Abstract
Hematopoietic cell transplants (HCTs) have been performed for decades, and the number of both autologous and allogeneic transplants is constantly increasing. Mobilized peripheral blood (PB) hematopoietic progenitor cells (HPCs) are the most common cell source for adult patients, replacing almost completely the traditional bone marrow (BM) graft. Cryopreservation of PB HPC graft allows collecting and storing the product for later use. Cryopreservation is an essential practice for autologous products but can also be helpful for allogeneic one. The cryopreservation process itself can decrease cell viability and potency, and some of the reagents that are used to protect cells during cryopreservation can have toxic effects at thaw. Maintaining functional and viable HPCs is fundamental for HCT success. Thawing approaches of cryopreserved PB HPC should either minimize cell exposure time to toxic elements or include measures to rapidly remove them after thawing.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The use of peripheral blood (PB) as the cell source for hematopoietic cell transplant (HCT) has been steadily replacing the use of bone marrow (BM). Mobilized PB is the major source of HPC for autologous hematopoietic cell transplants (auto-HCT) and is currently being used for more than 75% of adult related and unrelated allogeneic hematopoietic cell transplants (allo-HCT) (Pasquini and Zhu 2015). The number of autologous and allogeneic transplants in the USA and worldwide is constantly increasing, and the use of PB HPCs in the allogeneic transplant setting is increasing as well, despite its higher risk of graft-versus-host disease (GvHD) compared to BM grafts. The composition of PB products is different from the traditional BM. They typically contain two- to fivefold more CD34+ progenitor cells and tenfold more T-cells. The collection by apheresis results in a relatively smaller volume with significantly lower red blood cell (RBC) volume (Snyder and Haley 2004; Kao 2009). Due to the high CD34+ content, PB products provide much faster hematological reconstitution than BM or Cord Blood (CB). Development of new pharmacologic mobilization agents allowed graft collection from patients previously unable to mobilize enough HPC, thereby increasing the potential number of total collections and transplants (Brave et al. 2010; Keating 2011).
2 Cryopreservation of Peripheral Blood Graft
The stability of fresh cellular products is time sensitive, and, if done properly, cryopreservation allows long-term storage of viable and potent HPCs. For autologous donors, cryopreservation is essential, allowing advanced collection of cells for later auto-HCT. This also allows collecting and storing enough cells for possible multiple future transplants, which is a common practice for multiple myeloma (MM) patients. The use of cryopreservation of HPC for allo-HCT is not as common. PB HPCs are collected from related or unrelated donors and are typically infused fresh, within <72 h of apheresis collection. The National Marrow Donor Program (NMDP) requires products from non-related donors to be used fresh, and any cryopreservation requires additional approval. However, cryopreservation can be a powerful tool for allogeneic products as well. Often the donor availability is limited due to the need to travel or other restrictions, or the transplant has to be delayed after the donor has already been mobilized for HPC. Additionally, any product leftovers can be stored for possible future use, thus eliminating the need to re-collect the donor, i.e., donor T lymphocytes.
To allow long-term storage, PB procured HPC products are usually cooled slowly at a controlled rate (see Chap. 6) and stored below −150 °C in a vapor phase liquid nitrogen (LN2) freezer. The most commonly used cryoprotectant is dimethyl sulfoxide (DMSO), but other molecules, such as hydroxyethyl starch (HES), are used in combination with DMSO. HES is a high-molecular-weight polymer that does not penetrate cells and is used clinically as plasma expander in hypotensive patients (Vercueil et al. 2005). It can stabilize RBC and reduce the sudden changes in osmolality that occur when thawing cryopreserved cells. Adverse events associated with HES are rare, and it was recently shown not to have an association with adverse events which were previously described (Bothner et al. 1998; Wagner et al. 2002; Pagano et al. 2016). A typical cryopreservation media comprises of an isotonic solution containing protein source, such as donor plasma or commercially available human serum albumin (HSA), and 5–10% DMSO. Prolonged storage duration was not shown to affect HPC potency, and many studies have shown that cryopreserved HPC can retain engraftment potential for more than a decade (Spurr et al. 2002; Donnenberg et al. 2002; Broxmeyer et al. 2003; Foïs et al. 2007).
