Abstract
Bone morphogenetic proteins (BMPs)/growth and differentiation factors (GDFs) are involved not only in the physiological development of skeletal tissues but also in the pathological conditions in the tissues. Osteogenesis and chondrogenesis during skeletal formation can be studied in vitro using cell lines and primary cultured cells, which are able to differentiate into osteoblasts and chondrocytes in response to BMP/GDF signaling. These in vitro model systems have been applied to the examination of molecular mechanisms of skeletal disorders related to BMPs/GDFs. Moreover, these in vitro model systems are useful for the development of novel treatments for the disorders.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
Osteogenic members of the transforming growth factor -β (TGF-β) family, such as bone morphogenetic proteins (BMPs) and growth and differentiation factors (GDFs), regulate skeletal development during embryogenesis and tissue regeneration in various vertebrates [1, 2]. Optimal activity of BMPs and GDFs is required for normal skeletal tissue because inadequate activity or overactivity causes skeletal disorders in humans and other animals (please see other chapters for details). As Marshall R. Urist originally reported [3], new bone formation is induced by osteogenic BMPs and GDFs in vivo. It has been reported that the implantation of a pharmacological dosage of BMPs or GDFs induces chondrocytes and osteoblasts in the implants within a week [4–8], suggesting that those osteogenic ligands directly regulate differentiation of chondrocytes and osteoblasts from progenitor cells. In this chapter, I will describe in vitro assay models to study molecular mechanisms underlying skeletal disorders in humans.
1 Phenotypic Markers of Skeletal Tissue-Forming Cells
1.1 Osteoblasts
Osteoblasts are unique and specialized cells that form bone tissue in vivo [9–11]. They are believed to develop from undifferentiated mesenchymal cells during embryonic development. The bone-forming osteoblasts secrete typical organic components of bone matrices, such as type I collagen, bone sialoprotein, osteonectin, and osteocalcin [9–11]. Moreover, osteoblasts regulate the accumulation of minerals, such as hydroxyapatite (calcium phosphate) crystals, in the organic bone matrix (osteoid) by removing pyrophosphate with high alkaline phosphatase (ALP) activity [9]. Osteoclast-dependent bone resorption is indirectly regulated by osteoblasts via expression of receptor activated nuclear factor-kB ligand (RANKL) and its decoy receptor osteoprotegerin (OPG) as well as macrophage colony-stimulating factor (M-CSF) [10, 12, 13]. These differentiations and functions of osteoblasts are regulated by various extracellular stimuli, including a calcium hormone, parathyroid hormone (PTH), various cytokines, and growth factors. Runx2 and Osterix are transcription factors abundantly expressed in osteoblasts. Thus, the expression levels of these phenotypic markers are examined to study osteoblast differentiation in vitro.
1.2 Chondrocytes
Although chondrocytes, similar to osteoblasts, are also derived from undifferentiated mesenchymal cells, they are specialized cells that form cartilage tissue, which is a template before bone formation in endochondral ossification [11, 14–16]. Commitment of chondrocyte differentiation in progenitor cells is regulated by critical transcription factors, such as SOX9, SOX5, and SOX6 [11, 14–16]. Type II collagen and aggrecan are abundantly secreted by proliferating chondrocytes in growth plates. Terminally differentiated hypertrophic chondrocytes express type X collagen, metalloproteinase-13 (MMP-13), and ALP and induce a transition from cartilage to bone tissues [11, 14–16].
2 C2C12 Myoblasts for BMP/GDF Research
2.1 C2C12 Myoblasts
The murine myoblast cell line C2C12 was originally established from regenerating thigh muscle for studying the molecular mechanisms of myogenesis [17]. Indeed, C2C12 myoblasts proliferate as mononuclear cells expressing MyoD, a skeletal muscle-specific transcription factor, and differentiate into myocytes expressing proteins for muscle contraction such as myosin heavy chain and troponin T (Fig. 1). The cells fuse together and form multinucleated myotubes in vitro (Fig. 1). However, C2C12 myoblasts are also widely used for studying BMP signaling and BMP-induced osteoblastic differentiation.
2.2 Osteoblastic Differentiation of C2C12 Myoblasts by BMPs
In the early 1990s, just after molecular cloning of several BMPs, in in vitro assay systems that reflect the bone-inducing activity of BMPs in vivo were developed [18–21]. These systems allowed the evaluation of biological activity of each recombinant BMP produced, which was needed to study intracellular signal transduction of BMPs. Among the cells examined, C2C12 myoblasts showed the high response to BMP-2, which was evaluated by the induction of ALP activity in vitro [20]. Moreover, the expression of other phenotypic markers related to osteoblast differentiation, such as osteocalcin secretion and PTH receptor, were also induced by the treatment with BMP-2 in C2C12 cells [20]. In contrast, the C2C12 myoblasts treated with BMP-2 were suppressed to express markers related to skeletal muscle differentiation, such as myogenin, myosin heavy chain, and troponin T, and they remained as mononuclear cells [20]. Although BMP-2 induced the expression of type II collagen mRNA and small droplets stained with oil red-O staining, it was still unclear whether chondrogenesis and/or adipogenesis occurred in the cells.
