Abstract
Systolic hypertension is a common condition in the elderly and is considered a major determinant not only of cardiovascular morbidity and mortality, but also cognitive decline, frailty and loss of autonomy. We have now evidence that in community living hypertensive subjects over 80 years old, decreasing blood pressure with pharmacological treatment is able to reduce the rate of cardiovascular events and total mortality. By contrast the efficacy of this treatment in preventing dementia is more controversial. A systolic BP of 150 mmHg is an acceptable cut-off value both for the diagnosis of hypertension and as a target for treatment in most patients >80 years old. To avoid over-treating, it is important to confirm the diagnosis with blood pressure monitoring at home. Treatment should be initiated and followed up in a shared decision making process, taking the patients’ preferences into account. The risk of drug-induced orthostatic hypotension should always be taken into account but should rarely be a reason not to treat. Avoiding “going too low” is important not only at the initiation of therapy, but also during follow-up. Prospectively, other than blood pressure values could better evaluate the age-related arterial alterations especially in the very elderly frail subjects. In this respect, assessment of arterial stiffness could provide significant new information in order to estimate the risk and evaluate the potential benefits of treatment in the very elderly.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The prevalence of hypertension markedly increases with age, reaching >60 % after the age of 70 [1]. However, its biological and prognostic significance, as well as the clinical benefits of its treatment, remain complex issues. The most typical form of hypertension in older persons is isolated systolic hypertension (ISH). With aging, there is a continuous increase in systolic blood pressure (SBP), but after the age of approximately 60 there is a progressive decline in diastolic BP (DBP). Pulse pressure, defined as the difference between SBP and DBP, increases in consequence . These changes can be attributed to a progressive increase in the stiffness of large arteries [2, 3]. Pulse pressure in itself becomes a strong cardiovascular (CV) risk factor, whereas the association between mean BP and CV risk diminishes or disappears. Thus, the pathophysiology of ISH differs from that of essential hypertension in younger adults. It follows that the associated CV risks and the benefits of treatment must be verified in older hypertensive persons, and cannot be extrapolated from studies carried out in younger persons.
Several large population studies have indicated that hypertension remains associated with an increased risk of stroke and coronary heart disease (CHD) even in old age. Key studies carried out in patients with ISH, in particular the Systolic Hypertension in the Elderly Program (SHEP) and Systolic Hypertension in Europe (Syst-Eur) trials, have convincingly shown that antihypertensive treatment decreases the risk of stroke and heart failure, although the reductions in the risk of CHD were disappointing [4, 5]. However, these studies were not performed in very old patients (mean age: approximately 70).
More recently, the Hypertension in the Very Elderly (HYVET) study, performed in patients >80 years old, has confirmed that antihypertensive treatment decreases the risk of stroke and heart failure. The study also demonstrated a reduction in all-cause mortality. This was particularly important, as previous non-controlled trials or subgroup analysis of controlled trials had suggested that antihypertensive treatment increases mortality in patients >80 years old. The results of the HYVET study were impressive enough to lead to the premature interruption of the trial on ethical grounds [6]. Taken together, these results suggest that essentially all patients with hypertension should receive treatment, which represents a formidable challenge in terms of both resource allocation and safety. The aim of this chapter is to discuss some of the issues related to patient selection, safety, and clinical relevance of antihypertensive treatment.
2 The Diagnosis of Hypertension
ISH is usually defined by a SBP >140 and a DBP <90 mmHg. However, the measurement of blood pressure is hampered by considerable between-measure variability and by the artifactual increase in BP when measured in a medical office, the so-called white-coat effect. It follows that many patients with an office SBP >160 mmHg in fact do not present with true hypertension. The problem of white-coat hypertension and therefore possible patient misclassification worsens with age. In a hypertension clinic, we found that the difference in SBP between office measures and ambulatory blood pressure monitoring (ABPM) is considerable at all ages and reaches approximately 40 mmHg in patients >80 years old [7]. A substudy of the Syst-Eur trial investigated clinical outcomes according to BP measured by ABPM. Less than 25 % of patients had sustained hypertension, defined as a mean SBP >160 mmHg by ABPM. Importantly, the benefits of treatment could be demonstrated only in this subgroup [8]. This study suggested that even in large intervention trials many patients included actually present with white-coat hypertension rather than true ISH. These considerations suggest that the diagnosis of ISH should be confirmed either by ABPM or BP monitoring at home, before engaging in a possibly lifelong treatment.
