Abstract
Glioblastoma (GBM) is the most common and deadly primary brain cancer. Patients diagnosed with GBM have a mean survival time of only 21 months, despite an intense push over the past several decades to dissect underlying mechanisms and develop new therapies. Whereas discovery efforts related to GBM have traditionally focused on cell-intrinsic factors, such as genetic and epigenetic lesions, it has more recently become clear that cell-extrinsic factors within the tumor microenvironment play important pathogenic roles as well. More surprisingly, physical aspects of the microenvironment, including tissue structure and mechanics, can regulate signaling events that contribute to dysplasia, invasion, and metastasis. This chapter will describe the basic biology of physical microenvironmental regulation of the GBM, with a focus on the extracellular matrix. We will also describe how components of the physical microenvironment can be recapitulated using biomaterials technology and how these new platforms can contribute to next-generation culture systems for discovery and screening.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
5.1 Introduction
Glioblastoma (GBM) is the most common primary brain cancer, accounting for approximately 54% of all the brain tumors in the United States (Agnihotri et al. 2013). In addition to its high prevalence, GBM is also the most aggressive and lethal brain cancer, leading to death an average of 21 months from the time of diagnosis. Unfortunately given the severity of the diagnosis, there is currently no definitive treatment for patients afflicted with this disease. This is often attributed to the diffuse nature of the tumor, in which a primary tumor spreads outward from its point of origin, causing tumor cells to occupy large tracts of brain tissue, making complete surgical resection impractical if not impossible in most cases (Louis et al. 2007). This feature of GBM has long been observed and recognized as a critical bottleneck to successful therapy. It was most poignantly demonstrated by the neurosurgeon Dr. Walter Dandy in the 1920s, when he took the extreme step of removing an entire hemisphere of a brain affected with GBM in comatose patients only to see the tumor return post-resection (Dandy 1928).
The standard treatment of primary GBM consists of an intensive combination of surgical resection, radiotherapy, and a variety of traditional and directed chemotherapies (most notably, temozolomide) in an effort to ablate the tumor and prevent recurrence. Even given this extreme course of treatment, tumor recurrence occurs in approximately 90% of patients (Stupp et al. 2005; Berens and Giese 1999). The failure of current treatments is increasingly attributed to the cellular, genetic, and molecular heterogeneity of GBM tumors that appear similarly in clinical and histopathological presentation. This implies that GBM is not a single, unified disease but instead a collection of a few, if not many, distinct diseases that share clinical features. A comprehensive transcriptomic analysis from the Cancer Genome Atlas has led to a classification scheme involving four distinct genetic subtypes of GBM: classical, mesenchymal, proneural, and neural (McLendon et al. 2008; Verhaak et al. 2010). In addition to the genetic variability between patients in different tumors, there is also substantial intratumor heterogeneity, as exemplified by the emerging paradigm that tumor progression is driven by a potentially rare subset of “tumor initiating cells” (a.k.a. cancer stem cells) that share many of the genetic and phenotypic hallmarks of neural stem cells (Altaner 2008). Adding to this complexity, cells can transdifferentiate, spontaneously or under the influence of specific differentiation drivers, to pro-tumorigenic cell types. For example, tumor cells have been observed to transdifferentiate into endothelial cells and compete with host endothelial cells to populate tumor vasculature (Soda et al. 2011). Because GBMs represent myriad and unique genetic and molecular configurations, conventional treatments targeting aberrant genes or signaling pathways would only be expected to influence the subset of cells that fit the genetic framework targeted by the drug. Furthermore, recent high-resolution in vivo imaging efforts have suggested that GBM tumor cells can physically connect and exchange material over very long distances with membrane microtubes, the presence of which correlates with radioresistance. Thus, GBMs may represent an “organ within an organ” capable of a coordinated response to therapy (Osswald et al. 2015).
Given the spatial and temporal complexity of GBM, scientists have been increasingly searching for clinical targets that are shared by large percentages of GBM subtypes. Instead of focusing on intracellular signaling targets, new drugs aim to manipulate the extracellular environment as a means to harness cells even with substantial genetic, epigenetic, and molecular abnormalities. These extracellular regulatory components, collectively known as the microenvironment, include the extracellular matrix (ECM), stromal and other nontumor cells near or within the tumor, and soluble and ECM-bound signals. In particular, targeting the contributions of the physical microenvironment, such as normalizing the mechanical properties of tumor cells and their environment, has drawn considerable interest as a therapeutic target. In the next few paragraphs, we will describe how each of these components regulates GBM progression (reviewed extensively in Charles et al. 2011; Payne and Huang 2013; Ulrich and Kumar 2011).