3 DMSO Toxicity and Cryopreservation-Related Infusion Adverse Events
Cryopreservation can induce cell damage due to ice formation and dehydration (Mazur et al. 1972). Lovelock and Bishop described the properties and use of DMSO for cryopreservation of living cells (Lovelock and Bishop 1959). DMSO is a rapid penetrating molecule that increases the tolerance of cells to the osmotic stress induced by cryopreservation. It was originally used as an anti-inflammatory reagent but was later found to cause an array of side effects when administered to patients (Yellowlees et al. 1980; Runckel and Swanson 1980; Samoszuk et al. 1983). DMSO toxicity in HPC product infusion was shown to affect multiple organs including respiratory, cardiovascular, gastrointestinal, hepatic, and renal systems. Side effects related to infusion of thawed products are usually mild or moderate, most commonly nausea, vomiting, and hypertension. Other side effects such as abdominal cramps, chills, flushing, headaches, and diarrhea have been reported as well (Zambelli et al. 1998; Alessandrino et al. 1999; Sauer-Heilborn et al. 2004; Davis et al. 1990). Severe side effects are rare, but cardiovascular, neurological, and respiratory side effects have been reported, with some of them being severe or fatal (Windrum et al. 2005; Benekli et al. 2000; Zenhäusern et al. 2000; Rapoport et al. 1991; Hoyt et al. 2000; Dhodapkar et al. 1994; Smith et al. 1987). The rate of side effects was shown to correlate with increase in DMSO volume (Davis et al. 1990). Beside DMSO toxicity, thawed products contain cell debris, toxin, and free hemoglobin, and all of these substances can induce side effects when administered to patients.
Infusion toxicity was also shown to correlate with total nucleated cell (TNC) dose and granulocytes, which have reduced osmotic tolerance and tend to lyse releasing cytokines during cryopreservation (Foïs et al. 2007; Davis et al. 1990). RBCs lyse at thaw, and higher RBC concentration was shown to be associated with cardiac toxicity and arrhythmia (Alessandrino et al. 1999).
Besides DMSO’s toxicity to the patient, the same levels of DMSO that help maintain cells during cryopreservation can be lethal to the cells when thawed (Arakawa et al. 1990; Fahy 1986). DMSO destabilizes the phospholipid membranes at higher temperatures, increasing the membrane leakage and cell destruction (Arakawa et al. 1990; Anchordoguy et al. 1992). Therefore, thawing approaches of cryopreserved PB graft should either include steps to minimize the cell exposure time to DMSO or include measures that will remove DMSO rapidly after thaw.
4 Thawing Practices
Methods to process cryopreserved PB graft for transplantation should minimize cell loss, maintain cell viability, and prevent introduction of microbial contamination.
Thawing should be done rapidly to avoid the possibility of recrystallization of any small intracellular ice nuclei, and steps should be taken to reduce DMSO concentration to prevent potentially damaging osmotic swelling (Woods et al. 2000).
4.1 Bedside Thaw
Direct thaw and administration of a unit to the patient with no additional manipulation are the most commonly used methods for infusion of cryopreserved PB graft for adult patients. It is often called bedside thaw because it is typically performed in adjacent to the patient bedside, thus limiting the time between thaw and infusion and reducing the potential damage to the cells from DMSO exposure.
To maintain the product frozen, it is delivered in a validated container. Some centers transport the bags on dry ice that can maintain the temperature between −75 and −80 °C; most transplant centers use liquid nitrogen-charged dry shippers that maintain the temperature below −135 °C. The thawing rate is as important as the cryopreservation rate. Rapid thaw can help reduce intracellular recrystallization of ice due to suboptimal cryopreservation procedure (Mazur 2004; Baust et al. 2009). HPCs are typically cryopreserved with low cooling rate (1 °C/min; see Chap. 6), but it was shown that thawing in 37 °C sustains higher cell viability compared to 4 °C (Bowman et al. 1996). Once ready to be thawed, the cryopreserved bag is removed from the dry shipper and is placed in an additional overwrap to prevent potential leaking in case of compromised bags. The wrapped unit is placed in a water bath containing sterile water validated to maintain temperature ranging between 37 and 40 °C. The unit is removed from the water bath when all the ice crystals dissolve. Many laboratories use alternative dry warming devices, instead of a water bath for thawing. The advantage of these devices is the fact that the units do not have to be submerged in water, a potential source of microbial contamination, and the device cleaning between products is easy.
