Abstract
Purpose of Review
Patients with long-standing ulcerative colitis have an increased risk for the development of colorectal cancer (CRC). Colitis-related dysplasia appears to confer the greatest risk. Colonoscopic surveillance to detect dysplasia has been advocated by gastrointestinal societies. The aim of surveillance is the reduction of mortality and morbidity of CRC through detection and resection of dysplasia or detecting CRC at an earlier and potentially curable stage. Traditional surveillance has relied on mucosal assessment with targeted biopsy of visible lesions and random biopsy sampling on the premise that dysplasia was not visible at endoscopy. Advances in optical technology permitting increased detection of dysplasia and evidence that most dysplasia is visible has had practice-changing implications.
Recent Findings
Emerging evidence favours chromoendoscopy (CE) for dysplasia detection and is gaining wider acceptance through recent international (International Consensus Statement on Surveillance and Management of Dysplasia in Inflammatory Bowel Disease (SCENIC)) recommendations and endorsed by many gastrointestinal societies. Adoption of CE as the gold standard of surveillance has been met with by scepticism, from conflicting data, operational barriers and the need to understand the true impact of increasingly higher dysplasia detection on overall CRC mortality.
Summary
Valid debate notwithstanding, implementation of a risk stratification protocol that includes CE is an effective approach allowing earlier detection of dysplasia and colorectal neoplasia, determination of surveillance intervals with appropriate allocation of resources and limiting morbidity from CRC and colonoscopy itself. Further prospective data should define the true and long-term impact of dysplasia detection with modern techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with long-standing inflammatory bowel disease (IBD) have an increased risk for development of colorectal cancer (CRC) [1]. Risk factors for CRC in ulcerative colitis (UC) include young age of disease onset, longer disease duration, greater extent of colonic involvement, coexistent primary sclerosing cholangitis (PSC), active endoscopic or histological inflammation, family history of CRC in a first-degree relative diagnosed under 50 years, history of dysplasia, colonic strictures, inflammatory (“pseudo”) polyps, a shortened tubular colon and male gender [2, 3, 4••, 5,6,7,8,9,10]. Of these established risk factors, colitis-related dysplasia appears to confer the greatest risk, leading gastrointestinal societies to advocate colonoscopic surveillance to detect dysplasia in high-risk patients [2, 3, 4••, 5,6,7, 9, 11]. The aim of endoscopic surveillance is the reduction of mortality and morbidity of CRC through detection and resection of dysplasia or detecting CRC at an earlier and potentially curable stage [12, 13].
Mucosal assessment with targeted biopsies of visible lesions and random biopsy sampling has long been the basis of surveillance, relying on the prevailing notion that dysplasia is frequently not associated with visible mucosal abnormalities [14]. Advances in optical technology permitting better endoscopic identification of dysplasia and acknowledgement that most dysplasia in IBD patients is in fact visible have significantly influenced our paradigms with dysplasia surveillance and management, providing an impetus for training and adoption of better methods of dysplasia detection with the ultimate aim of reduction of CRC morbidity and mortality [13, 14].
Epidemiology and Risk Factors for CRC in IBD
IBD is the third highest risk factor for the development of CRC, accounting for 1–2% of CRC cases in the general population and being responsible for 10–15% of all deaths in IBD patients [5, 15]. The cumulative CRC risk is considerable, 2% at 10 years, 8% at 20 years and 18% [16]. Recent studies report a decrease in the incidence of CRC and a significant decrease in the rates of colectomy for dysplasia, a temporal reduction attributable to aggressive control of inflammation through newer classes of medications, greater uptake of surveillance, permitting earlier detection and resection of dysplasia before CRC develops and indeed optimal timing of colectomy when appropriate [17, 18].
Risk factors for CRC have been listed above [2, 3, 4••, 5,6,7, 9]. Subtotal colitis or pancolitis confers a high risk, with the extent of colonic involvement based on endoscopic and histological criteria and on whichever reveals more extensive disease [19, 20]. Although patients with proctitis or proctosigmoiditis are not at increased risk per se, many patients will develop more proximal disease over the course of their lifetime and a screening colonoscopy is recommended 8 years after the onset of symptoms even in patients with previously isolated proctitis to confirm extent of disease [4••, 5, 9, 21]. PSC confers a 4-fold increased risk for colonic neoplasia [22]. Thus, patients with IBD and PSC should undergo surveillance colonoscopy annually from the time PSC is diagnosed [2, 4••, 5, 7, 9, 11, 23]. The known risk factors for CRC in IBD are almost all non-modifiable with the possible exception of inflammation [8, 10, 24, 25••]. Colonic strictures in UC (but not in CD), a shortened tubular colon and multiple pseudopolyps also increase CRC risk, with the latter significantly limiting the ability to adequately survey the colon. These clinically important associations may significantly influence dysplasia surveillance and should factor into discussions with patients about their risk of developing CRC and planning surveillance examinations.
In contrast to the well-recognised adenoma-carcinoma sequence for sporadic CRC, colitis-associated CRC stems from a “field change” effect, progressing from non-dysplastic mucosa to either visible or invisible low-grade dysplasia (LGD) and high-grade dysplasia (HGD) to carcinoma [26••]. Biological differences between sporadic CRC and colitis-associated CRC deserve mention here. Chromosomal instability, microsatellite instability and DNA hypermethylation, which are features of sporadic CRC, are also seen in colitis-associated CRC, but curiously, occur before dysplasia or cancer can be detected [27]. Inflammation alone may trigger these changes through the production of reactive oxygen species (ROS), which in turn may cause cellular injury and become oncogenic [27]. Indeed, IBD has been considered an “oxyradical overload” disease [27,28,29]. Notably, the loss of APC function is both less frequent and occurs later in the course of colitis-associated CRC but its frequency has been reported to be as high as 50–100% in lesions with HGD [27, 30]. Conversely, p53 mutations occur early and may be detected in mucosa that is non-dysplastic or indefinite for dysplasia [27]. Aneuploidy (abnormal DNA content) occurs as a consequence of chromosomal instability; its presence strongly correlates with dysplasia, with approximately 20–50% of dysplastic lesions and 50–90% of colitis-associated CRC demonstrating aneuploidy [31, 32]. Activation of proto-oncogenes, k-ras and Src has also been noted in colitis-associated CRC and HGD [30, 33]. Molecular testing for alterations in cellular DNA content (e.g. p53 and APC gene mutations) and aneuploidy, employing stool- or lavage-based diagnostics, has the potential for sampling a greater surface area of the colon and appear promising [34, 35].
Dysplasia—Definitions and Terminology
Biopsies at colonoscopy are graded as “positive” for dysplasia, “negative” for dysplasia or “indefinite” for dysplasia and further classified as LGD, HGD or carcinoma [26••]. The differentiation between LGD and “indefinite for dysplasia” can be difficult and often needs a second opinion from a specialist gastrointestinal pathologist for confirmation [26••, 36].
Previous terminology and older guidelines characterised lesions as sporadic adenomas (found outside an area of inflammation) or as dysplasia-associated lesion or mass (DALM) if detected within an area of colitis [2, 3, 7, 9].
