Abstract
The risk of colorectal cancer (CRC) in the ulcerative colitis (UC) population is real and is the cause of death for up to 15 % of inflammatory bowel disease (IBD) patients. Controversy surrounds the use of prophylactic colectomy when dysplasia is detected. The relatively high risk of progression to CRC must be weighed against the risks associated with total proctocolectomy (TPC) ± ileal pouch anal anastomosis (IPAA), which, in contrast, are relatively low, particularly when performed in an elective setting and by an experienced surgeon. In addition to substantially reducing the CRC risk, TPC results in the elimination of future UC flares and the necessity for medical treatment whilst eliminating the need for frequent CRC surveillance. As more powerful techniques for lesion detection become widespread, the detection of dysplasia will likely increase, increasing the relevance of the question ‘What is the most appropriate management of patients with ulcerative colitis and dysplasia?’
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Inflammatory Bowel Disease
- Ulcerative Colitis
- Primary Sclerosing Cholangitis
- Endoscopic Mucosal Resection
- Ulcerative Colitis Patient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The risk of colorectal cancer (CRC) in the ulcerative colitis (UC) population is real and is the cause of death for up to 15 % of inflammatory bowel disease (IBD) patients [1, 2]. Controversy surrounds the use of prophylactic colectomy when dysplasia is detected. The relatively high risk of progression to CRC must be weighed against the risks associated with total proctocolectomy (TPC) ± ileal pouch anal anastomosis (IPAA), which, in contrast, are relatively low, particularly when performed in an elective setting and by an experienced surgeon. In addition to substantially reducing the CRC risk, TPC results in the elimination of future UC flares and the necessity for medical treatment whilst eliminating the need for frequent CRC surveillance. As more powerful techniques for lesion detection become widespread, the detection of dysplasia will likely increase, increasing the relevance of the question ‘What is the most appropriate management of patients with ulcerative colitis and dysplasia?’
Search Strategy
The PubMed database was searched using the following terms ‘dysplasia, carcinoma, neoplasia, DALM, ALM, dysplasia associated mass or lesion, adenoma like lesion or mass and ulcerative colitis or inflammatory bowel disease or IBD.’ The search was limited to full length English language manuscripts published between Jan 1, 1980 and Oct 1, 2015. All references in each manuscript identified from the PubMed search were then individually reviewed and examined for relevance and potential inclusion.
Incidences of Dysplasia and Colorectal Cancer (CRC)
Studies on UC dysplasia typically provide incidence rates obtained from the use of conventional endoscopy. Any grade of dysplasia is found in up to 2 % of UC patients at 5 years and 33 % at 15 years [4, 18]. Ten and 15 year rates of high grade dysplasia (HGD) of 7 % and 12 % respectively have been reported. Similar to CRC, incidence is highest in patients with pancolitis [15].
Median time from UC diagnosis to CRC diagnosis varies from 4 to 23 years [4, 19]. Compared to the general population, the relative risk of CRC in UC patients is as high as 16-fold [20]. Meta-analysis inclusive of 116 studies has demonstrated an overall prevalence of CRC in UC patients of 3.7 %, increasing to 5.4 % in the presence of pancolitis [21]. IBD-CRC patients are approximately 7 years younger than sporadic CRC and share the same cancer specific mortality rates on a stage for stage basis [22]. The mean age at CRC diagnosis ranges from 43 to 60 years and the mean interval between diagnosis of UC and CRC is approximately 16 years [17, 23, 24], which is consistent with the majority of UC diagnoses being made in individuals in their 20s to early 30s [21].
Disease Defined Risk Factors: Disease Duration, Age of Onset, Disease Extent, PSC
CRC incidence dramatically increases 8–10 years after the onset of UC symptoms. Cumulative probabilities of developing CRC are up to 4 % by 10 years and 8 % by 20 years [15, 21, 25]. Rates after 30 years are less uniformly reported and vary from 2.6 to 34 % [20, 25, 26]. Primary sclerosing cholangitis (PSC) has consistently been shown to increase the risk of CRC through a yet undetermined pathophysiological mechanism. Studies on a potential correlation between young age at UC diagnosis and/or childhood onset and CRC are conflicting with the majority showing no correlation [25]. Dysplasia is typically but not universally found in areas of current or burnt out colitis [27, 28], leading to an increased risk in more extensive disease distribution [20, 25]. An earlier CRC onset has also been suggested in pan vs left sided colitis [29].
