Abstract
Although severe symptoms and deteriorating function of the affected hand are the main reasons patients seek treatment for carpal tunnel syndrome (CTS), much variability exists in assessing CTS symptoms. Today, there is no reference standard to determine the severity and thus the optimal treatment option for CTS. Traditional means of measuring the impairment of the median nerve lack qualities necessary to evaluate outcome measures that are important to patients. Subjective evaluations such as health and functioning questionnaires have proven to be valid and responsive in assessing outcomes of interest. The debate remained over the appropriate treatment, based on the severity of CTS, and the most suitable outcome questionnaire to measure responsiveness of the treatment. This review will focus on current evidence from clinical outcome research regarding measurement of CTS severity scoring systems and comparisons of current instruments based on desirable properties of a validated questionnaire.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Although carpal tunnel syndrome (CTS) is the most common wrist and hand disorder [1,2,3], much controversy still exists regarding standardization of its treatments and outcome measures [4]. CTS occurs following compression of the median nerve within the carpal tunnel [1] and is associated with severe pain, numbness, and tingling in the affected hand [5, 6]. Traditionally, clinical evaluation of CTS focused on measuring neuromuscular impairment of the nerve [5, 7], manifested by reduced sensibility and grip strength [2, 7]. However, owing to the fact that CTS symptoms may not necessarily be accompanied by physical changes in sensation and strength of the median nerve in the hand [3, 5], assessing the severity of CTS and the outcomes of treatment has remained a challenge [8]. More recently, in addition to the traditional set of physical measurements [5, 9], physicians have started employing subjective methods such as questionnaires that place more emphasis on outcomes that matter the most to patients [10, 11]. Health outcome questionnaires, whether administered verbally by the physician at the clinic or self-administered by the patient, are examples of subjective tools used for assessment of severity of symptoms and functional status in CTS [10,11,12,13].
Today, more than ever, the healthcare system is constrained by limited resources and increasing demand. Thus, medicine is under stringent scrutiny to not only deliver high-quality care but to do so in a cost-effective way [14]. Additionally, with the establishment of the Patient-Centered Outcomes Research Institute (PCORI) under the Affordable Care Act (ACA) [14], and recognition of the patient as an active participant in medical decision-making, health outcome questionnaires have become important tools for inclusion of patients’ perspectives. This chapter will explore and evaluate available assessment tools, particularly health outcome questionnaires commonly used to measure CTS severity and treatment outcomes.
Assessment of Severity of Symptoms and Optimal Treatment Option
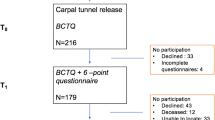
Treatment suggestions for CTS depend on a physician’s assessment of a patient’s history and severity of symptoms [15, 16]. If symptoms are mild to moderate and CTS is diagnosed early, nonsurgical methods including wrist splinting, nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, or injection of corticosteroid drugs such as cortisone may reduce the inflammation and alleviate some or all of the symptoms, either temporarily or over the long term [3]. If, however, the symptoms have become severe, surgery may be the most effective option [3]. Despite the high prevalence of and extensive body of literature on CTS [17, 18], perhaps because there is no easy way of determining the severity of the condition, debate, and controversy regarding assessment and treatment of CTS continue [19]. Thus, most physicians choose to apply a combination of tools in their assessments of severity and effectiveness of treatment (Fig. 9.1) [19].
Objective Measurement Tools
In order to check the health of the median nerve, and usually when symptoms of CTS are severe enough for the patient to be considered for surgery, electrodiagnostic studies are performed [20]. There are two types of electrodiagnostic nerve tests: (1) nerve condition velocity (NCV) measures the speed of electricity as it passes through a nerve and (2) electromyogram (EMG) checks the electrical activities of nerves and muscles [21]. Based on these test results and the patient’s history of CTS, the symptom severity scale of the condition will be defined as mild, moderate, or severe [7]. Nerve tests are expensive and painful for patients; many physicians argue that patients may not need to go through these tests [7, 19].
