Abstract
Oldest old subjects represent a fast-rising share of world population characterized by complex clinical features, including high vascular risk and uncertainty regarding risk-to-benefit ratio of antihypertensive treatment. European guidelines in 2013 have introduced the need to personalize antihypertensive treatment targets according to age and health status. Approach to clinical assessment of blood pressure in old age is peculiar, including the need for orthostatic hypotension assessment, the frequent usefulness of ambulatory blood pressure monitoring, and the role of functional and cognitive measures to screen for frailty. Observational and intervention studies published during the last years suggest that a strict BP control might be beneficial in some older subjects but might harm other ones, probably the frailest. Future epidemiological and intervention studies including specific profiles of frailty are warranted, to identify the most appropriate blood pressure targets in the perspective of personalized medicine.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Systolic Blood Pressure
- Mild Cognitive Impairment
- High Blood Pressure
- Arterial Hypertension
- Antihypertensive Treatment
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
8.1 Introduction
The importance of blood pressure (BP) assessment among oldest old is highlighted by several reasons. The most obvious one is represented by the steep increase of old age population share since 1960 and the even steeper increase forecasted during the next 30 years all over the world [1]. This increase will be multiplicative in the subgroup of subjects aged 80+, with an expected triplication by 2050 in Spain, Germany, and Japan and a seven-time increase in Korea and China [2]. The second reason of the importance and peculiarity of this population is linked to the incidence and prevalence of comorbidities, frailty, and loss of autonomy, which greatly increase among subjects aged 80+ [3]. Finally and most important, subjects in this age stratum have both highest cardiovascular risk and potentially severe adverse effects from BP treatment, with limited evidence from randomized clinical trials regarding risk and benefits of antihypertensive treatment.
In fact, while the prevalence of high BP and the risk of vascular diseases are clearly associated with old age, the risk of syncope, falls, and fractures also increases with age, with low BP representing a major risk factor [4]. Orthostatic hypotension in particular seems to be associated both with antihypertensive treatment and with an increased fall risk [5] and was also found to increase the risk for mortality and cardiovascular events in a recent meta-analysis [6]. Of notice, in a large population-based study, older subjects showed a significant increase in hospitalizations for hip fracture over the 45 days after initiation of antihypertensive drug treatment [7]. Moreover hypotension-related events in old age are likely to be more common in real life than in clinical trials in which treatment is delivered by expert physicians, and patients are followed closely. Therefore, both the benefits (including preserving autonomy) and the risks of antihypertensive therapy should be considered before starting treatment in frail older population.
Finally, the data from randomized clinical trials seem somehow at an odd with observational studies, showing that in the very old population low BP values represent a risk factor for morbidity and mortality, at least as strong as high BP [8–10]. Although the possibility of reverse causality (i.e., more severe clinical conditions in subjects with lower BP) has been advocated for these data, a pathophysiologically founded hypothesis is that in frail very old subjects an impairment of the mechanisms preserving perfusion might critically decrease blood flow to vital organs (the heart, brain, kidney) [11]. Therefore the choice of most appropriate BP target in these subjects is still a matter of debate.
8.2 Epidemiology
Arterial hypertension (AH) represents the leading risk factor for global disease burden due to its great prevalence and deep impact on morbidity and mortality [12]. Overall the prevalence of AH appears to be around 30–45 % of the general population, presenting higher values in Europe (44 %) than in the United States (28 %) [13].
Although rise of BP values is not a normal part of aging, the prevalence of AH increases progressively with age, and thus most older subjects are hypertensive [14]. Data from the Framingham Heart Study in men and women free of AH at 55 years of age indicate that the remaining lifetime risks for development of AH until the age of 80 are 93 % and 91 %, respectively [15]. In other words, more than 90 % of individuals who are free of AH at 55 years of age will develop it during their remaining life-span. Several epidemiological surveys conducted in the United States and Europe conclude that AH prevalence in the elderly ranges between 53 and 72 % [16].
From the epidemiological standpoint, there are important subgroups with distinctive characteristics. AH prevalence is less in women than in men until 45 years of age, is similar in both genders from 45 to 64 years of age, and is much higher in women than men >65 years of age. Age-adjusted AH prevalence, both diagnosed and undiagnosed, from 1999 to 2002, was 78 % for older women and only 64 % for older men [17]. Both the prevalence and severity of AH increase markedly with advancing age in women, so that, after age 60 years, a majority of women (age 60–79 years: 48.8 %; age ≥80 years: 63 %) have stage 2 AH (BP ≥160/100 mmHg) or receive antihypertensive treatment [18]. Furthermore, BP control is difficult to achieve in elderly hypertensives [19]. Thus, although older patients with AH are more likely to be aware of their condition and receiving treatment than middle-aged patients, BP control rates are lower in the elderly, especially after age 80 years [14].
AH in old age is commonly characterized by elevated systolic blood pressure (SBP), with often normal or even low diastolic blood pressure (DBP), which reflects a progressive increase in aortic stiffness during aging, in part related to increased collagen with cross-linking and degradation of elastin fibers [19]. Typically SBP rises gradually throughout adult life, while DBP peaks and plateaus in late middle age, declining slightly thereafter. The widened pulse pressure is a reflection of increased arterial stiffness [19]. Therefore, the proportion of hypertensive patients with isolated systolic hypertension increases with age, with this condition affecting 65 % of patients with AH >60 years of age and over 90 % >70 years of age [20]. The prevalence of isolated systolic hypertension is higher in women than in men, whereas the proportion of AH attributable to solely elevated SBP in older adults is similar across racial and ethnic groups [14].
