Abstract
IBD has classically been associated with malnutrition and weight loss, although this has become less common with advances in treatment and greater proportions of patients attaining clinical remission. However, micronutrient deficiencies are still relatively common, particularly in CD patients with active small bowel disease and/or multiple resections. In this chapter, we will discuss the major essential micronutrients (B vitamins, vitamin C, fat-soluble vitamins, calcium, magnesium, and trace elements) and the risk of deficiency in IBD patients. We will also discuss risk factors for deficiency, clinical manifestations, diagnostic methods, and treatment for replacement. In addition, we will discuss the evidence for utilizing nutritional supplementation for primary and secondary prevention of IBD-related complications in high-risk patient populations, such as wound healing, skeletal bone loss, and colorectal cancer prevention.
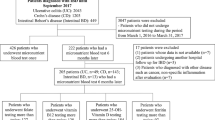
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Inflammatory bowel disease
- Crohn’s disease
- Ulcerative colitis
- Nutrition
- Nutritional assessment
- Nutritional deficiencies
- Micronutrient deficiencies
- Vitamins
- Vitamin deficiency
- Minerals
- Trace elements
- Calcium
- Dietary supplements
- Vitamins
- Nutritional status
- Parenteral nutrition
- Folic acid
- Vitamin B12/cyanocobalamin
- Vitamin B6/pyridoxine
- Vitamin A
- Vitamin K
- Vitamin C
Introduction
The inflammatory bowel diseases (IBD), which include ulcerative colitis and Crohn’s disease , are chronic inflammatory conditions of the gastrointestinal tract which increase patients’ risk of malnutrition. Previous retrospective studies demonstrated that as many as 70–80 % of IBD patients exhibited weight loss during their disease course [1–4]. However, most of these studies were performed from the 1960–1980s and primarily included hospitalized patients with severe active disease, often on chronic steroid therapy .
In the last three decades, there have been several important advances in the treatment of IBD —namely, the development of multiple biologic drugs and increased use of “top-down” strategies with early combination therapy—that may be leading to a greater proportion of IBD patients attaining sustained clinical remission. Nutritional studies performed in the post-biologic era seem to suggest that IBD patients who are in remission generally have similar macronutrient intake [5, 6] and similar body mass indices [7, 8] as healthy controls. In fact, several recent studies have reported that there is a growing proportion of obese IBD patients [7, 9, 10].
In general, malnutrition can be divided into forms that involve deficiencies in macronutrients (energy and protein intake) and those of micronutrients (vitamins, minerals, trace elements). Protein-energy malnutrition can result in weight loss and loss of muscle mass, and most often occurs with active, severe IBD. However, micronutrient deficiencies can occur even with disease that is relatively mild or in remission. Multiple simultaneous deficiencies in micronutrients are more common in patients with Crohn’s disease (CD) , especially those with fistulas, strictures, or prior surgical resections of the small bowel [2].
Numerous vitamin and mineral deficiencies have been reported in IBD patients [1–4]. Notably, the research in this area is lacking, as many of the studies are limited by small sample sizes, retrospective design, and frequent use of non-validated nutritional assessment methods and statistical analysis. In addition, laboratory testing that is clinically available (often measurements of plasma or serum levels of micronutrients) can be inaccurate in reflecting micronutrient status, and optimal levels of many micronutrients have yet to be established.
The most common micronutrient deficiencies in IBD patients are those of iron and vitamin D , which are discussed in detail in separate chapters. In this section, we will review the available data on the other micronutrient deficiencies that can occur with IBD and their clinical significance in this population.
Normal Micronutrient Absorption and Dietary Requirements
Vitamins and minerals are required for diverse biochemical functions in the body, including regulation of cell and tissue growth, energy metabolism, and direct antioxidant actions [11, 12]. Since all vitamins and many minerals (the so-called essential elements ) are not sufficiently synthesized by humans, they need to be obtained from the diet.
Vitamins are organic compounds that can be classified as either water- or fat-soluble. Water-soluble vitamins (B vitamins, vitamin C) are readily absorbed in the intestinal lumen across enterocyte membranes by either diffusion (for non-charged, low-molecular vitamins such as vitamins B3, B6, and C) or by carrier-dependent active transport. The fat-soluble vitamins (A, D, E, and K) are hydrophobic substances that are dissolved first within fat droplets, then broken down by lipases and combined with bile salts in the duodenum to form mixed micelles which can diffuse across the enterocyte membrane [11].