Patient Defined Risk Factors: Family History of CRC, Medication Usage, Smoking, Patient Awareness
Family history is a known risk factor for both sporadic carcinoma and IBD associated CRC. CRC risk is at least doubled in UC patients with relatives with CRC and is ninefold greater if the relative is under the age of 50 at CRC diagnosis [23, 30]. Conversely, a family history of IBD does not increase UC-CRC risk [20]. Studies on medication usage in UC and CRC are limited to the older anti-inflammatory drugs, with data on the newer biologics and anti-integrins lacking. Several previous studies including a meta-analysis of 9 studies and 1932 patients, have suggested a protective effect with regular 5-aminosalicylic acid (5-ASA) use [21, 23, 24, 31]. Although a paradoxical effect of smoking and decreased UC incidence and disease severity is well known, the effect of smoking on UC-CRC risk is understudied. Eaden’s small case control study demonstrated no association [23].
CRC risk may be underappreciated by UC patients themselves and probably negatively impacts care. The majority of 199 survey respondents with UC for an average of 8 years recognized that CRC risk was increased, however approximately 75 % stated that they were “unlikely” or “very unlikely” to develop CRC within the next 10 years [32].
Classification of UC Dysplasia
Dysplasia in UC has typically been regarded as flat in most cases. When it is raised and found within areas of inflammation, it has been termed a dysplasia associated lesion or mass (DALM) and classically has been viewed as colonoscopically unresectable. These definitions and concepts are now in question with the development of newer more advanced techniques of endoscopic polyp removal. A polypoid lesion found in an area free of inflammation is termed an adenoma-like mass or lesion (ALM) and is akin to an adenomatous polyp in a non-UC patient.
Grading of dysplasia ranges from mild or low grade (LGD) to more severe or high grade dysplasia (HGD). LGD is histologically similar to inflammation with tall columnar epithelial cells with mild nuclear stratification. HGD is similar to carcinoma in situ [7]. Salient features of HGD include prominent heterochromatin and more irregular nuclear stratification within the epithelial layer. These subtle differences lead to poor interobserver agreement between grading pathologists especially for LGD. When LGD slides are reviewed by a second set of pathologists, agreement with the original LGD diagnosis ranges from 7 to 43 % and varies depending on the number of pathologists reviewing [4, 11, 33, 34]. Dixon et al demonstrated a similarly poor consensus of agreement on HGD, as low as 33 % [35]. Correlation was not improved when specialist gastrointestinal pathologists grated the specimens, compared to general histopathologists [36].
1. A second pathologist’s opinion for LGD is often necessary (Strong recommendation based on moderate-high quality evidence).
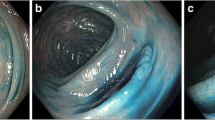
Inadequate tissue sampling during colonoscopy may lead to missed lesions. Mathematical modelling to determine the number of random biopsies required to detect dysplasia with 90 % confidence calculated that 45 biopsies would be required. When the number of biopsies decreases to 10, 26 % confidence was predicted [37, 38]. New enhanced methods of lesion detection including chromoendoscopy which began in the early 2000s, have dramatically increased the sensitivity of surveillance colonoscopy particularly for difficult to detect, flat dysplastic lesions [39–42].