White coat hypertension, a term reserved for those not on antihypertensive medications but with persistently elevated office BP (≥140/90 mmHg) together with a normal home BP or daytime ambulatory BP (≤135/85 mmHg), is also more common in the elderly and is more frequent among centenarians [21]. Masked hypertension, defined as normal office BP associated with high BP at home, is also frequent in the elderly and is associated with a high vascular risk profile [22]. Contrary to white coat hypertension, masked hypertension has been shown to be associated with an increased risk of cardiovascular events [23]. The frequency of non-dipping – defined as a nocturnal BP drop <10 % of daytime values – also increases with age [19]. As discussed below, these data should support the usefulness of home BP monitoring in elderly hypertensives.
In regard to treatment efficacy, resistant hypertension – defined as BP that remains above goal in spite of the concurrent use of three drugs at optimal dose amounts, one of whom should be a diuretic – has a substantial prevalence across all ages but is more frequent among older subjects [24].
AH is the most important risk factor for cardiovascular diseases in the elderly population, with estimates that 69 % of patients with incident myocardial infarction, 77 % with incident stroke, and 74 % with incident heart failure have antecedent AH. In addition, AH is a major risk factor for incident diabetes mellitus, as well as for atrial fibrillation and chronic kidney disease [14].
Therefore, the positive association of high BP with cardiovascular risk and mortality is maintained at higher age, although this association seems to loosen or even be reverted among very old, frail subjects [11]. Thus, despite the large body of evidence in middle-aged populations, the predictive value of high BP in the rapidly growing population of oldest old is still debated, as is the question of whether AH should be treated and if so, how intensively.
8.3 Clinical Assessment of BP in Older Subjects
8.3.1 Peculiar Aspects of BP Measurement
Recent guidelines reaffirm the need to obtain the BP measure in sitting position after 3–5 min of rest, repeating the measurement at least twice 1–2 min apart and obtaining the measure on both sides at the first visit [13]. Specific aspects of BP measurement should be cared of in aged subjects. First, the age-associated increase of arterial stiffness, apart from being a main determinant on increased SBP values in old age, may affect the risk of pseudohypertension, which is quite common in old age and is defined as a falsely heightened SBP in comparison with the intra-arterial measurement [25]. This phenomenon is explained by the increased cuff insufflation pressure needed to obtain the collapse of brachial artery walls, due to the increased rigidity of the tunica media. The presence of pseudohypertension can be suspected with the Osler’s maneuver, which is performed by assessing the palpability of the pulseless radial or brachial artery distal to the point of occlusion of the artery by cuff pressure [26]. While the Osler’s maneuver is positive in about 10 % of older subjects, its ability to detect pseudohypertension has been questioned, and the measure of upper limb pulse wave velocity has been proposed as a more appropriate way of screening for this condition [27].
With a similar mechanism, arterial stiffness may be the cause of auscultatory gap phenomenon, which is defined by decrease or disappearance of Korotkoff sounds during BP measurement. The improper interpretation of this gap may lead to BP monitoring errors, namely, an underestimation of SBP and/or an overestimation of DBP. In order to correct for an auscultatory gap, the radial pulse should be monitored by palpation. Moreover, the examiner can avoid being confused by an auscultatory gap by always inflating a BP cuff to 20–40 mmHg higher than the pressure required to occlude the brachial pulse. The presence of an auscultatory gap has been associated with carotid atherosclerosis and increased arterial stiffness in hypertensive patients, independently of age, thus suggesting that it may have a prognostic relevance [28].
Among older subjects, BP should be measured in the sitting position, immediately after reaching the standing position, and again twice, when this position has been maintained for 1 and 3 min. Thus it is possible to detect orthostatic hypotension, defined as a decline of at least 20 mmHg of SBP and/or 10 mmHg of DBP in standing vs. the sitting position [13]. The detection of this condition is particularly important in older subjects, as it is particularly frequent and has been associated with falls, cardiovascular events, and total mortality [5, 6]. Therefore the choice of antihypertensive treatment should be based on orthostatic together with sitting BP values.
A critical point regarding BP measure in old age is represented by the discrepancy between office and out-of-office BP measures, including both home BP monitoring and 24-h ambulatory blood pressure monitoring (ABPM). In fact a meta-analysis of available studies shows that this discrepancy is age dependent, with office BP values increasing more steeply with age in comparison with daytime ABPM measures. In particular, office BP values tend to be higher than daytime ABPM ones after the age of 50 years for SBP and after the age of 45 years for DBP, while the reverse is true at younger ages [29]. This results in age-associated increases of “white coat hypertension” risk. This condition is defined as having elevated office BP without elevated daytime BP (or alternatively non-elevated 24-h BP) on ABPM in individuals not taking antihypertensive medication. White coat hypertension may also refer to individuals taking antihypertensive medication. However, the preferred terms for this subset of patients is “treated white coat hypertension” or “white coat uncontrolled hypertension” [30].
