twigt et al. 2012; Al-Gubory 2013). However, there is a vast knowledge deficit to fill, and targeted studies are needed to elucidate the role of ROS in normal reproductive physiology and fertility, as well as in reproductive pathologies. In this chapter, we review the major dietary antioxidants implicated in female reproductive health and fertility. This chapter also reviews the role played by antioxidants in female reproductive health and fertility and antioxidant interventions for the prevention and treatment of reproductive pathologies in association with oxidative stress.
5.2 Dietary Antioxidants
Dietary antioxidants, including isoflavones, tocopherol (vitamin E), provitamin A carotenoids, and ascorbate (vitamin C), as well as dietary antioxidant cofactors, mainly copper, zinc, manganese, and selenium, have been targeted as nutritional antioxidants for prevention of recurrent spontaneous abortion and treatment of unexplained infertility, and some preliminary studies examining antioxidant supplementation during the periconception period have been encouraging (Ramakrishnan et al. 2012; Gernand et al. 2016).
5.2.1 Isoflavones
Phytoestrogens are nonsteroidal compounds that mimic the conformation of estradiol and are able to bind to estrogen receptors and interact with estrogen signaling pathways. They have a higher affinity for estrogen receptor-beta than for estrogen receptor-alpha (Cederroth et al. 2012). Soy products are the predominant source of dietary phytoestrogens in humans, the most studied subclass being the isoflavones (i.e., genistein, daidzein, and glycitein—other subclasses include flavonols, catechins, etc.). Whereas soy products had been rare in the Western diet with the exception of oils, more and more processed foods, including granola bars, cereals, hot dogs, sausages, and infant formula, now contain soy products as fortifiers and meat substitutes (Patisaul and Jefferson 2010; Cederroth et al. 2012). Dietary intake varies widely between individuals (e.g., the “typical” Asian diet results in isoflavone consumption as high as 50 mg/kg body weight/day, whereas 1–3 mg/day total is more common in the Western diet) (Mortensen et al. 2009). As a point of comparison, infants fed exclusively soy formula consume approximately 6–9 mg/kg body weight/day in isoflavones (Cao et al. 2009), resulting in a mean plasma isoflavone concentration of 980 μg/L (compared to 9.4 μg/L in breast-milk-fed infants and 4.7 μg/L in cow’s milk-based formula-fed infants) (Cederroth et al. 2012). Seasonal variation also influences the phytoestrogen content of foods (e.g., the total isoflavone content of raw soybeans can range from 18 to 562 mg/100 g) (Mortensen et al. 2009).
Phytoestrogens from soy protein products are able to alter the synthesis, secretion, metabolism, and transport of natural hormones in the body. As a result they can affect such processes as sexual development and puberty, gamete production, pregnancy, and lactation (Patisaul and Jefferson 2010; Cederroth et al. 2012; Kim and Park 2012). In fact, the endocrine-disrupting properties of soy isoflavones were first discovered when a group of ewes grazing in a red clover patch developed infertility, later attributed to a phytoestrogen compound in red clover called formononetin (Cederroth et al. 2012). Isoflavones regulate plasma sex hormone-binding globulin (sHBG) levels and aromatase and 5-α reductase and displace testosterone and 17-β estradiol from sHBG sites (Patisaul and Jefferson 2010; Cederroth et al. 2012). As powerful as soy compounds have the potential to be, the effects and impact of soy compounds on reproductive health are not yet clear, as the differences in nomenclature, formulations, dosages, routes, times, and durations of administration are not standardized across studies and are therefore difficult to compare.
5.2.2 Antioxidant Vitamins
Vitamin E, vitamin C, and the carotenoids are among the major dietary antioxidants (Rock et al. 1996; Johnson et al. 2003). Vitamin E is a group of eight fat-soluble compounds that functions as a direct antioxidant. The discovery of vitamin E in 1922 and its essential role in rat reproduction is credited to Evans and Bishop (1922). Since that time, countless studies have been undertaken to determine the specific function of vitamin E and to test the potential benefits of vitamin E supplementation, particularly in fertility, that to date have been inconclusive (Brigelius-Flohe and Galli 2010). ß-carotene, the main source of provitamin A, and vitamin C (ascorbic acid) are both important ROS scavenging antioxidants (Burton and Ingold 1984; Weber et al. 1996).
5.3 Antioxidant Enzymes and Cofactors
The essential nutrients copper, zinc, manganese, and selenium are important factors in maintaining health, reproduction, and fertility (Bedwal and Bahuguna 1994). They are cofactors for copper, zinc-superoxide dismutase (Cu, Zn-SOD, or SOD1), manganese-SOD (Mn-SOD or SOD2), and selenium-glutathione peroxidases (SeGPXs), respectively (Rahman 2007). These cofactors are present at the enzyme catalytic site and their availability can determine the activity of such enzymes. SODs act to convert two superoxide radicals into hydrogen peroxide (H2O2) and oxygen. The family GPX catalyzes the reduction of H2O2 to water or lipid hydroperoxides to alcohol. Like GPX, catalase (CAT) decomposes H2O2 to water and oxygen. Although selenium is not itself an antioxidant, inadequate selenium is thought to adversely affect GPX activity (Fujii et al. 2005). Most of the GPX isoforms in mammals contain selenium and are dependent upon selenium for their function (Brigelius-Flohé and Maiorino 2013).
5.4 Antioxidants in Normal Reproductive Physiology
There is increasing evidence that antioxidants play a vital role in reproductive health and fertility. The local cellular environment influences oocyte development, ovulation, successful fertilization, and maintenance of early pregnancy. ROS and antioxidants have emerged as ubiquitous participants in normal human reproductive processes.
5.4.1 Puberty and Menarche
The age of puberty has decreased over the past 150 years creating much speculation into the etiology of the change, which is likely multifactorial. The decline has slowed or plateaued since the 1960s in the Western world; however, a decline is now being seen in some developing countries (Pierce and Hardy 2012). One hypothesis is that there has been a change in nutritional intake among today’s population. From a pregnant woman’s intake affecting fetal development, through lactation and the effects on breastfed infants, to the relatively recent expansion in soy-based infant formulas, to the changes in childhood food consumption and the explosion of childhood overweight and obesity, there are literally endless points along the spectrum of reproductive development that are subject to influence. Attention has gone into the effects of soy and soy products on reproductive development, as soy and the isoflavones it contains have known estrogenic properties and are able to interfere with the hypothalamic-pituitary axis.
Studies have reported conflicting results regarding phytoestrogen exposure and timing of puberty. A recent prospective longitudinal study (Adgent et al. 2012) found that soy-formula-fed infants experienced earlier menarche in comparison to breast-fed or other types of formula-fed infants. In this study, white females with term singletons were enrolled during pregnancy, and infants (n = 2124) fed soy formula (approximately 6–9 mg/kg/day isoflavone intake, with plasma levels reaching up to 1000 ng/mL (Patisaul and Jefferson 2010) at or before 4 months of age) experienced a median age at menarche of 12.4 years compared to 12.8 years in the general study population (n = 2920) and the exclusively breast-fed population (n = 631) (Adgent et al. 2012). Another study (Zung et al. 2008) showed a significantly higher prevalence of breast buds in the second year of life in children fed soy formula, while a study by Bernbaum et al. showed re-estrogenized vaginal epithelium at 6 months of age in soy formula-fed infants in comparison to human or cow’s milk-fed counterparts, whose vaginal epithelium did not re-estrogenize (Bernbaum et al. 2008). A Korean case-control study of approximately 200 girls (Kim et al. 2011), both with central precocious puberty (CPP) and age-matched controls, reported a significantly higher prevalence of CPP in girls with total serum isoflavone levels ≥30 nmol/L than those with levels <30 nmol/L.