It has been reported that TGF-β1 does not induce heterotopic ossification in vivo [22]. In C2C12 cell cultures in vitro, TGF-β1 has been shown to inhibit myogenesis, but it does not induce any markers related to osteoblast differentiation in vitro [20]. Other inhibitors of myogenesis, such as fibroblast growth factors (FGFs), suppress myogenesis of C2C12 myoblasts but do not induce the markers of osteoblastic differentiation, suggesting that the inducing capacity of osteoblastic differentiation of C2C12 cells is limited for the osteogenic members of the TGF-β family. In addition, all-trans-retinoic acid has been shown to induce ALP activity in C2C12 and another mesenchymal cell line, C3H101/2 clone 8, but it does not induce other markers related to osteoblast differentiation [20]. Together, these findings suggest that C2C12 cells can reflect the osteogenic and non-osteogenic activities of the members of TGF-β family in vitro.
The differentiation capacity of C2C12 cells into osteoblastic cells in vitro has been applied to evaluate osteogenic activity of 14 types of human BMP (BMP-2 through BMP-15), which were individually overexpressed in the cells using adenovirus vectors [23, 24]. In the assay, not only BMP-2 but also BMP-4, BMP-6, BMP-7, and BMP-9 have been found to induce ALP activity [23, 24]. After transplantation of these C2C12 cells expressing each BMP in mice, BMP-2, BMP-6, BMP-7, and BMP-9 have been found to induce heterotopic ossification in vivo [24]. It is possible that the failure of BMP-4 to induce heterotopic ossification in vivo was due to rapid diffusion of the ligand.
2.3 Applications of C2C12 Myoblasts for Signaling Molecules of BMPs/GDFs
The osteoblastic differentiation of C2C12 cells in response to osteogenic BMPs is clear and easily detectable because the basal levels of ALP or osteocalcin expression are quite low in the untreated C2C12 cells. Thus, this cell line has been used to elucidate intracellular signaling molecules of BMPs, and the findings have been expanded to studies of human skeletal disorders related to BMPs later.
2.3.1 Receptors
Osteogenic BMPs and GDFs bind to type II receptors (BMPR-II, ActR-IIA, and ActR-IIB) and type I receptors (ALK1, ALK2, ALK3, and ALK6) [25–31], and they are expressed in C2C12 cells even though ALK1 and ALK6 are quite low [32, 33]. Each BMP and GDF binds to various combinations of the type I and type II receptors that are expressed on target cell plasma membranes and activates intracellular signaling.
Both types of receptors are transmembrane serine/threonine kinase. Although type II receptors are active regardless of ligand binding, type I receptors are inactive and activated by type II receptors via phosphorylation at the glycine/serine rich domain (GS domain) in the intracellular region at the juxtamembrane [25–31]. Type I receptors, rather than type II receptors, determine intracellular signaling pathways. Overexpression of constitutively active forms of type I receptors for osteogenic BMPs and GDFs (ALK1, ALK2, ALK3, or ALK6) in C2C12 cells can inhibit myogenesis and induce osteoblastic differentiation without the addition of exogenous ligands [33–35]. In contrast, overexpression of dominant negative forms of type I receptors, which have the extracellular ligand-binding domain and transmembrane domain but lack a functional intracellular kinase domain, inhibits osteoblastic differentiation of C2C12 cells even in the presence of ligands [32]. These findings support a hypothesis that type I receptors are downstream effectors of type II receptors.
2.3.2 Transcription Factors
The type I receptors bound to osteogenic ligands phosphorylate intracellular signaling molecules in the cytoplasm and subsequently transduce intracellular signaling. Smad1, Smad5, and Smad9 (also known as Smad8) are known as major substrates critical for downstream signaling [25–31]. The type I receptors phosphorylate two serine residues in the serine-valine-serine (SVS) motif at the carboxyl termini of these Smad proteins [25–31]. The phosphorylation of the carboxyl termini leads to a conformational change of Smad proteins and allows them to form complexes with other transcriptional regulators, such as coactivators and corepressors including Smad4 and RAN-binding domain-containing protein 2, respectively [36–38].
Indeed, co-expression of a constitutively active type I receptor kinase, with Smad1 or Smad5, which is a substrate of the receptor kinase, induces osteoblastic differentiation of C2C12 cells [39–41]. This induction is blocked by addition of a small molecule inhibitor of type I receptor kinases, such as LDN-193189 and LDN-212854, thus supporting that the kinase activity of type I receptors is essential for intracellular signal transduction through Smad proteins [39–41].
Stimulation of cells with a ligand of BMP/GDF members activates multiple intracellular signaling pathways, including Smad1, Smad5, Smad9, phosphatidylinositol-3 kinase, and p38 mitogen activated protein kinase. C2C12 cells have been used to examine the role of each Smad pathway in osteoblastic differentiation. To activate only one phosphorylated Smad without activating the others, the constitutively activated forms of Smad1, Smad5, and Smad9 have been generated by substituting the SVS motif with the DVD sequence in each Smad [36, 38]. The DVD forms of Smad1, Smad5, and Smad9 are recognized by an antibody against phosphorylated Smad1/Smad5/Smad9 [36, 38]. Moreover, they activate transcription of target genes and osteoblastic differentiation of C2C12 cells without addition of ligands or active receptors [36, 38]. However, Smad9 shows weaker transcriptional activity than Smad1 and Smad5 and fails to activate osteoblastic differentiation of the cells, owing to a deletion of a small part of the linker region [38]. Interestingly, expression of Smad9 mRNA has been found to be induced by BMP-4 stimulation in C2C12 cells, similarly to that of an inhibitory Smad, Smad6 [38]. Although Smad6 suppresses BMP receptors, Smad9 suppresses a constitutively active form of Smad1 as a dominant negative Smad [38].