The majority of studies regarding white coat hypertension have observed no increased cardiovascular risk for this condition in comparison with normotension. This has been confirmed in particular among older subjects with a clinical diagnosis of isolated systolic hypertension at clinical measurement and normal BP values at ABPM, whose 10-year risk of cardiovascular morbidity and mortality was similar to subjects with persistently normal BP values, both among treated and non-treated subjects [31]. Moreover, the phenomenon is highly prevalent among older disabled subjects: in a sample of older nursing home patients undergoing ABPM, it was detected in 33 % of the whole sample and in 70 % of those with high BP at office assessment [32].
The suspect of white coat hypertension is the first indication for ABPM cited in European guidelines [33]. Other indications include the suspect of masked hypertension, the detection of abnormal BP circadian rhythm (including “non-dipping” status, postprandial hypotension, and “morning surge”), and the assessment of response to treatment in complex cases (e.g., high BP variability and resistant hypertension). For all these reasons, ABPM is frequently useful among very old subjects. The superior prognostic ability of ABPM values compared with clinical ones in predicting the risk of mortality and cardiovascular events [34] represents a further reason to perform the assessment in conditions where prognostication is particularly challenging, such as complex geriatric patients. Although ABPM assessment is sometimes considered difficult to perform and poorly tolerated in older patients with cognitive impairment, this was found not to be the case for the vast majority of dementia patients in a memory clinic, with the only exception of those with severe behavioral disorders [35]. However, when ABPM is deemed as non-feasible, home BP measurements seem to be a reliable alternative [34].
8.3.2 The Role of Cognitive and Functional Status
Limitations in activities of daily living and cognitive impairment frequently occur during old age. Several longitudinal data have associated high BP with risk of disability onset [36]. This effect appears at least partly mediated by increased stroke risk [37], although higher BP has been associated with increased risk of motor impairment also in a cohort of older stroke-free subjects [38]. This association appears to be mediated by cognitive impairment onset and might be at least partly explained by the onset of microvascular cerebral lesions, such as white matter lesions, without acute cerebrovascular events [39]. Of notice, the extent of brain microvascular changes has been associated with extra-cerebral end-organ damages in AH, including chronic kidney damage [40], increased left ventricular mass [41], and retinal microvascular changes [42].
Moreover high BP at midlife has been associated with cognitive impairment and dementia in old age in several cohort studies [43]. Data are less consistent regarding the effect of BP on risk of cognitive impairment among older subjects. In fact, while some studies have confirmed this association among older subjects [44], other studies could not confirm it and have observed just the opposite [45]. On the whole it seems that, while high BP is still associate d with increased risk of cognitive decline 10 years later among “young old” (age range 65–74), it might have a neutral effect between 75 and 84 and even act as a preventive factor among subjects aged 85+ [46]. On the other hand, it has repeatedly been shown that, while long-lasting high BP values are associated with increased dementia risk, dementia onset is associated with subsequent decline of BP values, possibly caused by an altered vascular control due to brain damage [47].
Finally, a poorer self-reported physical and mental health has been associated with lower BP values, not only among older subjects but also among younger adults with history of vascular disorders [48]. Therefore it is not surprising that lower BP is associated with lower grip strength, an objective measure of physical performance, among subjects aged 85 [49] and, similarly, with a worse cognitive and physical performance in centenarians [50].
Therefore, the assessment of cognitive and functional status in older hypertensives subjects has two different aims:
-
1.
To have an indirect, easy obtainable estimate of brain end-organ damage associated with high BP.
-
2.
To assess the prognostic role of BP values in the context of the biological age of the single subject. As it will be discussed below, target BP values might differ in old age according to “frailty status,” which in turn can be estimated by validated and reproducible measures of cognitive and functional status.
Several short measures of cognitive status among older subjects exist and can be used in clinical practice. Among such measures, Mini Mental State Examination (MMSE) [51] is one of the best known and probably represents a “gold standard” for brief cognitive assessment, due to its widespread use both in clinical and in research setting all over the world, the ability to reliably identify dementia and stage its severity, and the possibility to follow up patients over time [52]. The administration of the test is 5–10 min long, depending on patient’s cognitive status, and includes items testing orientation to space and time, memory, attention and calculation, word finding, phrase repetition, comprehension of spoken and written language, and constructional praxis. The total score is included between 0 and 30, with 24 being the most widely adopted cutoff for dementia. Locally validated rules exist to adjust the score for age and education. While this instrument is widely adopted in geriatric facilities, it will be probably felt as too time-consuming in a typical hypertension clinic. A suitable, less time-consuming alternative for cognitive screening is the Mini-Cog [53], which requests only a 2-min assessment, including the recall of the three words, similar to the MMSE, and the drawing of a clock. The scoring of the test is straightforward, as shown in Fig. 8.1.
Mini-Cog test (Borson et al. [53]): administration and scoring
Ask the patient to repeat three semantically unrelated words.
Ask the patient to draw a clock.
Draw a circle.
Add the numbers.
Set the time on 11:10.
Ask the patient to recall the previously repeated words.
Clock Drawing Test (CDT) is normal if all numbers are present in the right sequence and position and clock’s hands are in the right position.
Test is scored according to the following algorithm
To reduce the risk of false positives, it is recommended to corroborate the suspect of dementia, as resulting from Mini-Cog, with:
-
1.
Report of cognitive impairment by the patient himself and/or relatives, according to accepted criteria for dementia and mild cognitive impairment [54]
-
2.