Subjective Measurement Tools
In addition to objective measurement tools , there are a variety of subjective tools that physicians may use to assess the severity of CTS [7]. For example, common clinical provocative CTS tests include Phalen’s test [22], Tinel’s sign [22, 23], the Durkan’s carpal compression test (CCT) [24], or the Katz-Stirrat hand diagram [7, 25] (Table 9.1).
Qualities of a Good Severity Measurement Tool for CTS
Although most traditional CTS tests have been performed commonly in clinical settings, assessments of their validity, reliability, and responsiveness do not necessarily yield the same results [25]. For example, research shows no correlation between the severity of CTS and results of the Tinel’s, Durkan’s carpal compression, and Katz-Stirrat hand diagram tests [7]. Phalen’s test was the only test to show a positive association between results of the nerve conducting test and severity of CTS [7]. Higher CTS severity scores are positively associated with a higher probability of the Phalen’s test being positive [7]. Reliability of these tests ranged from moderate (0.51 for Tinel’s sign, with a confidence interval of 0.13–0.88) to excellent (0.95 for the Katz-Stirrat hand diagram, with a confidence interval of 0.84–1.00) [7].
Outcome Assessment Tools
In developing any health status questionnaire , there is a tradeoff between breadth and depth of measurement [26]. Generic health outcome questionnaires seek to evaluate health using a broad perspective, ranging from physical to social health. For example, the 36-Item Short-Form Health Survey (SF-36) evaluates eight different domains of health and well-being without being related to any specific illness [27]. Generic questionnaires are usually useful when comparing health status across various conditions [28]. On the other hand, questionnaires that were developed to measure health outcomes related to a specific condition such as CTS or rheumatoid arthritis seek to evaluate symptoms and functions that are very specific to an illness (more depth and less breadth). For example, the Carpal Tunnel Questionnaire (CTQ) evaluates all major symptoms or functions that are specifically related to CTS (e.g., hand and wrist numbness or pain at night) [10]. For health surveys measuring general health status, such as the SF-36, breadth is more important than sensitivity toward a specific illness [26]. On the other hand, for illness-specific questionnaires such as the CTQ, the focus is more on sensitivity to changes in conditions specific to carpal tunnel [7, 9, 29, 30].
Outcome questionnaires have been developed to examine the responsiveness of treatment for CTS in a standardized and non-biased way. A good outcome questionnaire should be reproducible, valid, reliable, and responsive to changes in symptom relief and functioning status (Table 9.2) [26, 30, 31]. With a direct annual cost of more than one billion dollars, carpal tunnel release is the most common surgical procedure performed on the hand [10]. Although patients with CTS are mostly concerned about symptom relief and improvement in hand function [31], up until 1993 the responsiveness of the treatment, including surgical procedures, had been mostly assessed by using physical/objective measurement tools such as nerve studies [10, 31]. Because it was primarily the surgeons who had performed the operations who conducted the outcome studies, the probability of bias was relatively high in supporting the success of the surgical treatment [4]. In this section, we will describe and compare the health questionnaires commonly used to assess the severity and treatment outcomes of CTS. First, we will describe each of the following questionnaires: (1) the Carpal Tunnel Questionnaire (CTQ) ; (2) the Michigan Hand Questionnaire (MHQ) ; (3) the Disability of Arm, Shoulder, or Hand Questionnaire (DASH) ; and (4) the 36-Item Short-Form Health Survey (SF-36) . We will then use properties associated with validated questionnaires to evaluate commonly used health instruments [4, 32].
Carpal Tunnel Questionnaire (CTQ) [10]
Brigham and Women’s Carpal Tunnel Questionnaire (CTQ) is an example of a disease-specific questionnaire designed to evaluate CTS [4]. The CTQ, developed by Levine et al., contains two separate scales: (1) symptom severity and (2) functional status [10]. Severity of CTS is measured using an 11-item multiple-choice questionnaire, focusing on pain, numbness, tingling, and nocturnal symptoms. Each item is scored from 1 (none or mild) to 5 (severe). The mean of all 11 scores is reported as the overall symptom severity of CTS. To measure functional status, an 8-item functioning questionnaire measures a range of activities [10]. Each listed activity is scored from 1 (no difficulty) to 5 (cannot do at all). A higher score on both scales shows a higher severity or a more limited hand/wrist function [10].