Osterix (also known as SP7) is a transcription factor essential for bone formation during embryogenesis in mice. Osterix was identified as a novel transcription factor in C2C12 cells stimulated with BMP [42]. Osterix-deficient mice lack bone formation due to a loss of osteoblast differentiation similarly to Runx2-deficient mice. A premature natural mutation of Osterix/SP7 has been identified in a patient with osteogenesis imperfecta, type XII (MIM: 613849) [43]. Heterozygous loss-of-function mutation of RUNX2 has been found in patients with cleidocranial dysplasia (MIM: 119600) [44–46].
2.3.3 Early Response Genes of BMP Signaling
Although BMP/GDF proteins are multifunctional growth factors, they activate transcription of common genes within an hour after binding in various types of cells. The inhibitor of differentiation/DNA binding (Id) genes, Id1, Id2, and Id3, have been identified as the early responsive genes of BMP signaling [47, 48]. The regulatory elements in their 5′ enhancer regions have a conserved GGCGCC sequence, which is recognized by a complex of Smad1/5 and Smad4 [47, 48]. The same sequence has been found in the 5′ region of BMP-inducible transcript-1, which is also induced by BMP signaling within an hour [48]. The regulatory regions of the BMP early responsive genes can be placed in front of the luciferase gene to examine quantitatively examine BMP-specific intracellular signaling [47, 48]. However, the direct targets of Smad proteins, which regulate osteoblastic differentiation upstream of Osterix and/or Runx2 in the BMP/GDF signaling pathway, still need to be clarified.
3 Models of Chondrogenesis
Because osteogenic BMPs and GDFs induce cartilage before the induction of bone tissue in vivo, the differentiation of chondrocytes in response to ligands are examined in vitro.
3.1 Skeletal Muscle Cells
The induction of cartilage in skeletal muscle by BMPs in vivo suggests that skeletal muscle contains progenitor cells of chondrocytes. Thus, the minced skeletal muscle has been cultured on the demineralized bone matrix to examine the chondrogenesis in vitro [49]. Histological analysis has identified chondrocytes in the cavities formed in the bone matrix, confirming that the possibility of the presence of chondrocyte progenitor cells in the skeletal muscle [49]. Chondrogenesis-inducing activity in the extracts of the demineralized bone matrix has been examined in vitro using skeletal muscle cells embedded in agarose by monitoring synthesis of cartilage-specific proteoglycans [50]. Recent studies of cell lineage tracing using fluorescent proteins have revealed that the progenitor cells in the skeletal muscle tissue, which differentiate into chondrocytes and/or osteoblasts in response to BMP signaling, are interstitial mesenchymal cells, not satellite cells or endothelial cells [51].
3.2 Embryonic Fibroblasts, Embryonic Stem Cells, and Induced Pluripotent Stem Cells
Embryonic fibroblasts and embryonic stem (ES) cells are used in vitro as sources of pluripotent cells. In these types of cells, chondrogenesis is inducible in pellet cultures in the presence of TGF-β and/or BMPs. Cells prepared from chicken or mouse embryonic limb buds also show the chondrogenic activity in high-density micromass cultures. Recently, induced pluripotent stem (iPS) cells established from patients with skeletal disorders have also been used in chondrogenesis in vitro.
4 Analysis of Skeletal Disorders Related to BMP Activity In Vitro
4.1 Fibrodysplasia Ossificans Progressiva
Fibrodysplasia ossificans progressiva (FOP) (MIM: 135100) is a rare disorder characterized by progressive heterotopic ossification in soft tissues, such as skeletal muscle, tendon, and ligaments, after birth [27, 28, 52]. Although the soft tissues are almost normal at birth, muscle trauma induces an acute heterotopic ossification. The incidence of FOP is estimated to be one in two million, regardless of race, gender, location, or age [52]. The involvement of BMP signaling has been suggested in heterotopic ossification in FOP [53]. Although there is no approved treatment for inhibiting heterotopic ossification in FOP, the in vitro models are useful for studying the molecular mechanisms of the disease and the development of novel treatments.
4.1.1 Functional Changes of ALK2/ACVR1 in FOP
In 2006, a recurrent mutation in both familial and sporadic cases of FOP was identified in one BMP type I receptor, ALK2/ACVR1 [54]. The mutation, c.617G>A, causes an Arg to His substitution mutation of ALK2 at position 206 (p.R206H) in the GS domain, which is a phosphorylation site of BMP type II receptors [54]. The mutation changes conformation of the GS domain and affects the interaction between the GS domain and kinase domain.
Functional changes of the mutant ALK2 has been examined in vitro using C2C12 cells. Transient overexpression of ALK2(R206H) in C2C12 cells induces phosphorylation of Smad1/Smad5/Smad9 and activates a BMP-specific luciferase reporter driven by an enhancer region of the early responsive gene of BMP signaling, such as Id1 [39–41]. ALP activity, a typical marker of osteoblastic differentiation of C2C12 cells, is also induced when ALK2(R206H) is co-expressed with Smad1 or Smad5 [39–41]. Moreover, myogenesis of is suppressed in the ALK(R206H)-expressing C2C12 cells [39, 40]. These BMP activities induced by the mutant ALK2 are blocked by treatment with a small chemical inhibitor against BMP type I receptor kinases [39–41], suggesting that the kinase activity of the mutant ALK2 is increased and phosphorylated Smad1 and/or Smad5 mediate the biological activity of the receptor.