3 Blood Pressure Targets in Antihypertensive Therapy
The selection of optimal blood pressure targets in antihypertensive therapy still remains an area of uncertainty. The evidence from randomized controlled trials remains sketchy and different targets may apply in different age groups. A recent US consensus statement proposes a SBP <140 and a DBP <90 mmHg as general targets, while recognizing the arbitrary character of this recommendation [9]. However, as mentioned, the main inclusion criterion in the most relevant clinical trials was a SBP >160 mmHg [4–6]. The SBP achieved with therapy after 1 year was approximately 145–150 mmHg in both the Syst-Eur and the HYVET studies [4, 6]. Thus, the clinical benefits of treatment in these studies were obtained with higher SBP pressure values than recommended in the US consensus statement. It is quite possible that achieving lower SBP values may lead to even better clinical outcomes, but there is little evidence in support of this hypothesis so far. Conversely, intensive treatment targeting lower SBP values is likely to be associated with a higher incidence of side effects. There are few studies on the incidence of antihypertensive drug side effects in geriatric populations. The Action to Control Cardiovascular Risk in Diabetes (ACCORD) study in diabetic patients (mean age: 62.2 years) compared standard and intensive BP treatment strategies [10]. The intensive strategy did result in lower SBP values (119 compared to 133 mmHg) and in a somewhat lower incidence of stroke. However, it was burdened by a higher incidence of severe side effects (3.3 vs. 1.3 %), stage 3 chronic renal failure (4.2 vs. 2.2 %), and hypokalemia (2.1 vs. 1.1 %). It is likely that the incidence and severity of complications of intensive therapy would be much higher in frail, geriatric patients. Indeed, patients >80 years of age account for more than half of adverse drug events requiring hospital admission [11]. For instance, the risk of severe hyponatremia due to diuretic therapy is not well known, but may be substantial in patients with multiple comorbidities. While awaiting further evidence, it seems reasonable to propose a SBP value of 150 mmHg both for the diagnosis of ISH, and as a target for therapy in patients >80 years of age. We have insisted on the importance of confirming the diagnosis by ABPM or by BP monitoring at home. Somewhat lower SBP cut-off values for the diagnosis of ISH, 135–140 mmHg, must be applied using these methods.
4 The Role of Associated Risk Factors
In young adults, hypertension is often evaluated in the context of metabolic syndrome. Metabolic syndrome represents a cluster of risk factors including diabetes and/or glucose intolerance, dyslipidemia, obesity and/or insulin resistance, and hypertension [12]. The metabolic syndrome concept recognizes that these risk factors are clustered, with obesity as a common denominator. It also emphasizes that weight loss should have favorable effects on associated risk factors, including hypertension [13]. However, several studies have shown that the prognostic significance of metabolic syndrome markedly decreases with age [14–16]. The prognostic significance of obesity itself actually declines with age [17], and there may even be an inverse association between obesity and mortality in very old populations [18, 19]. It is not surprising that metabolic syndrome is no longer a risk factor in older persons when obesity, its key component, ceases to be one. The interdependence of risk factors composing metabolic syndrome also declines with increasing age [7]. These considerations indicate that metabolic syndrome or its components should not be used to stratify CV risk in older patients, and to modulate the indication for antihypertensive therapy. Further, there is neither theoretical support nor clinical evidence for the notion that weight reduction may improve blood pressure in older hypertensive patients.
