Abstract
Background
The effectiveness of the surgical treatment of carpal tunnel syndrome (CTS) is well known on short term. However, limited data is available about long-term outcome after carpal tunnel release (CTR). The aims of this study were to explore the long-term outcome after CTR and to identify prognostic factors for long-term outcome.
Methods
Patients with clinically defined CTS underwent CTR and completed the Boston Carpal Tunnel Questionnaire at baseline (T0), at about 8 months (T1), and after a median follow-up of 9 years (T2), as well as a 6-point scale for perceived improvement (at T1 and T2). Potentially prognostic factors were identified by logistic regression analysis and correlation.
Results
At long-term follow-up, 87 patients (40.3%) completed the questionnaires. Mean score on Symptom Severity Scale (2.87 to 1.54; p < 0.001) and Functional Status Scale (2.14 to 1.51; p < 0.001) improved at 8 months and did not change significantly after 8 months. A favorable outcome was reported in 81.6%. A good treatment outcome after 8 months and to a lesser extent a lower FSS score at T0 were associated with a better long-term outcome.
Conclusions
CTR is a robust treatment for CTS and its effect persists after a period of 9 years. The most important factor associated with long-term outcome is treatment outcome after about 8 months and to a lesser extent functional complaints preoperatively. Outcome is independent of patient characteristics, electrodiagnostic test results, or findings at the initial neurological examination.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carpal tunnel release (CTR) is considered as the most effective treatment for CTS [24]. In our initial study, we demonstrated complete relieve of symptoms 7–9 months after open CTR in 60.6% and 48.0% of patients with electrodiagnostically confirmed typical and atypical (sensory complaints not restricted to the median nerve territory) CTS, respectively. Another 35.0% reported partial recovery [6]. Moreover, in patients with clinically defined CTS, but normal electrodiagnostic studies (EDX), effectiveness of CTS after 6 months has been proven [11]. Mean follow-up for these three groups together was approximately 8 months.
Resolution of symptoms may, however, not occur before 9 months or more, and recurrence of symptoms has been reported to start from 3 months up to 4 years after CTR [17, 23, 26]. In addition, strength and hand function may not improve significantly until after 24 months [12]. These results highlight the importance of long-term follow-up data of CTR exceeding 24 months, in order to capture the full range of clinical outcome. We hypothesized that long-term outcome after CTR is favorable and that further improvement after 8 months still occurs. The aims of this study are to explore the long-term outcome of CTR in patients of our initial studies and to identify prognostic factors for long-term outcome.
Methods and materials
Patients
Patients referred because of a suspicion of a CTS were included during the period 2007–2009 and prospectively followed if they fulfilled the clinical criteria for CTS and gave their written consent. The criteria for CTS were pain and/or paresthesias in the median nerve territory (whether or not including digits 4 and/or 5) and 2 or more of the following criteria: (1) nocturnal paresthesias; (2) aggravation of paresthesias by activities such as driving a car, riding a bike, holding a book, or holding a telephone; and (3) paresthesias relieved by shaking the hand (positive Flick sign) [29]. Exclusion criteria were age younger than 18 years, a significant language barrier, a history or clinical signs of polyneuropathy or known hereditary neuropathy with liability to pressure palsies, previous trauma or surgery to the wrist, a history of rheumatoid arthritis, diabetes mellitus, thyroid disease, alcoholism, arthrosis of the wrist, pregnancy, or severe atrophy of the abductor pollicis brevis muscle (APB). Permission from the local Medical Ethics Committee (Arnhem Nijmegen, NL59236.091.16) was obtained. The study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki.
Examination
Patients underwent a neurological examination, an EDX, and ultrasonography (US) in a standardized way. The neurophysiological protocol has been described previously in more detail [7]. In summary, three different EDX sensory tests were performed (DIG-4 test, DIG-1 test, and PALM test) and one motor test (distal motor latency APB muscle). Patients with absence of compound muscle action potential (CMAP) of the APB or severely reduced amplitude (i.e., < 0.6 mV) were excluded. The ultrasonographic cross-sectional area (CSA) of the median nerve was measured at the carpal tunnel inlet according to a generally accepted method [28]. Normal values were determined individually depending on the wrist circumference, described in a previous paper [8].