In contrast, phytoestrogen exposure later in life, from food rather than formula, has been associated with delayed markers of puberty. A German longitudinal study of over 200 healthy children (Cheng et al. 2010) reported that girls with the highest levels of dietary isoflavones (423.4–19,178 μg/day) experienced onset of breast development and reached peak height velocity approximately 7–8 months later than those girls with the lowest intakes (4.1–21.9 μg/day). Adding evidence to dietary isoflavones’ ability to delay breast development, a different German study (Cheng et al. 2012) reported that girls with the highest tertile intake of isoflavones (≥423 μg/day) experienced onset of Tanner stage 2 breast development 0.7 years later than girls with isoflavone intake in the lowest tertile (≤22 μg/day).
Jefferson et al. studied the effects of genistin (the glycosylated form of genistein and the substance that contributes >65% of the isoflavone content of soy formulas) in the reproductive health of rats. They found that supplementation with oral genistin (20, 40, and 60 mg/kg/day via genistein-equivalent doses, 6.25 mg/kg/day genistein = 10 mg/kg/day of genistin) resulted in altered ovarian differentiation (multioocyte follicles), delayed vaginal opening, abnormal estrous cycles, decreased fertility, and delayed parturition compared to control rats who were not supplemented. There was a positive correlation between dose and magnitude of effect. For comparison, infants fed soy formula are estimated to consume 4–7 mg/kg/day of genistein (Jefferson et al. 2009). Although the doses administered in the study are higher than those generally consumed by infants on soy formula, the pharmacokinetics of genistein in infants are not known, and further research is needed to determine health effects based on the dose and timing of exposure.
Outside of studies involving soy products, other studies have focused on the effects of vitamins and minerals on puberty, and there has been conflicting evidence. Higher consumption of dietary vitamin A (in the form of both retinol and beta-carotene) by 10–14-year-old girls has been associated with both a lower (Maclure et al. 1991) and higher (Moisan et al. 1990) age at menarche. A study of British girls (Rogers et al. 2010) found that those with higher intakes of magnesium or zinc were associated with an earlier age at menarche, while those with higher thiamin or iron intakes experienced later menarche (Kissinger and Sanchez 1987). It is unknown whether these effects can be attributed specifically to the vitamins’ and minerals’ antioxidant properties.
5.4.2 Menstrual Cycle
The normal female reproductive cycle is orchestrated by the interplay of various hormones, mainly luteinizing hormone (LH), follicle-stimulating hormone (FSH), estrogen, and progesterone, on the hormone-sensitive reproductive organs, ovaries, and uterus. There have been few studies examining the natural fluctuations in antioxidants across the normal menstrual cycle, and those that have been completed may lack the power to show significant differences within individuals. One study examining nine micronutrients, six lipids and lipid peroxidases, and antioxidant enzymes including GPX, SOD, and paraoxonase failed to show significant differences within nine healthy women across the menstrual cycle; however, it did show significant variation between individuals (Browne et al. 2008).
In contrast, Cornelli et al. did report variation in oxidative stress in individual women across the menstrual cycle (Cornelli et al. 2013). They found that the level of oxidative stress, as measured by the reactive oxygen metabolites test (d-ROMs), which measures hydroperoxide plasma levels and is used as a representative measure of oxidative stress, increases a few days before the estrogen peak and lasts through the progesterone phase, suggesting that a woman is in a state of relative oxidative stress for two-thirds of the normal menstrual cycle. Similarly, Michos et al. reported a steady increase in the total antioxidant capacity, alongside the increase in estradiol concentration, from the time of menstruation to ovulation in healthy, eumenorrheic Greek women (Michos et al. 2006). A Polish study of 12 women (Karowicz-Bilinska et al. 2008) also reported increased oxidative stress during the luteal phase. In their study, urinary H2O2, which has been proposed as a noninvasive marker for whole-body oxidative stress, was analyzed on each day of the menstrual cycle. Despite variations between individuals, a consistent pattern emerged within individuals: the level of H2O2 was found to be significantly lower across the entire follicular phase as compared to the luteal phase (Karowicz-Bilinska et al. 2008), suggesting that whole-body oxidative stress is increased during the luteal phase of the menstrual cycle.
5.4.3 Ovarian Function
Ovarian follicular development is dependent upon a number of mechanisms. The finite pool of primordial follicles must mature into the primary, preantral, and antral stage follicles and then finally reach the preovulatory stage and release during ovulation. Decreased levels of antioxidant enzymes have been reported in the follicular fluid of women with unexplained infertility, and ROS are known to be detrimental to oocyte quality (Tamura et al. 2008). ROS are involved in the follicular fluid environment, folliculogenesis, and steroidogenesis. Oocyte maturation is affected by ROS and antioxidants such as SOD1, SOD2, and GPX, which has been illuminated by immunohistochemical localization, mRNA expression studies, and thiobarbituric acid localization (Agarwal et al. 2006).
Unlike most organs, the function of the ovary is significantly influenced by ovarian and follicular development in utero. Bernal et al. reported that maternal undernutrition could have long-lasting and profound effects on the reproductive potential of offspring (Bernal et al. 2010). The process is unclear, though there is some thought that leptin acts as a metabolic signal to the central reproductive axis, acting as a permissive neuro-regulatory factor for the onset of puberty, and both stimulating and inhibiting ovulatory processes and ovarian steroidogenesis. It appears that maternal undernutrition may also increase oxidative stress in the developing fetus and offspring. In a study of rats (Bernal et al. 2010), maternal caloric undernutrition (rats fed 50% of a standard control diet) during pregnancy and lactation was shown to significantly reduce the primary and secondary follicle counts in their offspring. Antral follicle counts were reduced significantly in offspring of mothers undernourished during any stage of pregnancy and/or lactation. These offspring were found to have increased ovarian protein carbonyls and reduced levels of peroxiredoxin 3 hyperoxidation mRNA (a mitochondrial antioxidant protein that breaks down endogenous hydroperoxides), implying decreased antioxidant defenses and increased oxidative damage. It is speculated that oxidative stress accelerates reproductive maturity along with faster decline in ovarian reserve (Bernal et al. 2010).
Isoflavones have also been shown to modulate the normal reproductive cycle. A recent meta-analysis of 47 studies (Hooper et al. 2009) revealed that in premenopausal women, consumption of soy isoflavones in intervention groups reduced circulating LH and FSH and increased menstrual cycle length as compared to controls. However, subgroup analyses by isoflavone intake level (<25 mg/day, 25 to <50 mg/day, 50 to <75 mg/day, 75 to <100 mg/day, ≥100 mg/day) showed no significant effect. In a review of almost 50 studies on premenopausal women given soy supplementation (Jefferson 2010), no effect was seen on estradiol, estrone, or sHBG, but there was a decrease in both LH and FSH and increased cycle length in those supplemented with soy. In contrast, a prospective cohort study of more than 250 healthy menstruating women (Filiberto et al. 2013) reported that isoflavone intake was not found to be associated with estradiol, free estradiol, progesterone, LH, or FSH concentrations, but isoflavone intake in the highest quartile (1.6–78.8 mg/day) was significantly associated with a greater sHBG concentration, in comparison with consumption in the lowest quartile (0.0–0.3 mg/day). Isoflavone intake was not associated with sporadic anovulation in this cohort. This study suggests that, though isoflavones may cause some endocrine effects, they may not interfere with ovulation. Of note, most studies have shown that there are no significant effects resulting from soy consumption at normal dietary levels (10–25 mg soy isoflavones/day, and even up to 50 mg/day), but the effects of ovulatory hormone (e.g., LH, FSH) disturbance are fairly consistent with higher levels (e.g., ≥100 mg soy isoflavones/day, a level that can be achieved through diets very high in soy) (Jefferson 2010). In one of the only studies to show hormonal disruption resulting from low doses of isoflavones (Faber and Hughes 1993), low doses of genistein (10 μg subcutaneous genistein) were shown to increase GnRH-induced LH release in rats, while high doses (100–1000 μg subcutaneous genistein) decreased release of LH.
