Abstract
Cardiovascular interventional and implantable devices must be safe and efficacious, as well as biocompatible. Surface treatment is of importance to the design and function of these devices. Lubricity, wear resistance, thrombogenicity, inflammation, and infections can all be affected significantly by surface treatments. The surfaces of cardiovascular interventional and implantable devices can either be modified with active or passive coating. Devices with active coating such as drug eluting stents (DES) deliver therapeutic agents that can enhance the mechanical function and modulate long-term vascular responses. In some implantable devices such as vascular grafts, endothelial cell growth is desirable. This is achievable with the addition of a coating or a modification to the surface properties of the device. This chapter reviews some of the most commonly used cardiovascular interventional and implantable devices with an overview of the role that surface treatments have in their functionality and safety.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
5.1 Introduction
Cardiovascular interventional tools are used in the treatments of coronary arterial diseases, heart failure, and peripheral arterial diseases. These devices are not intended for long-term implantation. There are two main interventional procedures that are performed today: percutaneous transluminal coronary angioplasty (PTCA) and stenting. Both are performed via catheterizations.
The earliest known cardiac catheterization was performed by Hales in 1711. More recently, Gruntzing and Myler performed the first human coronary angioplasty in May 1977 [1–3]. Currently, 1.2 million Americans undergo cardiac catheterization and over 1.5 million receive a percutaneous coronary intervention such as balloon angioplasty , atherectomy, or stent implantation annually [4].
Percutaneous transluminal coronary angioplasty (PTCA) , commonly known as balloon angioplasty, is performed by threading a balloon catheter through the femoral artery, located in the groin, to a trouble spot in an artery of the heart (Fig. 5.1). The balloon is then inflated, compressing the plaque and dilating (widening) the narrowed coronary artery so that blood can flow more easily. This is often accompanied by inserting an expandable metal stent. Stents are wire mesh tubes used to prop open arteries after PTCA.
Cardiovascular interventional devices commonly used include the following:
Guiding catheter —a long, thin, flexible tube that acts as a conduit for injection of contrast. A guiding catheter delivers other devices, i.e., a balloon catheter or a stent delivery catheter into the coronary vasculature. A guiding catheter often contains metallic braiding to help provide push-ability and torque-ability [5] (Fig. 5.2).
Guide wire —a long, thin, flexible wire that acts as a railing for delivery of a balloon catheter and stent delivery system. It is typically made from stainless steel or nickel titanium (Fig. 5.3).
Track-ability (the ease of tracking a balloon over the guide wire up to the target lesion) and push-ability (the ability to advance the balloon across the lesion) are more important to the practice of interventional cardiology than any other in vitro measure. However, there are no reliable in vitro methods for measuring these two properties. A variety of lubricious coatings exist for the guidewires, which reduce friction, facilitate advancement of interventional devices, and enhance lesion crossing. Examples include hydrophilic coatings, silicone (hydrophobic), and PTFE coating [6].
Hydrophilic coating must be hydrated to be effective. However, this might not be appropriate for all devices. Hydrophobic coatings, such as silicone, when applied to the surface, are not as lubricious as hydrophilic coatings but provide more tactile feedback as the physician manipulates the devices.
5.2 Key Surface Properties for Cardiovascular Interventional Devices
Friction is the primary metric of concern. However, where energy is transmitted from the surface of the devices, for example during ablation, the insulation material property also becomes a concern. Friction generally dissipates energy in the form of heat. This deficit must be overcome to maintain two objects moving at a constant velocity with respect to one another. The process of wear also accompanies the presence of frictional forces between two surfaces.
Magnitude of friction and wear is generally regulated by modification of the interface between the two surfaces. The various surface treatment methods, solid, liquid, and gas, all provide lubrication. Not only is the coefficient of friction a measurable of importance but also provides insights pertaining to the mechanism of lubrication. The principle lubrication mechanisms are hydrodynamic, elastohydrodynamic, mixed and boundary [7].
In cardiovascular applications, there is usually not sufficient film thickness between two surfaces to provide hydrodynamic lubrication, as the typical distance between the two surfaces is not sufficient. In hydrodynamic lubrication the surfaces are at greater distances from one another. Boundary lubrication represents the opposite situation where the distance between the two surfaces is minimal.
The lubrication mechanism is largely a function of surface property modification. An effective boundary lubricant usually interacts with the surface of the interventional or implantable device. Hydrophilic coatings usually provide effective boundary lubrication of cardiovascular interventional and implantable devices. Elastohydrodynamic lubrication provides a film thickness that is slightly less than that found in hydrodynamic lubrication. In this scenario, pressure waves can cause a deformation in the tissue surface opposite of the interventional or implantable device.