Surgery
All patients underwent open carpal tunnel release (CTR) within 2 months after inclusion. Surgery was performed in an identical way under local anesthesia by experienced neurosurgeons or orthopedic surgeons. An incision was made at the base of the palm of the hand. Then, the transverse carpal ligament was cut. After the ligament was cut, the skin was closed.
Questionnaires
Patients completed the widely used and validated Boston Carpal Tunnel Questionnaire (BCTQ), consisting of the Symptom Severity Scale (SSS) and Functional Status Scale (FSS) at baseline (T0) and at approximately 8 months after CTR (T1) (questionnaires were sent at 6 months, but some responded after a second call). To assess long-term follow-up (T2), in the summer of 2017, 10 years after the start of the study, patients were asked by mail to complete this questionnaire again. If they did not respond, we subsequently attempted to contact them by telephone and invited them to participate. In addition, at T1 and T2, patients rated their perceived treatment effect on a 6-point scale, with the following grades: 1 representing “I am completely asymptomatic”, 2 “I very rarely have complaints”, 3 “I occasionally have complaints”, 4 “I often have complaints”, 5 “My complaints are the same as before treatment”, and 6 representing “My complaints have increased”.
At T2, patients were also asked if they had had a second CTR because of recurrent or persisting symptoms; medical records were checked in case patients were lost to follow-up.
Statistical analysis
Statistical analyses were performed using SPSS Statistics 24.0. Comparisons between baseline data from participants of our study and of those who were lost to follow-up were assessed by applying an unpaired t test for continuous variables with normal distribution and Mann-Whitney test in case of non-normal distribution. Chi-square test was used for categorical variables. Changes in SSS and FSS during follow-up were assessed using the Wilcoxon signed rank test, and changes in 6-point scale were calculated by McNemar test.
For the sake of clinical relevancy, we reduced the 6-point scale into three categories: (a) “Full recovery” (consisting of grade 1 only); (b) “Favorable outcome” (consisting of grades 1 and 2), and (c) “Disappointing outcome” (consisting of grades 4 to 6). Odd ratios (OR) for potentially prognostic factors for full recovery were calculated applying binary logistic regression analysis. Spearman rank correlation coefficient (rs) was determined for assessment of correlations between different supposed prognostic factors and SSS as well as FSS. P < 0.05 was considered to be statistically significant. Normal distribution of data was assessed visually by plotting a histogram and performing the Kolomogorov-Smirnov method.
Results
Two-hundred and sixteen patients underwent CTR and completed the questionnaires at T0. At T1, 179 patients completed all questionnaires (4 patients delivered incomplete questionnaires, 33 declined to continue participation). After a median follow-up of 9.1 years (range 7.9–10.7 years), 146 patients were located. Out of the 134 patients still alive, 43 patients declined to continue participation and 4 patients’ addresses could not be traced, resulting in 87 patients participating in this study (response rate 40.3% of the initial group, 42.6% excluding the known deceased, see Fig. 1). Complete SSS and FSS data as well as 6-point questionnaires were available in all 87 patients. Mean age of the patients at inclusion was 50.5 ± 11.4 years (95% CI 48.1–53.0); 68 patients (78.4%) were women. Clinical features are presented in more detail in Table 1. Four patients (4.6%) underwent a repeat CTR because of persisting complaints (1) or recurrent complaints (3). There were no statistically significant differences in patient characteristics, EDX and US results at T0, SSS scores at T0 and T1, FSS score at T1, and frequency of reoperation between patients who completed long-term follow-up or those who did not (data not shown). However, in patients lost to follow-up, atrophy of APB at T0 was more frequent (18.4% vs. 6.9%, p = 0.021) and FSS at T0 was higher (2.41 ± 0.72 vs. 2.14 ± 0.66, p = 0.003).
Boston Carpal Tunnel Questionnaire
At T0, mean SSS was 2.87 ± 0.65 (95% CI 2.73–3.01) and improved after CTR to 1.54 ± 0.66 (95% CI 1.40–1.68, p < 0.001) at T1. At T2, the treatment effect appeared to persist, as SSS is 1.44 ± 0.61 (95% CI 1.31–1.57, p = 0.060). The same was seen for FSS with a mean score of 2.14 ± 0.66 (95% CI 2.00–2.29) at T0, which improved to 1.54 ± 0.65 (95% CI 1.40–1.68, p < 0.001) at T1 and 1.51 ± 0.69 (95% CI 1.36–1.66, p = 0.49) at T2 (Fig. 2).