DALMs were categorised as adenoma-like (if raised or with an endoscopic appearance of sporadic adenoma), or non-adenoma-like. Adenoma-like DALMs were considered suitable for endoscopic resection with close follow-up, whereas non-adenoma-like DALMs were an indication for surgery. Patients with HGD or multifocal low-grade dysplasia detected by random biopsy were traditionally offered surgery [2, 3, 7, 9]. Modern optical technology, permitting greater endoscopic identification of dysplasia and acknowledgement that most dysplasia is visible, has led to previous terminology being abandoned and enabled the adoption of new definitions, incorporating the terms “visible” and “invisible” to describe dysplasia within clearly identified lesions or within random biopsy samples respectively, with the addition of terms for ulceration and border of the lesion [5, 11, 26••]. In accordance with the Paris Classification, visible dysplasia is classified as polypoid (pedunculated or sessile) or non-polypoid (superficial elevated, flat or depressed) [26••, 37]. Thus, the term “endoscopically resectable” implies that distinct margins of the lesion can be identified, the lesion is completely excised on visual inspection after endoscopic resection, histological assessment is consistent with complete excision and biopsy specimens taken from mucosa immediately adjacent to the resection margin are free of dysplasia [26••].
Modern Dysplasia Surveillance
The aim of endoscopic surveillance is the reduction of mortality and morbidity of CRC through detection and resection of dysplasia or detecting CRC at an earlier and potentially curable stage [12, 13]. Endoscopic surveillance has been shown to reduce the risk of CRC-related death in IBD patients and to be cost-effective in various case-series, case-control studies and population-based cohort studies and recommended by gastrointestinal societal guidelines [2, 3, 4••, 5, 7, 9, 11, 26••]. Gastrointestinal society recommendations with surveillance intervals after a screening colonoscopy vary but universally agree and recommend annual screening for patients with the highest risk of IBD-associated CRC [2, 3, 4••, 5, 7, 9, 11, 26••]. This implies annual surveillance for patients with concomitant PSC, extensive colitis with active endoscopic or histological inflammation, a family history of CRC in a first-degree relative under the age of 50 and a personal history of dysplasia. European guidelines support a risk stratification approach increasing surveillance intervals to 5 years for patients with low risk [5, 6, 11]. US guidelines do not lengthen screening beyond 3 years currently [2, 4••, 7, 26••].
Successful surveillance hinges on the ability to detect dysplasia. Commitment to a surveillance programme is a significantly involved process that must take a considered approach to patient preference, anatomical factors and available expertise. Pseudopolyps and a shortened tubular colon may pose difficulties with dysplasia detection. Colonic inflammation can make endoscopic and pathologic discrimination of dysplasia difficult, emphasising that surveillance should take ideally place when the patient is in clinical remission though an inordinate delay in surveillance is not recommended regardless of ongoing symptoms. Furthermore, patients do not wish to consider colectomy until there is a relatively high certainty of cancer underscoring the importance of employing the best available technology and technique to detect (and resect) dysplasia, avoiding the development of IBD-associated CRC and need for colectomy [38].
Traditional surveillance employing random colonic biopsies was based on the premise that dysplasia is frequently not visible at endoscopy. The detection of dysplasia with 90% probability required 33 serial colonic biopsies from four quadrant biopsy specimens, taken every 10 cm and from each anatomical segment of the colon, a practice endorsed by many GI societies in earlier guidelines [2, 3, 7]. Modern endoscopic technology and techniques with accumulating evidence that most dysplasia is visible is changing this practice [5, 11, 26••]. Random biopsies would effectively sample less than 1% of total colonic mucosa with one study suggesting that up to 1266 random biopsies would be required for the detection of one additional episode of dysplasia [12]. A recent randomised control trial comparing random vs. targeted biopsy reported that both techniques detected a similar rate of neoplasia, but a larger number of biopsies and longer procedure time for random biopsies made targeted biopsies more cost-effective [39]. In a study of colonoscopic surveillance every 2 years, interval cancers were seen between 10 and 28 months after a dysplasia-free examination, reflecting poorly on the practice of random biopsies alone for dysplasia detection [40].
Modern imaging techniques including chromoendoscopy (CE), narrow-band imaging (NBI) and confocal endomicroscopy are adjunctive techniques to detect subtle mucosal abnormalities and are discussed below.
Chromoendoscopy has demonstrated a superior diagnostic yield and therapeutic advantage when compared with standard random biopsy and white-light technique for index screening of dysplasia in several studies [41,42,43] and is supported by meta-analysis demonstrating that CE with targeted biopsies is 8.9 times more likely to detect any dysplasia and 5.2 times more likely to detect non-polypoid dysplasia than white-light endoscopy (WLE) with random biopsy [44]. Another meta-analysis demonstrated a significantly greater proportion of dysplasia detection at CE (RR 1.8, absolute risk increase 6%) than WLE alone [26••]. The growing body of evidence supporting CE with targeted biopsy has emboldened gastrointestinal society recommendations in recent years. American Gastroenterological Association (AGA) guidelines recognise and support CE with targeted biopsies as a reasonable alternative to WLE in experienced hands [2], as do European [5, 11] and recent American Society for Gastrointestinal Endoscopy (ASGE) guidelines [4••] all endorsing CE. A landmark publication (International Consensus Statement on Surveillance and Management of Dysplasia in Inflammatory Bowel Disease (SCENIC)) recommends CE over standard WLE and recommends CE over high-definition (HD) colonoscopy for dysplasia surveillance [26••]. CE was also demonstrated to be cost-effective [45, 46••].
Chromoendoscopy Technique
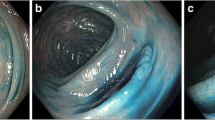
CE involves the use of topical contrast agents, 0.1% methylene blue or 0.03–0.5% indigo carmine. Optimal bowel preparation is vital. Excellent resources are available for colonoscopists to consolidate and enhance skills with CE and lesion recognition [26••, 47••].
The colonic mucosa is sprayed segmentally with contrast agent after caecal intubation and upon withdrawal, using a spray catheter or through the forward water-jet channel using an automated pump [48, 49]. The dye enhances mucosal irregularities and delineates lesion morphology, size and borders to evaluate for endoscopic features of submucosal invasion [47••]. Endoscopically resectable lesions may be resected or tattooed and referred to an endoscopist with expertise in endoscopic mucosal resection or dissection as appropriate. Targeted biopsies should be taken from lesions deemed endoscopically unresectable and lesions of uncertain significance. At least two biopsies from several colonic segments are recommended to determine histological extent and severity of disease, which in turn affects the risk of dysplasia. Although random biopsies are not recommended in current guidelines [4••, 5, 6, 11], a recent study from GETAID has demonstrated the value of random biopsies in conjunction with CE in IBD patients at high risk of colitis-associated CRC [50]. In this prospective study of 1000 colonoscopies in 1000 patients, neoplasia was detected from targeted biopsies or in resected lesions in 82 patients. Dysplasia was detected in 7 patients additionally by random biopsies and in another 12 patients by random biopsies alone and was associated with a personal history of neoplasia, a shortened tubular colon and PSC [50]. These findings challenge the notion that random biopsies have no place when CE is performed with HD WLE and add credence to two retrospective studies supporting additional random biopsies in high-risk patients [51, 52]. Navaneethan and colleagues, in their retrospective study of 71 patients with PSC-UC undergoing a total of 267 colonoscopies, noted a significantly increased yield of neoplasia even in the absence of endoscopic features of prior inflammation [51]. Van den Broek and colleagues, in a retrospective study of 466 colonoscopies in 167 UC patients, also recommended random biopsies in the presence of PSC, a shortened colon and previous or visible neoplasia, although they did not note an impact of random biopsies in other patients [52].