5.4.4 Uterine Function
Cyclic changes in the endometrium are accompanied by cyclic variations in the expression of antioxidants. For instance, both SOD1 and SOD2 are highly expressed in the epithelial and stromal cells in the endometrium, and SOD1 and SOD2 expression increases consistently throughout the proliferative phase and into the mid-secretory phase, where it is at similar levels to those found during early pregnancy. SOD1 and SOD2 activity decrease, while lipid peroxide levels increase, just prior to menstruation. The shift in favor of oxidative stress leads to production of PGF2α, which causes endometrial shedding via vasoconstriction (Sugino 2007). Thioredoxin (TRX), another antioxidant, is expressed in the early secretory phase, and it has been shown in mice that the targeted disruption of TRX, results in lethal effects on an embryo (Agarwal et al. 2006).
Isoflavones have been a topic of interest with regard to their estrogenic effects on the endometrium. One randomized controlled trial (Unfer et al. 2004a) demonstrated a significant increase in the incidence of endometrial hyperplasia (3.8% vs 0%) in 179 women randomized to soy tablets (150 mg/day of isoflavones) for 5 years as compared to placebo. This intake can be readily achieved through diet alone and is about half the intake in a traditional Asian diet. One manifestation of focal endometrial overgrowth is in the formation of endometrial polyps, which consist of a vascular core surrounded by localized pedunculated overgrowths of endometrial stroma and glands. Polyp formation is poorly understood and it is unknown why some women form polyps while others do not. One study (Pejić et al. 2013) examining the fluctuations in antioxidant enzyme levels within polyps in concert with fluctuations in reproductive hormone levels found a negative correlation between LH and SOD (SOD1 and SOD2), and between FSH/LH and glutathione peroxidase in polyp tissue, while in the blood there was a positive correlation between estrogen and SOD levels. Similar to prior studies, Pejic et al. found lower levels of lipid hydroperoxides(LHP) in the blood during the luteal phase when compared to the follicular phase (Pejić et al. 2013).
Uterine leiomyomas, also called fibroids or myomas, are benign muscle tumors of the uterus; they contain a large amount of extracellular matrix, feeding vessels, and smooth muscle fibers, and are surrounded by a thin capsule of areolar tissue (Santulli et al. 2013).Suggested they can cause heavy bleeding and pelvic pain and are associated with infertility and adverse birth outcomes. The pathogenesis of fibroids is largely unknown. A large prospective cohort study involving 19,972 women (D’Aloisio et al. 2010) suggested that women who self-reported being fed soy formula in infancy had an increased risk of developing leiomyoma later in life (RR = 1.25; 95% CI 0.97–1.61). A case-control study (Santulli et al. 2013) involving women undergoing surgery for leiomyoma and controls undergoing surgery for various other pelvic pathologies, found a significantly higher level of serum protein carbonyl groups and advanced oxidation protein products (AOPP) in the fibroid group compared to controls, while serum thiol (an antioxidant) levels were lower. Interestingly, the serum AOPP levels were positively correlated with the fibroid weight, and serum AOPP and serum protein carbonyls were positively correlated with the duration of infertility.
5.4.5 Pregnancy
The corpus luteum is a transient organ whose function is to produce progesterone when fertilization occurs in order to maintain the pregnancy. The deterioration of the corpus luteum in the absence of pregnancy is thought to be due to ROS-mediated events, while evidence suggests that antioxidant enzymes play a role in corpus luteum rescue from apoptosis when pregnancy ensues (Al-Gubory et al. 2012). Antioxidants likely play a vital role in the function of the corpus luteum (Arianmanesh et al. 2011); however, the particular antioxidants involved in its maintenance have not yet been established.
The pathway from fertilization through implantation and continued embryonic and fetal development is dependent upon innumerable factors. The role of antioxidants in various steps along the way has been studied with inconclusive results. In a study of 99 New York state women attempting conception (Bloom et al. 2011), blood metals were measured to determine whether there was a relation between levels of arsenic, cadmium, lead, magnesium, nickel, selenium, and zinc and conception. There were no statistically significant differences found. The authors observed a 51.5% increase in the probability of conception for every 3.60 μg/L increase in serum magnesium level (β = 4.197, 95% CL β −0.216, 8.610, p = 0.062), while there was a 27.7% decrease in the probability of conception for every 0.54 μg/L increase in zinc level (β = −2.234, 95% CL β −5.004, 0.536, p = 0.114).
Pregnancy is a physiologic state characterized by increased metabolic demands and requirements for oxygen, which increases the rate of production of ROS. In comparison to age-matched, nonpregnant women, women even with uncomplicated pregnancies have elevated levels of oxidative stress and of circulating lipid peroxides (Aversa et al. 2012). At the same time, Aversa et al. report that levels of many antioxidants such as vitamin E, erythrocyte thiols, ceruloplasmin, and iron-binding capacity are increased, and levels of SOD and GPX have been shown to decrease in pregnancy relative to nonpregnant levels. Fugii et al. hypothesized that SOD1 helps to maintain pregnancy by preventing the accumulation of superoxide radicals, thereby decreasing synthesis of PGF2α, which has been shown to increase at the end of spontaneous abortion (Fujii et al. 2005). Although both oxidative stress and some antioxidant levels increase throughout pregnancy, the overall balance appears to sway in favor of elevated ROS (Aversa et al. 2012).
5.5 Antioxidants in Reproductive Disorders and Complications
ROS-induced cellular oxidative stress can adversely affect function of reproductive organs and fertility. Imbalance in the oxidant/antioxidant relationship has been implicated in numerous reproductive disorders and complications, including endometriosis, polycystic ovarian syndrome, oocyte aging, dysmenorrhea and premenstrual syndrome, spontaneous abortion, and infertility (Fig. 5.1).
5.5.1 Endometriosis
Endometriosis is characterized by implantation of endometrial tissue outside the uterus and is a chronic inflammatory disease that affects 21–44% of infertile women and 4–22% of fertile women (Tamura et al. 2009), (Fig. 5.2). This disease manifests symptomatically with chronic pelvic pain, progressive dysmenorrhea, and dyspareunia. Women with endometriosis have been shown to increase peritoneal fluid production, along with increased peritoneal fluid macrophage production of ROS (Tamura et al. 2009). This leads to a localized inflammatory reaction favoring oxidative stress; it is unknown whether the relative state of oxidative stress leads to, or is a result of, endometriosis.
A model of disease for endometriosis based on data from both animal and human studies (reprinted with permission from Flores et al. 2007)
A lower total antioxidant potential has been reported in the pelvic fluid and serum of infertile women with endometriosis as compared to infertile women without endometriosis. In a study on serum ROS markers in women undergoing pelvic laparoscopy for a variety of indications (Jackson et al. 2005), those who were diagnosed with endometriosis at the time of laparoscopy had a weak association with thiobarbituric acid-reducing substances (TBARS), a measure of lipid peroxidation. In a cohort study (Prieto et al. 2012) of 91 women with infertility, four markers of oxidative stress were studied in serum and follicular fluid samples obtained at the time of egg retrieval. Women with infertility due to endometriosis (n = 23) were shown to have lower levels of follicular fluid vitamin C, lower plasma SOD concentrations, and lower plasma vitamin E levels than women with infertility due to other reasons, who served as the controls (n = 68). The end products of lipid peroxidation are reactive aldehydes, such as malondialdehyde (MDA). There was a nonsignificant trend toward lower serum MDA levels in women with endometriosis. Jana et al. studied 135 women with infertility and similarly reported that those with endometriosis had higher levels of ROS, lipid peroxidation, and advanced oxidation protein products and lower levels of total antioxidant capacity, SOD, CAT, and glutathione than the controls with tubal factor infertility (without endometriosis). This study used proton nuclear magnetic resonance spectroscopy based on targeted metabolite profiling (Jana et al. 2013).