4.1.2 Molecular Mechanisms of the Activation of ALK2 in FOP
To date, more than 10 different mutations in the intracellular region, such as the GS domain and the kinase domain, of ALK2 have been identified from patients with typical or atypical FOP [28, 29]. All of the mutant ALK2 identified activate BMP signaling when they are overexpressed in C2C12 cells, although some mutants show quite weak activity [55]. FKBP12, a small binding protein for an immunosuppressor FK506, has been shown to bind to type I receptors for the TGF-β family and stabilize the inactive state of the kinase [56]. Crystal structures of the cytoplasmic domain of ALK2 and FKBP12 have revealed that the FOP mutations break critical interactions with FKBP12 [57].
In C2C12 cells, co-expression of BMP type II receptor, such as BMPR-II or ActR-IIB but not ActR-IIA, synergistically increases the kinase activity of the mutant forms of ALK2 associated with FOP but not the wild type or associated with heart diseases [55]. This stimulation depends on the kinase activity of the type II receptors. ALK2(Q207D), a constitutively active form created by genetic engineering, is activated even by the kinase activity-deficient type II receptors in C2C12 cells [55]. This suggests that the mutant forms of ALK2 associated with FOP are not constitutively active but require upstream effectors, such as type II receptors and possible ligands [55]. The threonine residue at position 203 in ALK2 is essential for the type II receptor-dependent activation of BMP signaling through regulating the phosphorylation levels of ALK2 by the type II receptors [55]. Moreover, the conserved Thr residues in other BMP type I receptors, such as ALK1, ALK3, and ALK6, are also required for the ligand-induced intracellular signaling [55].
Recently, Activin A, which is a non-osteogenic member of the TGF-β family, has been shown to activate BMP-like activity in cells expressing ALK2(R206H) [58]. Moreover, anti-Activin A antibody suppressed heterotopic ossification in conditional-on knock-in mice of human ALK2(R206H) [58]. These findings suggest that heterotopic ossification in patients with FOP is a ligand-dependent event, and Activin A is responsible for it.
4.1.3 Chondrogenesis Models in Vitro for FOP
Heterotopic skeletal tissues in FOP are formed through an endochondral ossification process, suggesting that mutant forms of ALK2 induce chondrocyte differentiation in progenitor cells in the soft tissues.
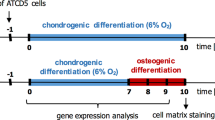
Murine ES cells that express human ALK2(R206H) under the control of the Tet-off system have been established, and their chondrogenic capacity in vitro has been analyzed [59]. Withdrawal of doxycycline from the culture medium induces the expression of ALK2(R206H), the phosphorylation of Smad1/5 and the expression of markers related to chondrocyte differentiation, such as type II collagen and aggrecan [59]. As expected, a small chemical inhibitor of the BMP type I receptor kinases inhibits these doxycycline-dependent events except for the expression of human ALK2 [59].
Knock-in mice of the ALK2(R206H) mutation have been examined. Although they show the malformation of great toe and the heterotopic ossification in soft tissues, similarly to patients with FOP, these mice die after birth [60]. Embryonic fibroblasts prepared from the knock-in mice show enhanced chondrogenic activity in vitro compared to that of wild-type mice [61]. iPS cells have been established from patients with typical FOP who carry the R206H mutation [62]. The iPS cells show accelerated chondrogenic ability in vitro compared to that of the gene-corrected and rescued iPS cells [63].
4.2 Brachydactyly, Symphalangism, and Multiple Synostosis Syndrome
Among BMPs/GDFs, GDF5 is a key regulator of skeletal development during embryogenesis, especially for digit and joint formation. Loss-of-function and gain-of-function mutations have been identified in a ligand (GDF5), receptor (BMPR-IB/ALK6), and antagonist (Noggin) in patients with skeletal disorders, such as brachydactyly, symphalangism, and multiple synostosis syndrome.
4.2.1 Gain-of-Function and Loss-of Function Mutations in GDF5
Human GDF5 has been shown to be mutated in skeletal malformation syndromes including brachydactyly type C (BDC) (MIM: 113100), which is characterized by the shortening of digits and hypersegmentation of phalanges and the recessive acromesomelic dysplasias of the Hunter-Thompson, Grebe, and DuPan types, which are characterized by short stature, severe limb shortening, and profound brachydactyly.
A mutation of p.L441P in GDF5 has been identified from patients showing short index fingers and variable clinodactyly, similarly to the patients with brachydactyly type A2 (BDA2) (MIM: 112600), which is caused by a mutation in BMPR-IB/ALK6 [64]. Another mutation in GDF5, p.R438L, has been identified in patients with proximal symphalangism (SYM1) (MIM: 185800) and is characterized by a bony fusion between the proximal and middle phalanges in the digits [64]. C2C12 cells express BMPR-IA/ALK3, but they do not express functional levels of BMPR-IB/ALK6. Thus, the cells respond to BMP-2, but they do not respond to GDF5 [64]. GDF5 stimulates chondrogenesis of chicken limb bud cells in micromass cultures [64]. The p.L441P mutant GDF5 seems to be a loss-of-function mutation because it does not show BMP/GDF-like activity in vitro [64]. In contrast, the p.R438L mutant is a gain-of-function mutation, because it has increased in binding affinity to BMPR-IA/ALK3 [64]. The p.R438L mutant GDF5, but not p.L441P, induces ALP activity in C2C12 cells and suppresses myogenesis similarly to BMP-2 [64].