It should be noted that in three prospective studies employing pan-colonic CE (not in a targeted fashion), and then obtaining targeted biopsies along with random biopsies, despite the low yield of random biopsies (0.1–0.4%), the additional percentage of patients diagnosed by random biopsies was notable (8.3–30.8%) [41, 42, 53]. Indeed, the SCENIC panellists did not reach a consensus on the utility of random biopsies when using CE [26••]. It seems appropriate to obtain random biopsies in addition to CE and targeted biopsy at least in patients with PSC and other risk factors for colitis-associated CRC.
Chromoendoscopy for Dysplasia Surveillance: Evidence and Controversy
Heightened sensitivity of CE in detecting dysplastic foci notwithstanding, there has been scepticism and debate about its universal adoption [26••, 54]. The SCENIC consensus recommendation for CE over HD WLE is conditional, based on two randomised controlled trials and several small observational studies [26••, 41, 55]. American and European guidelines have also based their recommendation supporting CE over HD WLE, citing this data and two meta-analyses, criticised for incomplete benefit/harm assessment [44, 54, 56]. The natural history of additional, smaller, flatter lesions identified at CE is currently not well understood [57]. Furthermore, progression from indefinite and low-grade dysplasia to cancer appears to be low in some high-risk cohorts even considering variables such as primary sclerosing cholangitis and previous advanced dysplasia [51, 58,59,60]. That said, data from the Surveillance, Epidemiology and End Results Medicare-linked database of patients over 67 years demonstrated that interval cancers 6 to 36 months after colonoscopy occurred in a much higher proportion of patients with IBD (15.1% with CD and 15.8% with UC) than patients without IBD (5.8%) highlighting that clinically relevant areas of neoplasia may be missed with “current” colonoscopy surveillance [40].
A growing body of evidence, since the SCENIC consensus in 2015, has added to our knowledge, supporting CE as the preferred technique despite others expressing reservations regarding its universal adoption [17, 61,62,63,64,65,66].
In a follow-up evaluation of their 2008 study of patients in an IBD surveillance programme, Marion and colleagues reported on 68 patients (from the original cohort of 115), with median disease duration of 21 years followed over a 5-year period [61, 67]. Patients underwent colonoscopic surveillance with random biopsy specimens, targeted WLE and dye-spray CE. After a mean of 3 surveillance colonoscopies per patient, 6 dysplastic lesions were detected by random biopsy technique, compared to 11 and 27 dysplastic lesions seen at WLE and CE, respectively [61]. CE was superior to random biopsy (OR 5.4; 95% CI, 2.9–9.9) and targeted WLE (OR 2.4; 95% CI, 1.4–4.0). A negative result from CE assessment was the best indicator for a dysplasia-free outcome and a positive result was associated with earlier referral for colectomy (HR 12.1; 95% CI, 3.2–46.2). Of 10 patients with dysplasia referred for colectomy, no carcinomas were found [61].
Gasia and colleagues reported on a cohort of 454 IBD patients undergoing surveillance assessments between 2011 and 2014 [62]. Patients underwent WLE, HD colonoscopy, virtual electronic or dye-spray CE. Just 30% patients underwent WLE or HD colonoscopy with random biopsy and 14% had virtual CE with random biopsy. Fewer patients underwent dye-spray CE with random (n = 4) or targeted (n = 24) biopsies. More neoplastic lesions were identified by targeted biopsies than random biopsies (19 vs. 8%). Four dysplastic lesions were seen at HD WLE. There was no difference in yield between dye CE, virtual CE and targeted WLE. No dysplasia was identified however, from random biopsy samples alone [62].
Mooiweer et al. studied outcomes from adoption of CE from 440 colonoscopies in 401 patients compared with historical outcomes of 1802 colonoscopies in 772 patients with WLE [65]. There was no difference in dysplasia detection in both groups (11 vs. 10%). A limitation of this study was the lack of data for examination factors (including bowel prep and withdrawal time), but the remarkably stable neoplasia detection over a decade in experienced hands led the investigators to suggest that CE is not superior to WLE [65].
Choi and colleagues reporting a 40-year experience with colonoscopic surveillance from St Mark’s Hospital, London, noted an increase in the incidence rate of dysplasia since the adoption of HD WLE and CE for surveillance but no decrease in the rate of colon cancer [17]. A significant increase in the proportion of early-stage (Duke’s A and B) vs. late-stage (Duke’s C and D) CRC was noted in the most recent decade. CE did not affect the outcome of CRC in IBD [17]. It is worth noting that HD WLE and CE were introduced at St Mark’s in 2006 and although patients were not randomised to CE between 2006 and 2012, the CRC incidence rate was 2.2/1000 patient-years in patients receiving at least one CE vs. 4.6 in those who had never received CE (p = 0.02) [17]. Adding to our understanding, the investigators identified four characteristics that were significantly associated with a later diagnosis of HGD or CRC. Non-polypoid lesion appearance, defined as Paris type 0-II (visible, slightly elevated or depressed), type 0-III (excavated), or plaque-like, was the strongest risk factor (HR 8.6; 95% CI 3–24.8), though macroscopically invisible dysplasia (HR, 4.1; 95% CI, 1.3–13.4), lesion size ≥ 1 cm (HR, 3.8; 95% CI, 1.5–13.4) and previous history of indefinite dysplasia (HR, 2.8; 95% CI, 1.2–6.5) also proved significant predictors. A strong positive correlation was noted between the number of these risk factors and a subsequent diagnosis of HGD or CRC. The strongest risk factor, non-polypoid dysplasia, was found at significantly greater frequency in those patients who underwent CE rather than WLE (15.8 vs. 7.8%, respectively), although exposure to CE did not lower the risk of HGD or CRC [17].
In a study from the Mayo Clinic, Deepak et al. reported an incremental diagnostic yield from CE [63]. IBD patients with colorectal dysplasia on WLE, endoscopic and histologic findings (median disease duration 18 years) were compared among the index WLE, first and subsequent CE [63]. Dysplasia was identified in 55 patients of 95 index cases at WLE. The first CE identified dysplastic lesions in 50 patients (34 new lesions not seen at index WLE), endoscopic resection was performed for 43 lesions and 14 patients underwent surgery with 2 cases of CRC and 3 cases of HGD. In subsequent CE assessments, 34 lesions were identified in 20 patients. The data support CE as a surveillance procedure in high-risk patients [63]. In addition to supporting CE as a preferred surveillance technique, these findings add credence to the practice of referring patients with endoscopically invisible dysplasia to an experienced endoscopist employing CE. Moreover, the relatively higher proportion of endoscopically visible dysplasia missed at HD WLE without CE arguably suggests that HD WLE without CE may be insufficient [68]. A prospective randomised trial reported recently also demonstrated a significantly higher dysplasia detection using CE with HD WLE over HD WLE alone at 26 lesions vs. 12 per patient, respectively [68].
A recent systematic review of 10 randomised trials (1500 participants) demonstrated a higher likelihood of detecting patients with dysplasia using CE over other techniques (RR, 1.37; 95% CI, 1.04–1.79) [46••]. On subgroup analyses, this effect was confirmed only if CE was compared with SD WLE (RR, 2.12; 95% CI, 1.15–3.91). CE needed a significantly longer procedural time compared with other techniques (mean difference, 8.91 min; 95% CI, 1.37–16.45) [46••].