5.2 The Role of the Microenvironment in GBM Malignancy
5.2.1 ECM
Conventionally thought to serve as simply a passive scaffold to hold tumor and tumor-associated cells in the proper location and orientation, an extensive body of research has made it clear that the ECM can actively drive tumor progression in most tumor types, especially in GBM. Aberrations in both the ECM components of the microenvironment and of cellular receptors can both contribute to this phenomenon. The most abundant component of the ECM in the brain is the polysaccharide hyaluronic acid (HA), a glycosaminoglycan made up of repeating units of d-glucuronic acid and N-acetyl-d-glucosamine (Laurent and Fraser 1992; Toole 2004). The overproduction of HA, which is observed in most GBM tumors, is associated with cell proliferation and diffuse invasion away from the primary tumor. Despite the common association of HA overproduction with GBM, it remains unclear whether HA differentially regulates the various GBM subtypes or how this additional HA interacts with tumor/stromal cell-derived matrix to promote invasion. Cells engage HA through a set of transmembrane receptors including CD44, whose overabundance is also associated with cell invasion and growth (Delpech et al. 1993; Wiranowska et al. 2010; Ariza et al. 1995). CD44 expression is enriched at the tumor margin, suggesting that CD44 may facilitate adhesion to HA within normal brain parenchyma. In addition to its implied role in cell migration, CD44-HA ligation enhances pro-tumorigenic signaling inside tumor cells such as through the Rho family of small GTPases and PI3 kinase, which affect cell motility and proliferation, respectively (Herishanu et al. 2011). CD44 engagement of osteopontin, a matrix sialoprotein, was recently shown to induce cleavage of CD44 and trafficking of the intracellular domain to the nucleus, where it triggers tumor stem cell-like behaviors (Pietras et al. 2014).
Although HA is the most abundant ECM constituent around tumor cells, there are many other ECM molecules present in the GBM microenvironment. Particularly consequential to tumor development is the presence of tumor-associated vasculature and its specific associated microenvironment, which contains collagen IV, collagen V, fibronectin, and laminin (Giese and Westphal 1996; Knott et al. 1998; Tysnes et al. 1999). These molecules have extensively been demonstrated to enhance motility, proliferation, and survival, both in vitro and in vivo, suggesting that the presence of vasculature in and around tumors enhances tumor progression not only by providing key nutrients to the cells but also by providing structural and insoluble signaling to tumor cells (Demuth and Berens 2004; Kaufman et al. 2005; Kawataki et al. 2007; Lathia et al. 2012).
In addition to presenting biochemical cues that enhance GBM progression, the ECM also encodes structural and mechanical cues that can promote tumor progression. Cells mechanically engage their environment and respond to microenvironmental forces using a suite of molecular mechanisms whose actions are collectively known as mechanosensing and mechanotransduction (Discher et al. 2005). In order to probe the mechanical properties of its environment, a cell must actively apply a deformation force to the matrix. Canonically, cells generate force via contraction of the actin-myosin cytoskeleton, which is then transmitted to ECM proteins, such as fibronectin or collagen, through adhesive complexes containing integrins (e.g., focal adhesions) that physically connect the ECM to the cytoskeleton. These adhesive complexes then respond to stress/strain generated across the adhesive complex and activate downstream signaling pathways that result in changes of focal adhesion size and composition, force generation, and the regulation of gene transcription (Oakes et al. 2012; Kolega et al. 1991; Chang and Kumar 2013; Geiger and Bershadsky 2001; Solon et al. 2007; Pelham and Wang 1997; Maniotis et al. 1997).
Clinical observations and molecular profiling support the hypothesis that tissue stiffness and the corresponding mechanosensitive machinery are critical for the progression of a variety of solid tumors, including GBM. Ultrasound imaging of strain magnitudes during GBM resection suggests that the margins of GBM tumors are substantially stiffer than the adjacent normal tissue, although it is unclear whether the increase in stiffness is the result of a change in the abundance, type, or cross-linking of ECM components. Additionally, the direct mechanism through which this may contribute to tumor progression remains to be extensively detailed in GBM (Selbekk et al. 2010). Another intriguing clinical observation is that tumor cells often diffusely migrate along structures in the brain that are intrinsically stiff, such as the basolateral membrane of tumor-associated blood vessels and white matter tracts, known collectively as the structures of Scherer (Scherer 1938, 1940). This observation suggests that the mechanical environment may provide efficient “highways” that direct the cells to migrate away from the primary tumor.