When a unit is thawed, it has to be administered to the patient promptly to reduce damage to the cells. If multiple units are required for the transplant, they will be thawed sequentially to ensure that the previous unit was infused without adverse reaction. Once thawed as described above, the product can be infused directly from the bag, or it can be transferred to a syringe. Infusion pumps are usually not used, and most centers infuse by gravity. The use of a syringe allows increasing the infusion rate, but transferring the product to a syringe in the noncontrolled environment of the patient bedside does increase the risk of introducing contamination.
Bedside thaw is an easy method that does not require highly trained technologists and can be performed by the nurses in the unit, if trained properly. Additionally, it results in very little cell loss, especially if the empty bag is adequately flushed with saline. It is commonly used in adult patients that can tolerate relatively higher volumes of DMSO compared to children.
The direct thaw method carries multiple disadvantages. Larger volumes of DMSO are associated with adverse outcomes, and poorly mobilized autologous patient often have to tolerate large infusion volume to achieve transplant CD34+ cell dose. To reduce the chance of side effects, the maximum recommended dose of DMSO is 1 mL/kg of recipient body weight per 24 h, which can sometimes force infusion over multiple days (AABB et al. 2016). Adverse events were reported for infusion of thawed PB HPCs, some of them severe or even fatal. Once the product is thawed, any delay in infusion can further subject the cells to potential damage due to exposure to relatively high concentration of DMSO, without the benefit of the stabilizing effect of the protein- or colloid-based wash or dilution solution. Additional downside is the fact that infusion preparation occurs outside of the controlled laboratory environment, preventing characterization and confirmation of product cellular content. If samples are obtained at the bedside for retrospective testing, the cell integrity and viability might be compromised due to DMSO exposure by the time they reach the laboratory.
4.2 Clumping and the Use of Filter
Delayed infusion of thawed products can result in clumping formation. Granulocyte breakage results in release of toxins and DNA which were shown to result in clumping. Clumping can clog the infusion access line and can pose additional risk to the patient. A 170-μm blood filter can be used to remove these clots and is used by many transplant centers (Alessandrino et al. 1999; López-Jiménez et al. 1994; Kessinger et al. 1990); some centers prefer not to use the filter due to potential HPC lost and blockage of the filter.
4.3 Thaw and Wash
The thawing and washing method is designed to reduce the volume of DMSO and other elements such as cell debris and cytokines and decrease additional long-term cell damage and potential infusion adverse reaction. There is immediate dilution of the thawed product with a solution containing protein, colloids, or anticoagulant additives. This helps stabilize the membrane and immediately reduces DMSO concentration and is followed by centrifugation step and removal of most of the DMSO and other toxins. Alternatively, automated wash procedures are used.
The wash procedure is performed in the controlled laboratory environment. The wash procedure is based on the method described by Rubinstein and colleagues for preparation of CB unit (Rubinstein et al. 1995). The wash solution described in Rubinstein’s report is a mixture of Dextran 40 and HSA. Some laboratories use a similar solution for wash of PB HPC product. Additional solutions are described by others, which are usually an isotonic based buffer, such as saline or Plasmalyte A, combined with additives such as HSA and citrate dextrose (ACD-A) (Foïs et al. 2007; Scerpa et al. 2011; Syme et al. 2004). The wash solution is usually prepared on the day of infusion and maintained refrigerated until processing. The traditional method uses dilution of the product with the wash solution, followed by centrifugation for DMSO and debris removal. The cryopreserved bag is placed in an overwrap and thawed as described above. Multiple bags can be thawed at the same time. The thawed unit is slowly reconstituted with an equal volume wash solution and further diluted with the same solution. The maximal volume depends on the size of the thawed product and the transfer pack that is used. These typically range between 300 and 600 mL. The cells are than centrifuged in 800–1000 × g for 10–20 min, usually in 4–10 °C. The supernatant is removed, and the cells are resuspended in the same solution to a final volume that is similar to the original cryopreserved product volume. This procedure removes most of the DMSO.