A multi-centre prospective study of 350 patients has provided “real-world” experience supporting of CE for IBD surveillance and challenging scepticism about the effectiveness of CE outside of a clinical trial setting and potential limitations posed by less experience [69]. Patients were systematically evaluated using WLE (SD in 41.5% and HD in 58.5%) for each colonic segment, followed by CE with 0.4% indigocarmine. A 57.4% incremental yield was noted with CE, comparable between SD and HD colonoscopy (51.5 vs. 52.3%; p = 0.30). Another interesting observation was comparable dysplasia detection between expert and non-expert colonoscopists (18.5 vs. 13.1%; p = 0.20) with no significant learning curve. Endoscopic findings predictive of dysplasia were proximal colonic lesions, protruding morphology, loss of innominate lines and a neoplastic Kudo pit pattern. The potential for a “Hawthorne effect” (diligence with performance of colonoscopy in a prospective study) and an incremental yield from a “second look” must be acknowledged, but this study does provide proof of principle for the wider and realistic adoption of CE for dysplasia surveillance in high-risk IBD patients [69].
Successful delivery of dysplasia surveillance using CE, however, hinges on many variables including appropriate training and expertise (endoscopist and team), lesion recognition, inter-observer variability among pathologists identifying and grading dysplasia and operational barriers including availability of dye and equipment and procedural time resulting in some reservation in adopting CE and referral to “experts” at the outset [26••]. Addressing the “learning curve”, the ESGE suggests 30 CE procedures performed with an expert [36], while an American study suggests that the completion of 16 CE procedures may be adequate for dysplasia detection [70].
The potential for methylene blue dye-related DNA damage with WLE [71] has been a concern but this was not demonstrated recently with the use of oral methylene blue MMX tablets [72].
Evolution in our knowledge of the natural history of dysplasia and the real implications of dysplasia found by CE through its wider adoption may unveil its real place in surveillance. Until then, evidence favours CE with targeted biopsy in individuals at high risk or with previous dysplasia. In the remaining majority of patients, careful assessment with either HD WLE and random biopsies or CE with dye spray may be appropriate with no compelling mandate for one over the other presently [26••]. A summary of recommendations from the SCENIC consensus for the surveillance and management of dysplasia in patients with IBD is outlined in Table 1.
Management of Dysplasia
Accurate identification of dysplasia and determination of its resectability is key to further management [26••]. Modern methods such as CE have greatly enhanced dysplasia detection. Lesions should be identified as being within or outside an area of known colitis. Lesions in segments outside an area of known colitis should be treated as sporadic adenomas with standard post-polypectomy surveillance recommendations [2, 11, 73].
Visible Dysplasia
Lesions in an area of known colitis should be assessed for endoscopic resectability and completely resected, if possible, by an experienced endoscopist regardless of underlying colitis or grade of dysplasia. Resection may be technically more difficult with inflammation, friability and scarring when tattooing and photo documentation may aid subsequent surveillance or resection [4••, 11, 26••]. Mucosa adjacent to the raised lesion should also be biopsied to evaluate for dysplasia. If completely resected with dysplasia-free margins and no invisible dysplasia elsewhere in the colon, surveillance colonoscopy may be recommended [11, 26••]. ECCO recommends surveillance with CE at 3 months and then annually while US Multi-Society guidelines recommend a 3–6-month check for larger sessile lesions excised piecemeal or via EMR/ESD with longer surveillance intervals if the initial repeat colonoscopy result is negative [11, 73]. Follow-up studies of endoscopically resectable polypoid lesions are reassuring demonstrating a low risk of developing dysplasia or carcinoma, supported by a recent meta-analysis [74,75,76,77,78].
A recent retrospective study from three Dutch tertiary IBD centres has challenged the practice of taking additional biopsies from mucosa surrounding visible resected lesions [79]. In their cohort of 196 patients (of 1065 patients undergoing colonoscopic surveillance) with at least 1 visible dysplastic lesion, biopsies of surrounding mucosa were taken in 71 patients. The dysplasia yield was 7 per 140 lesions (5%) and this decreased to 5 per 136 lesions (3.7%) when only lesions with LGD were analysed [79]. Two patients had HGD with surrounding dysplasia and were treated surgically whereas in patients with LGD and surrounding dysplasia, intensive surveillance was employed and at median 37 months follow-up; no further progression was noted. The authors concluded that the practice of routine biopsies from areas surrounding dysplastic sites is of doubtful value.
In challenging our prevailing notions, the authors question the validity of such practice and our paradigms with field dysplasia. There is currently no consensus on the number of biopsies or an optimal distance from the margin of the resection where the biopsy may be taken. Plausibly, limited visibility of lesion borders may impact on residual dysplastic tissue after resection with consequent management difficulties. However, biopsies from surrounding mucosa would assist the endoscopist in detecting residual dysplasia and indeed histological assessment as is considered standard practice currently [2, 5, 7, 26••]. The use of HD equipment complemented by advanced imaging techniques (such as CE) should assist more accurate characterisation of lesions and their margins, thereby reducing the need for random biopsies from the surrounding mucosa. Larger and prospective studies are needed to build the body of evidence needed to change the practice of taking biopsies from around resected dysplastic lesions at the present time.
The management of non-polypoid dysplastic lesions is still contentious [80, 81].
The SCENIC consensus makes a conditional recommendation for surveillance colonoscopy after complete removal of endoscopically resectable non-polypoid dysplastic lesions, recognising the higher CRC risk and greater endoscopic difficulty with resectability [26••].
Invisible Dysplasia
SCENIC defines invisible dysplasia as dysplasia identified on random (non-targeted) biopsies of colon mucosa without a visible lesion [26••]. Although previous data report progression of LGD at random biopsies between 20 and 23% [17, 82, 83], this has been challenged in recent studies which report a 3 and 10% subsequent rate of progression to CRC over 10 years [84,85,86]. Modern techniques and training identifying more visible dysplasia have likely affected this. AGA and the British Society of Gastroenterology (BSG) recommend colectomy for multifocal flat LGD, though BSG supports CE if there is uncertainty with the diagnosis and regular surveillance for patients who decline colectomy [2, 6]. The SCENIC consensus supports dysplasia confirmation by a second GI pathologist and referral to an endoscopist with expertise in CE and HD WLE to inform subsequent decisions regarding surveillance vs. colectomy [26••]. When visible dysplasia is identified in the same area as invisible dysplasia and the lesion is resectable, patients may remain in a surveillance programme [26••]. If dysplasia is not found, individualised discussions involving surveillance vs. colectomy are suggested [26••]. When high-grade dysplasia is confirmed by a second specialist pathologist, or incompletely resected raised dysplasia is discovered, colectomy is recommended [2, 9, 26••]. Several studies have shown the prevalence of synchronous CRC in patients with flat HGD between 42 and 45% [17, 87]. Of those who deferred colectomy and continued surveillance, 25% developed CRC [26••]. Flat non-targeted HGD and endoscopically unresectable lesions or a lesion with dysplasia in the adjacent mucosa are indications for colectomy [2, 4••, 11, 26••, 49].
It is difficult to distinguish regeneration and repair from dysplasia in the presence of chronic active inflammation, resulting in a pathological finding that is “indefinite for dysplasia”. In one study, a 9% 5-year progression rate to HGD or CRC was observed [82]. Surveillance should ideally take place after “optimal treatment” of underlying inflammation followed by endoscopic re-evaluation probably with CE when the patient is in clinical remission [26••]. As progression to CRC in patients with dysplasia is higher than those without dysplasia, a further surveillance examination is advisable within 3–6 months [2].