6-point scale
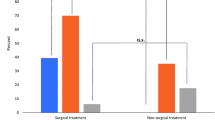
At T2, a favorable outcome (category B) was reported in 71 (81.6%) patients, 62 (71.3%) reported full recovery (category A). Fourteen patients (16.1%) had a disappointing outcome (category C). There were no statistical differences between T1 and T2, except the number of patients with full recovery which slightly increased (Table 2).
Between T1 and T2, 28 (32.2%) patients improved (Fig. 3, green zone), in 44 (50.6%) patients, no change occurred (yellow zone) and 15 (17.2%) patients deteriorated (orange zone).
Overview of the number of patients and their perceived improvement indicated on the 6-point scale at T1 and T2. A total of 87 patients completed this 6-point scale. Yellow: no change in score between T1 and T2. Green: improvement in score between T1 and T2. Orange: deterioration of score between T1 and T2
Of all patients who were free of complaints at T1 (50 patients), which is represented by the first column in the figure, 40 (80.0%) remain free of symptoms and 10 (20.0%) deteriorated at T2. Of the latter, five developed a disappointing outcome and four reported only rarely complaints.
Of the 37 patients who did not have full recovery at T1, 22 (59.5%) were asymptomatic at T2 (i.e., scoring above grade 1 at T1 and scoring at grade 1 at T2). Eight of the 15 patients (53.3%) with a disappointing outcome at T1 (i.e., grade 4.5 or 6 at T1) had a favorable outcome (i.e., grade 1 or 2) at T2. The chance to get a disappointing outcome after an initial favorable outcome is relatively low (6/65, 9.2%).
Prognostic factors
In binary logistic regression analysis, results on the 6-point scale and BCTQ at T1 appeared to be associated with outcome at T2 (Table 3). A favorable outcome at T1 especially is associated with a full recovery at T2 (OR = 4.80, p = 0.003). Electrodiagnostic test results, the BCTQ score at T0, as well as the patient characteristics and neurological examination were not associated with long-term outcome after CTR.
Comparable results are seen when these factors are correlated to the SSS and FSS at T2 (Table 4). For SSS at T2, weak correlations were found for “full recovery” (rs = − 0.289, p = 0.007), “favorable outcome” (rs = − 0.336, p = 0.001), “disappointing outcome” (rs = 0.326, p = 0.002), and FSS as well as SSS at T1 (both rs = 0.275, p = 0.010). A moderate correlation was found for FSS at T1 (rs = 0.413, p < 0.001). In addition, for FSS, weak correlations were demonstrated for “full recovery” (rs = − 0.251, p = 0.019), “favorable outcome” (rs = − 0.311, p = 0.003), and “disappointing outcome” (rs = 0.280, p = 0.009) at T1 and FSS at T0 (rs = 0.285, p = 0.007). A moderate correlation was found for FSS at T1 (rs = 0.406, p < 0.001). No correlation was demonstrated for patient characteristics, neurological examination, and electrodiagnostic test results.
Discussion
Previous studies have demonstrated excellent short-term results of CTR. This study shows that in most patients, this positive effect persists after a median of 9 years; a favorable outcome after about 8 months predicts a good outcome after 9 years.
After 9 years, SSS and FSS are still improved compared to baseline values. By applying the 6-point scale, a total of 81.6% reported a favorable outcome, most of them experienced a complete relief of complaints. A disappointing outcome was reported by 16.1%; two patients had been diagnosed with (severe) osteoarthritis during follow-up, and they assume that their progressive complaints are likely to be attributed to this comorbidity. Only 4.6% underwent a reoperation.
Our results are in accordance with scarce previous research. In a meta-analysis evaluating 13 studies about the effectiveness of CTR after 2 years, positive results were reported for CTR, with a clinical success rate varying between 75 and 90%. Recurrence rates of 3.7–57% are mentioned [17]. Nevertheless, different shortcomings of these studies were identified. Average follow-up of the reviewed studies was 4.7 years, with only one prospective study exceeding a follow-up of 7 years. As CTS is often a chronic disorder, it was stated that this duration of follow-up is possibly inadequate. Moreover, most studies have a retrospective design without pre-operative and/or short-term postoperative results to compare with the long-term data. This compromised accurate interpretation of results and therefore conclusions can be drawn on group level only, but not for individual patients. Furthermore, most studies did not use validated outcome measures. In a retrospective study, Louie et al. investigated 137 patients by validated self-administered questionnaires after a mean follow-up of 13 years. Mean SSS and FSS at follow-up were 1.3 and 1.5, respectively. Eighty-eight percent reported to be satisfied with surgery and only 8% was dissatisfied [18]. Atroshi et al. investigated the outcome of 124 patients, 11–16 years after randomization for open CTR or endoscopic CTR and also found a significant reduction of SSS and FSS 1 year after CTR, which was maintained at follow-up [1].