GBM cells also display distinct molecular aberrations suggesting that they may co-opt and alter their mechanosensing machinery as a means of enhancing their malignancy. For example, a critical and nodal mechanosensitive protein, focal adhesion kinase (FAK), is often overexpressed and mutated in GBM, which results in enhanced signaling in many pro-growth pathways (Rutka et al. 1999). Aberrant signaling and regulation of many other mechanosensitive proteins has also been observed in GBM, further demonstrating how GBM cells co-opt normal mechanosensing processes (Belot et al. 2001; Friedlander et al. 1996; Paulus et al. 1993).
Given the extensive changes to the ECM, mechanosensitive machinery, and clinical observations, it is clear that the regulation of the ECM-cell interaction is substantially dysregulated in GBM and actively contributes to tumor progression. Therefore, the composition and mechanical properties of the ECM may represent an integrative target for effective therapeutics.
5.3 Engineering Advanced Models of the GBM Microenvironment
The past decade has seen a dramatic expansion of in vivo models of GBM, including genetically engineered mouse models (Huse and Holland 2009) and patient-derived xenograft models (Tentler et al. 2012), and these platforms have contributed to mechanistic studies of GBM progression as well as preclinical evaluation of therapies. However, the complexity, expense, and limited throughput associated with these models make them impractical as a first-line platform for discovery and screening. At the same time, it is widely acknowledged that the traditional in vitro approach of culturing cells on glass or plastic surfaces in high concentrations of soluble growth factors omits key elements of the tumor microenvironment. This gap has created a need for next-generation culture technologies that retain the scalability and parallelization of traditional culture approaches while incorporating the complexities of the in vivo microenvironment. Recognizing an opportunity to address these needs, investigators are increasingly leveraging the tools of biomaterials science and microfabrication to create these new culture platforms.
5.3.1 Traditional Culture Systems
Two-dimensional (2D) culture systems have historically been the workhorse of in vitro systems for reductionist cell biology, including the study of ECM regulation of GBM. In this context, 2D culture systems generally consist of glass or plastic surfaces coated with a thin layer of ECM protein, proteoglycan, or reconstituted matrix preparation (e.g., Matrigel; see discussion below) to support cell adhesion. These systems greatly facilitate optical imaging and the recovery of cellular material for downstream analysis (e.g., Western blot, RT-PCR, RNA-seq, etc.). These straightforward approaches have established a critical foundation for the field’s understanding of many aspects of ECM regulation of GBM, including the roles of specific matrix components (fibronectin, vitronectin, and HA) and matrix metalloproteases (Giese et al. 1995; Koochekpour et al. 1995; Belien et al. 1999). However, the simplicity, ease of use, and experimental accessibility of these 2D cell culture systems also create a major drawback; it has become increasingly recognized that cells in three-dimensional (3D) systems behave quite differently than cells in 2D culture (Griffith and Schwartz 2006; Yamada and Cukierman 2007). In fact, the differences in presentation, organization, and polarity of ECM proteins in a 3D matrix can cause cells to respond to ECM cues in ways that would be impossible to predict from their responses to the same proteins on 2D monolayers. This was first demonstrated in pioneering studies in which the behavior of malignant breast cancer cells could be normalized simply by placing them in a 3D microenvironment (Weaver et al. 1997). Additionally, the stiffness of conventional culture dishes is many orders of magnitude above what is typically experienced by cells in vivo, which can disrupt normal tissue morphogenesis and amplify pro-oncogenic signaling (Elkin et al. 2007; Paszek et al. 2005). To overcome this limitation, researchers have begun to exploit advances in polymer science and engineering to develop systems that enable precise control of the physical and chemical properties of the extracellular environment while maintaining ease of use for conventional biological analysis. These systems offer researchers unparalleled insight into the mechanisms underlying GBM-ECM interactions.
5.3.2 Polymer-Based 3D Matrices
The use of native, biologically derived hydrogels was the next iteration in developing highly controlled GBM ECM mimics. These biopolymers, including HA, collagen I, and Matrigel—a laminin-rich ECM extracted from mouse sarcomas—are derived from living sources, purified, and then reconstituted in vivo. These systems have been used to study the mechanics of GBM growth and invasion. For example, U87 MG glioma spheroids grown in 3D Matrigel plugs exert both traction forces on the gel as cells radially invade and compressive forces as the spheroid expands (Gordon et al. 2003). Further studies including expanded cell lines and GBM models and more expansive matrix choices for 3D culture showed that the 3D matrix often presents multiple levels of feedback controlling tumor growth and invasion. Yang et al. modified collagen network architecture by specifically controlling collagen gelation temperature, finding that pore size is a key determinant of glioma invasive speed (Yang et al. 2010). It is rather impractical to decouple many of these variables using reconstituted matrices; therefore intensive efforts have been directed to developing matrices that offer more flexibility, control, and experiment-to-experiment repeatability. The adaptation of synthetic polymers for use as cell culture models has provided impressive customization and repeatability for specific cell culture properties (as previously reviewed in Seliktar 2012; Lutolf and Hubbell 2005).