A multidisciplinary team of hand surgeons, rheumatologists, and CTS patients developed the CTQ; it contains all essential properties of a valid health instrument: reproducibility, internal consistency, validity, responsiveness, and ease of use (Table 9.2) [32]. The main advantage of this questionnaire is that it is focuses on symptoms and functions most often observed among CTS patients, so it is the most sensitive and responsive questionnaire for CTS. Pearson correlation coefficients of above 90% indicate excellent reliability/reproducibility attributes for both sections of this questionnaire [10]. In contrast, because it is disease specific, the CTQ does not allow for comparisons among different conditions [4].
Regarding validity of the questionnaire , a high correlation between mean scores obtained from the two sections of the test, severity of symptoms and function status, shows that patients with more severe scores had more function limitations. However, the correlation scores between both severity of symptoms and function status and traditional objective tools such as nerve conducting tests show low or poor correlation. For example, the correlation between the result of symptom severity evaluated by the CTQ and the two-point discrimination test, using the Spearman coefficient, was 0.15 and statistically not significant [10]. This is not an indication of low validity of the questionnaire; the provocative and nerve conducting tests and the CTQ capture different outcomes and should be used as complementary tools [10,11,12, 29].
With the average effect size of 0.82, the CTQ proved to be a responsive tool in measuring clinical outcome changes [10]. Additionally, patients’ satisfaction with the result of treatment was associated with significant improvement in symptom relief and function status [10].
Michigan Hand Questionnaire (MHQ)
The MHQ is a 57-item hand-specific questionnaire with six different domains that can be administered all together or in isolation [33]. The six domains of the questionnaire include (1) function, (2) activities of daily living, (3) pain, (4) work performance, (5) aesthetics, and (6) patient satisfaction [33]. The MHQ is widely used for various hand disorders [34] and has been translated into many different languages and used in other countries [35, 36].
Patients are asked to answer each question for each domain using a scale of 1–5 [33]. The sum of scores for each domain can total up to 100. With the exception of the pain domain, in all other domains a score of 0 represents the worst outcome and score of 100 represents the best [33, 37]. Like DASH, the MHQ can also be used for other hand disorders [38, 39]. However, because it covers hand and the wrist in the global assessment, it is more specific. The MHQ is the only hand questionnaire that distinguishes between the two hands and can be used to compare the severity of symptoms and function of one hand with the other [30].
Like DASH, the MHQ also has a 12-item brief MHQ to reduce the burden of answering long questionnaires for patients [40]. Both the MHQ and brief MHQ have been proven to be reliable, valid, and responsive hand outcome instruments and used to assess effectiveness of treatments for different hand disorders including CTS [30, 39, 40]. The MHQ has many advantages over other similar hand questionnaires. The MHQ is specific to hands but not to any specific disorder; this gives the questionnaire a desirable depth and adequate breadth. Additionally, having different domains makes it flexible and responsive for each specific disorder. For example, in assessment of CTS, the aesthetics domain can be excluded without affecting the results of the questionnaire [30]. Also, because the MHQ distinguishes between the two hands makes it possible to compare the outcomes of the affected hand with the unaffected hand. Most importantly, because the MHQ can measure outcomes of all hand and wrist conditions (e.g., CTS, carpometacarpal thumb arthritis, rheumatoid arthritis of hand, etc.), it can be utilized in comparative effectiveness studies across various conditions.