Several factors are shown to be potentially of prognostic value. The outcome after approximately 8 months is of most interest. Patients free of symptoms after 8 months have an 80% chance to remain asymptomatic after 9 years. In contrast, only 59.5% of patients not free of complaints after 8 months, reported full recovery after 9 years (Fig. 3). Although this can be attributed for a small part to reoperations, this observation underlines the importance of long-term follow-up. The prognostic value of short-term outcome is extensively supported by the logistic regression analyses, in which a particular high odds ratio (OR) was found for “favorable outcome” and to a lesser extent for “full recovery” at 8 months for predicting a full recovery after 9 years. A disappointing outcome soon after surgery is associated with a disappointing outcome after 9 years. Similar results for SSS and FSS at 8 months are seen. Strikingly, no baseline patient characteristics, neurological examination results, or electrodiagnostic test results were associated with long-term outcome. Baseline FSS is correlated positively with SSS and FSS after 9 years; in other words, the more problems in hand function patients experience before CTR, the more symptoms and problems in hand function they will have after CTR. Impaired hand function generally reflects more severe CTS and is associated with increased intraneuronal microvascular dysfunction and nerve fiber injury. Therefore, improvement of complaints and function can be less in these patients [15, 19]. This is supported by the finding that restriction in hand function is a predictor for worse outcome of CTR [14].
Numerous studies assessed predictors for outcome after CTR. However, most studies were retrospective and had a follow-up period with a maximum of 6 months. Results are controversial, especially for the role of EDX. Some studies demonstrate that severe EDX abnormalities are associated with a worse outcome, while other studies failed to identify EDX as prognostic factor [2,3,4,5, 9, 10, 13, 16, 22]. The value of EDX is especially demonstrated to predict a worse outcome in severe CTS compared to patients with milder CTS based on EDX abnormalities, but not between individuals in the milder categories [2, 13]. We found no relationship between pre-operative EDX and long-term outcome. A possible reason could be that we did not include patients with very severe CTS (absent CMAP of the APB or severely reduced amplitude (i.e., < 0.6 mV)). On the other hand, this result could be biased by a relative underrepresentation of people with higher baseline FSS scores and atrophy of the APB (generally more severe motor function impairment), as these patients were more likely to be lost to follow-up.
Our study has some limitations. Firstly, only 40.3% of the initial patients were in the study at T2. A relatively high loss to follow-up is not surprising after such a long period of time, as was also encountered in a previous study in this field [20]. Fortunately, baseline characteristics and outcome after about 8 months were largely comparable in those who did and did not respond at T2, so bias is expected to be limited. Secondly, we did not have a control group, so a placebo effect cannot be excluded. Moreover, outcome was assessed by patient-reported outcome measures, rather than objective measurements such as EDX. However, a lack of concordance between patient-reported symptoms and EDX had previously been reported and patients’ perceptions about symptom relief and functional improvement are more important than objective measurements [21, 25, 27]. The strengths of our study include the long-term follow-up and the prospective design, which makes it possible to compare pre- and postoperative scores accurately at different time points. Moreover, validated outcome measures were applied.
In conclusion, CTR is a robust treatment for CTS and its effect persists after a period of 9 years. The most important factor associated with long-term outcome is treatment outcome after about 8 months and to a lesser extent functional complaints preoperatively. Outcome is independent of patient characteristics, electrodiagnostic test results, or findings at the initial neurological examination.