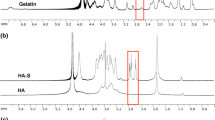
Using purely reconstituted matrices in the study of GBM is further complicated by the unique geometry of the brain GBM, which largely lacks the 3D fibrillar architecture observed in most other connective tissue ECMs (Thorne and Nicholson 2006). Our laboratory has taken an active interest in developing 3D matrices that mimic the unique architecture of the GBM-ECM by adopting an approach that merges the use of biologically derived hydrogels and synthetic hydrogels. In this system, HA is functionalized with methacrylate groups, which can be covalently conjugated to macromolecules functionalized with thiol groups via Michael addition chemistry. In our initial study with this system, we functionalized the matrix with a cysteine-terminated peptide containing the cell-adhesive RGD sequence and then cross-linked the HA backbone with dithiothreitol, which contains two thiol groups. This dual functionalization approach offered us independent control of cell-adhesive ligand density and stiffness over more than three orders of magnitude (Ananthanarayanan et al. 2011). Importantly, this matrix exhibited small-pore structures devoid of fibrils, similar to the architecture of native brain tissue. In addition to replicating the structural environment of GBM, this system contains many chemical components of the pathological GBM environment, including the presence of both the CD44 and RGD ligands that arise in the tumor from the overproduction of HA and fibronectin, principally. Using this system, we found that increasing the stiffness of the 3D matrix inhibited tumor spheroid invasion into the surrounding matrix when cell attachment to the matrix is primarily through integrin-RGD interactions or HA-CD44 interactions, suggesting that this platform may hold potential as a reductionist in vitro system for studying mechanisms that underlie GBM-ECM interactions that lead to enhanced tumorigenesis (Kim and Kumar 2014).
5.3.3 Microfabricated Platforms
Researchers have begun to adopt and leverage techniques initially developed to help reduce the size of transistors, most notably soft lithography, microfluidics, and light-based patterning, to improve the spatial precision with which mechanical and biochemical cues can be presented to cells (Khademhosseini et al. 2006; Ross et al. 2012; Polacheck et al. 2013). While these approaches do not, in general, allow true 3D encapsulation of cells, they are massively parallelizable and enable the creation of microenvironments that can be engineered on the length scale of a single cell (10 nm–10 μm). One of the first studies to investigate how microtopography can influence GBM behavior was performed by Zhu and colleagues, who used laser irradiation to create periodic ridges spaced a few hundred nanometers apart and reported that C6 rat glioma cells aligned parallel to the direction of the grooves (Zhu et al. 2004). Subsequent studies suggested that cells not only align parallel to grooves in a surface but also migrate persistently parallel to the groove, a physical guidance mechanism that may partially explain GBM’s preference to migrate along preformed structures in the brain architecture (Gallego-Perez et al. 2012). Our laboratory has expanded upon these studies by developing 3D confinement structures made of polyacrylamide that present cells with topographical guidance cues within a 3D environment. Using these microfabricated devices, we found that topographical migration, as observed in 2D systems, is present in 3D confinement channels and that narrow channels increase persistent migration regardless of the stiffness of the surrounding matrix (Fig. 5.1, Pathak and Kumar 2012). Our recent work studying the microchannel migration of breast cancer cells overexpressing the oncogene ErbB2 suggests that the physical microenvironment and oncogenic transformation can contribute to malignancy in an integrative manner (Pathak and Kumar 2013).
Orthogonal regulation of GBM cell motility by ECM stiffness and topographical confinement. The migration of U373-MG cells was studied using polyacrylamide-based microfabricated channels coated with fibronectin. Channel width, c w, and wall stiffness, E, were varied independently. Confinement in narrow channels increased migration speed for all values of wall stiffness (a) and relieved the inhibitory effect of high stiffness (b). Phase contrast images of the migrating cells are shown in (c). Figure adapted from Pathak and Kumar (2012), with permission
5.3.4 Molecular Discovery and Screening
While the sophistication of approaches for recapitulating and controlling the GBM microenvironment continues to improve rapidly, the field still lacks the ability to interrogate large parameter spaces, in which hundreds, or even thousands, of different parameter combinations can be tested systematically and simultaneously. This capability is critical because multiple parameters may interact in ways to influence cell behavior that are impossible to predict from results of studies in which only one variable is modulated in isolation (Engler et al. 2004). Dissecting this nonlinear integration by cells of multiple simultaneous inputs represents a grand challenge in understanding ECM regulation of cancer biology.