Additional mutations in GDF5, p.N445T/K, and p.W414R have been identified from patients with SYM1 and combined clinical features of brachydactyly type A2 (BDA2) and multiple synostosis syndrome 2 (SYNS2) (MIM: 610017), respectively [65]. These mutant GDF5 are insensitive and resistant to Noggin, similarly to BMP-9 and BMP-10 [65]. Overexpression of the mutant GDF5 or BMP-9 in the micromass cultures of chicken limb bud cells shows high chondrogenic activity [65], suggesting that normal joint formation induced by GDF5 requires a negative feedback through an antagonist, i.e., Noggin.
5 Conclusion
The original bone-inducing activity of BMPs can be reflected, at least in part, in in vitro model systems using cell lines or primary cultured cells. These systems have been applied to the examination of molecular mechanisms of skeletal disorders related to BMPs/GDFs. Moreover, these in vitro model systems are useful for the development of novel treatments for the disorders.
References
Jin L, Li X (2013) Growth differentiation factor 5 regulation in bone regeneration. Curr Pharm Des 19(19):3364–3373
Pignatti E, Zeller R, Zuniga A (2014) To BMP or not to BMP during vertebrate limb bud development. Semin Cell Dev Biol 32:119–127
Urist MR (1965) Bone: formation by autoinduction. Science 150:893–899
Wozney JM, Rosen V, Celeste AJ, Mitsock LM, Whitters MJ, Kriz RW, Hewick RM, Wang EA (1988) Novel regulators of bone formation: molecular clones and activities. Science 242(4885):1528–1534
Celeste AJ, Iannazzi JA, Taylor RC, Hewick RM, Rosen V, Wang EA, Wozney JM (1990 Dec) Identification of transforming growth factor beta family members present in bone-inductive protein purified from bovine bone. Proc Natl Acad Sci U S A 87(24):9843–9847
Sampath TK, Coughlin JE, Whetstone RM, Banach D, Corbett C, Ridge RJ, Ozkaynak E, Oppermann H, Rueger DC (1990) Bovine osteogenic protein is composed of dimers of OP-1 and BMP-2A, two members of the transforming growth factor-beta superfamily. J Biol Chem 265(22):13198–13205
Sampath TK, Maliakal JC, Hauschka PV, Jones WK, Sasak H, Tucker RF, White KH, Coughlin JE, Tucker MM, Pang RH et al (1992) Recombinant human osteogenic protein-1 (hOP-1) induces new bone formation in vivo with a specific activity comparable with natural bovine osteogenic protein and stimulates osteoblast proliferation and differentiation in vitro. J Biol Chem 267(28):20352–20362
Chang SC, Hoang B, Thomas JT, Vukicevic S, Luyten FP, Ryba NJ, Kozak CA, Reddi AH, Moos M Jr (1994) Cartilage-derived morphogenetic proteins. New members of the transforming growth factor-beta superfamily predominantly expressed in long bones during human embryonic development. J Biol Chem 269(45):28227–28234
Yamaguchi A, Komori T, Suda T (2000) Regulation of osteoblast differentiation mediated by bone morphogenetic proteins, hedgehogs, and Cbfa1. Endocr Rev 21(4):393–411
Katagiri T, Takahashi N (2002) Regulatory mechanisms of osteoblast and osteoclast differentiation. Oral Dis 8(3):147–159
Gómez-Picos P, Eames BF (2015) On the evolutionary relationship between chondrocytes and osteoblasts. Front Genet 6:297
Nakamura I, Takahashi N, Jimi E, Udagawa N, Suda T (2012 Apr) Regulation of osteoclast function. Mod Rheumatol 22(2):167–177
Kobayashi Y, Uehara S, Koide M, Takahashi N (2015 Jul 1) The regulation of osteoclast differentiation by Wnt signals. Bonekey Rep 4:713
Somoza RA, Welter JF, Correa D, Caplan AI (2014) Chondrogenic differentiation of mesenchymal stem cells: challenges and unfulfilled expectations. Tissue Eng Part B Rev 20(6):596–608
Jiang Y, Tuan RS (2015) Origin and function of cartilage stem/progenitor cells in osteoarthritis. Nat Rev Rheumatol 11(4):206–212
Abdallah BM, Jafari A, Zaher W, Qiu W, Kassem M (2015) Skeletal (stromal) stem cells: an update on intracellular signaling pathways controlling osteoblast differentiation. Bone 70:28–36
Blau HM, Chiu CP, Webster C (1983) Cytoplasmic activation of human nuclear genes in stable heterocaryons. Cell 32:1171–1180
Katagiri T, Yamaguchi A, Ikeda T, Yoshiki S, Wozney JM, Rosen V, Wang EA, Tanaka H, Omura S, Suda T (1990) The non-osteogenic mouse pluripotent cell line, C3H10T1/2, is induced to differentiate into osteoblastic cells by recombinant human bone morphogenetic protein-2. Biochem Biophys Res Commun 172(1):295–299