References
Atroshi I, Hofer M, Larsson GU, Ranstam J (2015) Extended follow-up of a randomized clinical trial of open vs endoscopic release surgery for carpal tunnel syndrome. JAMA 314:1399–1401. https://doi.org/10.1001/jama.2015.12208
Bland JD (2001) Do nerve conduction studies predict the outcome of carpal tunnel decompression? Muscle Nerve 24:935–940
Braun RM, Jackson WJ (1994) Electrical studies as a prognostic factor in the surgical treatment of carpal tunnel syndrome. J Hand Surg [Am] 19:893–900. https://doi.org/10.1016/0363-5023(94)90086-8
Chen SJ, Lin HS, Hsieh CH (2013) Carpal tunnel pressure is correlated with electrophysiological parameters but not the 3 month surgical outcome. J Clin Neurosci 20:272–277. https://doi.org/10.1016/j.jocn.2012.03.032
Choi SJ, Ahn DS (1998) Correlation of clinical history and electrodiagnostic abnormalities with outcome after surgery for carpal tunnel syndrome. Plast Reconstr Surg 102:2374–2380
Claes F, Kasius KM, Meulstee J, Grotenhuis JA, Verhagen WI (2014) Treatment outcome in carpal tunnel syndrome: does distribution of sensory symptoms matter? J Neurol Sci 344:143–148. https://doi.org/10.1016/j.jns.2014.06.044
Claes F, Kasius KM, Meulstee J, Verhagen WI (2013) Comparing a new ultrasound approach with electrodiagnostic studies to confirm clinically defined carpal tunnel syndrome: a prospective, blinded study. Am J Phys Med Rehabil 92:1005–1011. https://doi.org/10.1097/PHM.0b013e31829b4bd8
Claes F, Meulstee J, Claessen-Oude Luttikhuis TT, Huygen PL, Verhagen WI (2010) Usefulness of additional measurements of the median nerve with ultrasonography. Neurol Sci 31:721–725. https://doi.org/10.1007/s10072-010-0258-9
Concannon MJ, Gainor B, Petroski GF, Puckett CL (1997) The predictive value of electrodiagnostic studies in carpal tunnel syndrome. Plast Reconstr Surg 100:1452–1458
Conzen C, Conzen M, Rubsamen N, Mikolajczyk R (2016) Predictors of the patient-centered outcomes of surgical carpal tunnel release - a prospective cohort study. BMC Musculoskelet Disord 17:190. https://doi.org/10.1186/s12891-016-1046-3
De Kleermaeker F, Meulstee J, Claes F, Kasius KM, Verhagen WIM (2017) Treatment outcome in patients with clinically defined carpal tunnel syndrome but normal electrodiagnostic test results: a randomized controlled trial. J Neurol 264:2394–2400. https://doi.org/10.1007/s00415-017-8637-2
Katz JN, Fossel KK, Simmons BP, Swartz RA, Fossel AH, Koris MJ (1995) Symptoms, functional status, and neuromuscular impairment following carpal tunnel release. J Hand Surg [Am] 20:549–555. https://doi.org/10.1016/S0363-5023(05)80265-5
Kronlage SC, Menendez ME (2015) The benefit of carpal tunnel release in patients with electrophysiologically moderate and severe disease. J Hand Surg [Am] 40(438–444):e431. https://doi.org/10.1016/j.jhsa.2014.12.012
Kulick MI, Gordillo G, Javidi T, Kilgore ES Jr, Newmayer WL 3rd (1986) Long-term analysis of patients having surgical treatment for carpal tunnel syndrome. J Hand Surg [Am] 11:59–66
Leit ME, Weiser RW, Tomaino MM (2004) Patient-reported outcome after carpal tunnel release for advanced disease: a prospective and longitudinal assessment in patients older than age 70. J Hand Surg [Am] 29:379–383. https://doi.org/10.1016/j.jhsa.2004.02.003
Longstaff L, Milner RH, O'Sullivan S, Fawcett P (2001) Carpal tunnel syndrome: the correlation between outcome, symptoms and nerve conduction study findings. J Hand Surg (Br) 26:475–480. https://doi.org/10.1054/jhsb.2001.0616
Louie D, Earp B, Blazar P (2012) Long-term outcomes of carpal tunnel release: a critical review of the literature. Hand (N Y) 7:242–246. https://doi.org/10.1007/s11552-012-9429-x
Louie DL, Earp BE, Collins JE, Losina E, Katz JN, Black EM, Simmons BP, Blazar PE (2013) Outcomes of open carpal tunnel release at a minimum of ten years. J Bone Joint Surg Am 95:1067–1073. https://doi.org/10.2106/JBJS.L.00903
Luchetti R, Schoenhuber R, Alfarano M, Montagna G, Pederzini L, Soragni O (1991) Neurophysiological assessment of the early phases of carpal tunnel syndrome with the inching technique before and during operation. J Hand Surg (Br) 16:415–419