As the distance between the surfaces decreases from elastohydrodynamic lubrication, mixed lubrication occurs. Mixed lubrication has a higher coefficient of friction and wear rate than hydrodynamic lubrication. As a result of the dimensional constraints, most cardiovascular interventional and implantable devices provide lubrication via boundary and mixed lubrication.
The surface properties are modified in an attempt to minimize coefficient of friction. The two primary methods to accomplish this are hydrophobic and hydrophilic coating. Hydrophilic coating is activated by an aqueous environment; where a layer of slippery hydrogel is created on the device surface, reducing the friction force [8–10]. Hydrophilic coating might not be appropriate for all devices such as those that are not constantly hydrated [11]. Hydrophobic coatings such as silicone can also be applied to the surface but it is not as lubricious as a hydrophilic coating. It does, however, provide more tactile feedback to the operating physician.
5.3 Cardiovascular Implantable Devices
Unlike interventional tools , cardiovascular implantable devices remain in the cardiovascular system usually until the device must be removed as a result of functional failure. These failures can be classified as either mechanical or surface property failure. The heart, along with the arterial and venous system, can be defined as an electromechanical system. Certain implantable devices focus on treatment of electrical aspects while others focus on mechanical aspects.
5.4 Electrical Implantable Devices
The rhythm management of the heart is regulated by two different types of myocardial cells; pacemaker cells and conducting cells. Pacemaker cells, located in the sinoatrial (SA) node and atrioventricular (AV) node are ,respectively located where the superior vena cava and right atrium join in the inferior portion of the interatrial septum [4]. Conducting cells, referred to as the Bundles of His and Purkinje Fibers, serve the function of relaying action potentials from the SA node to the AV node and to all parts of the ventricle.
Devices used by clinicians in the regulation of the rhythm management of the heart include: implantable pulse generators (pacemakers), implantable cardioverter defibrillators (ICD) , pacemaker and ICD leads, and implantable loop recorders. These devices are generally implanted in the muscle cavity of the pectoral region (Figs. 5.4, 5.5, 5.6, 5.7 and 5.8).
Pacemakers deliver electrical impulses to the heart via a special conductor called a pacemaker lead (Figs. 5.4 and 5.5). One end of the lead is connected to the pacemaker and the other end of the lead contains a metallic electrode, which is in contact with the heart tissue, stimulating the heart to contract. The lead also carries information from the heart back to the pulse generator, which the physician accesses via a special external programmer [12, 13].
The pacemaker case is made of titanium, a metal that is 10 times as strong as steel, but much lighter. Titanium and its alloy are biocompatible. The titanium casing was developed to enclose the battery and circuitry. Epoxy resin with silicone rubber encased the inner components in previous designs.
Titanium casings with special filters help to shield the components and greatly reduce outside electromagnetic interference. Patients with these newly designed pacemakers can now safely use microwave ovens and other appliances and equipment found in the home and office.
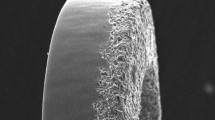
A nitride coating can be deposited via sputtering technique onto the surface of the pacemaker metallic electrode on the pacemaker leads to improve the sensing and pacing performances over an electrode with a smooth, unsputtered surface [14].
When the heart beats in asynchronous rhythms, the ICD deliver an electric shock that can “reset” the heart back to its normal rhythm. The standard material construction of the casing is the same as that of the pulse generator. Another implantable electrical device called an implantable loop recorder provides the function of recording an electrocardiogram (ECG) before and after the onset of symptoms (Fig. 5.8).
5.5 Mechanical Implantables
The heart, as a mechanical system, acts as a positive displacement pump to circulate blood through the cardiovascular system. Devices used by clinicians in the treatment of cardiovascular disease include: stents, vascular grafts and stent grafts, and heart valves.
A stent is a wire mesh tube used to prop open an artery during angioplasty (Fig. 5.9). The stent is collapsed to a small diameter and put over a balloon catheter. It is then moved into the area of the blockage. When the balloon is inflated, the stent expands, locks in place and forms a scaffold. This holds the artery open. The stent stays in the artery permanently, holds it open, improves blood flow to the heart muscle and relieves symptoms (i.e., chest pain) [15].
Stents have virtually eliminated many of the complications that used to accompany “plain old balloon angioplasty” (POBA) such as abrupt and unpredictable closure of the vessel, which can result in emergency bypass surgery. The additional structural strength of the stent can also help to keep the artery open while the healing process progresses.