Yamaguchi A, Katagiri T, Ikeda T, Wozney JM, Rosen V, Wang EA, Kahn AJ, Suda T, Yoshiki S (1991) Recombinant human bone morphogenetic protein-2 stimulates osteoblastic maturation and inhibits myogenic differentiation in vitro. J Cell Biol 113(3):681–687
Katagiri T, Yamaguchi A, Komaki M, Abe E, Takahashi N, Ikeda T, Rosen V, Wozney JM, Fujisawa-Sehara A, Suda T (1994) Bone morphogenetic protein-2 converts the differentiation pathway of C2C12 myoblasts into the osteoblast lineage. J Cell Biol 127(6 Pt 1):1755–1766
Rosen V, Nove J, Song JJ, Thies RS, Cox K, Wozney JM (1994) Responsiveness of clonal limb bud cell lines to bone morphogenetic protein 2 reveals a sequential relationship between cartilage and bone cell phenotypes. J Bone Miner Res 9(11):1759–1768
Sampath TK, Muthukumaran N, Reddi AH (1987) Isolation of osteogenin, an extracellular matrix-associated, bone-inductive protein, by heparin affinity chromatography. Proc Natl Acad Sci U S A 84(20):7109–7113
Cheng H, Jiang W, Phillips FM, Haydon RC, Peng Y, Zhou L, Luu HH, An N, Breyer B, Vanichakarn P, Szatkowski JP, Park JY, He TC (2003) Osteogenic activity of the 14 types of human bone morphogenetic proteins (BMPs). J Bone Joint Surg Am 85-A(8):1544–1552 Erratum in: J Bone Joint Surg Am. 2004 Jan;86-A(1):141
Kang Q, Sun MH, Cheng H, Peng Y, Montag AG, Deyrup AT, Jiang W, Luu HH, Luo J, Szatkowski JP, Vanichakarn P, Park JY, Li Y, Haydon RC, He TC (2004) Characterization of the distinct orthotopic bone-forming activity of 14 BMPs using recombinant adenovirus-mediated gene delivery. Gene Ther 11(17):1312–1320
Katagiri T, Suda T, Miyazozo K (2008) The bone morphogenetic proteins. In: Miyazono K, Derynck R (eds) The TGF-βFamily. Cold Spring Harbor Press, New York, pp. 121–149
Miyazono K, Kamiya Y, Morikawa M (2010) Bone morphogenetic protein receptors and signal transduction. J Biochem 147:35–51
Katagiri T (2010) Heterotopic bone formation induced by bone morphogenetic protein signaling: fibrodysplasia ossificans progressiva. J Oral Biosci 52:33–41
Katagiri T (2012) Recent topics in fibrodysplasia ossificans progressiva. J Oral Biosci 54:119–123
Katagiri T, Tsukamoto S (2013) The unique activity of bone morphogenetic proteins in bone: a critical role of the Smad signaling pathway. Biol Chem 394:703–714
Katagiri T, Tsukamoto S, Osawa K, and Kokabu S. Ligand-receptor interactions and their implications in delivering certain signaling for bone regeneration. In A tissue regeneration approach to bone and cartilage repair, Mechanical Engineering Series,Zreiqat H Rosen V and Dunstan C, editors. Springer, London, pp 1–15, 2014.
Katagiri T, Osawa K, Tsukamoto S, Fujimoto M, Miyamoto A, Mizuta T (2015) Bone morphogenetic protein-induced heterotopic bone formation: what have we learned from the history of a half century? Jpn Dent Sci Rev 51:42–50
Namiki M, Akiyama S, Katagiri T, Suzuki A, Ueno N, Yamaji N, Rosen V, Wozney JM, Suda T (1997) A kinase domain-truncated type I receptor blocks bone morphogenetic protein-2-induced signal transduction in C2C12 myoblasts. J Biol Chem 272(35):22046–22052
Akiyama S, Katagiri T, Namiki M, Yamaji N, Yamamoto N, Miyama K, Shibuya H, Ueno N, Wozney JM, Suda T (1997) Constitutively active BMP type I receptors transduce BMP-2 signals without the ligand in C2C12 myoblasts. Exp Cell Res 235(2):362–369
Fujii M, Takeda K, Imamura T, Aoki H, Sampath TK, Enomoto S, Kawabata M, Kato M, Ichijo H, Miyazono K (1999) Roles of bone morphogenetic protein type I receptors and Smad proteins in osteoblast and chondroblast differentiation. Mol Biol Cell 10(11):3801–3813
Aoki H, Fujii M, Imamura T, Yagi K, Takehara K, Kato M, Miyazono K (2001) Synergistic effects of different bone morphogenetic protein type I receptors on alkaline phosphatase induction. J Cell Sci 114(Pt 8):1483–1489
Nojima J, Kanomata K, Takada Y, Fukuda T, Kokabu S, Ohte S, Takada T, Tsukui T, Yamamoto TS, Sasanuma H, Yoneyama K, Ueno N, Okazaki Y, Kamijo R, Yoda T, Katagiri T (2010) Dual roles of Smad proteins in the conversion from myoblasts to osteoblastic cells by bone morphogenetic proteins. J Biol Chem 285(20):15577–15586
Ohte S, Kokabu S, Iemura S, Sasanuma H, Yoneyama K, Shin M, Suzuki S, Fukuda T, Nakamura Y, Jimi E, Natsume T, Katagiri T (2012) Identification and functional analysis of Zranb2 as a novel Smad-binding protein that suppresses BMP signaling. J Cell Biochem 113(3):808–814