Impairment in instrumental activities of daily living, especially use of telephone, handling medications, and finances, which appears to be fairly specific for dementia [55]
Lower extremity function measures are widely used in geriatric medicine as a measure of physical frailty, and several of them are usable as brief screener. The most validated single measure is represented by gait speed on a 4-m corridor, with speed <0.8 m/s (i.e., time to walk through 4 m >5 s) being a sensitive measure of physical frailty [56]. Gait speed is also included in more comprehensive physical performance tests, such as the short physical performance battery [57], which includes a balance test (measuring the ability to stand side by side, in semi-tandem, and in tandem), the abovementioned gait speed test, and the chair stand test, measuring the time needed to stand up for five times from a chair without using arms. Each subtest is scored from 0 to 4, with a total score ranging from 0 to 12 and values <10 indicating reduced physical performance and being associated with worse outcome, including higher risk of mortality, disability onset and progression, hospitalization, and institutionalization [58, 59]. While this assessment is more comprehensive in comparison with gait speed only, as it includes measures of balance and lower extremity muscle strength, the predictive values of gait speed alone seem to be similar to the complete performance test [60] (Fig. 8.2).
Finally, the presence of overt disability in basic activities of daily living (ADL: washing, dressing, going to the toilet, transferring, eating) has to be identified in older subjects with AH, as it appears to have a strong prognostic role beyond the presence of associated comorbid conditions, including high BP [61]. This is evident for nursing homes patients, in whom the prognostic role of BP has been found almost irrelevant in comparison with the presence of ADL disability and behavioral disorders [32], and possible beneficial effects of antihypertensive drugs have to be weighted carefully against the risk of brain hypoperfusion, falls, and fractures [7]. To screen for the presence of ADL disability, the single question regarding the ability to dress and undress oneself has been found to possess satisfactory accuracy to detect a significant impairment [62].
8.4 Treatment
8.4.1 Guidelines and Clinical Trials in the Oldest Old
Randomized clinical trials performed during last 20 years have clearly shown that the benefit of antihypertensive treatments on cardiovascular events is not significantly different at ages above rather than below 65 years, with a greater absolute benefit in the elderly because of the higher cardiovascular risk characterizing old age [63]. These results have been extended to very old age with Hypertension in the Very Elderly Trial (HYVET), which was prematurely terminated after the demonstration of a clear benefit of antihypertensive treatment in reducing total mortality, heart failure, and stroke in subjects aged 80+ [64].
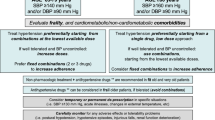
Yet some points have not been clarified yet, one of the first being the effect of age on the cutoff and the target for antihypertensive treatment. Since 2013, European [13] and US [65] guidelines have acknowledged different cutoffs and target values for antihypertensive drugs treatment in old age (Table 8.1). This was mainly based on the critical reappraisal of previous guidelines, which clearly indicated that the treatment of grade I AH and the previously indicated cutoff of 140/90 mmHg were not evidence-based in the elderly [66]. In fact all randomized clinical trials including only subjects 65+ had SBP ≥160 mmHg as inclusion criterion, enrolled subjects showed a mean baseline SBP included between 166 and 196 mmHg, and generally did not attained a mean SBP <140 mmHg in the actively treated group. This is particularly true for subjects enrolled in HYVET, who were over 80, with no severe comorbidity, had mean BP values 173/91 mmHg at baseline and attained BP values of 144 and 159 mmHg at follow-up in active treatment and placebo group, respectively [64].
Only few intervention studies have addressed the issue of different BP targets among older subjects, with somehow conflicting results. In a subgroup analysis of the FEVER study, 3179 older Chinese patients randomized to more intense treatment (low-dose hydrochlorothiazide plus felodipine, achieved SBP 138 mmHg) had a lower risk of stroke, cardiovascular events, and total mortality compared to the ones randomized to less intense treatment (low-dose hydrochlorothiazide plus placebo, achieved SBP 142 mmHg) [67]. Yet it has to be acknowledged that this was a subgroup analysis and that “older subjects” group was 65+, with a mean age 69.5. Two other Japanese studies have specifically focused on different treatment targets for older subjects [68, 69]. In the VALISH study, 3260 patients aged 70–84 (mean age 76) were randomized to strict BP control (target SBP < 140 mmHg, achieved SBP 137 mmHg) vs. moderate control (target SBP 140–150 mmHg, achieved SBP 142 mmHg). After 3 years the two groups did not differ for the primary composite end point neither for any of the secondary end points, including stroke, cardiac events, cardiovascular mortality, total mortality, and for incidence of adverse events [69]. Moreover, in the JATOS study, 4418 patients aged 65–85 (42 % over 75) were randomized to strict BP control (target SBP < 140 mmHg, achieved SBP 136 mmHg) vs. moderate control (target SBP 140–160 mmHg, achieved SBP 146 mmHg). After 2 years the two groups did not differ for the combined primary end point (stroke, cardiac events, renal failure) neither for total mortality nor for incidence of adverse events. Yet an interaction between age and treatment group was associated with primary end point, with the highest risk in the subgroup aged 75+ undergoing more strict control [68].
The abovementioned data are consistent with the results of a meta-analysis of data pertaining to subjects aged 80+ enrolled in different RCTs. In those subjects a significant effect of active treatment was confirmed for stroke, cardiovascular events, and heart failure, while no effect was observed for cardiovascular death and total mortality. In a meta-regression analysis, mortality risk was reduced in the treatment arm of trials that adopted a lower-intensity treatment and achieved the least BP reduction [70].