Disabilities of the Arm, Shoulder, or Hand Questionnaire (DASH)
DASH is a 30-item self-administered questionnaire that was designed to measure physical function and severity of symptoms in patients with any upper extremity musculoskeletal disorder [41,42,43]. DASH was developed to fill the gap in longitudinal assessment of patients with one or multiple upper extremity disorders or injuries [41]. DASH contains two main domains: (1) symptoms and (2) function status, including physical, social, and psychological functioning [43]. Patients are asked to choose the level of difficulty of doing an activity or severity of a symptom, using a five-point Likert scale, with a higher score indicating a greater level of severity and disability [41]. To calculate the DASH total score, one needs to add all the responses (ranging between 1 and 5) and subtract 30 from the total; then, the total has to be divided by 1.2 to get a DASH score out of 100 [41]. If more than three items are not answered (missing), the overall DASH score cannot be calculated [41]. DASH combines questions related to symptom severity and functioning into one single questionnaire. The total score ranges from 0 to 100, with 0 representing perfect functioning and 100 representing the worst symptoms and disability [43]. Examples of activities include preparing a meal, pushing a heavy door, and making a bed. The functioning portion of the questionnaire includes general questions regarding pain, weakness, or tingling of the arm, shoulder, or hand, ranging from none to extreme [41].
DASH has been translated into many different languages and used widely in other countries [42]. Late in 2005, a shorter version of DASH , an 11-item questionnaire called QuickDASH, was developed to ease the burden of answering too many questions for the patients [44]. Both the DASH and QuickDASH questionnaires have proven to be reliable, valid, and responsive to clinical changes for upper extremity injuries and disorders (Table 9.3) [42, 46].
The main advantage of DASH is that it is one questionnaire that can be applied to all upper extremity disorders, including CTS [10, 29, 30]. DASH is particularly useful for the assessment of upper extremity disorders in which the combination of symptoms and function can be assessed in one scale. However, DASH is a generic upper extremity questionnaire, which makes it less sensitive in assessing CTS responsiveness to treatment simply because symptoms specific to CTS improve more quickly than function outcomes [29, 30]. Thus, the combined scoring system of DASH for symptoms and function outcomes reduces the responsiveness of the questionnaire compared with the CTQ or the MHQ. This is because DASH puts more emphasis on the functional aspects of upper extremity disorder than on the severity of symptoms [12]. Additionally, DASH does not distinguish between the two hands, so one cannot use the questionnaire to compare the unaffected hand with the affected one [47].
36-Item Short-Form Health Survey (SF-36)
The SF-36 was developed in 1992 to be used not only in clinical practice but also in population research studies and health policy evaluations [26]. The SF-36 evaluates eight domains of health and well-being: (1) limitations of physical activity, (2) limitations in social activities, (3) limitations in usual role activities due to physical health, (4) pain, (5) mental health, (6) limitations in usual role activities due to mental health, (7) vitality (energy and fatigue), and (8) perception of general health [26]. The SF-36 uses the Likert scale—a psychometric method commonly used in questionnaires for scaling responses [48]. The interpretation of the results is based on the assumption that the averaged scored items represent the underlying health status that is being measured [27, 49]. The goal of SF-36 is to validly and precisely report the relevant differences and changes in health status and well-being [50].
Assessment of Common Outcome Questionnaires for CTS
During the last decade, various questionnaires have been developed to assess severity of symptoms, function status, and outcomes of treatment for CTS and other illnesses [10, 26, 33, 43]. In this chapter, we reviewed a few of the most common instruments, ranging from a completely generic one such as the SF-36 to the most specific one, the CTQ, that have been used for assessment of CTS. Although these instruments proved to possess all the properties of validated questionnaires, there are small variations among them when used to examine CTS. For example, research indicates less variability among hand outcome questionnaires such as the Carpal Tunnel Questionnaire (CTQ), the Michigan Hand Questionnaire (MHQ), and Disabilities of the Arm, Shoulder, and Hand (DASH). Compared with the SF-36 as an example of a generic questionnaire, hand and upper extremity questionnaires appear to be more responsive (Table 9.3) [29, 30, 51]. Physicians, researchers, and patients prefer the short forms of both DASH and the MHQ [40, 46]. The main versions of these two hand questionnaires take a longer time to complete . In addition to taking less time to complete, the short forms are similarly reproducible, valid, reliable, and responsive [40, 46]. Thus, they are the preferred instruments compared with their original versions. Considering the high prevalence of CTS and the importance of patient-centered health outcomes, depending on the context of the research, use of the appropriate outcome instrument is pertinent (Table 9.3).