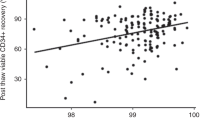
Unlike bedside thaw method, thawing and washing method is done in the controlled laboratory environment with all critical steps being performed in the biological safety cabinet, allowing sampling for prospective testing such as viability and potency. The major advantage of the wash procedure is the reduction in adverse reactions rates, probably due to the much lower volume of DMSO infused. Multiple studies have shown significantly lower infusion-related adverse effect of washed PB graft compared to non-washed, across all types of side effects monitored (Syme et al. 2004; Sánchez-Salinas et al. 2012; Akkök et al. 2009). This method was proven to reduce DMSO osmotic damage and maintain cell viability. When compared to the bedside thaw method, cell viability is stable for many hours, providing longer expiration time (Rodríguez et al. 2005).
Despite all the benefits listed above, the thaw and wash procedure does carry some disadvantages. The wash and centrifugation steps are associated with progenitor cell loss. Comparison studies report an average of 20% loss of TNC count post-wash and a similar loss of CD34+ cells (Syme et al. 2004; Akkök et al. 2009). Some of these cells can be recovered by applying a second centrifugation step, but this will increase the processing time and exposes the cells to additional damage. Akokke and colleagues showed that although time to neutrophil engraftment was similar for washed and non-washed autologous products, platelet engraftment was significantly delayed for washed products, resulting in a significantly higher number of platelet transfusions for patients (Akkök et al. 2009). Another factor to be considered when choosing to use the wash procedure is the risk of bag breakage. Although bag integrity can be compromised due to inappropriate bag sealing or during cryopreservation, the risk of bag breakage increases with any additional processing step, such as centrifugation. Compromised bag can result in major cell loss and potential microbial contamination. Lastly, it is also important to note that the thaw and wash method does require the availability of highly trained and qualified laboratory technologists, and for small programs that perform few transplants per year, this can be challenging.
5 Expert Point of View
In order to determine how to prepare PB HPCs for infusion, transplant centers need to assess multiple factors including the transplant program setting, the patient demographics, and the availability of trained laboratory staff. By reviewing these factors and the pros and cons of each method, programs can perform a risk assessment and come up with the best fitting approach.
Bedside thaw method is probably the most commonly used method for infusion of previously cryopreserved PB HPCs and, if done properly, results most of the time in hematological reconstitution. But many studies have shown that direct infusion of previously cryopreserved PB HPCs results in occurrence of adverse events, mostly mild or moderate. Most of these adverse events are attributed to the presence of DMSO, which has dose-dependent toxicity (López-Jiménez et al. 1994; Kessinger et al. 1990; Rowley et al. 1999). Factors such as TNC dose and granulocytes concentration are also shown to correlate with thawed autologous PB-mobilized HPC infusion adverse events (Cordoba et al. 2007; Khera et al. 2012).
Despite the relatively higher rates of adverse events, small volume adult transplant programs with limited availability of highly trained laboratory staff, or programs that do not have processing laboratory on site and use outside services, should consider using the bedside thaw method. The method does not reduce the DMSO volume, or any other toxins, but is simple and requires no processing.
On the other hand, programs that serve pediatric patient population or high-risk patients (see text above) might consider using the thaw wash method to reduce DMSO toxicity. The main disadvantages of the latter method is the complexity of the process and the risk of cell loss, but most comparison studies have shown no differences in neutrophil and platelet engraftment time between the methods, and sometimes the wash method results in a slightly shorter engraftment time, probably due to higher cell viability. All studies comparing infusion side effect outcomes demonstrate significantly lower rates for the washed products. This is the main reason to use the wash procedure, especially when serving very frail or pediatric patient population. This method removes most of the DMSO and other toxins and sustains cell viability for extended time.