The interaction between diabetes and hypertension is an important issue. Both the SHEP and the Syst-Eur trials have shown that antihypertensive treatment leads to spectacular reductions in the risk of CV events, in particular stroke, in diabetic patients [20, 21]. Such a subgroup analysis has not been reported for the HYVET study, possibly because of the low number of diabetic patients in this study. Antihypertensive treatment is clearly a priority in the management of older persons with diabetes [22]. However, in view of the data from the ACCORD study discussed previously, we do not believe that the presence of diabetes justifies lower SBP targets than in older nondiabetic patients.
5 The Risk of Orthostatic Hypotension
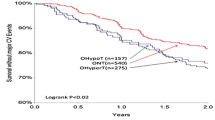
The prevalence of orthostatic hypertension (OH) (−20 in SBP or −10 mmHg in DBP in the upright position) in unselected subjects, aged 65 years or older, has been reported to vary widely between 5 and 30 % [23–25]. In a recent study in a population of 1,100 subjects over 80 years old living in nursing homes, the prevalence of OH was 18 % [26]. This value is similar to those reported for community-living older populations [27], but it is lower than that obtained for older people living in nursing homes , in which a prevalence higher than 30 % was reported [23]. A number of factors account for these discrepancies in prevalence values, including the definition of OH, the characteristics of the population studied (age range, institutionalized, or home-living), the composition of the population, and the influence of medication. Arterial stiffness, which underlies ISH, may also determine poor baroreceptor function and therefore contribute to the pathogenesis of OH [28]. Thus, arterial stiffness may determine both ISH and OH, and OH may be related to ISH rather than to its treatment. Drug-induced OH and a possible increase in the risk of falls is a common concern when treating hypertension in older persons. However, this concern is hard to substantiate.
In a large population study conducted in older British women, the prevalence of OH was elevated in subjects taking three or more antihypertensive drugs compared to those taking none. The association between antihypertensive drug prescriptions and OH was quite weak (hazard ratio = 1.26), and became nonsignificant after adjustment for other drug prescriptions or comorbidities, the latter being by themselves associated with OH [29]. Recent studies on older patients in the hospital or nursing home setting have shown that antihypertensive treatment is not associated with a higher prevalence of OH [26]. We have recently shown that in older subjects over 80 years old, those who had well-controlled hypertension with antihypertensive medication had lower prevalence of OH when compared to the other groups of subjects [26]. According to a recent meta-analysis, the association between antihypertensive drugs and the risk of falls is weak or even questionable, and certainly much weaker than the risk associated with most psychoactive drugs [30]. Thus, antihypertensive treatment should be closely monitored for OH, especially when multiple or combined drugs are prescribed. However, the risk of OH in itself should only rarely deter from treating hypertension. Parkinson’s disease is a special situation (not discussed in this chapter) where frequent, and often severe, preexisting OH is a serious limitation to the treatment of hypertension.
6 Hypertension and Cognitive Function
Aging is accompanied by an increasing prevalence of hypertension and cognitive decline and many cohort studies have in effect shown hypertension as a major risk factor for the occurrence of cognitive impairment in the old. The prevention of cognitive decline and dementia has become a major public health challenge in view of the increased longevity of the population. In this context, the discussion about a role of arterial hypertension that is potentially modifiable in the development of cognitive decline is a major issue in both research and clinical practice and a promising target for dementia prevention.
It was shown that hypertension can contribute to several cardiovascular alterations which are associated with impaired cognitive function and dementia. Although hypertension is one of the main risk factors for cerebrovascular disease, the relationship between BP levels and cognitive impairment is controversial. In the Framingham Heart Study, a high BP detected 20 years previously was inversely related with cognitive performance among untreated hypertensive subjects [31]. Since this initial observation, most epidemiological studies have confirmed the relationship between hypertension and cognitive decline. Hence, the Honolulu-Asia Aging Study (HAAS), which followed 3,735 subjects for over 30 years showed that the risk of cognitive decline at age 78 increased with the level of systolic BP measured 25 years earlier [32]. Longitudinal follow-up of patients with hypertension showed that hypertension was associated with a greater number of dementia cases observed 10–15 years later [33]. Even on a shorter follow-up period of 4 years, the Epidemiology of Vascular Aging (EVA) study found the risk of cognitive decline greater among patients with untreated chronic hypertension (odds ratio = 6) compared to a normotensive group [34]. However, this relationship between BP levels and cognitive decline in older populations was not found in many cross-sectional studies [35–37]. Moreover, hypertension duration, antihypertensive treatment, BP levels, cognitive profile and tests, and differences in the tested population, may contribute to explain the discrepancy about the relationship between hypertension and cognitive decline.