Not only the overall concentrations of antioxidants but also the fluctuations throughout the menstrual cycle have been studied in the context of endometriosis. Women with endometriosis have been shown to have consistently elevated levels of xanthine oxidase, SOD, CAT, and GPX expression throughout their cycles, whereas women without endometriosis have cyclic variations in these enzyme levels (Gupta et al. 2006). This may suggest that there is a consistently increased ROS burden in the setting of endometriosis, with a concomitant rise in antioxidant production in an attempt to combat oxidative damage. Once the importance of oxidative stress in the pathophysiology of endometriosis was discovered, studies involving interventions with antioxidant supplementation began to appear with some promising results, first in laboratory studies and animal models and later in humans. One study of human endometriotic and healthy endometrial cells both in vitro and implanted into mice (Ngô et al. 2009) showed increased ROS production, altered ROS detoxification pathways, and decreased catalase levels in endometriotic cell lines. Addition of the antioxidant, N-Acetyl-Cysteine (NAC), to the cultured cells in vitro and in mouse models seemed to counterbalance the oxidative stress markers in the endometriotic cell lines.
Resveratrol, a natural polyphenol synthesized by plants in response to ultraviolet radiation and fungal infections, has been studied for its antioxidant properties in a variety of conditions. In a mouse study, supplementation with resveratrol following injection of human endometriotic implants was shown to decrease the number of implants by 60% and the total volume by 80% compared to controls (Goud et al. 2008). The invasiveness of human endometrial stromal cells in culture was also decreased significantly with the addition of resveratrol, by up to 78%, in a concentration-dependent fashion compared to controls. In a similar study of resveratrol in mice (Rudzitis-Auth et al. 2013), supplementation with resveratrol was shown to inhibit angiogenesis in peritoneal and mesenteric endometrial implants along with reducing growth and resulting in lower final size of implants in comparison to controls not given resveratrol. Resveratrol is a promising antioxidant therapy for endometriosis and deserves further study.
As the long-term survival of endometriotic implants is dependent upon neovascularization, it has been postulated that high concentrations of vascular endothelial growth factor (VEGF) permit the growth of vasculature necessary for the survival of these implants. High concentrations of VEGF have been found in the peritoneal fluid of women with endometriosis (Chaudhury et al. 2013). Therefore, recent studies have focused on anti-angiogenic strategies for treatment of endometriosis. Nanoceria, or cerium oxide nanoparticles, have been studied in a variety of diseases for their antioxidant and anti-inflammatory properties. These particles can mimic SOD and CAT. In a study of mice injected with mouse endometrial implants (Chaudhury et al. 2013), those treated with nanoceria were found to have decreased levels of oxidative stress and angiogenic factors, along with decreased endometrial glands, in comparison to controls or those mice treated with NAC. Mice treated with nanoceria also had a higher number and quality of oocytes compared to control or NAC-treated mice. In another mouse study (Jana et al. 2012), curcumin, a known antioxidant and anti-inflammatory constituent of turmeric, was found to cause regression of endometriosis by inhibiting NF-kB translocation and matrix metalloprotein-3 (MMP-3) expression and to accelerate apoptosis in endometrial implants by a cytochrome-c mediated mitochondrial pathway. MMPs support the growth and invasion of endometrial implants and are modulated by NF-kB. In this study, curcumin upregulated p53 expression by about tenfold on Western blot densitometry (signal intensity 0.8 as compared to 0.1 in the control group) and the numbers of peritoneal endometrial glands were found to be decreased about threefold on densitometry (signal intensity of approximately 4 as compared to 12) by pretreatment with curcumin as compared to controls.
Vitamins C and E have been studied to improve endometriosis at both cellular and clinical levels. In a randomized, placebo controlled trial of 59 women with pelvic pain and a history of endometriosis and/or infertility (Kavtaradze et al. 2003), 43% of those in the intervention group (given 1200 IU of all-racemic vitamin E and 1000 mg of vitamin C daily for 2 months), reported a significant improvement in chronic daily pain as compared to the placebo group, who reported no significant improvement. Though not statistically significant, there was clinical improvement in dysmenorrhea and dyspareunia, with 37% reporting significant improvement in dysmenorrhea and 24% reporting significant improvement in dyspareunia compared to controls. Another study (Mier-Cabrera et al. 2008) randomized infertile women with endometriosis to 343 mg vitamin C and 84 mg all-racemic vitamin E versus placebo for 6 months. They found that plasma and peritoneal fluid levels of MDA and lipid hydroperoxidases were significantly decreased by 6 months in the intervention group as compared to the placebo group. Of note, the post-intervention pregnancy rates (19% in intervention group vs. 12% in placebo group by 9 months post-study) were not statistically significantly different.
5.5.2 Polycystic Ovarian Syndrome
Polycystic ovarian syndrome (PCOS) is the most common endocrine disorder of reproductive-aged women and also a common cause of infertility. It is characterized by anovulation, androgen excess, and insulin resistance (Fenkci et al. 2003). Like other reproductive pathologies, PCOS is likely to be partially caused by, and certainly results in, imbalance of oxidants and antioxidants. In a case-control study of 30 women with PCOS and 31 healthy age-matched controls (Fenkci et al. 2003), antioxidant status was measured in serum samples using 2,2′-azino-di-(3-ethylbenzthiazoline sulfonate acid (ABTS)) radical cation assay. Total antioxidant status was lower in women with PCOS than in controls. In another case-control study of 33 women with PCOS and 28 healthy controls (Hilali et al. 2013), serum prolidase, total oxidant status (TOS), as measured by the an automated method (Erel 2005), oxidative stress index (as measured by the percent ratio of TOS to total antioxidant status), LH, prolactin, and testosterone levels were significantly higher in women with PCOS as compared to controls, and total antioxidant status (TAS), measured by another automated method (Erel 2004) was lower in women with PCOS, however this difference was not statistically significant. In a Turkish study (Coskun et al. 2013) examining serum levels of selenium in 36 women diagnosed with PCOS and 33 age and body mass index-matched healthy controls, women with PCOS were found to have significantly lower plasma selenium levels than controls. There was also a statistically significant negative correlation noted between selenium level and LH and total testosterone level in all women studied. PCOS, along with other reproductive pathologies, is an area that would benefit greatly from further antioxidant research.
5.5.3 Oocyte Aging
Accumulating data suggest that ROS deteriorate oocyte quality and accelerate oocyte aging (Tamura et al. 2012). In order to protect the fragile oocytes from oxidative damage, antioxidants must be present in adequate concentrations. Oocyte senescence is thought to be at least partially modulated by an increase in oxidative stress, as a reduction in glutathione and catalase activity and an increase in SOD have been found in older women compared with younger women (Agarwal et al. 2006). It is unknown whether antioxidant defenses within the ovary decrease with age or whether the ROS concentration increases such that significant damage is caused to remaining oocytes, resulting in senescence. In a study of rat oocytes (Goud et al. 2008), young oocytes were resistant to H2O2 effects, while relatively “old” oocytes experienced accelerated aging when exposed to H2O2. When exposed to low levels of hypochlorous acid, young oocytes experienced accelerated aging, while lysis was seen in “old” oocytes. Furthermore, at high concentrations, oocyte viability was compromised in both age groups. This suggests that young oocytes have enhanced antioxidant defenses as compared to “old” oocytes. In fact, antioxidants such as vitamin C and reduced glutathione have been shown to be protective against postovulatory oocyte aging in vitro (Goud et al. 2008).
5.5.4 Dysmenorrhea and Premenstrual Syndrome
Antioxidant status has been studied in women with painful menses and premenstrual syndrome. In a study of 20 healthy women (Duvan et al. 2011), with clinically diagnosed premenstrual syndrome (PMS) and 21 controls, serum oxidant and antioxidant status was evaluated by measurement of lipid hydroperoxides, MDA, protein carbonyl, total thiol (T-SH), and total antioxidant capacity (TAC), measured by the ferric reducing ability of plasma (FRAP) assay via serum samples on day 3 and day 21 of the menstrual cycle. The PMS group was found to have statistically increased day 21 lipid hydroperoxides and decreased day 3 and day 21 TAC levels in comparison to the control group, suggesting that those with PMS have an increase in oxidative stress throughout the menstrual cycle.