A summary of the ASGE algorithm for the management of lesions detected at surveillance colonoscopy is shown in Fig. 1.
Evolving Imaging Modalities
Narrow-band imaging (NBI) is an optical CE technology using filters to enhance the contrast of the mucosa and vasculature. It has not demonstrated an increased yield for dysplasia detection in randomised studies compared to WLE or HD WLE [88,89,90,91]. A multicentre study comparing WLE with targeted and random biopsies to NBI found no difference in dysplasia detection rates [92]. SCENIC does not recommend NBI on the basis of current evidence [26••].
Confocal laser endomicroscopy (CLE) enables “real-time” histology of lesions, detected at colonoscopy, using intravenous administration of stains such as fluorescein. Following topical or intravenous application of a fluorescence agent, the CLE probe is applied to the mucosal surface, which highlights the extracellular matrix allowing for in vivo evaluation [93]. In a study comparing combined CE and CLE or conventional WLE, a 4.75-fold increase in neoplasia detection was seen with the combined approach (p = 0.005) requiring 50% fewer biopsies (p = 0.008) compared with conventional WLE [55]. An increased diagnostic yield with the need for fewer biopsies has been confirmed by other studies [94,95,96]. Limitations of this technique are increased length of time (approximately15–25 min more than WLE with target biopsy and CE with targeted biopsy, respectively), cost (US$175,000 for probe-based system) and a steep learning curve [94, 97,98,99].
Endocytoscopy is a novel technique that uses probe-based systems or EC-fitted endoscopes to obtain histology-equivalent images of the mucosa, following pretreatment with mucolytic agents and staining with dyes such as methylene blue and crystal violet [100]. It has not been tested in dysplasia surveillance to date [93].
Stool DNA testing for genetic alterations (part of the carcinogenesis cascade in IBD, e.g. BMP3 and mNDRG4) is being studied [101] and, in a recent study using a Markov model to simulate the clinical course of UC analysis of sDNA with CE for patients with positive results, was noted to be more cost-effective than CE or WLE alone [34]. Further studies in this area are needed.
Conclusions
Of all the known risk factors associated with the development of CRC in IBD, colitis-related dysplasia confers the greatest risk. Recognition that most dysplasia is visible at colonoscopy and advances in optical technology, allowing greater endoscopic identification of dysplasia, have emboldened our approach to surveillance and management of dysplasia, with the bulk of evidence favouring CE or HD WLE, at the very least for dysplasia detection. Scepticism, around available data, operational barriers and the need to understand the true impact of higher dysplasia detection on overall CRC mortality notwithstanding, a growing body of evidence, now backed by international consensus opinion, favours CE as a surveillance technique where expertise is available. Future studies should address current gaps in knowledge, in particular, practicalities around procedural cost, competency training and the true and long-term impact of dysplasia detection with modern techniques relating to IBD-CRC detection and survival. Meanwhile, implementation of a risk stratification protocol that includes CE is effective, enabling earlier detection of dysplasia and CRC, determination of surveillance intervals and decreasing morbidity from CRC. Meanwhile, the development of newer optical techniques and non-invasive methods for dysplasia detection has exciting implications for further research. Dysplasia detection in UC is a science in evolution, but with promising potential to impact positively on dysplasia-associated CRC risk for our patients.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Beaugerie L, Itzkowitz SH. Cancers complicating inflammatory bowel disease. N Engl J Med. 2015;373(195). https://doi.org/10.1056/NEJMc1505689.
Farraye FA, Odze RD, Eaden J, et al. AGA technical review on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology. 2010;138:746–74. 774 e1–4; quiz e12–3
Itzkowitz SH, Present DH, Crohn's, et al. Consensus conference: colorectal cancer screening and surveillance in inflammatory bowel disease. Inflamm Bowel Dis. 2005;11(3):314–21. https://doi.org/10.1097/01.MIB.0000160811.76729.d5.
•• American Society for Gastrointestinal Endoscopy Standards of Practice C, Shergill AK, Lightdale JR, et al. The role of endoscopy in inflammatory bowel disease. Gastrointest Endosc. 2015;81:1101–21 e1–13. A comprehensive evidence based update from the ASGE with useful algorithms for managing dysplasia in IBD patients
Magro F, Gionchetti P, Eliakim R, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. 2017;11(6):649–70.
Mowat C, Cole A, Windsor A, et al. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2011;60:571–607.
Kornbluth A, Sachar DB, Practice Parameters Committee of the American College of G. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010;105(3):501–23; quiz 524. https://doi.org/10.1038/ajg.2009.727.
Rutter M, Saunders B, Wilkinson K, et al. Severity of inflammation is a risk factor for colorectal neoplasia in ulcerative colitis. Gastroenterology. 2004;126:451–9.
Cairns SR, Scholefield JH, Steele RJ, et al. Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002). Gut. 2010;59(5):666–89. https://doi.org/10.1136/gut.2009.179804.
Colman RJ, Rubin DT. Histological inflammation increases the risk of colorectal neoplasia in ulcerative colitis: a systematic review. Intest Res. 2016;14(3):202–10. https://doi.org/10.5217/ir.2016.14.3.202.
Annese V, Daperno M, Rutter MD, et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis. 2013;7:982–1018.
Rutter MD, Riddell RH. Colorectal dysplasia in inflammatory bowel disease: a clinicopathologic perspective. Clin Gastroenterol Hepatol. 2014;12(3):359–67. https://doi.org/10.1016/j.cgh.2013.05.033.
Rutter MD, Saunders BP, Wilkinson KH, Kamm MA, Williams CB, Forbes A. Most dysplasia in ulcerative colitis is visible at colonoscopy. Gastrointest Endosc. 2004;60(3):334–9. https://doi.org/10.1016/S0016-5107(04)01710-9.
Rubin DT, Rothe JA, Hetzel JT, Cohen RD, Hanauer SB. Are dysplasia and colorectal cancer endoscopically visible in patients with ulcerative colitis? Gastrointest Endosc. 2007;65(7):998–1004. https://doi.org/10.1016/j.gie.2006.09.025.
Munkholm P. Review article: the incidence and prevalence of colorectal cancer in inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18(Suppl 2):1–5. https://doi.org/10.1046/j.1365-2036.18.s2.2.x.
Eaden JA, Abrams KR, Mayberry JF. The risk of colorectal cancer in ulcerative colitis: a meta-analysis. Gut. 2001;48(4):526–35. https://doi.org/10.1136/gut.48.4.526.
Choi CH, Rutter MD, Askari A, et al. Forty-year analysis of colonoscopic surveillance program for neoplasia in ulcerative colitis: an updated overview. Am J Gastroenterol. 2015;110(7):1022–34. https://doi.org/10.1038/ajg.2015.65.
Jess T, Simonsen J, Jorgensen KT, et al. Decreasing risk of colorectal cancer in patients with inflammatory bowel disease over 30 years. Gastroenterology. 2012;143:375–81. e1; quiz e13–4
Ekbom A, Helmick C, Zack M, et al. Ulcerative colitis and colorectal cancer. A population-based study. N Engl J Med. 1990;323:1228–33.