The question whether the treatment of hypertension prevents cognitive impairment and dementia is even more controversial. Some clinical trials demonstrated the beneficial effect of the use of antihypertensive therapy on the incidence of dementia. In the Syst-Eur trial, older people with ISH receiving a calcium channel blocker (nitrendipine) had a lower incidence of dementia [38]. In the 6,105 randomized participants in the Perindopril Protection Against Recurrent Stroke Study (PROGRESS), active treatment (perindopril for all and indapamide, a diuretic drug for those with neither an indication for, nor a contraindication to diuretics) was associated with reduced risks of stroke-related dementia and cognitive decline only in those with recurrent stroke [39].
However, the preventive effectiveness of antihypertensive therapy in the development of cognitive impairment remains controversial, since such effectiveness was not found by other studies. No protective effect of a thiazide diuretic on cognitive decline was found in the SHEP study, despite a reduction in blood pressure and a lower risk of stroke [5]. The Study on Cognition and Prognosis in the Elderly (SCOPE) [40] did not find any convincing evidence, in older hypertensive patients, that antihypertensive treatment confers a reduction in cognitive decline during angiotensin receptor blocker therapy, compared with control therapy. Cognitive function was well maintained in both treatment groups in the presence of substantial blood pressure reductions. A meta-analysis including the SCOPE, SHEP, and Syst-Eur studies suggested no convincing evidence that BP lowering in late life prevents the development of dementia or cognitive impairment in hypertensive patients with no apparent prior cerebrovascular disease [41]. In the first published results from the HYVET study , a double-blind, placebo-controlled trial of indapamide, with or without perindopril, in people aged 80 years and over at enrolment, antihypertensive treatment in older patients did not significantly reduce the incidence of dementia. Nevertheless, a meta-analysis (including the HYVET findings) supported the conclusion that antihypertensive treatment may potentially reduce the incidence of dementia [42]. In the secondary analysis of HYVET , a dynamic model of cognition that allows all outcomes (cognitive worsening, stability improvement, or death) to be categorized simultaneously detected small but significant benefits of the treatment [43].
The relationship between hypertension and cognitive function is probably more complex than a simple linear relationship, leading us to suggest that a midlife BP level is more important as a risk factor for late-life cognitive impairment and dementia than the BP levels evaluated in late life. Moreover, the hypothesis of a vascular involvement independent of BP level has been raised. Although BP levels can be decreased by antihypertensive therapy, vascular alterations (caused in part by hypertension) in a protracted, decade-long process are less sensitive to antihypertensive therapy in late life because they are already too far advanced before such intervention. Some studies show that markers of arterial aging may identify subjects at higher risk for cognitive decline, while BP alone does not appear to have a significant predictive value [37, 44, 45].
7 The Decision-Making Process in the Initiation and Follow-Up of Antihypertensive Therapy
Many patients may be reluctant to accept treatment, even when its benefits are clearly supported by clinical trials. There are few studies on patient drug observance in old age, but it seems obvious that patients’ initial acceptance and long-term observance are management issues that do not get simpler with increasing age. Beyond initial acceptance and implementation, antihypertensive treatment implies follow-up appointments, adjustments in drug schedules, and the burden of possible side effects. It seems logical to assume that patients’ observance and even safety are better when they are involved in the treatment and convinced of its benefits. Even when statistically significant, the benefits of a given treatment, in the patient’s view, may be insufficient to warrant the effort. Physicians themselves may not always be convinced that the benefits of treatment are clinically relevant.