The robotic spotting of ECM proteins has emerged as a highly useful, versatile, and high-throughput means to test the effects of ECM on cells. In this method, an array of microneedles is “inked” in an ECM protein and is robotically controlled to stamp the protein in a specific location on a target substrate. This process can be applied sequentially, and given the extremely precise control over the stamping location, different proteins, can be applied to thousands of independent spots (Fernandes et al. 2009). In this manner, an extremely high-throughput culture surface can be created that varies multiple parameters simultaneously. In one pilot study using this technology, Alberti et al. found that specific, but highly unpredictable, combinations of collagens I, II, and IV, laminin, and fibronectin controlled embryonic stem cell differentiation (Alberti et al. 2008). Similarly, ligand type and substrate stiffness can be varied using a robotic spotter attached to a UV light to initiate photopolymerization of a hydrogel precursor, with one study screening 17,000 distinct combinations of stiffness and ligand in one experiment (Anderson et al. 2004; Nakajima et al. 2007). Intriguingly, the photopolymerization used to create hydrogels in this experiment has micron-level resolution, allowing for the high-throughput investigation of mechanical inputs on a length scale smaller than that of a cell, an area of much needed investigation.
While these experiments offer unprecedented experimental power, they still require expensive and highly specialized instrumentation. As an alternative approach, we have developed a high-throughput system that can vary substrate stiffness and ligand orthogonally while maintaining ease of use and accessibility for investigators with standard biological and microfabrication capabilities. Our technique relies on the use of light to initiate orthogonal chemistries that can be leveraged to attach an ECM protein of choice and vary the mechanical properties of a gel (Rape et al. 2015). This system is based on HA, which has been modified to allow for specific light-based polymerization and functional group uncaging. Using the parallelization provided by the platform, we were able to condense experiments that would typically require hundreds of independent hydrogels onto a single substrate. We used this system to study the expression of the oncogenic microRNA, miR18a, in GBM cells and found that the microRNA is nonlinearly regulated by both stiffness and ECM in highly unpredictable ways (Fig. 5.2). While this pilot study was conducted as a 2D experiment, the platform could potentially be extended to more complex situations such as 3D geometries, as the specific chemistries used to perform the patterning are amenable to two-photon patterning, a highly precise means to locally control chemical processes in 3D matrices.
ECM-sensitive regulation of mir18a using dual gradient-patterned hydrogels. U373-MG cells were incubated with probes for mir18a for 16 h on HA-based hydrogels, and mir18a expression was quantified based on the fluorescent signals of individual cells. Mir18a expression was quantified for 16 unique matrix stiffness ligand combinations (a). Iso-fibronectin curves (light red to dark red equals low fibronectin to high fibronectin) show that substrate stiffness regulated miR18a expression at all fibronectin densities tested (b). Similarly, iso-stiffness curves (light blue to dark blue equals low stiffness to high stiffness) show that fibronectin density only regulates miR18a expression at high stiffness (c). Figure adapted from Rape et al. (2015), with permission
5.4 Future Directions
The use of engineered microenvironments is catalyzing a revolution in the understanding of how GBM cells interact with their environment and how these interactions lead to malignancy. This profound innovation, however, is only the beginning of a trajectory that promises to simplify, expedite, and increase the efficiency of the drug discovery process. Such efforts range from the identification of new therapeutic targets to streamlining the drug development pipeline, analogous to the current development organ-on-a-chip platforms for drug screening in other human tissues, including the heart and lungs (Huh et al. 2010; Mathur et al. 2015). To achieve this broad vision, a number of key barriers must be overcome.
First, the ability to simultaneously control multiple environmental parameters within a single, unified 3D space needs to be developed. Our own work illustrates the utility of photochemistry to create microenvironments with defined physical properties. Other labs are developing more sophisticated and customizable light-based chemistries, including the adoption of “click” chemistry for biological applications (DeForest et al. 2009). A next challenge will be to pattern multiple cell types at specific positions within these devices. Recent work has suggested that affixing DNA-based affinity tags to the cell surface may provide a useful way to organize large numbers of cells in a highly precise manner through DNA hybridization (Todhunter et al. 2015). The use of 3D printing to deposit cells selectively in three dimensions also holds great promise for this purpose (Murphy and Atala 2014). Perhaps the final hurdle to clear in developing a fully functional GBM mimic is vascularization of the tissue, which has historically been a challenge in tissue engineering due to difficulties in recapitulating complex cellular architectures (e.g., endothelial cells vs. pericytes vs. smooth muscle cells), delivering oxygen and nutrients, and integrating vasculature over culture-wide length scales. In GBM, the challenge is compounded by the fact that tumor vasculature is often structurally and functionally aberrant relative to host vasculature. New cell- and matrix-patterning technologies, when paired together with strategies to release provascular growth factors, should help accelerate progress in this area (Moon and West 2008).