Floren CH, Benoni C, Willen R. Histologic and colonoscopic assessment of disease extension in ulcerative colitis. Scand J Gastroenterol. 1987;22(4):459–62. https://doi.org/10.3109/00365528708991491.
Meucci G, Vecchi M, Astegiano M, et al. The natural history of ulcerative proctitis: a multicenter, retrospective study. Gruppo di Studio per le Malattie Infiammatorie Intestinali (GSMII). Am J Gastroenterol. 2000;95:469–73.
Soetikno RM, Lin OS, Heidenreich PA, Young HS, Blackstone MO. Increased risk of colorectal neoplasia in patients with primary sclerosing cholangitis and ulcerative colitis: a meta-analysis. Gastrointest Endosc. 2002;56(1):48–54. https://doi.org/10.1067/mge.2002.125367.
Saxena AP, Limdi JK, Farraye FA. Zeroing in on endoscopic and histologic mucosal healing to reduce the risk of colorectal neoplasia in inflammatory bowel disease. Gastrointest Endosc. 2017;86(6):1012–4. https://doi.org/10.1016/j.gie.2017.08.029.
Rubin DT, Huo D, Kinnucan JA, et al. Inflammation is an independent risk factor for colonic neoplasia in patients with ulcerative colitis: a case-control study. Clin Gastroenterol Hepatol. 2013;11:1601–8 e1–4.
•• Flores BM, O'Connor A, Moss AC. Impact of mucosal inflammation on risk of colorectal neoplasia in patients with ulcerative colitis: a systematic review and meta-analysis. Gastrointest Endosc 2017. A recent meta-analysis assessing the impact of histological inflammation on colorectal cancer risk in IBD raising further debate on whether mucosal healing alone is sufficient to reduce colitis-associated colorectal cancer risk.
•• Laine L, Kaltenbach T, Barkun A, et al. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology. 2015;148:639–651 e28. An international consensus with practice-changing implications to dysplasia surveillance and endorsed by most GI societies.
Rogler G. Chronic ulcerative colitis and colorectal cancer. Cancer Lett. 2014;345(2):235–41. https://doi.org/10.1016/j.canlet.2013.07.032.
Chiba T, Marusawa H, Ushijima T. Inflammation-associated cancer development in digestive organs: mechanisms and roles for genetic and epigenetic modulation. Gastroenterology. 2012;143(3):550–63. https://doi.org/10.1053/j.gastro.2012.07.009.
Hussain SP, Hofseth LJ, Harris CC. Radical causes of cancer. Nat Rev Cancer. 2003;3(4):276–85. https://doi.org/10.1038/nrc1046.
Redston MS, Papadopoulos N, Caldas C, et al. Common occurrence of APC and K-ras gene mutations in the spectrum of colitis-associated neoplasias. Gastroenterology. 1995;108:383–92.
Rubin CE, Haggitt RC, Burmer GC, Brentnall TA, Stevens AC, Levine DS, et al. DNA aneuploidy in colonic biopsies predicts future development of dysplasia in ulcerative colitis. Gastroenterology. 1992;103(5):1611–20. https://doi.org/10.1016/0016-5085(92)91185-7.
Burmer GC, Rabinovitch PS, Haggitt RC, Crispin d, Brentnall TA, Kolli VR, et al. Neoplastic progression in ulcerative colitis: histology, DNA content, and loss of a p53 allele. Gastroenterology. 1992;103(5):1602–10. https://doi.org/10.1016/0016-5085(92)91184-6.
Cartwright CA, Coad CA, Egbert BM. Elevated c-Src tyrosine kinase activity in premalignant epithelia of ulcerative colitis. J Clin Invest. 1994;93(2):509–15. https://doi.org/10.1172/JCI117000.
Kisiel JB, Konijeti GG, Piscitello AJ, Chandra T, Goss TF, Ahlquist d, et al. Stool DNA analysis is cost effective for colorectal cancer surveillance in patients with ulcerative colitis. Clin Gastroenterol Hepatol. 2016;14(12):1778–87. https://doi.org/10.1016/j.cgh.2016.07.018.
Kanthan R, Senger JL, Kanthan SC. Fecal molecular markers for colorectal cancer screening. Gastroenterol Res Pract. 2012;2012:184343.
Kaminski MF, Hassan C, Bisschops R, et al. Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2014;46(5):435–49. https://doi.org/10.1055/s-0034-1365348.
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc 2003;58:S3–43, 6, DOI: https://doi.org/10.1016/S0016-5107(03)02159-X.
Siegel CA, Schwartz LM, Woloshin S, Cole EB, Rubin DT, Vay T, et al. When should ulcerative colitis patients undergo colectomy for dysplasia? Mismatch between patient preferences and physician recommendations. Inflamm Bowel Dis. 2010;16(10):1658–62. https://doi.org/10.1002/ibd.21233.
Watanabe T, Ajioka Y, Mitsuyama K, et al. Comparison of targeted vs random biopsies for surveillance of ulcerative colitis-associated colorectal cancer. Gastroenterology. 2016;151:1122–30.
Wang YR, Cangemi JR, Loftus EV Jr, Picco MF. Rate of early/missed colorectal cancers after colonoscopy in older patients with or without inflammatory bowel disease in the United States. Am J Gastroenterol. 2013;108(3):444–9. https://doi.org/10.1038/ajg.2012.429.
Kiesslich R, Fritsch J, Holtmann M, et al. Methylene blue-aided chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2003;124:880–8.
Matsumoto T, Nakamura S, Jo Y, Yao T, Iida M. Chromoscopy might improve diagnostic accuracy in cancer surveillance for ulcerative colitis. Am J Gastroenterol. 2003;98(8):1827–33. https://doi.org/10.1111/j.1572-0241.2003.07580.x.
Hurlstone DP, McAlindon ME, Sanders DS, Keogh R, Lobo AJ, Cross SS. Further validation of high-magnification chromoscopic-colonoscopy for the detection of intraepithelial neoplasia and colon cancer in ulcerative colitis. Gastroenterology. 2004;126(1):376–8. https://doi.org/10.1053/j.gastro.2003.05.021.
Subramanian V, Mannath J, Ragunath K, et al. Meta-analysis: the diagnostic yield of chromoendoscopy for detecting dysplasia in patients with colonic inflammatory bowel disease. Aliment Pharmacol Ther. 2011;33:304–12.
Konijeti GG, Shrime MG, Ananthakrishnan AN, Chan AT. Cost-effectiveness analysis of chromoendoscopy for colorectal cancer surveillance in patients with ulcerative colitis. Gastrointest Endosc. 2014;79(3):455–65. https://doi.org/10.1016/j.gie.2013.10.026.
•• Iannone A, Ruospo M, Wong G, et al. Chromoendoscopy for surveillance in ulcerative colitis and Crohn’s disease: a systematic review of randomized trials. Clin Gastroenterol Hepatol 2017;(11):1684-1697. An important meta-analysis summarising the evidence for chromoendoscopy for dysplasia surveillance in IBD.
•• Soetikno R, Sanduleanu S, Kaltenbach T. An atlas of the nonpolypoid colorectal neoplasms in inflammatory bowel disease. Gastrointest Endosc Clin N Am. 2014;24(3):483–520. An essential resource for endoscopists for lesion recognition and chromoendoscopy. https://doi.org/10.1016/j.giec.2014.04.003.