Possible Future Direction
Thomas Bayes (1702–1761), an English statistician, mathematician, and philosopher, is mostly known for his work on probability [52]. According to his theory, the likelihood of having a particular condition can be estimated based on the previous probability of having that condition [53]. In statistics, this is called posterior probability [53]. From a clinical practice, posterior probability may allow a physician to mathematically combine a sequence of tests, avoiding unnecessary physical tests [53]. Theoretically, this approach adjusts for all sensitivities and specificities in the final probability value [53]. Thus, it may prove a valuable technique to help avoid expensive or uncomfortable physical exams such as nerve conduction tests (NCS) for diagnosis of CTS. For example, O’Gradaigh and Merry applied the Bayesian posterior probability technique to examine its validity among patients suspected of having CTS [54]. Prospectively, their algorithm proved to be reliable and had the same accuracy as NCS in diagnosing CTS patients [54]. Particularly for conditions with a high prevalence, such as CTS, Bayesian probability may be a useful technique in reducing the time, cost, and dissatisfaction involved in diagnosis and treatment [55,56,57,58].
Summary
The role of reliable and validated outcome instruments in measuring various health outcomes such as severity of symptoms, function status, health-related quality of life, and patient’s satisfaction with the undertaken treatment have become increasingly acknowledged. Over the past decade, there has been a tremendous effort by physicians, policy makers, and researchers to increase assessment and accountability in medicine. The increasing demand of our aging population and our limited resources give rise to the need for assessment and accountability. With an estimated annual cost of more than one billion dollars, CTS is the most common upper extremity disorder. Today, despite the tremendous progress during the 1990s in development of assessment and outcome questionnaires, controversy surrounding the treatment of CTS still remains. Future research using Bayesian probability algorithms may help streamline severity assessment and standardize treatment for CTS.
References
Sanz JR, Zamora B, San José J, Terán P. Carpal tunnel syndrome. J Hand Surg. 1994;19(6):1056–7.
Phalen GS. The carpal-tunnel syndrome. J Bone Joint Surg. 1966;48(2):211–28.
Keith MW, Masear V, Amadio PC, et al. Treatment of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009;17(6):397–405.
Patterson JD, Simmons BP. Outcomes assessment in carpal tunnel syndrome. Hand Clin. 2002;18(2):359–63.
Chung KC. Commentary: severe carpal tunnel syndrome. J Hand Surg. 2003;28(4):645–6.
Rempel D, Evanoff B, Amadio PC, et al. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am J Public Health. 1998;88(10):1447–51.
Priganc VW, Henry SM. The relationship among five common carpal tunnel syndrome tests and the severity of carpal tunnel syndrome. J Hand Ther. 2003;16(3):225–36.
Gerritsen AA, de Vet HC, Scholten RJ, Bertelsmann FW, de Krom MC, Bouter LM. Splinting vs surgery in the treatment of carpal tunnel syndrome: a randomized controlled trial. JAMA. 2002;288(10):1245–51.
Changulani M, Okonkwo U, Keswani T, Kalairajah Y. Outcome evaluation measures for wrist and hand–which one to choose? Int Orthop. 2008;32(1):1–6.
Levine DW, Simmons BP, Koris MJ, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg. 1993;75(11):1585–92.
Katz JN, Gelberman RH, Wright EA, Lew RA, Liang MH. Responsiveness of self-reported and objective measures of disease severity in carpal tunnel syndrome. Med Care. 1994;32(11):1127–33.
Amadio PC, Silverstein MD, Ilstrup DM, Schleck CD, Jensen LM. Outcome assessment for carpal tunnel surgery: the relative responsiveness of generic, arthritis-specific, disease-specific, and physical examination measures. J Hand Surg. 1996;21(3):338–46.
Hobby J, Watts C, Elliot D. Validity and responsiveness of the patient evaluation measure as an outcome measure for carpal tunnel syndrome. J Hand Surg. 2005;30(4):350–4.