Tsukamoto S, Mizuta T, Fujimoto M, Ohte S, Osawa K, Miyamoto A, Yoneyama K, Murata E, Machiya A, Jimi E, Kokabu S, Katagiri T (2014) Smad9 is a new type of transcriptional regulator in bone morphogenetic protein signaling. Sci Rep 4:7596. doi:10.1038/srep07596
Fukuda T, Kanomata K, Nojima J, Kokabu S, Akita M, Ikebuchi K, Jimi E, Komori T, Maruki Y, Matsuoka M, Miyazono K, Nakayama K, Nanba A, Tomoda H, Okazaki Y, Ohtake A, Oda H, Owan I, Yoda T, Haga N, Furuya H, Katagiri T (2008) A unique mutation of ALK2, G356D, found in a patient with fibrodysplasia ossificans progressiva is a moderately activated BMP type I receptor. Biochem Biophys Res Commun 377(3):905–909
Fukuda T, Kohda M, Kanomata K, Nojima J, Nakamura A, Kamizono J, Noguchi Y, Iwakiri K, Kondo T, Kurose J, Endo K, Awakura T, Fukushi J, Nakashima Y, Chiyonobu T, Kawara A, Nishida Y, Wada I, Akita M, Komori T, Nakayama K, Nanba A, Maruki Y, Yoda T, Tomoda H, PB Y, Shore EM, Kaplan FS, Miyazono K, Matsuoka M, Ikebuchi K, Ohtake A, Oda H, Jimi E, Owan I, Okazaki Y, Katagiri T (2009) Constitutively activated ALK2 and increased SMAD1/5 cooperatively induce bone morphogenetic protein signaling in fibrodysplasia ossificans progressiva. J Biol Chem 284(11):7149–7156
Ohte S, Shin M, Sasanuma H, Yoneyama K, Akita M, Ikebuchi K, Jimi E, Maruki Y, Matsuoka M, Namba A, Tomoda H, Okazaki Y, Ohtake A, Oda H, Owan I, Yoda T, Furuya H, Kamizono J, Kitoh H, Nakashima Y, Susami T, Haga N, Komori T, Katagiri T (2011) A novel mutation of ALK2, L196P, found in the most benign case of fibrodysplasia ossificans progressiva activates BMP-specific intracellular signaling equivalent to a typical mutation, R206H. Biochem Biophys Res Commun 407(1):213–218
Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, de Crombrugghe B (2002) The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell 108(1):17–29
Lapunzina P, Aglan M, Temtamy S, Caparrós-Martín JA, Valencia M, Letón R, Martínez-Glez V, Elhossini R, Amr K, Vilaboa N, Ruiz-Perez VL (2010) Identification of a frameshift mutation in Osterix in a patient with recessive osteogenesis imperfecta. Am J Hum Genet 87(1):110–114
Komori T, Yagi H, Nomura S, Yamaguchi A, Sasaki K, Deguchi K, Shimizu Y, Bronson RT, Gao YH, Inada M, Sato M, Okamoto R, Kitamura Y, Yoshiki S, Kishimoto T (1997) Targeted disruption of Cbfa1 results in a complete lack of bone formation owing to maturational arrest of osteoblasts. Cell 89(5):755–764
Otto F, Thornell AP, Crompton T, Denzel A, Gilmour KC, Rosewell IR, Stamp GW, Beddington RS, Mundlos S, Olsen BR, Selby PB, Owen MJ (1997) Cbfa1, a candidate gene for cleidocranial dysplasia syndrome, is essential for osteoblast differentiation and bone development. Cell 89(5):765–771
Mundlos S, Otto F, Mundlos C, Mulliken JB, Aylsworth AS, Albright S, Lindhout D, Cole WG, Henn W, Knoll JH, Owen MJ, Mertelsmann R, Zabel BU, Olsen BR (1997) Mutations involving the transcription factor CBFA1 cause cleidocranial dysplasia. Cell 89(5):773–779
Katagiri T, Imada M, Yanai T, Suda T, Takahashi N, Kamijo R (2002) Identification of a BMP-responsive element in Id1, the gene for inhibition of myogenesis. Genes Cells 7:949–960
Shin M, Ohte S, Fukuda T, Sasanuma H, Yoneyama K, Kokabu S, Miyamoto A, Tsukamoto S, Hohjoh H, Jimi E, Katagiri T (2013) Identification of a novel bone morphogenetic protein (BMP)-inducible transcript, BMP-inducible transcript-1, by utilizing the conserved BMP-responsive elements in the Id genes. J Bone Miner Metab 31(1):34–43
Nogami H, Urist MR (1974) Substrata prepared from bone matrix for chondrogenesis in tissue culture. J Cell Biol 62:510–519
Seyedin SM, Thompson AY, Bentz H, Rosen DM, McPherson JM, Conti A et al (1986) Cartilage-inducing factor-A. Apparent identity to transforming growth factor-beta. J Biol Chem 261:5693–5695
Wosczyna MN, Biswas AA, Cogswell CA, Goldhamer DJ (2012) Multipotent progenitors resident in the skeletal muscle interstitium exhibit robust BMP-dependent osteogenic activity and mediate heterotopic ossification. J Bone Miner Res 27:1004–1017
Kitterman JA, Kantanie S, Rocke DM, Kaplan FS (2005) Iatrogenic harm caused by diagnostic errors in fibrodysplasia ossificans progressiva. Pediatrics 116(5):e654–e661
Kaplan FS, Tabas JA, Zasloff MA (1990) Fibrodysplasia ossificans progressiva: a clue from the fly? Calcif Tissue Int 47:117–125