Rutter MD, Saunders BP, Schofield G, Forbes A, Price AB, Talbot IC. Pancolonic indigo carmine dye spraying for the detection of dysplasia in ulcerative colitis. Gut. 2004;53(2):256–60. https://doi.org/10.1136/gut.2003.016386.
Soetikno R, Subramanian V, Kaltenbach T, et al. The detection of nonpolypoid (flat and depressed) colorectal neoplasms in patients with inflammatory bowel disease. Gastroenterology. 2013;144:1349–52. 1352 e1–6
Moussata D, Allez M, Cazals-Hatem D, et al. Are random biopsies still useful for the detection of neoplasia in patients with IBD undergoing surveillance colonoscopy with chromoendoscopy? Gut 2017.
Navaneethan U, Jegadeesan R, Gutierrez NG, et al. Progression of low-grade dysplasia to advanced neoplasia based on the location and morphology of dysplasia in ulcerative colitis patients with extensive colitis under colonoscopic surveillance. J Crohns Colitis. 2013;7:e684–91.
van den Broek FJ, Stokkers PC, Reitsma JB, et al. Random biopsies taken during colonoscopic surveillance of patients with longstanding ulcerative colitis: low yield and absence of clinical consequences. Am J Gastroenterol. 2014;109(5):715–22. https://doi.org/10.1038/ajg.2011.93.
Hurlstone DP, Sanders DS, Atkinson R, Hunter MD, McAlindon ME, Lobo AJ, et al. Endoscopic mucosal resection for flat neoplasia in chronic ulcerative colitis: can we change the endoscopic management paradigm? Gut. 2007;56(6):838–46. https://doi.org/10.1136/gut.2006.106294.
Higgins PD. Miles to go on the SCENIC route: should chromoendoscopy become the standard of care in IBD surveillance? Am J Gastroenterol. 2015;110:1035–7.
Kiesslich R, Goetz M, Lammersdorf K, et al. Chromoscopy-guided endomicroscopy increases the diagnostic yield of intraepithelial neoplasia in ulcerative colitis. Gastroenterology. 2007;132:874–82.
Wu L, Li P, Wu J, Cao Y, Gao F. The diagnostic accuracy of chromoendoscopy for dysplasia in ulcerative colitis: meta-analysis of six randomized controlled trials. Color Dis. 2012;14(4):416–20. https://doi.org/10.1111/j.1463-1318.2010.02505.x.
Marion JF, Sands BE. The SCENIC consensus statement on surveillance and management of dysplasia in inflammatory bowel disease: praise and words of caution. Gastroenterology. 2015;148(3):462–7. https://doi.org/10.1053/j.gastro.2015.01.029.
Goldstone R, Itzkowitz S, Harpaz N, et al. Progression of low-grade dysplasia in ulcerative colitis: effect of colonic location. Gastrointest Endosc. 2011;74:1087–93.
Venkatesh PG, Jegadeesan R, Gutierrez NG, et al. Natural history of low grade dysplasia in patients with primary sclerosing cholangitis and ulcerative colitis. J Crohns Colitis. 2013;7:968–73.
Pekow JR, Hetzel JT, Rothe JA, Hanauer SB, Turner JR, Hart J, et al. Outcome after surveillance of low-grade and indefinite dysplasia in patients with ulcerative colitis. Inflamm Bowel Dis. 2010;16(8):1352–6. https://doi.org/10.1002/ibd.21184.
Marion JF, Waye JD, Israel Y, Present DH, Suprun M, Bodian C, et al. Chromoendoscopy is more effective than standard colonoscopy in detecting dysplasia during long-term surveillance of patients with colitis. Clin Gastroenterol Hepatol. 2016;14(5):713–9. https://doi.org/10.1016/j.cgh.2015.11.011.
Gasia MF, Ghosh S, Panaccione R, Ferraz JG, Kaplan GG, Leung Y, et al. Targeted biopsies identify larger proportions of patients with colonic neoplasia undergoing high-definition colonoscopy, dye chromoendoscopy, or electronic virtual chromoendoscopy. Clin Gastroenterol Hepatol. 2016;14(5):704–12 e4. https://doi.org/10.1016/j.cgh.2015.12.047.
Deepak P, Hanson GJ, Fletcher JG, Tremaine WJ, Pardi DS, Kisiel JB, et al. Incremental diagnostic yield of chromoendoscopy and outcomes in inflammatory bowel disease patients with a history of colorectal dysplasia on white-light endoscopy. Gastrointest Endosc. 2016;83(5):1005–12. https://doi.org/10.1016/j.gie.2015.09.021.
Krugliak Cleveland N, Colman RJ, Rodriquez D, Hirsch A, Cohen RD, Hanauer SB, et al. Surveillance of IBD using high definition colonoscopes does not miss adenocarcinoma in patients with low-grade dysplasia. Inflamm Bowel Dis. 2016;22(3):631–7. https://doi.org/10.1097/MIB.0000000000000634.
Mooiweer E, van der Meulen-de Jong AE, Ponsioen CY, et al. Chromoendoscopy for surveillance in inflammatory bowel disease does not increase neoplasia detection compared with conventional colonoscopy with random biopsies: results from a large retrospective study. Am J Gastroenterol. 2015;110(7):1014–21. https://doi.org/10.1038/ajg.2015.63.
Fumery M, Dulai PS, Gupta S, Prokop LJ, Ramamoorthy S, Sandborn WJ, et al. Incidence, risk factors, and outcomes of colorectal cancer in patients with ulcerative colitis with low-grade dysplasia: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2017;15(5):665–74 e5. https://doi.org/10.1016/j.cgh.2016.11.025.
Marion JF, Waye JD, Present DH, Israel Y, Bodian C, Harpaz N, et al. Chromoendoscopy-targeted biopsies are superior to standard colonoscopic surveillance for detecting dysplasia in inflammatory bowel disease patients: a prospective endoscopic trial. Am J Gastroenterol. 2008;103(9):2342–9. https://doi.org/10.1111/j.1572-0241.2008.01934.x.
Kaltenbach T, McQuaid KR, Soetikno R, Laine L. Improving detection of colorectal dysplasia in inflammatory bowel disease surveillance. Gastrointest Endosc. 2016;83(5):1013–4. https://doi.org/10.1016/j.gie.2015.11.003.
Carballal S, Maisterra S, Lopez-Serrano A, et al. Real-life chromoendoscopy for neoplasia detection and characterisation in long-standing IBD. Gut. 2016;
Picco MF, Pasha S, Leighton JA, Bruining D, Loftus EV Jr, Thomas CS, et al. Procedure time and the determination of polypoid abnormalities with experience: implementation of a chromoendoscopy program for surveillance colonoscopy for ulcerative colitis. Inflamm Bowel Dis. 2013;19(9):1913–20. https://doi.org/10.1097/MIB.0b013e3182902aba.
Davies J, Burke D, Olliver JR, et al. Methylene blue but not indigo carmine causes DNA damage to colonocytes in vitro and in vivo at concentrations used in clinical chromoendoscopy. Gut. 2007;56:155–6.
Repici A, Di Stefano AF, Radicioni MM, et al. Methylene blue MMX tablets for chromoendoscopy. Safety tolerability and bioavailability in healthy volunteers. Contemp Clin Trials. 2012;33(2):260–7. https://doi.org/10.1016/j.cct.2011.11.006.
Lieberman DA, Rex DK, Winawer SJ, Giardiello FM, Johnson d, Levin TR. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2012;143(3):844–57. https://doi.org/10.1053/j.gastro.2012.06.001.