Thiamin (vitamin B1) acts as an antioxidant (Lukienko et al. 2000) and has been studied as an intervention for dysmenorrhea. In an Indian crossover study of 556 women with dysmenorrhea (Gokhale 1996), 100 mg of thiamin daily for 3 months resulted in improvement in dysmenorrhea in >90% of women, compared to <1% of controls taking a placebo. There have been a few studies examining vitamin E supplementation for dysmenorrhea and menorrhagia with promising results (Ziaei et al. 2001, 2005; Butler and McKnight 1955). Although the mechanism of action is unclear, it is thought that vitamin E might inhibit arachidonic acid release and thereby decrease prostaglandin formation (Ziaei et al. 2005). Magnesium, vitamin B6, and omega-3 fatty acids have also been studied for dysmenorrhea with mixed results (Dennehy 2006). These areas would benefit from further study.
5.5.5 Infertility
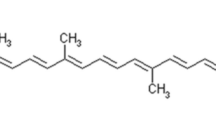
As has been shown with other reproductive functions, fertility can be affected by changes in the oxidant/antioxidant balance. Much research has gone into determining the causes behind infertility, and oxidative stress has been a frequent topic of both basic science and clinical studies (Ruder et al. 2008), (Fig. 5.3). Fairly consistently across studies, women with unexplained infertility have decreased antioxidant enzyme levels in their follicular fluid (Tamura et al. 2012). More specifically, follicular fluid from women with unexplained infertility was found to have decreased selenium content than in those women with tubal infertility or a known male-related cause (0.44 μmol/L vs. 0.51 μmol/L, p < 0.05) (Paszkowski et al. 1995). Women with unexplained infertility or premature ovarian failure have also been shown to have significantly higher serum levels of the autoantibody protein, selenium-binding protein-1 (Edassery et al. 2010). Increased oxidative stress alters the fatty acid profile due to peroxidative breakdown. As fatty acids are the precursors to prostaglandins, which mediate various reproductive processes, it is postulated that altered fatty acid profiles can have a direct effect on fertility. An Indian study (Mehendale et al. 2009) found significantly reduced fatty acid levels (eicosapentaenoic acid and erythrocyte docosahexaenoic acid) and increased levels of MDA along with decreased levels of vitamin E, in the serum of infertile women as compared to controls.
The role of oxidative stress in fertility (reprinted with permission from Ruder et al. 2008)
Black cohosh, a plant with conflicting evidence for its estrogenic properties, and other supplements have also been studied. Women with unexplained infertility undergoing ovulatory induction with clomiphene who were supplemented with black cohosh (120 mg/day for cycle days 1–12) were found to have increased levels of LH, progesterone, and estradiol, increased endometrial thickness, and increased pregnancy rates compared to controls (Shahin et al. 2008). In another study (Unfer et al. 2004b), women who were supplemented with luteal phase support using progesterone (50 mg daily) and phytoestrogen tablets (1500 mg soy isoflavone tablet daily containing 40–45% by weight genistein, 40–45% by daidzein, 10–20% glycitein) had significantly higher implantation, clinical pregnancy, and delivery rates compared to controls. A randomized controlled trial of 150 women with luteal phase defects (Dennehy 2006) found that supplementation with 750 mg/day of vitamin C resulted in a significantly higher fertility rate as compared to the placebo (25% vs. 11%); progesterone levels were also significantly increased in the treatment group (52.6% vs 21.7%).
Although the mechanism by which ROS affect fertility is not yet clear, elevated levels of ROS and inflammatory cytokines have been shown to reduce ciliary beat frequency in fallopian tubes (Comhaire 2010). This will surely be an area of continued research, as minimally invasive interventions to improve fertility have the potential to drastically reduce patient morbidity and cost to both patients and the healthcare system.
5.5.6 Spontaneous Abortion
The etiology of spontaneous abortion is, more often than not, unknown. Although many spontaneous abortions are due to chromosomal defects, environmental factors also play a large role, and the oxidant/antioxidant balance is likely to be a factor in the pathophysiology behind, or sequelae of, spontaneous abortions. Biochemical markers of ROS-induced membrane damage, such as lipid peroxidation products, reach very high levels immediately prior to spontaneous abortion (Gupta et al. 2007). While increased levels of antioxidants have been demonstrated in normal, healthy pregnancies, loss of antioxidant defenses has been seen in women with recurrent abortion (Şimşek et al. 1998).
Much research has focused on selenium status in women with spontaneous abortion, and results have been conflicting. A statistically significant decrease in serum or red blood cell selenium levels was found in women with a history of recurrent pregnancy loss in two studies, as compared to healthy nonpregnant women with at least one successful pregnancy and no history of spontaneous abortion (Kumar et al. 2002; Koçak et al. 1999). An observational study in the United Kingdom (Mistry et al. 2012) reported significantly lower serum selenium concentrations in women with first trimester spontaneous abortion in comparison to age-matched nonpregnant or healthy gestation-matched women. A case-control study in Indonesia (Abdulah et al. 2013) similarly reported significantly decreased serum selenium concentrations in women who had undergone spontaneous abortion compared with controls; glutathione peroxidase levels were similar in the two groups. However, two other studies reported no differences in serum selenium between women with recurrent spontaneous abortion and healthy women with no history of spontaneous abortion (Al-Kunani et al. 2001; Nicoll et al. 1999). Aberrant placentation has also been implicated in recurrent spontaneous abortion (Burton et al. 2003), and it is thought that this leads to increased oxidative stress and syncytiotrophoblast dysfunction, a proposed cause of spontaneous abortion. Gupta et al. reported elevated plasma levels of lipid peroxides and glutathione, as well as lower levels of vitamin E and β-carotene in women with spontaneous abortion (Gupta et al. 2007).
Few studies have yet attempted interventions with antioxidants during the periconception and early prenatal period. However, an Egyptian prospective study (Amin et al. 2008) enrolled 166 women with a history of recurrent unexplained pregnancy loss and treated one group with NAC (0.6 g) and folate (500 μg/day) and a control group solely with folate (500 μg/day). The intervention group with NAC + folate experienced a significantly higher rate of continuation of a living pregnancy beyond 20 weeks (RR 2.9; 95% CI 1.5–5.6) and also take-home baby rate (RR 1.98; 95% CI 1.3–4.0). Although antioxidant supplementation may hold promise in terms of increasing rates of conception and pregnancy retention (Al-Gubory 2013), the difficulties in getting Human Subject Committee approval for intervention studies concerning pregnant women will likely make progress in this area slow.
There is great interest in antioxidant supplementation for women with unexplained infertility. In a secondary data analysis of 437 women with unexplained infertility participating in the Fast Track and Standard Treatment Trial (FASTT) (Reindollar et al. 2010), women with body mass index ≥25 kg/m2 who had an increased intake of β-carotene from dietary supplements had a shorter time to pregnancy (HR 1.29, 95% CI 1.09–1.53 in continuous analyses adjusted for treatment, age, and total energy intake) (Ruder et al. 2014). Intake of vitamin C dietary supplements wasalso associated with a shorter time to pregnancy among women with body mass index <25 kg/m2 (HR 1.09, 95% CI 1.03–1.15) and women <35 years old (HR 1.10, 95% CI 1.02–1.18). Vitamin E supplementation was associated with a shorter time to pregnancy in women ≥35 years old (HR 1.07, 95% CI 1.01–1.13). These data support the theory that age, body mass index, and antioxidant status combined contribute to fertility and offer avenues for further study.