Shore EM, Xu M, Feldman GJ, Fenstermacher DA, Cho TJ, Choi IH, Connor JM, Delai P, Glaser DL, LeMerrer M, Morhart R, Rogers JG, Smith R, Triffitt JT, Urtizberea JA, Zasloff M, Brown MA, Kaplan FS (2006) A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nat Genet 38(5):525–527
Fujimoto M, Ohte S, Osawa K, Miyamoto A, Tsukamoto S, Mizuta T, Kokabu S, Suda N, Katagiri T (2015) Mutant activin-like kinase 2 in fibrodysplasia ossificans progressiva are activated via T203 by BMP type II receptors. Mol Endocrinol 29(1):140–152
Wang T, Li BY, Danielson PD, Shah PC, Rockwell S, Lechleider RJ, Martin J, Manganaro T, Donahoe PK (1996) The immunophilin FKBP12 functions as a common inhibitor of the TGF beta family type I receptors. Cell 86(3):435–444
Chaikuad A, Alfano I, Kerr G, Sanvitale CE, Boergermann JH, Triffitt JT, von Delft F, Knapp S, Knaus P, Bullock AN (2012) Structure of the bone morphogenetic protein receptor ALK2 and implications for fibrodysplasia ossificans progressiva. J Biol Chem 287(44):36990–36998
Hatsell SJ, Idone V, Wolken DM, Huang L, Kim HJ, Wang L, Wen X, Nannuru KC, Jimenez J, Xie L, Das N, Makhoul G, Chernomorsky R, D’Ambrosio D, Corpina RA, Schoenherr CJ, Feeley K, Yu PB, Yancopoulos GD, Murphy AJ, Economides AN (2015) ACVR1R206H receptor mutation causes fibrodysplasia ossificans progressiva by imparting responsiveness to activin A. Sci Transl Med 7(303):303ra137
Fujimoto M, Ohte S, Shin M, Yoneyama K, Osawa K, Miyamoto A, Tsukamoto S, Mizuta T, Kokabu S, Machiya A, Okuda A, Suda N, Katagiri T (2014) Establishment of a novel model of chondrogenesis using murine embryonic stem cells carrying fibrodysplasia ossificans progressiva-associated mutant ALK2. Biochem Biophys Res Commun 455(3–4):347–352
Chakkalakal SA, Zhang D, Culbert AL, Convente MR, Caron RJ, Wright AC, Maidment AD, Kaplan FS, Shore EM (2012) An Acvr1 R206H knock-in mouse has fibrodysplasia ossificans progressiva. J Bone Miner Res 27(8):1746–1756
Culbert AL, Chakkalakal SA, Theosmy EG, Brennan TA, Kaplan FS, Shore EM (2014) Alk2 regulates early chondrogenic fate in fibrodysplasia ossificans progressiva heterotopic endochondral ossification. Stem Cells 32:1289–1300
Matsumoto Y, Hayashi Y, Schlieve CR, Ikeya M, Kim H, Nguyen TD, Sami S, Baba S, Barruet E, Nasu A, Asaka I, Otsuka T, Yamanaka S, Conklin BR, Toguchida J, Hsiao EC (2013) Induced pluripotent stem cells from patients with human fibrodysplasia ossificans progressiva show increased mineralization and cartilage formation. Orphanet J Rare Dis 8:190
Matsumoto Y, Ikeya M, Hino K, Horigome K, Fukuta M, Watanabe M, Nagata S, Yamamoto T, Otsuka T, Toguchida J (2015) New protocol to optimize iPS cells for genome analysis of Fibrodysplasia Ossificans Progressiva. Stem Cells 33:1730–1742
Seemann P, Schwappacher R, Kjaer KW, Krakow D, Lehmann K, Dawson K, Stricker S, Pohl J, Plöger F, Staub E, Nickel J, Sebald W, Knaus P, Mundlos S (2005) Activating and deactivating mutations in the receptor interaction site of GDF5 cause symphalangism or brachydactyly type A2. J Clin Invest 115:2373–2381
Degenkolbe E, König J, Zimmer J, Walther M, Reißner C, Nickel J, Plöger F, Raspopovic J, Sharpe J, Dathe K, Hecht JT, Mundlos S, Doelken SC, Seemann P. A GDF5 point mutation strikes twice–causing BDA1 and SYNS2. PLoS Genet 2013. 9:e1003846.
Acknowledgments
I would like to thank the members of the Division of Pathophysiology, Research Center for Genomic Medicine, Saitama Medical University for their helpful discussions. This work was supported, in part, by JSPS KAKENHI Numbers 15K15556 and 25293326 and a grant-in-aid from the Support Project for the Formation of a Strategic Center in a Private University from the Ministry of Education, Culture, Sports, Science and Technology of Japan (MEXT) (S1311002).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Katagiri, T. (2017). Novel In Vitro Assay Models to Study Osteogenesis and Chondrogenesis for Human Skeletal Disorders. In: Vukicevic, S., Sampath, K. (eds) Bone Morphogenetic Proteins: Systems Biology Regulators. Progress in Inflammation Research. Springer, Cham. https://doi.org/10.1007/978-3-319-47507-3_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-47507-3_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-47505-9
Online ISBN: 978-3-319-47507-3
eBook Packages: MedicineMedicine (R0)