Once developed sufficiently, GBM-mimetic culture systems could be combined with other reverse-engineered systems of the tumor microenvironment, perhaps leading to a sort of “tumor on a chip.” The successful development of these and related technologies may immensely increase the speed and efficiency of the drug discovery process by bridging the gap between the culture plate and the animal model.
5.5 Conclusions
The physical components of the ECM microenvironment of GBM make up a complex system that contains many signals that contribute to tumor promotion and malignancy. Using the tools of chemistry, materials science, and microfabrication, researchers have developed sophisticated reductionist platforms that enable the direct interrogation of the biophysical interactions that lead to GBM progression. The further development of a truly mimetic tumor microenvironment will lead to not only a greater understanding of disease mechanisms but also yield platforms that facilitate high-throughput drug discovery and validation.
References
Agnihotri S, Burrell KE, Wolf A et al (2013) Glioblastoma, a brief review of history, molecular genetics, animal models and novel therapeutic strategies. Arch Immunol Ther Exp (Warsz) 61:25–41
Alberti K, Davey RE, Onishi K et al (2008) Functional immobilization of signaling proteins enables control of stem cell fate. Nat Methods 5:645–650
Altaner C (2008) Glioblastoma and stem cells. Neoplasma 55:369–374
Ananthanarayanan B, Kim Y, Kumar S (2011) Elucidating the mechanobiology of malignant brain tumors using a brain matrix-mimetic hyaluronic acid hydrogel platform. Biomaterials 32:7913–7923
Anderson DG, Levenberg S, Langer R (2004) Nanoliter-scale synthesis of arrayed biomaterials and application to human embryonic stem cells. Nat Biotechnol 22:863–866
Ariza A, López D, Mate JL et al (1995) Role of CD44 in the invasiveness of glioblastoma multiforme and the noninvasiveness of meningioma: an immunohistochemistry study. Hum Pathol 26:1144–1147
Belien ATJ, Paganetti PA, Schwab ME (1999) Membrane-type 1 matrix metalloprotease (MT1-MMP) enables invasive migration of glioma cells in central nervous system white matter. J Cell Biol 144:373–384
Belot N, Rorive S, Doyen I et al (2001) Molecular characterization of cell substratum attachments in human glial tumors relates to prognostic features. Glia 36:375–390
Berens ME, Giese A (1999) “…those left behind.” Biology and oncology of invasive glioma cells. Neoplasia 1:208–219
Chang C-W, Kumar S (2013) Vinculin tension distributions of individual stress fibers within cell–matrix adhesions. J Cell Sci 126:3021–3030
Charles NA, Holland EC, Gilbertson R et al (2011) The brain tumor microenvironment. Glia 59:1169–1180
Dandy WE (1928) Removal of right cerebral hemisphere for certain tumors with hemiplegia: preliminary report. JAMA 90:823–825
Deforest CA, Polizzoti BD, Anseth KS (2009) Sequential click reactions for synthesizing and patterning three-dimensional cell microenvironments. Nat Mater 8:659–664
Delpech B, Maingonnat C, Girard N et al (1993) Hyaluronan and hyaluronectin in the extracellular matrix of human brain tumour stroma. Eur J Cancer 29A:1012–1017
Demuth T, Berens ME (2004) Molecular mechanisms of glioma cell migration and invasion. J Neurooncol 70:217–228
Discher DE, Janmey P, Wang Y (2005) Tissue cells feel and respond to the stiffness of their substrate. Science 310:1139–1143
Elkin BS, Azeloglu EU, Costa KD et al (2007) Mechanical heterogeneity of the rat hippocampus measured by atomic force microscope indentation. J Neurotrauma 24:812–822
Engler A, Bacakova L, Newman C et al (2004) Substrate compliance versus ligand density in cell on gel responses. Biophys J 86:617–628
Fernandes TG, Diogo MM, Clark DS et al (2009) High-throughput cellular microarray platforms: applications in drug discovery, toxicology and stem cell research. Trends Biotechnol 27:342–349
Friedlander DR, Zagzag D, Shiff B et al (1996) Migration of brain tumor cells on extracellular matrix proteins in vitro correlates with tumor type and grade and involves alphaV and beta1 integrins. Cancer Res 56:1939–1947
Gallego-Perez D, Higuita-Castro N, Denning L et al (2012) Microfabricated mimics of in vivo structural cues for the study of guided tumor cell migration. Lab Chip 12:4424–4432