Dysplasia Management
Neoplastic Progression
Unlike sporadic CRC which follows a usual sequence of normal mucosa → adenoma → carcinoma, UC associated CRC does not necessarily follow the expected progression of LGD → HGD → CRC. This makes surgical recommendations problematic, especially in the individual patient. As demonstrated in several studies in Table 10.2, carcinoma is often detected in colectomy specimens in which only LGD or even no dysplasia was detected in prior colonoscopies. In Stolwijk’s study of over 290 UC patients undergoing surveillance, LGD preceded HGD or CRC in only 44 % of cases [15]. None of the 5 of 46 flat LGD (fLGD) patients that progressed to CRC had an interval finding of HGD in Ullman’s study [43]. In Rutter’s surveillance program of 600 patients with extensive colitis, CRC was found in 20 % of specimens that were resected for only LGD [12]. Choi and Zisman report similar rates of unexpected CRC in resections performed for LGD [3, 5].
A focus of UC dysplasia, especially HGD has been suggested to be a marker for synchronous lesions, including CRC [44–46]. An early study of 590 UC TPC specimens demonstrated that patients with a focus of HGD or LGD were 36 times more likely to have a concomitant CRC found as compared to UC specimens without dysplasia. Up to a 25 % synchronous tumor rate and 55 % synchronous dysplasia rate has been demonstrated in other TPC studies [19, 47].
Flat LGD
In patients with LGD and extensive UC for over 8 years, progression to CRC has been reported to be 13 % at 1 year to 33 % at 5 years [3, 5, 6, 10, 12, 15, 18] with a mean time to progression of 1.8–2.3 years [5, 6, 10]. Woolrich determined LGD to be an indicator of future carcinoma in 18 % of 121 patients [8]. A meta-analysis of 20 studies with 508 LGD patients provided a calculated positive predictive value (PPV) of 22 % for flat LGD (fLGD) as a predictor of CRC [48]. Zisman determined nonpolyoid dysplasia, size >1 cm, previous history of indefinite dysplasia and the presence of a stricture as risk factors for LGD progression. He stratified patients showing that CRC risk at 5 years ranged from 1.8 % in patients with no risk factors to over 60 % with three risk factors [3]. Befrits’ study, the only study which has shown no progression of LGD to subsequent HGD or CRC was small with only 16 patients with LGD [9]. Multiple retrospective studies and Thomas’ meta-analysis did not demonstrate differences in characteristics between patients with and without LGD prior to HGD and/or CRC [6, 15, 48] again showing the difficulty in making care recommendations in the specific patient.
2. Flat LGD warrants colectomy in the otherwise healthy patient due to the increased risk of unrecognized synchronous high risk lesions and the likelihood of developing subsequent HGD or CRC (Strong recommendation based on moderate-high quality evidence).
High Grade Dysplasia
Recent studies on long term HGD surveillance are lacking as patients typically undergo resection due an inordinately high risk of synchronous CRC, as high as 45 % in earlier studies [49, 50]. In a systematic review, 32 % (of 47 patients) with HGD on colonoscopy had CRC discovered on resection pathology [50]. Some smaller studies report lower rates, [27] but sampling errors, the need for repetitive colonoscopy, and the fear of synchronous CRC or progression over time has led to TPC being the immediate recommendation in the otherwise healthy UC patient with HGD. HGD identified on random biopsies represents an especially concerning circumstance, since overt signs of polyp formation that would focus the attention of the examiner is lacking. Similarly, multiple areas of dysplasia, especially when flat, can only be addressed by colectomy.
3. HGD, multifocality and flat dysplasia are all high risk features for the development of CRC in the UC patient and warrants total proctocolectomy in the surgically fit patient (Strong recommendation based on moderate-high quality evidence).
DALMS
The PPV for DALMs as predictors of CRC is 41 % as calculated by meta-analysis [48]. 43 % of 47 DALM patients in the small systematic review described above were found to ultimately have CRC [50]. Blackstone et al described a series of 12 resected DALMs. CRC was found in 7, including all 5 single polypoid masses. None had invasive carcinoma on preoperative biopsy [7]. Selective resection of DALMs in the form of polypectomy was proposed by one meta-analysis of 10 studies and 376 UC patients, but with a mean follow up of only 2.8 colonoscopies after resection. Many of these studies had very low patient numbers and mean follow up and number of colonscopies varied greatly across the study cohorts included [17]. Kisiel reported higher rates in 77 of 95 DALM patients who underwent polypectomy with cumulative incidences of cancer of 2 % at 1 year and 13 % at 5 years cited [51]. The value of more advanced colon sparing techniques such as endoscopic mucosal resection, has not been fully evaluated in this high risk group of patients. Thus close colonoscopic surveillance is required after colonoscopic excision.