Evidence from randomized clinical trials (RCTs) is typically based on observations lasting <5 years, whereas treatment is theoretically lifelong. In younger adults, we make the assumption that the benefits of treatment observed in RCTs persist in a linear manner over time. However, although life expectancy in older persons is easily underestimated, it is an inescapable reality that the older the patient, the shorter the available time for treatment. Let us illustrate the issue (see Fig. 5.1) with a hypothetical population aged 50–60 years, with a CV risk of 20 % over 10 years; this risk is reduced by 50 % by treatment. In this case, the number needed to treat is 20 over 5 years. If the treatment is pursued over 20 years (and assuming linear benefits), the number needed to treat decreases to 5 over 20 years, undisputedly a very significant benefit . Such a benefit is not a realistic expectation in older subjects. Thus, even if the risk reduction afforded by treatment per time unit is larger in older subjects, a shortened life expectancy may limit the true benefit of treatment. It follows that the decision to treat hypertension must reach a balance between the evidence from RCTs, the physician’s clinical judgment (including priority and safety issues), and the patient’s willingness to initiate and continue such a treatment.
We undertook a study to determine patients’ willingness to accept antihypertensive treatment and their desire to participate in the decision-making process [46]. Patients received standardized explanations about the outcomes, benefits, and risks of treatment; they were then asked whether they were willing to accept treatment in different scenarios, with varying risks, risk reductions, and incidence of side effects. Only a small minority of patients (4–7 %) clearly refused treatment. The majority of patients seemingly accepted antihypertensive therapy, but in fact appeared uneasy with the complex reasoning about hypertension. Most patients wanted extensive medical information, but only limited, variable participation in decision-making. They appeared to prefer delegating final medical decisions; nonetheless, they wanted to be informed and wanted their general attitudes to be taken into account.
The patients’ preferences—and reluctance—must be understood and dealt with before taking the decision to treat—or not to treat. Initial acceptance does not mean that patients understand and accept long-term therapy. A shared treatment plan, which favors safety and compliance, requires detailed explanations not only at initiation but also repeatedly during follow-up.
8 Blood Pressure and Reverse Causality
Several studies have challenged the classical association between hypertension and CV or all-cause mortality in the very old, and even observed inverse associations between both SBP and DBP and mortality [47–50]. A Dutch study in a community-dwelling population aged >85 years suggested that the inverse association between SBP and mortality disappears after adjustment for comorbidities [50]. A decline in BP over time in older hypertensive subjects is common and has even been observed in the control group of the HYVET study. This decline has been associated with increased mortality [51, 52]. BP may decrease as a result of incident heart failure or other comorbidities. However, a recent retrospective study in diabetic patients has shown that blood pressure decreases in the 4 years preceding death, more rapidly than in surviving age-matched patients, and that this observation is not accounted for by age, sex, race, medications, and comorbidities [52]. Reduced blood pressure may also be associated with features of malnutrition, such as reduced salt intake or weight loss. Being overweight and/or obese is associated with elevated blood pressure via multiple mechanisms including hyperinsulinemia or insulin resistance, hyperleptinemia, and activation of the hypothalamic melanocortin system [53]. Weight loss could possibly lower blood pressure by antagonizing these mechanisms. Irrespective of the underlying mechanism(s), when a decreasing BP is a marker of declining health, a high BP may become a marker of good health in a phenomenon of reverse causality. In the presence of arterial stiffness, declining BP may further decrease an already low DBP, which in turn leads to lower coronary perfusion [54]. Patients with former hypertension may carry a worse prognosis than those with stable hypertension while being classified as nonhypertensive, thus confusing the classical association between BP and mortality. Of particular interest, this reverse relationship between BP and mortality is observed in very old and/or frail and polypathological, polymedicated subjects. Alternative approaches for the estimation of CV risk in these subjects, such as direct measurements of arterial functional properties could actually provide better information [55].