Geiger B, Bershadsky A (2001) Assembly and mechanosensory function of focal contacts. Curr Opin Cell Biol 13:584–592
Giese A, Westphal M (1996) Glioma invasion in the central nervous system. Neurosurgery 39:235–250
Giese A, Loo MA, Rief MD et al (1995) Substrates for astrocytoma invasion. Neurosurgery 37:294–301
Gordon VD, Valentine MT, Gardel ML et al (2003) Measuring the mechanical stress induced by an expanding multicellular tumor system: a case study. Exp Cell Res 289:58–66
Griffith LG, Schwartz MA (2006) Capturing complex 3D tissue physiology in vitro. Nat Rev Mol Cell Biol 7:211–224
Herishanu Y, Gibellini F, Njuguna N et al (2011) CD44 signaling via PI3K/AKT and MAPK/ERK pathways protects CLL cells from spontaneous and drug induced apoptosis through MCL-1. Leuk Lymphoma 52:1758–1769
Huh D, Matthews BD, Mammoto A et al (2010) Reconstituting organ-level lung functions on a chip. Science 328(5986):1662–1668
Huse HT, Holland EC (2009) Genetically engineered mouse models of brain cancer and the promise of preclinical testing. Brain Pathol 19(1):132–143
Kaufman LJ, Brangwynne CP, Kasza KE et al (2005) Glioma expansion in collagen I matrices: analyzing collagen concentration-dependent growth and motility patterns. Biophys J 89:635–650
Kawataki T, Yamane T, Naganuma H et al (2007) Laminin isoforms and their integrin receptors in glioma cell migration and invasiveness: evidence for a role of alpha5-laminin(s) and alpha3beta1 integrin. Exp Cell Res 313:3819–3831
Khademhosseini A, Langer R, Borenstein J et al (2006) Microscale technologies for tissue engineering and biology. Proc Natl Acad Sci USA 103:2480–2487
Kim Y, Kumar S (2014) CD44-mediated adhesion to hyaluronic acid contributes to mechanosensing and invasive motility. Mol Cancer Res 12(10):1416–1429
Knott JC, Mahesparan R, Garcia-Cabrera I et al (1998) Stimulation of extracellular matrix components in the normal brain by invading glioma cells. Int J Cancer 75:864–872
Kolega J, Janson LW, Taylor DL (1991) The role of solation-contraction coupling in regulating stress fiber dynamics in nonmuscle cells. J Cell Biol 114:993–1003
Koochekpour S, Pilkington GJ, Merzak A (1995) Hyaluronic acid/CD44H interaction induces cell detachment and stimulates migration and invasion of human glioma cells in vitro. Int J Cancer 63:450–454
Lathia JD, Li M, Hall PE et al (2012) Laminin alpha 2 enables glioblastoma stem cell growth. Ann Neurol 72:766–778
Laurent TC, Fraser JR (1992) Hyaluronan. FASEB J 6:2397–2404
Louis DN, Ohgaki H, Wiestler OD et al (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114:97–109
Lutolf MP, Hubbell JA (2005) Synthetic biomaterials as instructive extracellular microenvironments for morphogenesis in tissue engineering. Nat Biotechnol 23:47–55
Maniotis AJ, Chen CS, Ingber DE (1997) Demonstration of mechanical connections between integrins, cytoskeletal filaments, and nucleoplasm that stabilize nuclear structure. Proc Natl Acad Sci USA 94:849–854
Mathur A, Loskill P, Shao K et al (2015) Human iPSC-based cardiac microphysiological system for drug screening applications. Sci Rep 5:8883
McLendon R, Friedman A, Bigner D et al (2008) Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455:1061–1068
Moon JJ, West JL (2008) Vascularization of engineered tissues: approaches to promote angio-genesis in biomaterials. Curr Top Med Chem 8(4):300–310
Murphy SV, Atala A (2014) 3D bioprinting of tissues and organs. Nat Biotechnol 32:773–785
Nakajima M, Ishimuro T, Kato K et al (2007) Combinatorial protein display for the cell-based screening of biomaterials that direct neural stem cell differentiation. Biomaterials 28:1048–1060
Oakes PW, Beckham Y, Stricker J et al (2012) Tension is required but not sufficient for focal adhesion maturation without a stress fiber template. J Cell Biol 196:363–374
Osswald M, Jung E, Sahm F et al (2015) Brain tumor cells interconnect to a functional and resistant network. Nature 528(7850):93–98
Paszek MJ, Zahir N, Johnson KR et al (2005) Tensional homeostasis and the malignant phenotype. Cancer Cell 8(3):241–245
Pathak A, Kumar S (2012) Independent regulation of tumor cell migration by matrix stiffness and confinement. Proc Natl Acad Sci USA 109(26):10334–10339
Pathak A, Kumar S (2013) Transforming potential and matrix stiffness co-regulate confinement sensitivity of tumor cell migration. Int Biol 5:1067–1075