6 Future Direction
Future efforts should be directed to improve and standardize cell/graft manufacturing, cryopreservation, and thawing of hematopoietic graft. Better understanding of the mechanism of cell damage by cryopreservation will help optimize the process. That should include parameters such as sample harvest and preparation, optimal cell concentration, additives used in the process, freezing curves, and more. Additionally, development of alternative, less toxic cryoprotectant agents will reduce the need to wash cells and will result in more stable products with lower toxicity.
There are constantly ongoing attempts to develop alternative cryoprotecting molecules either without or with reduced DMSO concentration (Bakken et al. 2003; Zeisberger et al. 2011). Disaccharide molecules such as trehalose and sucrose were shown to maintain membrane and protein integrity during cryopreservation, and their combination with DMSO concentration as low as 2.5% in cryopreservation of CB was shown to be compatible with the traditional 10% DMSO concentration (Woods et al. 2000; Rodrigues et al. 2008; Zhang et al. 2003). Recent publication by Svalgaard and colleagues explored the use of low-molecular-weight carbohydrate Pentaisomaltose (PIM) as an alternative to DMSO in cryopreservation of PB grafts. They demonstrated that progenitor cell recovery and potency were similar between PB products cryopreserved with PIM and DMSO (Svalgaard et al. 2016).
Automated wash devices are available for many years but are not often used by processing facility for PB HPC wash. They are expensive, require additional training, and are associated with the risk of additional HPC loss. Few automated devices were evaluated for washing of cryopreserved HPC products. Automated washing systems can provide a uniform standardized method that, if done properly, can increase cell recovery and reduce potential introduction of microbial contamination during processing. Some of these are 510(k) devices licensed for a specific use, and others have more usage flexibility. Regardless, each device has to be validated for the specific cell source use. Different automated devices were shown by few groups to result in high cell recovery and viable progenitor cells (Foïs et al. 2007; Scerpa et al. 2011; Sánchez-Salinas et al. 2012; Rodríguez et al. 2005; Perotti et al. 2004). All systems apply a single-use disposable set and different cell separation methodology. They were all shown to remove most of the DMSO and result in high CD34+ cell recovery. TNC recovery with these systems is usually between 75% and 90%, probably due to removal of granulocytes that do not sustain the cryopreservation and thawing process. Fois and colleagues used the traditional COBE 2991 cell washer, which uses centrifugal force to separate cells based on their type, size, and density, to wash cryopreserved PB HPCs. They reported substantial TNC loss, mainly due to granulocyte presence, and high CD34+ cell recovery. Few groups demonstrated the use of SEPAX cell processing system (Biosafe, Switzerland), a device designed as CB processing system, for washing of PB HPCs. This device separates cellular components through rotation of the syringe chamber and component transfer through a syringe piston. The wash with SEPAX proves to be at least as good as the manual wash method (see text above) and results in high CD34+ cell recovery (Scerpa et al. 2011; Sánchez-Salinas et al. 2012), CytoMate (Baxter, Chicago, IL), a spinning membrane against cell separating device, was shown to remove more than 95% of DMSO from products and recover more than 80% of CD34+ cells. The products resulted in significantly lower rates of infusion adverse reactions, and as demonstrated for washed products, time to neutrophil platelet engraftment was compatible to non-washed products, regardless of the TNC loss (Rodríguez et al. 2005; Calmels et al. 2003; Lemarie et al. 2005). Few other devices, such as the Lovo Cell Processing System (Fresenius Kabi), were introduced in the last few years. The expansion of the cellular therapy field and the introduction of new therapies encourage the industry to manufacture smaller and better applications for cell processing that are also in compliance with good manufacturing practices (GMPs).