Vascular grafts are classified into two major categories. Large diameter grafts (>10 mm) primarily made up of Dacron (80 %) and PTFE (20 %) are primarily used for aortic and iliac artery reconstruction. The small caliber grafts (<10 mm) are primarily used for coronary artery bypass grafts (CABG) , lower-extremity bypass procedures, and hemodialysis access. The patency rates for the synthetic graft material are better for the aortic and iliac artery reconstruction than for when small caliber grafts are used. Saphenous vein grafts and internal mammary grafts both have greater patency rates than the small caliber vascular grafts with the internal mammary artery providing the superior patency rates.
Dacron (polyethylene terphthlate) and PTFE (polytetrafluoroethylene) maintain their tensile strength for years after being implanted. However, other materials such as Nylon (polyamide), Ivalon, and Orlon decrease in tensile strength after months of being implanted. Woven Dacron grafts are nonporous with no stretch while knitted Dacron grafts have variable stretch and are porous. As previously mentioned, the patency rates for the use of these grafts are better for large vessel grafts [16].
Neointimal hyperplasia, which occurs in the anastomotic area, is the prime reason of failure of small caliber grafts. The low compliance rates leading to compliance mismatch play a role as well. The neointimal hyperplasia could be caused by platelet deposition with local release of platelet-derived growth factor (PDGFP) , other growth factor stimulation of smooth muscle cell (SMC) proliferation, monocyte recruitment, complement activation, leukocyte deposition, chronic inflammation, and mechanical stimuli such as stress and shear abnormalities [16]. Additionally, the optimal sizing of a graft is important to provide a wall shear rate that will increase the long-term patency of the synthetic grafts [17].
Other devices within this classification include stent grafts and heart valves. Stent grafts combine the mechanical scaffolding function of stents and conduit function of vascular grafts. Heart valves provide a mechanical replacement for failing bicuspid and tricuspid valves.
These devices primary function is to serve either a structural or dynamic primary function. However, the surface treatment of these devices does have a significant effect on the efficacy of these devices.
5.6 Important Surface Properties for Implantable Cardiovascular Devices
The surface properties of materials are modified to reduce adherence to vascular tissue. This can be accomplished via various treatment methods. However, the surface modification is not always solely for mechanical purposes. The surface modification can also provide therapeutic benefit.
Pyrolitic carbon is used in cardiovascular applications in artificial hearts and prosthetic heart valves. The material has similarities to graphite with covalent bonding present between the graphene sheets. The risk of thrombosis is reduced when using pyrolytic carbon, as blood clots are less likely to form when it is used. However, as a precaution, the patient who receives a prosthetic heart valve must be on an anticoagulant regimen.
In addition to prosthetic heart valves, bioprosthetic heart valves, made from porcine valves or bovine pericardium, can be used to replace the natural valves. The tissue of the valves can be treated to prevent calcification via special processing [18].
The Mosaic® aortic and mitral bioprosthesis, manufactured by Medtronic, uses the AOA method, which has been observed to reduce the buildup of calcium in animal studies. The only stented valve in the U.S. that incorporates this tissue treatment is the Mosaic® bioprosthesis. One likely method of the AOA process function is via the binding of free aldehyde groups of glutaraldehyde to the amino group of AOA molecules. This process, referred to as capping, is believed to inhibit the mineralization of tissues. Another viable mechanism by which AOA treatment minimizes calcification is slowing down the diffusion of calcium ions though the treated tissues (Fig. 5.10).
The surfaces of stents have evolved to include the delivery of drugs that have proven successful in the reduction of restenosis rates. Restenosis rates have been observed to reduce significantly when the stent surface is coated such that siromilus and paclitaxel are eluted [19]. Biodegradable materials using the mechanism of autologous cell seeding has shown potential. However, the pretreatment of materials increases the opportunity for infection. A biodegradable graft material made up of polylactic-co-glycolic acid as a biodegradable scaffold material compounded with a collagen microsponge has shown positive results. No thrombus formation was observed, while the polylactic-co-glyclolic acid scaffold was almost completely absorbed over a 6-month period [20]. Polyethylene oxide (PEO) has also been used to modify biomaterial surfaces to minimize or prevent protein absorption and cell adhesion.
Minimization of thrombosis is a key to the reduction or restenosis where stents are implanted. To achieve this goal, usually the mechanisms focused on are minimizing coagulation, platelet adhesion, and platelet activation. However, the role of complement activation prior to platelet activation and the role of leukocytes could play a significant role in the minimization of thrombosis as well [21].
Surface oxide formation has also been observed to be a significant factor in determining the degree of thrombosis. However, amorphous oxide film may provide a solution to the thrombosis caused by metal [22].
Several other surface modifications of the stents to reduce restenosis and thrombogenicity by improved biocompatibility have also been evaluated with varying degrees of success: metallic coatings: gold, titanium, copper; phosphorylcholine (PC), a synthetic mimetic outer wall of red blood cells; heparin; silicon carbide; and carbon and fluorinated diamond like carbon (F-DLC) [23–25].