5.6 Conclusions
Although there is a growing interest in the role of antioxidants in normal reproductive physiology and also their therapeutic role in various pathologies, there are many methodological issues that make conclusive data difficult to produce. There are numerous forms of most antioxidants, and the forms and dosages used in different studies are so varied that it is difficult to compare results. While animal models are an excellent place to start, more human studies are needed. However, as antioxidants are present in a variety of foods and supplements, it becomes difficult to control for these exposures when analyzing human data in observational studies. Therefore, randomized controlled trials are ideal but are rarely approved in the setting of human conception and pregnancy, an area that would benefit greatly from further study. The spectrum of normal oxidant and antioxidant levels, both in organs and in serum, is still unknown, and it is difficult to draw conclusions without a solid basis for comparison. Many more carefully conducted, controlled, and adequately powered studies are needed in this field of research.
Normal human physiology is dependent upon a fine balance between oxidants and antioxidants. The female reproductive system and fertility are complicated and dynamic topics, of which much is still unknown. As studies continue to emerge, it is becoming increasingly clear that there is a complex and multifaceted interplay between ROS and antioxidants in the normal healthy state and that pathology emerges when this balance is offset. Whether oxidative stress is causative to pathologic conditions or results from them is unknown; however, it is clear that conditions ranging from spontaneous abortion to endometriosis favor oxidative stress and interventions with antioxidants have the potential to slow, reverse, or prevent these conditions. Unfortunately, studies examining antioxidant supplementation have been inconclusive to date. There is a vast knowledge deficit to fill, and many more studies are needed to elucidate the role of antioxidants and oxidative status in normal reproductive physiology and fertility, as well as in reproductive pathology. Antioxidants in reproductive health and fertility are a subject in its infancy and will continue to unfold as researchers and clinicians study this intriguing topic.
References
Abdulah R, Noerjasin H, Septiani L, Mutakin, Defi IR, Suradji EW, Puspitasari IM, et al. Reduced serum selenium concentration in miscarriage incidence of Indonesian subjects. Biol Trace Elem Res. 2013;154:1–6.
Adgent MA, Daniels JL, Rogan WJ, Adair L, Edwards LJ, Westreich D, Maisonet M, et al. Early-life soy exposure and age at menarche. Paediatr Perinat Epidemiol. 2012;26:163–75.
Agarwal A, Gupta S, Sharma RK. Role of oxidative stress in female reproduction. Reprod Biol Endocrinol. 2005;3:1–21.
Agarwal A, Gupta S, Sikka S. The role of free radicals and antioxidants in reproduction. Curr Opin Obstet Gynecol. 2006;1:325–32.
Al-Gubory KH, Fowler PA, Garrel C. The roles of cellular reactive oxygen species, oxidative stress and antioxidants in pregnancy outcomes. Int J Biochem Cell Biol. 2010;42:1634–50.
Al-Gubory KH, Garrel C, Faure P, Sugino N. Roles of antioxidant enzymes in corpus luteum rescue from reactive oxygen species-induced oxidative stress. Reprod Biomed Online. 2012;25:551–60.
Al-Gubory KH. Chapter 1: Maternal nutrition, oxidative stress and prenatal developmental outcomes. In: Agarwal A, Rizk B, Aziz N, editors. Handbook: studies on women’s health, oxidative stress in applied basic research and clinical practice. New York, NY: Springer Science and Business Media, Humana Press Inc; 2013. p. 1–31.
Al-Kunani AS, Knight R, Haswell SJ, Thompson JW, Lindow SW. The selenium status of women with a history of recurrent miscarriage. Br J Obstet Gynaecol. 2001;108:1094–7.
Amin AF, Shaaban OM, Bediawy MA. N-acetyl cysteine for treatment of recurrent unexplained pregnancy loss. Reprod Biomed Online. 2008;17:722–6.
Arianmanesh M, McIntosh R, Lea RG, Fowler PA, Al-Gubory KH. Ovine corpus luteum proteins, with functions including oxidative stress and lipid metabolism, show complex alterations during implantation. J Endocrinol. 2011;210:47–58.
Aversa S, Pellegrino S, Barberi I, Reiter RJ, Gitto E. Potential utility of melatonin as an antioxidant during pregnancy and in the perinatal period. J Matern Fetal Neonatal Med. 2012;25:207–21.
Bedwal RS, Bahuguna A. Zinc, copper and selenium in reproduction. Experientia. 1994;50:626–40.
Bernal AB, Vickers MH, Hampton MB, Poynton RA, Sloboda DM. Maternal undernutrition significantly impacts ovarian follicle number and increases ovarian oxidative stress in adult rat offspring. PLoS One. 2010;5:15558.
Bernbaum JC, Umbach DM, Ragan NB, Ballard JL, Archer JI, Schmidt-Davis H, Rogan WJ. Pilot studies of estrogen-related physical findings in infants. Environ Health Perspect. 2008;116:416–20.
Butler EB, McKnight E. Vitamin E in the treatment of primary dysmenorrhea. Lancet. 1955;268:844–7.
Bloom MS, Buck Louis G, Sundaram R, Kostyniak PJ, Jain J. Associations between blood metals and fecundity among women residing in New York State. Reprod Toxicol. 2011;31:158–63.
Brigelius-Flohe R, Galli F. Vitamin E: a vitamin still awaiting the detection of its biological function. Mol Nutr Food Res. 2010;54:583–7.
Brigelius-Flohé R, Maiorino M. Glutathione peroxidases. Biochim Biophys Acta. 2013;1830:3289–303.
Browne RW, Bloom MS, Schisterman EF, Hovey K, Trevisan M, Wu C, Liu A, et al. Analytical and biological variation of biomarkers of oxidative stress during the menstrual cycle. Biomarkers. 2008;13:160–83.
Burton GW, Ingold KU. B-carotene: an unusual type of lipid antioxidant. Science. 1984;224:569–73.
Burton GJ, Hempstock J, Jauniaux E. Oxygen, early embryonic metabolism and free radical-mediated embryopathies. Reprod Biomed Online. 2003;6:84–96.
Cao Y, Calafat AM, Doerge DR, Umbach DM, Bernbaum JC, Twaddle NC, Ye X, et al. Isoflavones in urine, saliva, and blood of infants: data from a pilot study on the estrogenic activity of soy formula. J Expo Sci Environ Epidemiol. 2009;19:223–34.
Cederroth CR, Zimmermann C, Nef S. Soy, phytoestrogens and their impact on reproductive health. Mol Cell Endocrinol. 2012;355:192–200.
Cetin I, Berti C, Calabrese S. Role of micronutrients in the periconceptional period. Hum Reprod. 2010;16:80–95.
Chaudhury K, Babu KN, Singh AK, Das S, Kumar A, Seal S. Mitigation of endometriosis using regenerative cerium oxide nanoparticles. Nanomedicine. 2013;9:439–48.
Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Diet and lifestyle in the prevention of ovulatorydisorder infertility. Obstet Gynecol. 2007;110:1050–8.
Cheng G, Buyken AE, Shi L, Karaolis-Danckert N, Kroke A, Wudy SA, Degen GH, et al. Beyond overweight: nutrition as an important lifestyle factor influencing timing of puberty. Nutr Rev. 2012;70:133–52.
Cheng G, Remer T, Prinz-Langenohl R, Blaszkewicz M, Degen GH, Buyken AE. Relation of isoflavones and fiber intake in childhood to the timing of puberty. Am J Clin Nutr. 2010;92:556–64.
Comhaire F. The role of food supplementation in the treatment of the infertile couple and for assisted reproduction. Andrologia. 2010;42:331–40.
Cornelli U, Belcaro G, Cesarone MR, Finco A. Analysis of oxidative stress during the menstrual cycle. Reprod Biol Endocrinol. 2013;11:74.
Coskun A, Arikan T, Kilinc M, Arikan DC, Ekerbiçer HÇ. Plasma selenium levels in Turkish women with polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol. 2013;168:183–6.