References
AABB AAoTB, American Red Cross, American Society for Blood and Marrow, Transplantation ASfA, America’s Blood Centers, College of American Pathologists, Cord Blood Association, Foundation for the Accreditation of, Cellular Therapy I, International NetCord Foundation, International Society for Cellular Therapy, JACIE Accreditation Office, Program NMD (2016) Circular of information for the use of cellular therapy products. Bethesda, MD, AABB
Akkök CA, Holte MR, Tangen JM, Ostenstad B, Bruserud O (2009) Hematopoietic engraftment of dimethyl sulfoxide-depleted autologous peripheral blood progenitor cells. Transfusion 49(2):354–361
Alessandrino P, Bernasconi P, Caldera D et al (1999) Adverse events occurring during bone marrow or peripheral blood progenitor cell infusion: analysis of 126 cases. Bone Marrow Transplant 23(6):533–537
Anchordoguy TJ, Carpenter JF, Crowe JH, Crowe LM (1992) Temperature-dependent perturbation of phospholipid bilayers by dimethylsulfoxide. Biochim Biophys Acta 1104(1):117–122
Arakawa T, Carpenter JF, Kita YA, Crowe JH (1990) The basis for toxicity of certain cryoprotectants: a hypothesis. Cryobiology 27:401–415
Bakken AM, Bruserud O, Abrahamsen JF (2003) No differences in colony formation of peripheral blood stem cells frozen with 5% or 10% dimethyl sulfoxide. J Hematother Stem Cell Res 12(3):351–358
Baust JG, Gao D, Baust JM (2009) Cryopreservation: an emerging paradigm change. Organogenesis 5(3):90–96
Benekli M, Anderson B, Wentling D, Bernstein S, Czuczman M, McCarthy P (2000) Severe respiratory depression after dimethylsulphoxide-containing autologous stem cell infusion in a patient with AL amyloidosis. Bone Marrow Transplant 25(12):1299–1301
Bothner U, Georgieff M, Vogt NH (1998) Assessment of the safety and tolerance of 6% hydroxyethyl starch (200/0.5) solution: a randomized, controlled epidemiology study. Anesth Analg 86(4):850–855
Bowman CA, Yu M, Cottler-Fox M (1996) Evaluation of methods for preparing and thawing cryopreserved CD34+ and CD34− cell lines for use as reagents in flow cytometry of hematopoietic progenitor cells. Transfusion 36(11-12):985–988
Brave M, Farrell A, Ching Lin S et al (2010) FDA review summary: Mozobil in combination with granulocyte colony-stimulating factor to mobilize hematopoietic stem cells to the peripheral blood for collection and subsequent autologous transplantation. Oncology 78(3-4):282–288
Broxmeyer HE, Srour EF, Hangoc G, Cooper S, Anderson SA, Bodine DM (2003) High-efficiency recovery of functional hematopoietic progenitor and stem cells from human cord blood cryopreserved for 15 years. Proc Natl Acad Sci U S A 100(2):645–650
Calmels B, Houzé P, Hengesse JC, Ducrot T, Malenfant C, Chabannon C (2003) Preclinical evaluation of an automated closed fluid management device: Cytomate, for washing out DMSO from hematopoietic stem cell grafts after thawing. Bone Marrow Transplant 31(9):823–828
Cordoba R, Arrieta R, Kerguelen A, Hernandez-Navarro F (2007) The occurrence of adverse events during the infusion of autologous peripheral blood stem cells is related to the number of granulocytes in the leukapheresis product. Bone Marrow Transplant 40(11):1063–1067
Davis JM, Rowley SD, Braine HG, Piantadosi S, Santos GW (1990) Clinical toxicity of cryopreserved bone marrow graft infusion. Blood 75(3):781–786
Dhodapkar M, Goldberg SL, Tefferi A, Gertz MA (1994) Reversible encephalopathy after cryopreserved peripheral blood stem cell infusion. Am J Hematol 45(2):187–188
Donnenberg AD, Koch EK, Griffin DL et al (2002) Viability of cryopreserved BM progenitor cells stored for more than a decade. Cytotherapy 4(2):157–163
Fahy GM (1986) The relevance of cryoprotectant “toxicity” to cryobiology. Cryobiology 23(1):1–13