Moreover in observational studies of subjects aged 85+, SBP <140 mmHg has repeatedly been associated with higher mortality risk [8–10]. Yet this association might differ according to antihypertensive treatment status, as shown in an international study of home BP monitoring in older subjects aged 80+, aimed at identifying optimal BP targets in regard to mortality risk over a 5.5-year follow-up. In fact, cardiovascular mortality and morbidity showed a direct association with SBP among subjects non-treated with antihypertensives, with highest risk at values >152 mmHg, while it showed a curvilinear association with SBP in the subgroup receiving antihypertensive drugs, with an increased cardiovascular risk for SBP <127 mmHg [71]. Moreover the risk associated with low BP in old age appears to be greater among subjects with a history of AH at midlife, in regard both to survival [8] and to brain atrophy and cognitive decline [72].
On the whole the cited data raise a caveat for excessive SBP lowering among actively treated subjects in very old age, with a cutoff for increased risk around the age of 80, especially for those with a long-standing history of AH. On a pathophysiological ground, the observed epidemiological and clinical data might be explained by a small reduction of perfusion of vital organs coupled with an altered vascular autoregulation associated with chronic AH, possibly leading to critical hypoperfusion if associated with decreased BP [72]. This hypothesis has not been proven yet, as a recent study of the association between BP and cerebral blood flow of very old subjects with mild cognitive impairment was not able to show any correlation between lower BP values and cerebral hypoperfusion [73]. Moreover it should be remembered that low BP is often associated with more severe clinical, and especially cardiovascular, conditions and that at least part of the observed association might be confounded by comorbidities. For these and other reasons, the so-called J-curve phenomenon regarding the prognostic role of BP has been widely debated [74].
The Systolic Blood Pressure Intervention Trial (SPRINT) [75] has strengthened the position of those supporting the preventive efficacy of aggressive BP treatment also among older subjects. In patients at high cardiovascular risk and already using antihypertensive drugs, a treatment strategy targeting a systolic BP of 120 mmHg resulted in lower incidence of major cardiovascular events and death from any cause compared to a less strict approach targeting a systolic BP of 140 mmHg; this result was also statistically significant in the subgroup (28 % of the entire sample, n=2636) of patients more than 75 years old. Yet, it has to be pointed out that patients with severe disability, living in nursing, affected by dementia, decompensated heart failure, previous stroke, or diabetes were excluded from the study. Conversely included subjects had a mean 20 % 10-year Framingham cardiovascular risk score and a mean BMI of 30. On the whole SPRINT results add relevant information regarding antihypertensive treatment of a significant part of the older population but seem to apply to high vascular risk patients without disability and abovementioned diseases, and therefore may not be unconditionally applied to the oldest old.
8.4.2 Frailty Detection and Antihypertensive Treatment Choices
Apart from chronological age, several studies in most recent years have pointed out at a role for “frailty” in increasing the risk associated with antihypertensive treatment among elderly subjects [11].
In geriatric research frailty is conceptualized as a physiological syndrome characterized by decreased functional reserve and diminished resistance to stressors, causing vulnerability to adverse health outcomes, including disability and death [76]. While frailty should be reliably identified with a comprehensive geriatric assessment, identifying multiple physical, mental, and social impairments whose accumulation may ultimately lead to the increased vulnerability status [77], rapid screener for this condition is often needed in clinical practice due to time and resource constraints. Therefore simple clinical tools have been operationalized to detect frailty with sufficient sensitivity and specificity [56], instruments based on lower extremity performance being among the most useful for this purpose [59].
An analysis from the National Health and Nutrition Examination Survey (NHANES) supports a role for motor performance as a powerful modulator of BP-associated risk. In fact, in a cohort of 2340 older subjects (mean age 74), the association between BP and a 7-year mortality varied markedly among subjects, according to their ability to walk 6 m as fast walkers (≥0.8 m/s), slow walkers (<0.8 m/s), or unable to complete the task. In fact, while high SBP was associated with increased mortality among fast walkers, the association disappeared among slow walkers and was reverted among subjects unable to walk, who had a greater risk associated with low values of SBP and DBP [78].
In keeping with these data, a condition of overt disability in activities of daily living associated with low BP has been identified as a condition with a negative prognostic outcome among oldest old (age 85+), in terms of both increased risk of cognitive decline [45] and increased risk for stroke [79]. Moreover, in the vast group of disabled nursing home subjects, BP was found as unrelated to a 1-year mortality risk in one study [32] and inversely associated with increased 2-year mortality risk in another one [80]. Of notice, in the latter study the increased risk for mortality was restricted to subjects with SBP < 130 mmHg in combination with 2+ antihypertensive drugs, thus supporting the need of less intensive treatment in this highly impaired population.