4. DALMS should be viewed as very high risk lesions in the UC patient justifying TPC in most fit individuals. If able to be completely removed colonoscopically, aggressive subsequent surveillance is necessary (Strong recommendation based on moderate-high quality evidence).
ALMS
By definition, ALMs are within areas of the colon without inflammation. Thus they may be treated similarly to sporadic adenomas due to a low risk of CRC. Hurlstone followed ALMs and DALMs in over 180 patients over a median follow-up of 4.1 years as compared with over 1600 non-UC Controls who had undergone endoscopic mucosal resection (EMR) or polypectomy for lesions. Recurrence rates were low in both groups [52]. Torres et al studied ALMs and DALMs in 59 CD and UC patients and found that CRC only developed in DALMs. However, the group was highly selected leading to the recommendation of endoscopic resection with close, 6 monthly surveillance with colonoscopy [30].
5. ALMs can be viewed as typical polyps, amenable to polypectomy (Weak recommendation based on low quality evidence).
A Personal View of the Data
Due to the lack of consistent progression of inflammation to LGD to HGD to CRC, recommendations for surgical management of UC dysplasia leans towards treating the worst case scenario. This is especially the case since UC patients with dysplasia are frequently middle aged with a life expectancy that should not be foreshortened by preventable malignancy. Couple this with the above described poor concordance between pathologists and one is frequently led to the recommendation of early resection when any form of dysplasia is found on colonoscopy, but especially when HGD or flat dysplasia is found on random sampling. The high incidence of unexpected synchronous CRC when TPC is done for dysplasia further justifies an aggressive surgical approach.
Recently, chromoendoscopy has suggested itself to be a more sensitive and accurate method of following the equivocal patient; however this has not been thoroughly studied. Similarly the use of EMR for DALMs is also understudied, but really is only considered in highly specialized centers by very committed caregivers, and then only with intense colonoscopic follow up (every 6 months). This surveillance itself becomes an added burden, with attendant complications, costs and potential difficulty with patient compliance.
Thus, in the surgically fit patient we advocate TPC in all patients with any grade of pathologically confirmed dysplasia [45]. In the patient with LGD, this may sometimes require a second colonoscopy (frequently chromoendoscopy) for confirmatory biopsies, possibly after a period of intense medical management to minimize inflammation. However, any single confirmed focus of HGD should send the otherwise healthy and consenting patient directly to surgery. Besides eliminating the risk of CRC, patients are effectively “cured” of their colitis by TPC, with elimination of most medications and their attendant side effects and costs, improvement in bowel habit (especially with the IPAA) and elimination of burdensome surveillance colonoscopies [53]. The more difficult dilemma is the surgical high risk or elderly patient or patient refusing surgery, who has a less compelling indication for surgery, a single focus of LGD for example. After thorough counselling, such a patient can be considered for close surveillance using chromoendoscopy and/or EMR if a lesion is visualized. If the dysplasia is colonic (not rectal), and localized as can be best determined, a subtotal colectomy and ileorectal anastomosis, or even segmental colectomy will decrease the risk of synchronous or metachronous lesions, and will be surgically less morbid. The patient will still need close colonoscopic surveillance, however. Similarly, a segmental resection (or even TAC/IRA) for DALM is possible in the higher risk patient. It avoids a stoma, but any procedure less that TPC needs preoperative confirmation of a dysplasia free rectum which then requires continued surveillance after this more limited surgery.
References
Averboukh F, Ziv Y, Kariv Y, et al. Colorectal carcinoma in inflammatory bowel disease: a comparison between Crohn’s and ulcerative colitis. Colorectal Dis. 2011;13:1230–5.
Connelly TM, Koltun WA. The cancer “fear” in IBD patients: is it still REAL? J Gastrointest Surg. 2014;18:213–8.