Means KR Jr, Dubin NH, Patel KM, Pletka JD (2014) Long-term outcomes following single-portal endoscopic carpal tunnel release. Hand (N Y) 9:384–388. https://doi.org/10.1007/s11552-014-9614-1
Mondelli M, Reale F, Padua R, Aprile I, Padua L (2001) Clinical and neurophysiological outcome of surgery in extreme carpal tunnel syndrome. Clin Neurophysiol 112:1237–1242
Mondelli M, Reale F, Sicurelli F, Padua L (2000) Relationship between the self-administered Boston questionnaire and electrophysiological findings in follow-up of surgically-treated carpal tunnel syndrome. J Hand Surg (Br) 25:128–134. https://doi.org/10.1054/jhsb.2000.0361
Nancollas MP, Peimer CA, Wheeler DR, Sherwin FS (1995) Long-term results of carpal tunnel release. J Hand Surg (Br) 20:470–474
Padua L, Coraci D, Erra C, Pazzaglia C, Paolasso I, Loreti C, Caliandro P, Hobson-Webb LD (2016) Carpal tunnel syndrome: clinical features, diagnosis, and management. Lancet Neurol 15:1273–1284. https://doi.org/10.1016/S1474-4422(16)30231-9
Schrijver HM, Gerritsen AA, Strijers RL, Uitdehaag BM, Scholten RJ, de Vet HC, Bouter LM (2005) Correlating nerve conduction studies and clinical outcome measures on carpal tunnel syndrome: lessons from a randomized controlled trial. J Clin Neurophysiol 22:216–221
Soltani AM, Allan BJ, Best MJ, Mir HS, Panthaki ZJ (2014) Revision decompression and collagen nerve wrap for recurrent and persistent compression neuropathies of the upper extremity. Ann Plast Surg 72:572–578. https://doi.org/10.1097/SAP.0b013e3182956475
Tang CQY, Lai SWH, Tay SC (2017) Long-term outcome of carpal tunnel release surgery in patients with severe carpal tunnel syndrome. Bone Joint J 99-B:1348–1353. https://doi.org/10.1302/0301-620X.99B10.BJJ-2016-0587.R2
Visser LH, Smidt MH, Lee ML (2008) High-resolution sonography versus EMG in the diagnosis of carpal tunnel syndrome. J Neurol Neurosurg Psychiatry 79:63–67. https://doi.org/10.1136/jnnp.2007.115337
Witt JC, Hentz JG, Stevens JC (2004) Carpal tunnel syndrome with normal nerve conduction studies. Muscle Nerve 29:515–522. https://doi.org/10.1002/mus.20019
Acknowledgments
The authors would like to thank all the participants who participated in this study.
Funding
This research received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Permission from the local Medical Ethics Committee (Arnhem Nijmegen) was obtained. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Presentation at a conference
Not applicable.
Clinical trial number
Not applicable.
Additional information
Comments
This is a well designed prospective study that looks at the outcome of patients undergoing open Carpal Tunnel Release surgery at both intermediate (8 months) and long (9 years) term postoperative time points. The results are in line with other retrospective, prospective, and the few randomized clinical trial studies that have been done. However there are few studies that have looked at the results at such long term postoperative time points and correlated outcome, both intermediate and long term, with both preoperative baseline clinical features, as assessed by standardized and validated questionnaires, and diagnostic test results (using both electrodiagnostic and ultrasound modalities). This study confirms that patients can continue to improve over many years and that such improvement is maintained in the majority of patients. It is not surprising that the few patients with very severe disease did not have a high success rate. It is also reassuring that only a few patients underwent a re-operation. This study has limitations which are well described in the discussion. Overall, it makes an important contribution to the literature confirming the long term benefits of Carpal Tunnel Release Surgery.
Michel Kliot
CA, USA
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Peripheral Nerves
Rights and permissions
About this article
Cite this article
De Kleermaeker, F.G.C.M., Meulstee, J., Bartels, R.H.M.A. et al. Long-term outcome after carpal tunnel release and identification of prognostic factors. Acta Neurochir 161, 663–671 (2019). https://doi.org/10.1007/s00701-019-03839-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-03839-y