References
Blake, D. M., & Maness, P. C. (1999). Separation and Purification Methods, 28(1), 1–50.
Byrne, J. A., Eggins, B. R., Brown, N. M. D., McKinney, B., & Rouse, M. (1998). Applied Catalysis, B: Environmental, 1998(17), 25–36.
Byrne, J. A., Davidson, A., Dunlop, P. S. M., & Eggins, B. R. (2002). Journal of Photochemistry and Photobiology A: Chemistry, 148, 365–374.
Byrne, J. A., Hamilton, J. W. J., McMurray, T. A., Dunlop, P. S. M., Jackson, V., Donaldson, A., et al. (2006). Abstracts of the NSTI conference, Boston.
Coleman, H. M., Routledge, E. J., Sumpter, J. P., Eggins, B. R., & Byrne, J. A. (2004). Water Research, 38, 3233–3240.
Cosnier, S., Gondran, C., Senillou, A., Gratzel, M., & Vlachopoulos, N. (1997). Electroanalysis, 9(18), 1387–1392.
Dunlop, P. S. M., Byrne, J. A., Manga, N., & Eggins, B. R. (2002). Journal of Photochemistry and Photobiology A: Chemistry, 148, 355–363.
Fujishima, A., & Honda, K. (1972). Nature, 238, 37–38.
Fujishima, A., Rao, T. N., & Tryk, D. A. (2000). Journal of Photochemistry and Photobiology C: Photochemistry Reviews, 1, 1–21.
Giavaresi, G., Ambrosio, L., Battiston, G. A., Casellato, U., Gerbasi, R., Finia, M., et al. (2004). Biomaterials, 25, 5583–5591.
Hoffman, M. R., Martin, S. T., Choi, W., & Bahnemann, D. W. (1995). Chemical Reviews, 95, 69–96.
Holgers, K. M., & Ljungh, A. (1999). Biomaterials, 20, 1319–1326.
Huang, N., Yang, P., Leng, Y. X., Chen, J. Y., Sun, H., Wang, J., et al. (2003). Biomaterials, 24, 2177–2187.
Kuhn, K. P., Chaberny, I. F., Massholder, K., Stickler, M., Benz, V. W., Sonntag, H.-G., & Erdinger, L. (2003). Chemosphere, 53, 71–77.
Lee, S.-H., Kim, H.-W., Lee, E.-J., Li, L.-H., & Kim, H.-E. (2006). Journal of Biomaterials Applications, 20, 195–208.
Liu, X., Zhao, X., Ding, C., & Chu, P. K. (2006). Applied Physics Letters, 88, 13905.
McMurray, T. A., Byrne, J. A., Dunlop, P. S. M., Winkelman, J. G. M., Eggins, B. R., & McAdams, E. T. (2004). Applied Catalysis, A: General, 262(1), 105–110.
McMurray, T. A., Byrne, J. A., Dunlop, P. S. M., & McAdams, E. T. (2005). Journal of Applied Electrochemistry, 35, 723–731.
Mills, A., & Le Hunte, S. (1997). Journal of Photochemistry and Photobiology A: Chemistry, 108, 1–35.
Nygren, H., Tengvall, P., & Lundstrom, I. (1997). Journal of Biomedical Materials Research, 34, 487–492.
Ohko, Y., Utsumi, Y., Niwa, C., Tatsuma, T., Kobayakawa, K., Satoh, Y., et al. (2001). Journal of Biomedical Materials Research (Applied Biomaterials), 58, 97–101.
Pan, J., Leygraf, C., Thierry, D., & Ektessabi, A. M. (1997). Journal of Biomedical Materials Research, 35, 309–318.
Ramires, P. A., Romito, A., Cosentino, F., & Milella, E. (2001). Biomaterials, 22, 1467–1474.
Shani Sekler, M., Levi, Y., Polyak, B., Dunlop, P. S. M., Byrne, J. A., & Marks, R. S. (2004). Journal of Applied Toxicology, 24, 395–400.
Yang, Y., Glover, R., & Ong, J. L. (2003). Colliods and Surfaces B: Biointerfaces, 30, 291–297.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Whitt, M., Senarith, P., Handy, R., Jackson, M.J. (2016). Cardiovascular Interventional and Implantable Devices. In: Ahmed, W., Jackson, M.J. (eds) Surgical Tools and Medical Devices. Springer, Cham. https://doi.org/10.1007/978-3-319-33489-9_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-33489-9_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-33487-5
Online ISBN: 978-3-319-33489-9
eBook Packages: EngineeringEngineering (R0)