Choi CH, Ignjatovic-Wilson A, Askari A, et al. Low-grade dysplasia in ulcerative colitis: risk factors for developing high-grade dysplasia or colorectal cancer. Am J Gastroenterol. 2015;110:1461–71.
Jess T, Loftus Jr EV, Velayos FS, et al. Incidence and prognosis of colorectal dysplasia in inflammatory bowel disease: a population-based study from Olmsted County, Minnesota. Inflamm Bowel Dis. 2006;12:669–76.
Zisman TL, Bronner MP, Rulyak S, et al. Prospective study of the progression of low-grade dysplasia in ulcerative colitis using current cancer surveillance guidelines. Inflamm Bowel Dis. 2012;18:2240–6.
Ullman T, Croog V, Harpaz N, Sachar D, Itzkowitz S. Progression of flat low-grade dysplasia to advanced neoplasia in patients with ulcerative colitis. Gastroenterology. 2003;125:1311–9.
Blackstone MO, Riddell RH, Rogers BHG, Levin B. Dysplasia-associated lesion or mass (DALM) detected by colonoscopy in long-standing ulcerative-colitis – an indication for colectomy. Gastroenterology. 1981;80:366–74.
Woolrich AJ, DaSilva MD, Korelitz BI. Surveillance in the routine management of ulcerative colitis: the predictive value of low-grade dysplasia. Gastroenterology. 1992;103:431–8.
Befrits R, Ljung T, Jaramillo E, Rubio C. Low-grade dysplasia in extensive, long-standing inflammatory bowel disease: a follow-up study. Dis Colon Rectum. 2002;45:615–20.
Ullman TA, Loftus Jr EV, Kakar S, Burgart LJ, Sandborn WJ, Tremaine WJ. The fate of low grade dysplasia in ulcerative colitis. Am J Gastroenterol. 2002;97:922–7.
Lim CH, Dixon MF, Vail A, Forman D, Lynch DA, Axon AT. Ten year follow up of ulcerative colitis patients with and without low grade dysplasia. Gut. 2003;52:1127–32.
Rutter MD, Saunders BP, Wilkinson KH, et al. Thirty-year analysis of a colonoscopic surveillance program for neoplasia in ulcerative colitis. Gastroenterology. 2006;130:1030–8.
Pekow JR, Hetzel JT, Rothe JA, et al. Outcome after surveillance of low-grade and indefinite dysplasia in patients with ulcerative colitis. Inflamm Bowel Dis. 2010;16:1352–6.
Goldstone R, Itzkowitz S, Harpaz N, Ullman T. Progression of low-grade dysplasia in ulcerative colitis: effect of colonic location. Gastrointest Endosc. 2011;74:1087–93.
Stolwijk JA, Langers AM, Hardwick JC, et al. A thirty-year follow-up surveillance study for neoplasia of a dutch ulcerative colitis cohort. Sci World J. 2013;2013:274715.
Provenzale D, Kowdley KV, Arora S, Wong JB. Prophylactic colectomy or surveillance for chronic ulcerative colitis? A decision analysis. Gastroenterology. 1995;109:1188–96.
Wanders LK, Dekker E, Pullens B, Bassett P, Travis SP, East JE. Cancer risk after resection of polypoid dysplasia in patients with longstanding ulcerative colitis: a meta-analysis. Clin Gastroenterol Hepatol. 2014;12:756–64.
Lofberg R, Brostrom O, Karlen P, Tribukait B, Ost A. Colonoscopic surveillance in long-standing total ulcerative colitis – a 15-year follow-up study. Gastroenterology. 1990;99:1021–31.
Choi PM, Zelig MP. Similarity of colorectal cancer in Crohn’s disease and ulcerative colitis: implications for carcinogenesis and prevention. Gut. 1994;35:950–4.
Askling J, Dickman PW, Karlen P, et al. Family history as a risk factor for colorectal cancer in inflammatory bowel disease. Gastroenterology. 2001;120:1356–62.
Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48:526–35.