Burwell SM. Setting value-based payment goals—HHS efforts to improve US health care. N Engl J Med. 2015;372(10):897–9.
Bland JD. A neurophysiological grading scale for carpal tunnel syndrome. Muscle Nerve. 2000;23(8):1280–3.
Kadzielski J, Malhotra LR, Zurakowski D, Lee S-GP, Jupiter JB, Ring D. Evaluation of preoperative expectations and patient satisfaction after carpal tunnel release. J Hand Surg. 2008;33(10):1783–8.
Piazzini DB, Aprile I, Ferrara PE, et al. A systematic review of conservative treatment of carpal tunnel syndrome. Clin Rehabil. 2007;21(4):299–314.
Gerritsen A, Uitdehaag B, Van Geldere D, Scholten R, de Vet H, Bouter L. Systematic review of randomized clinical trials of surgical treatment for carpal tunnel syndrome. Br J Surg. 2001;88(10):1285–95.
Ono S, Clapham PJ, Chung KC. Optimal management of carpal tunnel syndrome. Int J Gen Med. 2010;3:255.
Katz JN, Larson MG, Sabra A, et al. The carpal tunnel syndrome: diagnostic utility of the history and physical examination findings. Ann Intern Med. 1990;112(5):321–7.
Jablecki CK, Andary CMT, So YT, Wilkins DE, Williams FH, Committee AQA. Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. Muscle Nerve. 1993;16(12):1392–414.
Kuschner S, Ebramzadeh E, Johnson D, Brien W, Sherman R. Tinel’s sign and Phalen’s test in carpal tunnel syndrome. Orthopedics. 1992;15(11):1297–302.
Gelberman RH, Hergenroeder PT, Hargens AR, Lundborg GN, Akeson WH. The carpal tunnel syndrome. A study of carpal canal pressures. J Bone Joint Surg. 1981;63(3):380–3.
Georgiew F. Provocative tests used in the diagnosis of carpal tunnel syndrome. Med Rehabil. 2007;11(4):7–17.
Wöber C, Zeitlhofer J. The serial use of two provocative tests in the clinical diagnosis of carpal tunnel syndrome. Acta Neurol Scand. 1998;98(5):328–32.
Ware Jr JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83.
Ware JE, Kosinski M. SF-36 physical & mental health summary scales: a manual for users of version 1. Lincoln, RI: Quality Metric; 2001.
Bessette L, Sangha O, Kuntz KM, et al. Comparative responsiveness of generic versus disease-specific and weighted versus unweighted health status measures in carpal tunnel syndrome. Med Care. 1998;36(4):491–502.
Gay RE, Amadio PC, Johnson JC. Comparative responsiveness of the disabilities of the arm, shoulder, and hand, the carpal tunnel questionnaire, and the SF-36 to clinical change after carpal tunnel release. J Hand Surg. 2003;28(2):250–4.
Kotsis SV, Chung KC. Responsiveness of the Michigan hand outcomes questionnaire and the disabilities of the arm, shoulder and hand questionnaire in carpal tunnel surgery. J Hand Surg. 2005;30(1):81–6.
Chung KC. Current status of outcomes research in carpal tunnel surgery. Hand. 2006;1(1):9–13.
Ware J. Methodological considerations in the selection of health status assessment procedures. In: Assessment of quality of life in clinical trials of cardiovascular therapies. New York: Lejacq; 1984. p. 87–111.
Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg. 1998;23(4):575–87.
Chatterjee JS, Price PE. Comparative responsiveness of the Michigan Hand Outcomes Questionnaire and the Carpal Tunnel Questionnaire after carpal tunnel release. J Hand Surg. 2009;34(2):273–80.
van der Giesen FJ, Nelissen RG, Arendzen JH, de Jong Z, Wolterbeek R, Vlieland TPV. Responsiveness of the Michigan hand outcomes questionnaire–Dutch language version in patients with rheumatoid arthritis. Arch Phys Med Rehabil. 2008;89(6):1121–6.