Finally, subjects with cognitive impairment might represent a subpopulation at high risk for brain hypoperfusion. Yet in this condition the data are not clear-cut. In fact, one study of 1385 subjects with mild cognitive impairment (mean age 73.6, baseline MMSE 28/30) has found a faster progression of cognitive decline over 2 years among subjects with repeated detection of high BP (≥140/90 mmHg) [81]. In keeping with these data, subjects with mild cognitive impairment (mean age 67.8, baseline MMSE 26/30) have been found to have an increased risk of conversion to Alzheimer’s disease after 5 years, while antihypertensive treatment reduced the risk [82]. Conversely a subsequent study conducted with ambulatory BP monitoring in a sample of 172 older subjects with dementia or mild cognitive impairment (mean age 79, MMSE 22/30) has observed an increased risk of cognitive decline after 9 months among subjects with lower mean daytime SBP (<129 mmHg) actively treated with antihypertensive drugs [83]. Another study of 141 subjects with mild cognitive impairment (mean age 74) has observed an independent association between orthostatic hypotension and increased risk for conversion to dementia after 2 years [84]. Therefore, the presence of mild cognitive impairment might be a caveat for possible detrimental effects of excessive BP lowering, at least among oldest old and for subjects with orthostatic hypotension and overt dementia. ABPM seems to be more useful than clinical measure in predicting the cognitive detrimental effects of low BP.
On the whole, the presence of functional disability, motor impairment, and cognitive impairment might be useful markers of increased vulnerability to antihypertensive treatment. These factors together with old age can suggest a more prudent approach to vascular risk factor prevention, including antihypertensive treatment [85]. A treatment discontinuation randomized trial of 385 older subjects 75+ with mild cognitive decline (mean age 81, MMSE 26/30) was recently published. Subjects were included if they took at least one antihypertensive drug, and SBP was ≤160 mmHg. After 16 weeks SBP went from 148.8 mmHg to 154.2 mmHg, but no positive effect was evident on cognitive function, psychological status, or daily functioning [86]. Further studies of treatment de-intensification are warranted, with the aim of identifying the role of different BP measures (clinical vs. ambulatory) and different BP targets for specific subgroups of frail older subjects.
Conclusion
Oldest old subjects represent a fast-rising share of world population who lacks firm indications regarding prognostic meaning of BP values and preventive or harmful effects of antihypertensive treatment. The need to differentiate antihypertensive treatment targets according to age and health status introduced by European guidelines represents an opportunity to personalize medical approach to this diverse population group. Observational and intervention studies published during the last years suggest that a strict BP control might be beneficial in some older subjects (as shown by SPRINT trial) but might harm other ones, probably the frailest. Comprehensive geriatric assessment is useful in detecting vulnerability indicators, and simple cognitive and functional measures should be used to screen for older subjects who need a more cautious approach. Future epidemiological and intervention studies targeting specific profiles of frailty are warranted, to support personalized antihypertensive treatment strategies for oldest old subjects.
Bibliography
WHO. World report on aging and health. Luxembourg; 2015. http://apps.who.int/iris/bitstream/10665/186463/1/9789240694811_eng.pdf?ua=1
OECD. Health at a glance 2015. OECD indicators. Paris: OECD Publishing; 2015.
Berrut G, Andrieu S, Araujo de Carvalho I, et al. Promoting access to innovation for frail old persons. IAGG (International Association of Gerontology and Geriatrics), WHO (World Health Organization) and SFGG (Société Française de Gériatrie et de Gérontologie) Workshop–Athens January 20–21, 2012. J Nutr Health Aging. 2013;17:688–93.
Jansen S, Bhangu J, de Rooij S, Daams J, Kenny RA, van der Velde N. The Association of Cardiovascular Disorders and Falls: a systematic review. J Am Med Dir Assoc. 2015;17:193–9.
Pepersack T, Gilles C, Petrovic M, et al. Prevalence of orthostatic hypotension and relationship with drug use amongst older patients. Acta Clin Belg. 2013;68:107–12.
Angelousi A, Girerd N, Benetos A, et al. Association between orthostatic hypotension and cardiovascular risk, cerebrovascular risk, cognitive decline and falls as well as overall mortality: a systematic review and meta-analysis. J Hypertens. 2014;32:1562–71; discussion 71.
Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med. 2012;172:1739–44.
van Bemmel T, Gussekloo J, Westendorp RG, Blauw GJ. In a population-based prospective study, no association between high blood pressure and mortality after age 85 years. J Hypertens. 2006;24:287–92.
Rastas S, Pirttila T, Viramo P, et al. Association between blood pressure and survival over 9 years in a general population aged 85 and older. J Am Geriatr Soc. 2006;54:912–8.
Molander L, Lovheim H, Norman T, Nordstrom P, Gustafson Y. Lower systolic blood pressure is associated with greater mortality in people aged 85 and older. J Am Geriatr Soc. 2008;56:1853–9.
Muller M, Smulders YM, de Leeuw PW, Stehouwer CD. Treatment of hypertension in the oldest old: a critical role for frailty? Hypertension. 2014;63:433–41.
Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219.
Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics–2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:480–6.
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–62.
Sundquist J, Winkleby MA, Pudaric S. Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: an analysis of NHANES III, 1988–1994. Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 2001;49:109–16.
Reynolds K. Trends in health status and health care use among older women. National Center for Health Statistics. Centers for Disease Control and Prevention; 2007.
Lloyd-Jones DM, Evans JC, Levy D. Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA. 2005;294:466–72.
Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2011;123:2434–506.
Franklin SS, et al. Hemodynamic patterns of age-related changes in blood pressure The Framingham Heart Study. Circulation. 1997;96:308–15.
Wiinberg N, Høegholm A, Christensen HR, et al. 24-h ambulatory blood pressure in 352 normal Danish subjects, related to age and gender. Am J Hypertens. 1995;8:978–86.
Cacciolati C, Hanon O, Alpérovitch A, Dufouil C, Tzourio C. Masked hypertension in the elderly: cross-sectional analysis of a population-based sample. Am J Hypertens. 2011;24:674–80.