D’Aloisio AA, Baird DD, DeRoo LA, Sandler DP. Association of intrauterine and early-life exposures with diagnosis of uterine leiomyomata by 35 years of age in the sister study. Environ Health Perspect. 2010;118:375–81.
Dennehy CE. The use of herbs and dietary supplements in gynecology: an evidence-based review. J Midwifery Womens Health. 2006;51:402–9.
Duvan CI, Cumaoglu A, Turhan NO, Karasu C, Kafali H. Oxidant/antioxidant status in premenstrual syndrome. Arch Gynecol Obstet. 2011;283:299–304.
Edassery SL, Shatavi SV, Kunkel JP, Hauer C, Brucker C, Penumatsa K, Yu Y, et al. Autoantigens in ovarian autoimmunity associated with unexplained infertility and premature ovarian failure. Fertil Steril. 2010;94:2636–41.
Erel O. A novel automated direct measurement method for total antioxidant capacity using a new generation, more stable ABTS radical cation. Clin Biochem. 2004;37:277–85.
Erel O. A new automated colorimetric method for measuring total oxidant status. Clin Biochem. 2005;38:1103–11.
Evans HM, Bishop KS. On the existence of a hitherto unrecognized dietary factor essential for reproduction. Science. 1922;56(1458):650–1.
Faber KA, Hughes CL Jr. Dose-response characteristics of neonatal exposure to genistein on pituitary responsiveness to gonadotropin releasing hormone and volume of the sexually dimorphic nucleus of the preoptic area (SDN-POA) in postpubertal castrated female rats. Reprod Toxicol. 1993;7:35–9.
Fenkci V, Fenkci S, Yilmazer M, Serteser M. Decreased total antioxidant status and increased oxidative stress in women with polycystic ovary syndrome may contribute to the risk of cardiovascular disease. Fertil Steril. 2003;80:123–7.
Filiberto AC, Mumford SL, Pollack AZ, Zhang C, Yeung EH, Schliep KC, Perkins NJ, et al. Usual dietary isoflavone intake and reproductive function across the menstrual cycle. Fertil Steril. 2013;100:1727–34.
Flores I, Rivera E, Ruiz LA, Santiago OI, Vernon MW, Appleyard CB. Molecular profiling of experimental endometriosis identified gene expression patterns in common with human disease. Fertil Steril. 2007;87:1180–99.
Fujii J, Iuchi Y, Okada F. Fundamental roles of reactive oxygen species and protective mechanisms in the female reproductive system. Reprod Biol Endocrinol. 2005;3:43.
Gernand AD, Schulze KJ, Stewart CP, West KP Jr, Christian P. Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nat Rev Endocrinol. 2016;12:274–89.
Gokhale LB. Curative treatment of primary (spasmodic) dysmenorrhea. Indian J Med Res. 1996;103:227–31.
Goud AP, Goud PT, Diamond MP, Gonik B, Abu-Soud HM. Reactive oxygen species and oocyte aging: role of superoxide, hydrogen peroxide, and hypochlorous acid. Free Radic Biol Med. 2008;44:1295–304.
Gupta S, Agarwal A, Banerjee J, Alvarez JG. The role of oxidative stress in spontaneous abortion and recurrent pregnancy loss: a systematic review. Obstet Gynecol Surv. 2007;62:335–47.
Gupta S, Agarwal A, Krajcir N, Alvarez JG. Role of oxidative stress in endometriosis. Reprod Biomed Online. 2006;13:126–34.
Hilali N, Vural M, Camuzcuoglu H, Camuzcuoglu A, Aksoy N. Increased prolidase activity and oxidative stress in PCOS. Clin Endocrinol (Oxf). 2013;79:105–10.
Hooper L, Ryder JJ, Kurzer MS, Lampe JW, Messina MJ, Phipps WR, Cassidy A. Effects of soy protein and isoflavones on circulating hormone concentrations in pre- and post-menopausal women: a systematic review and meta-analysis. Hum Reprod Update. 2009;15:423–40.
Jackson LW, Schisterman EF, Dey-Rao R, Browne R, Armstrong D. Oxidative stress and endometriosis. Hum Reprod. 2005;20:2014–20.
Jana SK, Dutta M, Joshi M, Srivastava S, Chakravarty B, Chaudhury K. 1H NMR based targeted metabolite profiling for understanding the complex relationship connecting oxidative stress with endometriosis. Biomed Res Int. 2013;2013:1–9.
Jana S, Paul S, Swarnakar S. Curcumin as anti-endometriotic agent: implication of MMP-3 and intrinsic apoptotic pathway. Biochem Pharmacol. 2012;83:797–804.
Jefferson WN. Adult ovarian function can be affected by high levels of soy. J Nutr. 2010;140:2322–5.
Jefferson WN, Doerge D, Padilla-Banks E, Woodling KA, Kissling GE, Newbold R. Oral exposure to genistin, the glycosylated form of genistein, during neonatal life adversely affects the female reproductive system. Environ Health Perspect. 2009;117:1883–9.
Johnson LJ, Meacham SL, Kruskall LJ. The antioxidants--vitamin C, vitamin E, selenium, and carotenoids. J Agromedicine. 2003;9:65–82.
Karowicz-Bilinska A, Plodzidym M, Krol J, Lewinska A, Bartosz G. Changes of markers of oxidative stress during menstrual cycle. Redox Rep. 2008;13:237–40.
Kavtaradze N, Domiguez CE, Rock JA, Partasarathy S, Murphy AA. Vitamin E and C supplementation reduces endometriosis related pelvic pain. Fertil Steril. 2003;80:S221–2.
Kim J, Kim S, Huh K, Kim Y, Joung H, Park M. High serum isoflavone concentrations are associated with the risk of precocious puberty in Korean girls. Clin Endocrinol (Oxf). 2011;75:831–5.
Kim SH, Park MJ. Effects of phytoestrogen on sexual development. Korean J Pediatr. 2012;55:265–71.
Kissinger DG, Sanchez A. The association of dietary factors with the age of menarche. Nutr Res. 1987;7:471–9.
Koçak I, Aksoy E, Ustün C. Recurrent spontaneous abortion and selenium deficiency. Int J Gynaecol Obstet. 1999;6:79–80.
Kumar KS, Kumar A, Prakash S, Swamy K, Jagadeesan V, Jyothy A. Role of red cell selenium in recurrent pregnancy loss. J Gynaecol Obstet. 2002;22:181–3.
Lukienko PI, Mel’nichenko NG, Zverinskii IV, Zabrodskaya SV. Antioxidant properties of thiamine. Bull Exp Biol Med. 2000;130:874–6.
Maclure M, Travis LB, Willett W, MacMahon B. A prospective cohort study of nutrient intake and age at menarche. Am J Clin Nutr. 1991;54:649–56.
Mehendale SS, Kilari Bams AS, Deshmukh CS, Dhorepatil BS, Nimbargi VN, Joshi SR. Oxidative stress-mediated essential polyunsaturated fatty acid alterations in female infertility. Hum Fertil. 2009;12:28–33.
Michos C, Kiortsis DN, Evangelou A, Karkabounas S. Antioxidant protection during the menstrual cycle: the effects of estradiol on ascorbic-dehydroascorbic acid plasma levels and total antioxidant plasma status in eumenorrhoic women during the menstrual cycle. Acta Obstet Gynecol Scand. 2006;85:960–5.
Mier-Cabrera J, Genera-García M, De la Jara-Díaz J, Perichart-Perera O, Vadillo-Ortega F, Hernández-Guerrero C. Effect of vitamins C and E supplementation on peripheral oxidative stress markers and pregnancy rate in women with endometriosis. Int J Gynecol Obstet. 2008;100:252–6.
Mistry HD, Williams PJ. The importance of antioxidant micronutrients in pregnancy. Oxid Med Cell Longev. 2011;2011:841749.