Öksüz Ç, Akel BS, Oskay D, Leblebicioğlu G, Hayran KM. Cross-cultural adaptation, validation, and reliability process of the Michigan Hand Outcomes Questionnaire in a Turkish population. J Hand Surg. 2011;36(3):486–92.
Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42(6):619–22.
Horng Y-S, Lin M-C, Feng C-T, Huang C-H, H-C W, Wang J-D. Responsiveness of the Michigan Hand Outcomes Questionnaire and the Disabilities of the Arm, Shoulder, and Hand questionnaire in patients with hand injury. J Hand Surg. 2010;35(3):430–6.
Kotsis SV, Lau FH, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and physical measurements in outcome studies of distal radius fracture treatment. J Hand Surg. 2007;32(1):84–90.
Waljee JF, Kim HM, Burns PB, Chung KC. Development of a brief, 12-item version of the Michigan Hand Questionnaire. Plast Reconstr Surg. 2011;128(1):208.
Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the wole or the parts?: Validity, reliability, and responsiveness of the disabilities of the arm, shoulder and hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128–42.
Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4(1):11.
Hudak PL, Amadio P, Bombardier C. The Upper Extremity Collaborative Group (UECG). Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. Am J Ind Med. 1996;29(6):602–8.
Beaton DE, Wright JG, Katz JN. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg. 2005;87(5):1038–46.
Manktelow RT, Binhammer P, Tomat LR, Bril V, Szalai JP. Carpal tunnel syndrome: Cross-sectional and outcome study in Ontario workers. J Hand Surg. 2004;29A:307–17.
Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006;7(1):44.
Yucel H, Seyithanoglu H. Choosing the most efficacious scoring method for carpal tunnel syndrome. Acta Orthop Traumatol Turc. 2015;49(1):23–9.
Likert R. A technique for the measurement of attitudes. In: Archives of psychology. New York: New York University; 1932.
Stewart AL. Measuring functioning and well-being: the medical outcomes study approach. Durham, NC: Duke University Press; 1992.
McHorney CA, Ware Jr JE, Rogers W, Raczek AE, Lu JR. The validity and relative precision of MOS short-and long-form health status scales and Dartmouth COOP charts: results from the Medical Outcomes Study. Med Care. 1992;30(5 Suppl):MS253–65.
Husted JA, Cook RJ, Farewell VT, Gladman DD. Methods for assessing responsiveness: a critical review and recommendations. J Clin Epidemiol. 2000;53(5):459–68.
Press SJ, Press JS. Bayesian statistics: principles, models, and applications. New York: Wiley; 1989.
Macartney FJ. Diagnostic logic. Br Med J (Clin Res Ed). 1987;295(6609):1325–31.
O’Gradaigh D, Merry P. A diagnostic algorithm for carpal tunnel syndrome based on Bayes’s theorem. Rheumatology. 2000;39(9):1040–1.
Elstein AS, Schwarz A. Clinical problem solving and diagnostic decision making: selective review of the cognitive literature. BMJ. 2002;324(7339):729–32.
Achim A, Bezerianos A, Tsakalides P. Novel Bayesian multiscale method for speckle removal in medical ultrasound images. IEEE Trans Med Imaging. 2001;20(8):772–83.
Rifkin RD, Hood Jr WB. Bayesian analysis of electrocardiographic exercise stress testing. N Engl J Med. 1977;297(13):681–6.
Miettinen OS, Caro JJ. Foundations of medical diagnosis: what actually are the parameters involved in Bayes’ theorem? Stat Med. 1994;13(3):201–9.
Funding
This work was supported by the Midcareer Investigator Award in Patient-Oriented Research (2 K24-AR053120-06) (to Dr. Kevin C. Chung).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Mahmoudi, E., Chung, K.C. (2017). Severity Scoring Systems for Carpal Tunnel Syndrome and Outcome Tools. In: Duncan, S., Kakinoki, R. (eds) Carpal Tunnel Syndrome and Related Median Neuropathies. Springer, Cham. https://doi.org/10.1007/978-3-319-57010-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-57010-5_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-57008-2
Online ISBN: 978-3-319-57010-5
eBook Packages: MedicineMedicine (R0)