Angeli F, Reboldi G, Verdecchia P. Masked hypertension: evaluation, prognosis, and treatment. Am J Hypertens. 2010;23:941–8.
Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–19.
Franklin SS, Wilkinson IB, McEniery CM. Unusual hypertensive phenotypes: what is their significance? Hypertension. 2012;59:173–8.
Messerli FH, Ventura HO, Amodeo C. Osler’s maneuver and pseudohypertension. N Engl J Med. 1985;312:1548–51.
Belmin J, Visintin JM, Salvatore R, Sebban C, Moulias R. Osler’s maneuver: absence of usefulness for the detection of pseudohypertension in an elderly population. Am J Med. 1995;98:42–9.
Cavallini MC, Roman MJ, Blank SG, Pini R, Pickering TG, Devereux RB. Association of the auscultatory gap with vascular disease in hypertensive patients. Ann Intern Med. 1996;124:877–83.
Ishikawa J, Ishikawa Y, Edmondson D, Pickering TG, Schwartz JE. Age and the difference between awake ambulatory blood pressure and office blood pressure: a meta-analysis. Blood Press Monit. 2011;16:159–67.
Reynolds K, Bowling CB, Sim JJ, Sridharan L, Harrison TN, Shimbo D. The utility of ambulatory blood pressure monitoring for diagnosing white coat hypertension in older adults. Curr Hypertens Rep. 2015;17:86.
Franklin SS, Thijs L, Hansen TW, et al. Significance of white-coat hypertension in older persons with isolated systolic hypertension: a meta-analysis using the International Database on Ambulatory Blood Pressure Monitoring in Relation to Cardiovascular Outcomes population. Hypertension. 2012;59:564–71.
Mossello E, Pieraccioli MC, Zanieri S, et al. Ambulatory blood pressure monitoring in older nursing home residents: diagnostic and prognostic role. J Am Med Dir Assoc. 2012;13:760.e1–5.
Parati G, Stergiou G, O’Brien E, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359–66.
Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005;19:80–7.
Nesti N, Pieraccioli MC, Mossello E, et al. Tolerability of ambulatory blood pressure monitoring (ABPM) in cognitively impaired elderly. Blood Press. 2014;23:377–80.
Lawes CM, Vander Hoorn S, Rodgers A, Hypertension ISo. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–8.
Shah RC, Wilson RS, Bienias JL, Arvanitakis Z, Evans DA, Bennett DA. Blood pressure and lower limb function in older persons. J Gerontol A Biol Sci Med Sci. 2006;61:839–43.
Elias MF, Dore GA, Davey A, Robbins MA, Elias PK. From blood pressure to physical disability: the role of cognition. Hypertension. 2010;55:1360–5.
Hajjar I, Quach L, Yang F, et al. Hypertension, white matter hyperintensities, and concurrent impairments in mobility, cognition, and mood: the Cardiovascular Health Study. Circulation. 2011;123:858–65.
Makin SD, Cook FA, Dennis MS, Wardlaw JM. Cerebral small vessel disease and renal function: systematic review and meta-analysis. Cerebrovasc Dis. 2015;39:39–52.
Sierra C, de la Sierra A, Paré JC, Gómez-Angelats E, Coca A. Correlation between silent cerebral white matter lesions and left ventricular mass and geometry in essential hypertension. Am J Hypertens. 2002;15:507–12.
Yau PL, Hempel R, Tirsi A, Convit A. Cerebral white matter and retinal arterial health in hypertension and type 2 diabetes mellitus. Int J Hypertens. 2013;2013:329602.
Qiu C, Winblad B, Fratiglioni L. The age-dependent relation of blood pressure to cognitive function and dementia. Lancet Neurol. 2005;4:487–99.
Skoog I, Lernfelt B, Landahl S, et al. 15-year longitudinal study of blood pressure and dementia. Lancet. 1996;347:1141–5.
Sabayan B, Oleksik AM, Maier AB, et al. High blood pressure and resilience to physical and cognitive decline in the oldest old: the Leiden 85-plus Study. J Am Geriatr Soc. 2012;60:2014–9.
Euser SM, van Bemmel T, Schram MT, et al. The effect of age on the association between blood pressure and cognitive function later in life. J Am Geriatr Soc. 2009;57:1232–7.
Joas E, Backman K, Gustafson D, et al. Blood pressure trajectories from midlife to late life in relation to dementia in women followed for 37 years. Hypertension. 2012;59:796–801.
Muller M, Jochemsen HM, Visseren FL, et al. Low blood pressure and antihypertensive treatment are independently associated with physical and mental health status in patients with arterial disease: the SMART study. J Intern Med. 2013;274:241–51.
Taekema DG, Maier AB, Westendorp RG, de Craen AJ. Higher blood pressure is associated with higher handgrip strength in the oldest old. Am J Hypertens. 2011;24:83–9.
Szewieczek J, Dulawa J, Francuz T, et al. Mildly elevated blood pressure is a marker for better health status in Polish centenarians. Age (Dordr). 2015;37:9738.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Mossello E, Boncinelli M. Mini-mental state examination: a 30-year story. Aging Clin Exp Res. 2006;18:271–3.
Borson S, Scanlan J, Brush M, Vitaliano P, Dokmak A. The mini-cog: a cognitive ‘vital signs’ measure for dementia screening in multi-lingual elderly. Int J Geriatr Psychiatry. 2000;15:1021–7.
Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270–9.
Cromwell DA, Eagar K, Poulos RG. The performance of instrumental activities of daily living scale in screening for cognitive impairment in elderly community residents. J Clin Epidemiol. 2003;56:131–7.
Clegg A, Rogers L, Young J. Diagnostic test accuracy of simple instruments for identifying frailty in community-dwelling older people: a systematic review. Age Ageing. 2015;44:148–52.
Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–61.
Vasunilashorn S, Coppin AK, Patel KV, et al. Use of the Short Physical Performance Battery Score to predict loss of ability to walk 400 meters: analysis from the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2009;64:223–9.
Minneci C, Mello AM, Mossello E, et al. Comparative study of four physical performance measures as predictors of death, incident disability, and falls in unselected older persons: the insufficienza Cardiaca negli Anziani Residenti a Dicomano Study. J Am Geriatr Soc. 2015;63:136–41.
Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–31.
Marengoni A, von Strauss E, Rizzuto D, Winblad B, Fratiglioni L. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med. 2009;265:288–95.
Di Bari M, Profili F, Bandinelli S, et al. Screening for frailty in older adults using a postal questionnaire: rationale, methods, and instruments validation of the INTER-FRAIL study. J Am Geriatr Soc. 2014;62:1933–7.
Blood Pressure Lowering Treatment Trialists C, Turnbull F, Neal B, et al. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta-analysis of randomised trials. BMJ. 2008;336:1121–3.
Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–98.
James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National Committee (JCN 8). JAMA. 2014;311:507–20.
Zanchetti A, Grassi G, Mancia G. When should antihypertensive drug treatment be initiated and to what levels should systolic blood pressure be lowered? A critical reappraisal. J Hypertens. 2009;27:923–34.
Zhang Y, Zhang X, Liu L, Zanchetti A, Group FS. Is a systolic blood pressure target <140 mmHg indicated in all hypertensives? Subgroup analyses of findings from the randomized FEVER trial. Eur Heart J. 2011;32:1500–8.
JatosStudyGroup. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS). Hypertens Res. 2008;31:2115–27.
Ogihara T, Saruta T, Rakugi H, et al. Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension. 2010;56:196–202.
Bejan-Angoulvant T, Saadatian-Elahi M, Wright JM, et al. Treatment of hypertension in patients 80 years and older: the lower the better? A meta-analysis of randomized controlled trials. J Hypertens. 2010;28:1366–72.
Aparicio LS, Thijs L, Boggia J, et al. Defining thresholds for home blood pressure monitoring in octogenarians. Hypertension. 2015;66:865–73.
Muller M, Sigurdsson S, Kjartansson O, et al. Joint effect of mid- and late-life blood pressure on the brain: the AGES-Reykjavik study. Neurology. 2014;82:2187–95.
Foster-Dingley JC, Moonen JE, de Craen AJ, de Ruijter W, van der Mast RC, van der Grond J. Blood pressure is not associated with cerebral blood flow in older persons. Hypertension. 2015;66:954–60.
Andrikou E, Bafakis I, Grassos C, Papaspyropoulos A, Kranidis A. J-curve phenomenon: a matter of debate. Hellenic J Cardiol. 2012;53:357–66.
Wright JT, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16.
Walston J, Hadley EC, Ferrucci L, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc. 2006;54:991–1001.
Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752–62.
Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012;172:1162–8.
Sabayan B, van Vliet P, de Ruijter W, Gussekloo J, de Craen AJ, Westendorp RG. High blood pressure, physical and cognitive function, and risk of stroke in the oldest old: the Leiden 85-plus Study. Stroke. 2013;44:15–20.
Benetos A, Labat C, Rossignol P, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: The PARTAGE Study. JAMA Intern Med. 2015;175:989–95.
Goldstein FC, Levey AI, Steenland NK. High blood pressure and cognitive decline in mild cognitive impairment. J Am Geriatr Soc. 2013;61:67–73.
Li J, Wang YJ, Zhang M, et al. Vascular risk factors promote conversion from mild cognitive impairment to Alzheimer disease. Neurology. 2011;76:1485–91.
Mossello E, Pieraccioli M, Nesti N, et al. Effects of low blood pressure in cognitively impaired elderly patients treated with antihypertensive drugs. JAMA Intern Med. 2015;175:578–85.
Hayakawa T, McGarrigle CA, Coen RF, et al. Orthostatic blood pressure behavior in people with mild cognitive impairment predicts conversion to dementia. J Am Geriatr Soc. 2015;63:1868–73.
Mossello E. Targeting vascular risk factors in older adults: from polypill to personalized prevention. JAMA Intern Med. 2015;175:1949–50.
Moonen JE, Foster-Dingley JC, de Ruijter W, et al. Effect of discontinuation of antihypertensive treatment in elderly people on cognitive functioning-the DANTE Study Leiden: a randomized clinical trial. JAMA Intern Med. 2015;175:1622–30.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Mossello, E., Desideri, G., Ungar, A. (2017). Hypertension in the Oldest Old, Beyond Guidelines. In: Ungar, A., Marchionni, N. (eds) Cardiac Management in the Frail Elderly Patient and the Oldest Old. Springer, Cham. https://doi.org/10.1007/978-3-319-43468-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-43468-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-43466-7
Online ISBN: 978-3-319-43468-1
eBook Packages: MedicineMedicine (R0)