Paulus W, Baur I, Schuppan D et al (1993) Characterization of integrin receptors in normal and neoplastic human brain. Am J Pathol 143:154–163
Payne LS, Huang P (2013) The pathobiology of collagens in glioma. Mol Cancer Res 11(10):1129–1140
Pelham RJ, Wang Y (1997) Cell locomotion and focal adhesions are regulated by substrate flexibility. Proc Natl Acad Sci USA 94:13661–13665
Pietras A, Katz AM, Ekstrom EJ et al (2014) Osteopontin-CD44 signaling in the glioma perivascular niche enhances cancer stem cell phenotypes and promotes aggressive tumor growth. Cell Stem Cell 14(3):357–369
Polacheck WJ, Zervantonakis IK, Kamm RD (2013) Tumor cell migration in complex microenvironments. Cell Mol Life Sci 70:1335–1356
Rape A, Zibinsky M, Murthy N, Kumar S (2015) A synthetic hydrogel for the high-throughput study of cell-ECM interactions. Nat Commun 6:8129
Ross AM, Jiang ZX, Bastmeyer M, Lahann J (2012) Physical aspects of cell culture substrates: topography, roughness, and elasticity. Small 8:336–355
Rutka JT, Muller M, Hubbard SL et al (1999) Astrocytoma adhesion to extracellular matrix: functional significance of integrin and focal adhesion kinase expression. J Neuropathol Exp Neurol 58:198–209
Scherer H (1938) Structural development in gliomas. Am J Cancer 34:333–348
Scherer HJ (1940) The forms of growth in gliomas and their practical significance. Brain 63:1–35
Selbekk T, Brekken R, Solheim O et al (2010) Tissue motion and strain in the human brain assessed by intraoperative ultrasound in glioma patients. Ultrasound Med Biol 36:2–10
Seliktar D (2012) Designing cell-compatible hydrogels for biomedical applications. Science 336:1124–1128
Soda Y, Marumoto T, Friedmann-Morvinski D, Soda M, Liu F et al (2011) Transdifferentiation of glioblastoma cells into vascular endothelial cells. Proc Natl Acad Sci USA 32(37):12950–12960
Solon J, Levental I, Sengupta K et al (2007) Fibroblast adaptation and stiffness matching to soft elastic substrates. Biophys J 93:4453–4461
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Tentler JJ, Tan AC, Weekes CD et al (2012) Patient-derived tumour xenografts as models for oncology drug development. Nat Rev Clin Oncol 9:338–350
Thorne RG, Nicholson C (2006) In vivo diffusion analysis with quantum dots and dextrans predicts the width of brain extracellular space. Proc Natl Acad Sci USA 103:5567–5572
Todhunter ME, Jee NY, Hughes AJ et al (2015) Programmed synthesis of three-dimensional tissues. Nat Methods 12:975–981
Toole BP (2004) Hyaluronan: from extracellular glue to pericellular cue. Nat Rev Cancer 4:528–539
Tysnes BB, Mahesparan R, Thorsen F et al (1999) Laminin expression by glial fibrillary acidic protein positive cells in human gliomas. Int J Dev Neurosci 17:531–539
Ulrich T, Kumar S (2011) Mechanobiology in health and disease in the central nervous system. In: Nagatomi J (ed) Mechanobiology handbook. CRC Press, Boca Raton, pp 391–411
Verhaak RGW, Hoadley KA, Purdom E et al (2010) Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 17:98–110
Weaver VM, Petersen OW, Wang F et al (1997) Reversion of the malignant phenotype of human breast cells in three-dimensional culture and in vivo by integrin blocking antibodies. J Cell Biol 137(1):231–245
Wiranowska M, Ladd S, Moscinski LC et al (2010) Modulation of hyaluronan production by CD44 positive glioma cells. Int J Cancer 127:532–542
Yamada KM, Cukierman E (2007) Modeling tissue morphogenesis and cancer in 3D. Cell 130:601–610
Yang Y, Motte S, Kaufman LJ (2010) Pore size variable type I collagen gels and their interaction with glioma cells. Biomaterials 31:5678–5688
Zhu BS, Zhang QQ, Lu QH et al (2004) Nanotopographical guidance of C6 glioma cell alignment and oriented growth. Biomaterials 25:4215–4223
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Rape, A., Kumar, S. (2017). Engineering Advanced Models of the Glioblastoma Microenvironment Using Biomaterials. In: Brekken, R., Stupack, D. (eds) Extracellular Matrix in Tumor Biology. Biology of Extracellular Matrix. Springer, Cham. https://doi.org/10.1007/978-3-319-60907-2_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-60907-2_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-60906-5
Online ISBN: 978-3-319-60907-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)