Engelsgjerd M, Farraye FA, Odze RD. Polypectomy may be adequate treatment for adenoma-like dysplastic lesions in chronic ulcerative colitis. Gastroenterology. 1999;117(6):1288–94; discussion 1488-91. https://doi.org/10.1016/S0016-5085(99)70278-7.
Odze RD, Farraye FA, Hecht JL, Hornick JL. Long-term follow-up after polypectomy treatment for adenoma-like dysplastic lesions in ulcerative colitis. Clin Gastroenterol Hepatol. 2004;2(7):534–41. https://doi.org/10.1016/S1542-3565(04)00237-X.
Rubin PH, Friedman S, Harpaz N, et al. Colonoscopic polypectomy in chronic colitis: conservative management after endoscopic resection of dysplastic polyps. Gastroenterology. 1999;117:1295–300.
Vieth M, Behrens H, Stolte M. Sporadic adenoma in ulcerative colitis: endoscopic resection is an adequate treatment. Gut. 2006;55:1151–5.
Wanders LK, Dekker E, Pullens B, et al. Cancer risk after resection of polypoid dysplasia in patients with longstanding ulcerative colitis: a meta-analysis. Clin Gastroenterol Hepatol. 2014;12:756–64.
Ten Hove JR, Mooiweer E, Dekker E, et al. Low rate of dysplasia detection in mucosa surrounding dysplastic lesions in patients undergoing surveillance for inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2017;15(2):222–8 e2. https://doi.org/10.1016/j.cgh.2016.08.035.
Smith LA, Baraza W, Tiffin N, et al. Endoscopic resection of adenoma-like mass in chronic ulcerative colitis using a combined endoscopic mucosal resection and cap assisted submucosal dissection technique. Inflamm Bowel Dis. 2008;14:1380–6.
Blonski W, Kundu R, Furth EF, et al. High-grade dysplastic adenoma-like mass lesions are not an indication for colectomy in patients with ulcerative colitis. Scand J Gastroenterol. 2008;43:817–20.
Ullman T, Croog V, Harpaz N, et al. Progression of flat low-grade dysplasia to advanced neoplasia in patients with ulcerative colitis. Gastroenterology. 2003;125:1311–9.
Thomas T, Abrams KA, Robinson RJ, et al. Meta-analysis: cancer risk of low-grade dysplasia in chronic ulcerative colitis. Aliment Pharmacol Ther. 2007;25(6):657–68. https://doi.org/10.1111/j.1365-2036.2007.03241.x.
Befrits R, Ljung T, Jaramillo E, et al. Low-grade dysplasia in extensive, long-standing inflammatory bowel disease: a follow-up study. Dis Colon rectum. 2002;45:615–20.
Hata K, Watanabe T, Kazama S, et al. Earlier surveillance colonoscopy programme improves survival in patients with ulcerative colitis associated colorectal cancer: results of a 23-year surveillance programme in the Japanese population. Br J Cancer. 2003;89:1232–6.
Lim CH, Dixon MF, Vail A, Forman D, Lynch d, Axon AT. Ten year follow up of ulcerative colitis patients with and without low grade dysplasia. Gut. 2003;52(8):1127–32. https://doi.org/10.1136/gut.52.8.1127.
Bernstein CN, Blanchard JF, Kliewer E, Wajda A. Cancer risk in patients with inflammatory bowel disease: a population-based study. Cancer. 2001;91(4):854–62. https://doi.org/10.1002/1097-0142(20010215)91:4<854::AID-CNCR1073>3.0.CO;2-Z.
Dekker E, van den Broek FJ, Reitsma JB, et al. Narrow-band imaging compared with conventional colonoscopy for the detection of dysplasia in patients with longstanding ulcerative colitis. Endoscopy. 2007;39(3):216–21. https://doi.org/10.1055/s-2007-966214.
Ignjatovic A, East JE, Subramanian V, Suzuki N, Guenther T, Palmer N, et al. Narrow band imaging for detection of dysplasia in colitis: a randomized controlled trial. Am J Gastroenterol. 2012;107(6):885–90. https://doi.org/10.1038/ajg.2012.67.
van den Broek FJ, Fockens P, van Eeden S, et al. Narrow-band imaging versus high-definition endoscopy for the diagnosis of neoplasia in ulcerative colitis. Endoscopy. 2011;43(02):108–15. https://doi.org/10.1055/s-0030-1255956.
Pellise M, Lopez-Ceron M, Rodriguez de Miguel C, et al. Narrow-band imaging as an alternative to chromoendoscopy for the detection of dysplasia in long-standing inflammatory bowel disease: a prospective, randomized, crossover study. Gastrointest Endosc. 2011;74:840–8.
Leifeld L, Rogler G, Stallmach A, Schmidt C, Zuber-Jerger I, Hartmann F, et al. White-light or narrow-band imaging colonoscopy in surveillance of ulcerative colitis: a prospective multicenter study. Clin Gastroenterol Hepatol. 2015;13(10):1776–81 e1. https://doi.org/10.1016/j.cgh.2015.04.172.
Neumann H, Kiesslich R. Endomicroscopy and endocytoscopy in IBD. Gastrointest Endosc Clin N Am. 2013;23(3):695–705. https://doi.org/10.1016/j.giec.2013.03.006.
Gunther U, Kusch D, Heller F, et al. Surveillance colonoscopy in patients with inflammatory bowel disease: comparison of random biopsy vs. targeted biopsy protocols. Int J Color Dis. 2011;26:667–72.
Hlavaty T, Huorka M, Koller T, et al. Colorectal cancer screening in patients with ulcerative and Crohn’s colitis with use of colonoscopy, chromoendoscopy and confocal endomicroscopy. Eur J Gastroenterol Hepatol. 2011;23:680–9.
Rispo A, Castiglione F, Staibano S, et al. Diagnostic accuracy of confocal laser endomicroscopy in diagnosing dysplasia in patients affected by long-standing ulcerative colitis. World J Gastrointest Endosc. 2012;4:414–20.
Naymagon S, Marion JF. Surveillance in inflammatory bowel disease: chromoendoscopy and digital mucosal enhancement. Gastrointest Endosc Clin N Am. 2013;23:679–94.
Subramanian V, Ragunath K. Advanced endoscopic imaging: a review of commercially available technologies. Clin Gastroenterol Hepatol. 2014;12(3):368–76 e1. https://doi.org/10.1016/j.cgh.2013.06.015.
Committee AT. Confocal laser endomicroscopy. Gastrointest Endosc. 2014;80:928–38.
Committee AT, Kwon RS, Wong Kee Song LM, et al. Endocytoscopy. Gastrointest Endosc. 2009;70(4):610–3. https://doi.org/10.1016/j.gie.2009.06.030.
Kisiel JB, Yab TC, Nazer Hussain FT, Taylor WR, Garrity-Park MM, Sandborn WJ, et al. Stool DNA testing for the detection of colorectal neoplasia in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013;37(5):546–54. https://doi.org/10.1111/apt.12218.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Inflammatory Bowel Disease
Rights and permissions
About this article
Cite this article
Limdi, J.K., Farraye, F.A. An Update on Surveillance in Ulcerative Colitis. Curr Gastroenterol Rep 20, 7 (2018). https://doi.org/10.1007/s11894-018-0612-2
Published:
DOI: https://doi.org/10.1007/s11894-018-0612-2