Mistry HD, Broughton Pipkin F, Redman CW, Poston L. Selenium in reproductive health. Am J Obstet Gynecol. 2012;206:21–30.
Moisan J, Meyer F, Gingras S. A nested case-control study of the correlates of early menarche. Am J Epidemiol. 1990;132:953–61.
Mortensen A, Kulling SE, Schwartz H, Rowland I, Ruefer CE, Rimbach G, Cassidy A, et al. Analytical and compositional aspects of isoflavones in food and their biological effects. Mol Nutr Food Res. 2009;53:S266–309.
Negi R, Pande D, Kumar A, Khanna RS, Khanna HD. Evaluation of biomarkers of oxidative stress and antioxidant capacity in the cord blood of preterm low birth weight neonates. J Matern Fetal Neonatal Med. 2012;25:1338–41.
Nicoll AE, Norman J, Macpherson A, Acharya U. Association of reduced selenium status in the aetiology of recurrent miscarriage. Br J Obstet Gynaecol. 1999;106:1188–91.
Ngô C, Chéreau C, Nicco C, Weill B, Chapron C, Batteux F. Reactive oxygen species controls endometriosis progression. Am J Pathol. 2009;175:225–34.
Paszkowski T, Traub AI, Robinson SY, McMaster D. Selenium dependent glutathione peroxidase activity in human follicular fluid. Clin Chim Acta. 1995;236:173–80.
Patisaul HB, Jefferson W. The pros and cons of phytoestrogens. Front Neuroendocrinol. 2010;31:400–19.
Pejić SA, Kasapović JD, Todorović AU, Stojiljković VR, Gavrilović LV, Popović NM, Pajović SB. Antioxidant enzymes in women with endometrial polyps: relation with sex hormones. Eur J Obstet Gynecol Reprod Biol. 2013;170:241–6.
Pierce R, Hardy M. Commentary: the decreasing age of puberty - as much a psychosocial as biological problem? Int J Epidemiol. 2012;41:300.
Prieto L, Quesada JF, Cambero O, Pacheco A, Pellicer A, Codoceo R, Garcia-Velasco JA. Analysis of follicular fluid and serum markers of oxidative stress in women with infertility related to endometriosis. Fertil Steril. 2012;98:126–30.
Rahman K. Studies on free radicals, antioxidants, and co-factors. Clin Interv Aging. 2007;2:219–36.
Ramakrishnan U, Grant F, Goldenberg T, Zongrone A, Martorell R. Effect of women’s nutrition before and during early pregnancy on maternal and infant outcomes: a systematic review. Paediatr Perinat Epidemiol. 2012;26(Suppl 1):285–301.
Reindollar RH, Regan MM, Neumann PJ, Levine B, Thornton KL, Alper MM, Goldman MB. A randomized clinical trial to evaluate optimal treatment for unexplained infertility: the fast track and standard treatment (FASTT) trial. Fertil Steril. 2010;94:888–99.
Rock CL, Jacob RA, Bowen PE. Update on the biological characteristics of the antioxidant micronutrients: vitamin C, vitamin E and the carotenoids. J Am Diet Assoc. 1996;96:693–702.
Rogers IS, Northstone K, Dunger DB, Cooper AR, Ness AR, Emmett PM. Diet throughout childhood and age at menarche in a contemporary cohort of British girls. Public Health Nutr. 2010;13:2052–63.
Ruder EH, Hartman TJ, Blumberg J, Goldman MB. Oxidative stress and antioxidants: exposure and impact on female fertility. Hum Reprod Update. 2008;14:345–57.
Ruder EH, Hartman TJ, Reindollar RH, Goldman MB. Female dietary antioxidant intake and time to pregnancy among couples treated for unexplained infertility. Fertil Steril. 2014;101:759–66.
Rudzitis-Auth J, Menger MD, Laschke MW. Resveratrol is a potent inhibitor of vascularization and cell proliferation in experimental endometriosis. Hum Reprod. 2013;28:1339–47.
Santulli P, Borghese B, Lemarechal H, Leconte M, Millischer A, Batteux F, et al. Increased serum oxidative stress markers in women with uterine leiomyoma. PLoS One. 2013;8:72069.
Sekhon LH, Gupta S, Kim Y, Agarwal A. Female infertility and antioxidants. Curr Wom Health Rev. 2010;6:84–95.
Shahin AY, Ismail AM, Zahran KM, Makhlouf AM. Adding phytoestrogens to clomiphene induction in unexplained infertility patients - a randomized trial. Reprod Biomed Online. 2008;16:580–8.
Şimşek M, Naziroǧlu M, Şimşek H, Çay M, Aksakal M, Kumru S. Blood plasma levels of lipoperoxides, glutathione peroxidase, beta carotene, vitamin A and E in women with habitual abortion. Cell Biochem Funct. 1998;16:227–31.
Sugino N. The role of oxygen radical-mediated signaling pathways in endometrial function. Placenta. 2007;28:133–6.
Tamura H, Takasaki A, Miwa I, Taniguchi K, Maekawa R, Asada H, Taketani T, Matsuoka A, Yamagata Y, Shimamura K, Morioka H, Ishikawa H, Reiter RJ, Sugino N. Oxidative stress impairs oocyte quality and melatonin protects oocytes from free radical damage and improves fertilization rate. J Pineal Res. 2008;44:280–7.
Tamura H, Nakamura Y, Korkmaz A, Manchester LC, Tan DX, Sugino N, Reiter RJ. Melatonin and the ovary: physiological and pathophysiological implications. Fertil Steril. 2009;92:328–43.
Tamura H, Takasaki A, Taketani T, Tanabe M, Kizuka F, Lee L, Tamura I, Maekawa R, Aasada H, Yamagata Y, Sugino N. The role of melatonin as an antioxidant in the follicle. J Ovarian Res. 2012;5:5.
Twigt JM, Bolhuis ME, Steegers EA, Hammiche F, van Inzen WG, Laven JS, Steegers-Theunissen RP. The preconception diet is associated with the chance of ongoing pregnancy in women undergoing IVF/ICSI treatment. Hum Reprod. 2012;27:2526–31.
Unfer V, Casini ML, Costibile M, Mignosa S, Gerli S, Di Renzo GC. Endometrial effects of long term treatment with phytoestrogens: a randomized, double-blind, placebo-controlled study. Fertil Steril. 2004a;82:145–8.
Unfer V, Casini ML, Gerli S, Costabile L, Mignosa M, DiRenzo GC. Phytoestrogens may improve the pregnancy rate in in vitro fertilization - embryo transfer cycles: a prospective, controlled, randomized trial. Fertil Steril. 2004b;82:1509–13.
Weber P, Bendich A, Schalch W. Vitamin C and human health - a review of recent data relevant to human requirements. Int J Vit. Nutr Res. 1996;66:19–30.
Ziaei S, Faghihzadeh S, Sohrabvand F, Lamyian M, Ememgholy T. A randomized placebo-controlled trial to determine the efficacy of vitamin E in treatment of primary dysmenorrhea. Br J Obstet Gynaecol. 2001;108:1181–3.
Ziaei S, Zakeri M, Kazemnejad A. A randomized controlled trial of vitamin E in the treatment of primary dysmenorrhea. Br J Obstet Gynaecol. 2005;112:466–9.
Zung A, Glaser T, Kerem Z, Zadik Z. Breast development in the first 2 years of life: an association with soy-based infant formulas. J Pediatr Gastroenterol Nutr. 2008;46:191–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Darché, R.L., Ruder, E.H., Blumberg, J., Hartman, T.J., Goldman, M.B. (2017). Antioxidants in Reproductive Health and Fertility. In: Al-Gubory, K., Laher, I. (eds) Nutritional Antioxidant Therapies: Treatments and Perspectives. Springer, Cham. https://doi.org/10.1007/978-3-319-67625-8_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-67625-8_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-67623-4
Online ISBN: 978-3-319-67625-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)