Bansal P, Sonnenberg A. Risk factors of colorectal cancer in inflammatory bowel disease. Am J Gastroenterol. 1996;91:44–8.
Eaden J, Abrams K, Ekbom A, Jackson E, Mayberry J. Colorectal cancer prevention in ulcerative colitis: a case-control study. Aliment Pharmacol Ther. 2000;14:145–53.
Pinczowski D, Ekbom A, Baron J, Yuen J, Adami HO. Risk factors for colorectal cancer in patients with ulcerative colitis: a case-control study. Gastroenterology. 1994;107:117–20.
Gyde SN, Prior P, Allan RN, et al. Colorectal-cancer in ulcerative-colitis – a cohort study of primary referrals from 3 centers. Gut. 1988;29:206–17.
Greenstein AJ, Slater G, Heimann TM, Sachar DB, Aufses Jr AH. A comparison of multiple synchronous colorectal cancer in ulcerative colitis, familial polyposis coli, and de novo cancer. Ann Surg. 1986;203:123–8.
Rutter M, Saunders B, Wilkinson K, et al. Severity of inflammation is a risk factor for colorectal neoplasia in ulcerative colitis. Gastroenterology. 2004;126:451–9.
Gupta RB, Harpaz N, Itzkowitz S, et al. Histologic inflammation is a risk factor for progression to colorectal neoplasia in ulcerative colitis: a cohort study. Gastroenterology. 2007;133:1099–105; quiz 1340–1091.
Greenstein AJ, Sachar DB, Pucillo A, et al. Cancer in universal and left-sided ulcerative colitis: clinical and pathologic features. Mt Sinai J Med. 1979;46:25–32.
Nuako KW, Ahlquist DA, Mahoney DW, Schaid DJ, Siems DM, Lindor NM. Familial predisposition for colorectal cancer in chronic ulcerative colitis: a case-control study. Gastroenterology. 1998;115:1079–83.
Velayos FS, Terdiman JP, Walsh JM. Effect of 5-aminosalicylate use on colorectal cancer and dysplasia risk: a systematic review and metaanalysis of observational studies. Am J Gastroenterol. 2005;100:1345–53.
Siegel CA, Schwartz LM, Woloshin S, et al. When should ulcerative colitis patients undergo colectomy for dysplasia? Mismatch between patient preferences and physician recommendations. Inflamm Bowel Dis. 2010;16:1658–62.
Eaton JE, Smyrk TC, Imam M, et al. The fate of indefinite and low-grade dysplasia in ulcerative colitis and primary sclerosing cholangitis colitis before and after liver transplantation. Aliment Pharmacol Ther. 2013;38:977–87.
van Schaik FD, ten Kate FJ, Offerhaus GJ, et al. Misclassification of dysplasia in patients with inflammatory bowel disease: consequences for progression rates to advanced neoplasia. Inflamm Bowel Dis. 2011;17:1108–16.
Dixon MF, Brown LJ, Gilmour HM, et al. Observer variation in the assessment of dysplasia in ulcerative colitis. Histopathology. 1988;13:385–97.
Eaden J, Abrams K, McKay H, Denley H, Mayberry J. Inter-observer variation between general and specialist gastrointestinal pathologists when grading dysplasia in ulcerative colitis. J Pathol. 2001;194:152–7.
Rubin CE, Haggitt RC, Burmer GC, et al. DNA aneuploidy in colonic biopsies predicts future-development of dysplasia in ulcerative-colitis. Gastroenterology. 1992;103:1611–20.
Awais D, Siegel CA, Higgins PD. Modelling dysplasia detection in ulcerative colitis: clinical implications of surveillance intensity. Gut. 2009;58:1498–503.
Marion JF, Waye JD, Present DH, et al. Chromoendoscopy-targeted biopsies are superior to standard colonoscopic surveillance for detecting dysplasia in inflammatory bowel disease patients: a prospective endoscopic trial. Am J Gastroenterol. 2008;103:2342–9.
Kiesslich R, Fritsch J, Holtmann M, et al. Methylene blue-aided chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2003;124:880–8.