Foïs E, Desmartin M, Benhamida S et al (2007) Recovery, viability and clinical toxicity of thawed and washed haematopoietic progenitor cells: analysis of 952 autologous peripheral blood stem cell transplantations. Bone Marrow Transplant 40(9):831–835
Hoyt R, Szer J, Grigg A (2000) Neurological events associated with the infusion of cryopreserved bone marrow and/or peripheral blood progenitor cells. Bone Marrow Transplant 25(12):1285–1287
Kao GS (2009) Assessment of collection quality. In: Areman EM, Loper K (eds) Cellular therapy: principles, methods, and regulations. AABB, Bethesda, MD, pp 291–302
Keating GM (2011) Plerixafor: a review of its use in stem-cell mobilization in patients with lymphoma or multiple myeloma. Drugs 71(12):1623–1647
Kessinger A, Schmit-Pokorny K, Smith D, Armitage J (1990) Cryopreservation and infusion of autologous peripheral blood stem cells. Bone Marrow Transplant 5(Suppl 1):25–27
Khera N, Jinneman J, Storer BE et al (2012) Limiting the daily total nucleated cell dose of cryopreserved peripheral blood stem cell products for autologous transplantation improves infusion-related safety with no adverse impact on hematopoietic engraftment. Biol Blood Marrow Transplant 18(2):220–228
Lemarie C, Calmels B, Malenfant C et al (2005) Clinical experience with the delivery of thawed and washed autologous blood cells, with an automated closed fluid management device: CytoMate. Transfusion 45(5):737–742
López-Jiménez J, Cerveró C, Muñoz A et al (1994) Cardiovascular toxicities related to the infusion of cryopreserved grafts: results of a controlled study. Bone Marrow Transplant 13(6):789–793
Lovelock JE, Bishop MW (1959) Prevention of freezing damage to living cells by dimethyl sulphoxide. Nature 183(4672):1394–1395
Mazur P (2004) Principles of cryobiology. In: Fuller BJ, Lane N, Benson E (eds) Life in the frozen state. CRC, Boca Raton, FL, pp 3–66
Mazur P, Leibo SP, Chu EH (1972) A two-factor hypothesis of freezing injury. Evidence from Chinese hamster tissue-culture cells. Exp Cell Res 71(2):345–355
Pagano MB, Harmon C, Cooling L et al (2016) Use of hydroxyethyl starch in leukocytapheresis procedures does not increase renal toxicity. Transfusion 56(11):2848–2856
Pasquini M, Zhu X (2015) Current uses and outcomes of hematopoietic stem cell transplantation: CIBMTR summary slides. http://www.cibmtr.org
Perotti CG, Del Fante C, Viarengo G et al (2004) A new automated cell washer device for thawed cord blood units. Transfusion 44(6):900–906
Rapoport AP, Rowe JM, Packman CH, Ginsberg SJ (1991) Cardiac arrest after autologous marrow infusion. Bone Marrow Transplant 7(5):401–403
Rodrigues JP, Paraguassú-Braga FH, Carvalho L, Abdelhay E, Bouzas LF, Porto LC (2008) Evaluation of trehalose and sucrose as cryoprotectants for hematopoietic stem cells of umbilical cord blood. Cryobiology 56(2):144–151
Rodríguez L, Velasco B, García J, Martín-Henao GA (2005) Evaluation of an automated cell processing device to reduce the dimethyl sulfoxide from hematopoietic grafts after thawing. Transfusion 45(8):1391–1397
Rowley S, MacLeod B, Heimfeld S, Holmberg L, Bensinger W (1999) Severe central nervous system toxicity associated with the infusion of cryopreserved PBSC components. Cytotherapy 1(4):311–317
Rubinstein P, Dobrila L, Rosenfield RE et al (1995) Processing and cryopreservation of placental/umbilical cord blood for unrelated bone marrow reconstitution. Proc Natl Acad Sci U S A 92(22):10119–10122
Runckel DN, Swanson JR (1980) Effect of dimethyl sulfoxide on serum osmolality. Clin Chem 26(12):1745–1747
Samoszuk M, Reid ME, Toy PT (1983) Intravenous dimethylsulfoxide therapy causes severe hemolysis mimicking a hemolytic transfusion reaction. Transfusion 23(5):405
Sánchez-Salinas A, Cabañas-Perianes V, Blanquer M et al (2012) An automatic wash method for dimethyl sulfoxide removal in autologous hematopoietic stem cell transplantation decreases the adverse effects related to infusion. Transfusion 52(11):2382–2386