The inverse epidemiological association between BP and mortality should not lead to the denial of the benefits of antihypertensive therapy documented in clinical trials. However, the issues of reverse causality confuse the risk stratification according to BP. The progressive decline in BP over time in older patients also suggests that the requirements for antihypertensive treatment may decrease over time. In our view this issue clearly deserves more attention from both clinicians and researchers. Strategies for verifying whether a given treatment remains appropriate over time would be welcome. For the time being, adhering to blood pressure targets—and avoiding going much lower—is probably the best way to avoid overtreatment, not only at the initiation of therapy, but also during follow-up. Unfortunately, precise guidelines cannot be proposed, as there is no simple lower BP threshold below which treatment reduction should always be attempted. Another important issue is the management of putative drug side effects. If faced with a putative drug side effect, it may be quite rewarding to stop the drug rather than to replace it, and to add a new one only if the SBP rises again above targets.
9 Conclusions
The treatment of arterial hypertension is a key strategy for the prevention of stroke and heart failure even in very old hypertensive patients. However, it is a challenging public health task given the sheer number of patients, the complexity, duration, and cost of treatment, and safety issues. To avoid overtreatment, it is important to confirm the diagnosis with ABPM or by BP monitoring at home. A systolic BP of 150 mmHg is an acceptable cut-off value both for the diagnosis of hypertension and as a target for treatment in most patients >80 years old. Avoiding going too low is important for treatment safety. Treatment should be initiated and followed up in a shared decision-making process, taking the patients’ preferences into account. These strategies will help to ensure treatment adequacy and safety. Conversely, the fear of drug-induced OH should in itself only rarely be a reason not to treat. The possibility that the prognostic value of high BP and the benefits of antihypertensive drugs decrease in very old and frail subjects must be kept in mind. Such a decrease may render patients more vulnerable to drug side effects. Avoiding going too low is important not only at the initiation of therapy, but also during follow-up.
References
Lakatta EG, Levy D (2003) Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: part I: aging arteries: a “set up” for vascular disease. Circulation 107:139–146
Franklin SS, Gustin WIV, Wong ND et al (1997) Hemodynamic patterns of age-related changes in blood pressure: the framingham heart study. Circulation 96:308–315
Benetos A, Salvi P, Lacolley P (2011) Blood pressure regulation during the aging process: the end of the ‘hypertension era’? J Hypertens 29:646–652
Staessen JA, Fagard R, Thijs L et al (1997) Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The systolic hypertension in Europe (Syst-Eur) trial investigators. Lancet 350:757–764
Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension (1991) Final results of the systolic hypertension in the elderly program (SHEP). SHEP cooperative research group. JAMA 265:3255–3264
Beckett NS, Peters R, Fletcher AE et al (2008) Treatment of hypertension in patients 80 years of age or older. N Engl J Med 358:1887–1898
Vyssoulis G, Karpanou E, Adamopoulos D et al (2011) Effect of age on interdependence and hierarchy of cardiovascular risk factors in hypertensive patients. Am J Cardiol 108:240–245
Fagard RH, Staessen JA, Thijs L et al (2000) Response to antihypertensive therapy in older patients with sustained and nonsustained systolic hypertension. Systolic hypertension in Europe (Syst-Eur) trial investigators. Circulation 102:1139–1144
Aronow WS, Fleg JL, Pepine CJ et al (2011) ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American college of cardiology foundation task force on clinical expert consensus documents developed in collaboration with the American academy of neurology, American geriatrics society, American society for preventive cardiology, American society of hypertension, American society of nephrology, association of black cardiologists, and European society of hypertension. J Am Coll Cardiol 57:2037–2114