Pellise M, Lopez-Ceron M, Rodriguez de Miguel C, et al. Narrow-band imaging as an alternative to chromoendoscopy for the detection of dysplasia in long-standing inflammatory bowel disease: a prospective, randomized, crossover study. Gastrointest Endosc. 2011;74:840–8.
Subramanian V, Mannath J, Ragunath K, Hawkey CJ. Meta-analysis: the diagnostic yield of chromoendoscopy for detecting dysplasia in patients with colonic inflammatory bowel disease. Aliment Pharmacol Ther. 2011;33:304–12.
Ullman T, Croog V, Harpaz N, et al. Progression to colorectal neoplasia in ulcerative colitis: effect of mesalamine. Clin Gastroenterol Hepatol. 2008;6:1225–30; quiz 1177.
Allen DC, Biggart JD, Pyper PC. Large bowel mucosal dysplasia and carcinoma in ulcerative colitis. J Clin Pathol. 1985;38:30–43.
Connelly TM, Koltun WA. The surgical treatment of inflammatory bowel disease-associated dysplasia. Exp Rev Gastroenterol Hepatol. 2013;7:307–21; quiz 322.
Ransohoff DF, Riddell RH, Levin B. Ulcerative colitis and colonic cancer. Problems in assessing the diagnostic usefulness of mucosal dysplasia. Dis Colon Rectum. 1985;28:383–8.
Kiran RP, Khoury W, Church JM, Lavery IC, Fazio VW, Remzi FH. Colorectal cancer complicating inflammatory bowel disease: similarities and differences between Crohn’s and ulcerative colitis based on three decades of experience. Ann Surg. 2010;252:330–5.
Thomas T, Abrams KA, Robinson RJ, Mayberry JF. Meta-analysis: cancer risk of low-grade dysplasia in chronic ulcerative colitis. Aliment Pharmacol Ther. 2007;25:657–68.
Gorfine SR, Bauer JJ, Harris MT, Kreel I. Dysplasia complicating chronic ulcerative colitis: is immediate colectomy warranted? Dis Colon Rectum. 2000;43:1575–81.
Bernstein CN, Shanahan F, Weinstein WM. Are we telling patients the truth about surveillance colonoscopy in ulcerative-colitis. Lancet. 1994;343:71–4.
Kisiel JB, Loftus Jr EV, Harmsen WS, Zinsmeister AR, Sandborn WJ. Outcome of sporadic adenomas and adenoma-like dysplasia in patients with ulcerative colitis undergoing polypectomy. Inflamm Bowel Dis. 2012;18:226–35.
Hurlstone DP, Sanders DS, Atkinson R, et al. Endoscopic mucosal resection for flat neoplasia in chronic ulcerative colitis: can we change the endoscopic management paradigm? Gut. 2007;56:838–46.
Remzi FH, Preen M. Rectal cancer and ulcerative colitis: does it change the therapeutic approach? Colorectal Dis. 2003;5:483–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Additional information
Editor’s Note
The concepts and controversies surrounding the identification and management of dysplasia in IBD are evolving rapidly. It appears that most areas of dysplasia are actually grossly visible with high definition scopes and enhancement techniques (e.g., chromoendoscopy). If lesions can be clearly defined, they can be more readily removed endoscopically and followed carefully with serial endoscopy.
The authors have outlined an aggressive approach, especially to the management of low grade dysplasia; many IBD specialists may espouse a more nuanced view with careful endoscopic surveillance offered as an alternative for many of these patients.
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Connelly, T.M., Koltun, W.A. (2017). IBD: Management of Dysplasia in Patients with Ulcerative Colitis. In: Hyman, N., Umanskiy, K. (eds) Difficult Decisions in Colorectal Surgery. Difficult Decisions in Surgery: An Evidence-Based Approach. Springer, Cham. https://doi.org/10.1007/978-3-319-40223-9_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-40223-9_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-40222-2
Online ISBN: 978-3-319-40223-9
eBook Packages: MedicineMedicine (R0)