Sauer-Heilborn A, Kadidlo D, McCullough J (2004) Patient care during infusion of hematopoietic progenitor cells. Transfusion 44(6):907–916
Scerpa MC, Daniele N, Landi F et al (2011) Automated washing of human progenitor cells: evaluation of apoptosis and cell necrosis. Transfus Med 21(6):402–407
Smith DM, Weisenburger DD, Bierman P, Kessinger A, Vaughan WP, Armitage JO (1987) Acute renal failure associated with autologous bone marrow transplantation. Bone Marrow Transplant 2(2):195–201
Snyder EL, Haley NR (eds) (2004) Cellular therapy: a physician’s handbook, 1st edn. Bethesda, MD, AABB
Spurr EE, Wiggins NE, Marsden KA, Lowenthal RM, Ragg SJ (2002) Cryopreserved human haematopoietic stem cells retain engraftment potential after extended (5-14 years) cryostorage. Cryobiology 44(3):210–217
Svalgaard JD, Haastrup EK, Reckzeh K et al (2016) Low-molecular-weight carbohydrate Pentaisomaltose may replace dimethyl sulfoxide as a safer cryoprotectant for cryopreservation of peripheral blood stem cells. Transfusion 56(5):1088–1095
Syme R, Bewick M, Stewart D, Porter K, Chadderton T, Glück S (2004) The role of depletion of dimethyl sulfoxide before autografting: on hematologic recovery, side effects, and toxicity. Biol Blood Marrow Transplant 10(2):135–141
Vercueil A, Grocott MP, Mythen MG (2005) Physiology, pharmacology, and rationale for colloid administration for the maintenance of effective hemodynamic stability in critically ill patients. Transfus Med Rev 19(2):93–109
Wagner JE, Barker JN, DeFor TE et al (2002) Transplantation of unrelated donor umbilical cord blood in 102 patients with malignant and nonmalignant diseases: influence of CD34 cell dose and HLA disparity on treatment-related mortality and survival. Blood 100(5):1611–1618
Windrum P, Morris TC, Drake MB, Niederwieser D, Ruutu T, Subcommittee ECLWPC (2005) Variation in dimethyl sulfoxide use in stem cell transplantation: a survey of EBMT centres. Bone Marrow Transplant 36(7):601–603
Woods EJ, Liu J, Derrow CW, Smith FO, Williams DA, Critser JK (2000) Osmometric and permeability characteristics of human placental/umbilical cord blood CD34+ cells and their application to cryopreservation. J Hematother Stem Cell Res 9(2):161–173
Yellowlees P, Greenfield C, McIntyre N (1980) Dimethylsulphoxide-induced toxicity. Lancet 2(8202):1004–1006
Zambelli A, Poggi G, Da Prada G et al (1998) Clinical toxicity of cryopreserved circulating progenitor cells infusion. Anticancer Res 18(6B):4705–4708
Zeisberger SM, Schulz JC, Mairhofer M et al (2011) Biological and physicochemical characterization of a serum- and xeno-free chemically defined cryopreservation procedure for adult human progenitor cells. Cell Transplant 20(8):1241–1257
Zenhäusern R, Tobler A, Leoncini L, Hess OM, Ferrari P (2000) Fatal cardiac arrhythmia after infusion of dimethyl sulfoxide-cryopreserved hematopoietic stem cells in a patient with severe primary cardiac amyloidosis and end-stage renal failure. Ann Hematol 79(9):523–526
Zhang XB, Li K, Yau KH et al (2003) Trehalose ameliorates the cryopreservation of cord blood in a preclinical system and increases the recovery of CFUs, long-term culture-initiating cells, and nonobese diabetic-SCID repopulating cells. Transfusion 43(2):265–272
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this chapter
Cite this chapter
Reich-Slotky, R. (2018). Peripheral Blood Hematopoietic Progenitor Cell Graft Thawing. In: Schwartz, J., Shaz, B. (eds) Best Practices in Processing and Storage for Hematopoietic Cell Transplantation . Advances and Controversies in Hematopoietic Transplantation and Cell Therapy. Springer, Cham. https://doi.org/10.1007/978-3-319-58949-7_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-58949-7_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-58948-0
Online ISBN: 978-3-319-58949-7
eBook Packages: MedicineMedicine (R0)