The ACCORD Study Group (2010) Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 362:1575–1585
Budnitz DS, Lovegrove MC, Shehab N, Richards CL (2011) Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 365:2002–2012
Alberti KG, Zimmet P, Shaw J (2006) Metabolic syndrome–a new world-wide definition. A consensus statement from the international diabetes federation. Diabetes Med 23:469–480
The Diabetes Prevention Program Research Group (2005) Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program. Diabetes Care 28:888–894
Thomas F, Pannier B, Benetos A, Vischer UM (2011) The impact of the metabolic syndrome—but not of hypertension—on all-cause mortality disappears in the elderly. J Hypertens 29:663–668
Wang J, Ruotsalainen S, Moilanen L et al (2007) The metabolic syndrome predicts cardiovascular mortality: a 13-year follow-up study in elderly non-diabetic Finns. Eur Heart J 28:857–864
Salminen M, Kuoppamaki M, Vahlberg T et al (2010) The metabolic syndrome defined by modified international diabetes federation criteria and mortality: a 9-year follow-up of the aged in Finland. Diabetes Metab 36:437–442
Stevens J, Cai J, Pamuk ER et al (1998) The effect of age on the association between body-mass index and mortality. N Engl J Med 338:1–7
Vischer UM, Safar ME, Safar H et al (2009) Cardiometabolic determinants of mortality in a geriatric population: is there a “reverse metabolic syndrome”? Diabetes Metab 35:108–114
Janssen I, Katzmarzyk PT, Ross R (2005) Body mass index is inversely related to mortality in older people after adjustment for waist circumference. J Am Geriatr Soc 53:2112–2118
Curb JD, Pressel SL, Cutler JA et al (1996) Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic hypertension in the elderly program cooperative research group. JAMA 276:1886–1892
Tuomilehto J, Rastenyte D, Birkenhager WH et al (1999) Effects of calcium-channel blockade in older patients with diabetes and systolic hypertension. Systolic hypertension in Europe trial investigators. N Engl J Med 340:677–684
Vischer UM, Bauduceau B, Bourdel-Marchasson I et al (2009) A call to incorporate the prevention and treatment of geriatric disorders in the management of diabetes in the elderly. Diabetes Metab 35:168–177
Laurent S, Cockcroft J, Van Bortel L et al (2006) Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 27:2588–2605
Masaki KH, Schatz IJ, Burchfiel CM et al (1998) Orthostatic hypotension predicts mortality in elderly men: the Honolulu heart program. Circulation 98:2290–2295
Rutan GH, Hermanson B, Bild DE et al. (1992) Orthostatic hypotension in older adults. The cardiovascular health study. CHS collaborative research group. Hypertension 19:508–519
Valbusa F, Labat C, Salvi P et al (2012) Orthostatic hypotension in very old individuals living in nursing homes: the PARTAGE study. J Hypertens 30:53–60
Lipsitz LA (1989) Orthostatic hypotension in the elderly. N Engl J Med 321:952–957
Mattace-Raso FU, van der Cammen TJ, Knetsch AM et al (2006) Arterial stiffness as the candidate underlying mechanism for postural blood pressure changes and orthostatic hypotension in older adults: the Rotterdam study. J Hypertens 24:339–344
Kamaruzzaman S, Watt H, Carson C, Ebrahim S (2010) The association between orthostatic hypotension and medication use in the British women’s heart and health study. Age Ageing 39:51–56
Woolcott JC, Richardson KJ, Wiens MO et al (2009) Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 169:1952–1960
Elias MF, Wolf PA, D’Agostino RB et al (1993) Untreated blood pressure level is inversely related to cognitive functioning: the Framingham study. Am J Epidemiol 138:353–364
Launer LJ, Ross GW, Petrovitch H et al (2000) Midlife blood pressure and dementia: the Honolulu-Asia aging study. Neurobiol Aging 21:49–55
Skoog I, Lernfelt B, Landahl S et al (1996) 15-year longitudinal study of blood pressure and dementia. Lancet 347:1141–1145
Tzourio C, Dufouil C, Ducimetiere P, Alperovitch A (1999) Cognitive decline in individuals with high blood pressure: a longitudinal study in the elderly. EVA study group. Epidemiology of vascular aging. Neurology 53:1948–1952
Desmond DW, Tatemichi TK, Paik M, Stern Y (1993) Risk factors for cerebrovascular disease as correlates of cognitive function in a stroke-free cohort. Arch Neurol 50:162–166
Di Carlo A, Baldereschi M, Amaducci L et al (2000) Cognitive impairment without dementia in older people: prevalence, vascular risk factors, impact on disability. The Italian longitudinal study on aging. J Am Geriatr Soc 48:775–782
Watfa G, Rossignol P, Kearney-Schwartz A et al (2010) Use of calcium channel blockers is associated with better cognitive performance in older hypertensive patients with subjective memory complaints. J Hypertens 28:2485–2493
Forette F, Seux ML, Staessen JA et al (2002) The prevention of dementia with antihypertensive treatment: new evidence from the systolic hypertension in Europe (Syst-Eur) study. Arch Intern Med 162:2046–2052
Tzourio C, Anderson C, Chapman N et al (2003) Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Arch Intern Med 163:1069–1075
Lithell H, Hansson L, Skoog I et al (2003) The study on cognition and prognosis in the elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens 21:875–886
McGuinness B, Todd S, Passmore P, Bullock R (2009) Blood pressure lowering in patients without prior cerebrovascular disease for prevention of cognitive impairment and dementia. Cochrane Datab Syst Rev (4):CD004034
Peters R, Beckett N, Forette F et al (2008) Incident dementia and blood pressure lowering in the Hypertension in the very elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol 7:683–689
Peters R, Beckett N, Beardmore R et al (2010) Modelling cognitive decline in the Hypertension in the very elderly trial [HYVET] and proposed risk tables for population use. PLoS ONE 5:e11775
Benetos A, Watfa G, Hanon O et al (2012) Pulse wave velocity is associated with 1-year cognitive decline in the elderly older than 80 years: the PARTAGE study. J Am Med Dir Assoc 13:239–243
Kearney-Schwartz A, Rossignol P, Bracard S et al (2009) Vascular structure and function is correlated to cognitive performance and white matter hyperintensities in older hypertensive patients with subjective memory complaints. Stroke 40:1229–1236
Perret-Guillaume C, Genet C, Herrmann FR et al (2011) Attitudes and approaches to decision making about antihypertensive treatment in elderly patients. J Am Med Dir Assoc 12:121–128
Langer RD, Ganiats TG, Barrett-Connor E (1989) Paradoxical survival of elderly men with high blood pressure. BMJ 298:1356–1357
van Hateren KJJ, Landman GWD, Kleefstra N et al (2010) Lower blood pressure associated with higher mortality in elderly diabetic patients (ZODIAC-12). Age Ageing 39:603–609
Rönnback M, Isomaa B, Fagerudd J et al (2006) Complex relationship between blood pressure and mortality in type 2 diabetic patients. Hypertension 47:168–173
Boshuizen HC, Izaks GJ, van Buuren S, Ligthart GJ (1998) Blood pressure and mortality in elderly people aged 85 and older: community based study. BMJ 316:1780–1784
Satish S, Zhang DD, Goodwin JS (2001) Clinical significance of falling blood pressure among older adults. J Clin Epidemiol 54:961–967
Rogers MAM, Ward K, Gure TR et al (2011) Blood pressure trajectories prior to death in patients with diabetes. Diabetes Care 34:1534–1539
Greenfield JR, Miller JW, Keogh JM et al (2009) Modulation of blood pressure by central melanocortinergic pathways. N Engl J Med 360:44–52
Messerli FH, Mancia G, Conti CR et al (2006) Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann Intern Med 144:884–893
Benetos A, Buatois S, Salvi P et al (2010) Blood pressure and pulse wave velocity values in the institutionalized elderly aged 80 and over: baseline of the PARTAGE study. J Hypertens 28:41–50
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag Italia
About this chapter
Cite this chapter
Benetos, A., Vischer, U.M., Watfa, G. (2012). Hypertension in the Very Old: Special Features, Therapeutic Approaches, and Problems. In: Berbari, A., Mancia, G. (eds) Special Issues in Hypertension. Springer, Milano. https://doi.org/10.1007/978-88-470-2601-8_5
Download citation
DOI: https://doi.org/10.1007/978-88-470-2601-8_5
Published:
Publisher Name: Springer, Milano
Print ISBN: 978-88-470-2600-1
Online ISBN: 978-88-470-2601-8
eBook Packages: MedicineMedicine (R0)