Dietary minerals are inorganic elements that are important in the makeup of cellular structure and as cofactors and catalysts in enzymatic processes. The so-called “macro” minerals are those present in larger quantities in the body (i.e., kilo- or milligrams) and include calcium, phosphate, potassium, magnesium, and iron. Trace elements are present in very small amounts in the body (i.e., nanograms or parts per million), and include zinc, copper, and selenium. Macrominerals and trace elements are absorbed by passive or active transport through the intestinal mucosa, often using specialized transport proteins such as the calcium-specific TRPV6 (Transient Receptor Protein) or the more diverse DMT1 (divalent metal transporter 1) which transports several divalent metals including ferrous (Fe2+), zinc (Zn2+), and copper (Cu2+) [11, 12].
Normally, over 95 % of vitamins and minerals within food are absorbed in the proximal small bowel, usually prior to reaching the mid-jejunum [11]. The exception to this is vitamin B12, which, when bound to intrinsic factor, is absorbed in the terminal ileum. In addition, the distal ileum also absorbs bile acids, which are critical for the absorption of fat and fat-soluble vitamins.
Dietary Requirements
Recommendations for the dietary intake of individual vitamins and minerals vary tremendously, ranging on the order of nanograms to milligrams per day. In the United States, the most widely accepted dietary guidelines were developed by the Institute of Medicine’s Food and Nutrition Board , mainly for public health purposes such as food labeling and school meal planning . These guidelines (often termed “Dietary Reference Intakes ”) were expanded recently to account for new data that certain nutrients may help promote health and prevent disease [11, 12]. In addition, because of the recognition that a growing number of persons (39 % of American adults surveyed in the National Health and Nutrition Examination Survey [NHANES] [13]), take multivitamins and other dietary supplements, DRIs also now include information about levels associated with toxicity.
The DRI’s are actually a set of four reference values (Table 5.2):
-
Recommended Dietary Allowance (RDA): Average daily dietary intake of a nutrient that is sufficient to meet the requirement of nearly all (97–98 %) healthy persons. This is the most commonly referenced DRI value.
-
Adequate Intake (AI): For nutrients for which an RDA cannot be determined based on a lack of available data. The AI is established based on observed intakes of that individual nutrient by a group of healthy persons.
-
Tolerable Upper Intake Level (UL): Highest daily intake of a nutrient that is likely to pose no risks of toxicity for almost all individuals.
-
Estimated Average Requirement (EAR) is the amount of a nutrient that is estimated to meet the requirement of half of all healthy individuals in the population.
These values are listed in Table 5.2, and are also available online on the USDA or IOM websites:
http://fnic.nal.usda.gov/dietary-guidance/dietary-reference-intakes/dri-tables,
http://www.iom.edu/Activities/Nutrition/SummaryDRIs/DRI-Tables.aspx.
It is important to recognize that the DRI values were established based on healthy populations and thus may not reflect the needs of IBD patients. Notably, for patients with active disease and significant diarrhea, daily requirements for iron, potassium, calcium, magnesium, and zinc may increase significantly [2, 5]. In addition, many of the foods that are rich in these micronutrients may be difficult for some IBD patients to tolerate (refer to Table 5.2 for a list of foods). Therefore, oral supplementation may be required in certain situations, though caution must be taken with regard to counseling about supplementation, especially with certain micronutrients such as zinc and vitamin A, in which there is a narrow margin between the recommended dietary allowance (RDA) and the upper limit (UL) exists. In general, careful monitoring of supplementation should be practiced with any micronutrient that has an UL.
Pathophysiology of Micronutrient Deficiencies in IBD
Micronutrient deficiencies in IBD patients can occur by multiple mechanisms. As summarized in Table 5.1, there are a multitude of risk factors in IBD, which can be related to disease symptoms (i.e., diarrhea, anorexia), disease-related complications (i.e., bowel resection), and from drug treatments (i.e., sulfasalazine and folate antagonism).
One of the most important and probably underrecognized mechanisms for malnutrition in IBD is reduced food intake. Globally reduced intake and specific avoidance of foods is common among IBD patients. This may be particularly significant with active disease, due to anorexia (secondary to inflammatory cytokines, including interleukin IL-6, and tumor necrosis factor-alpha [TNF-α]) [14]. Many patients also self-restrict their diet to minimize symptoms of abdominal pain and diarrhea, commonly thought to be exacerbated by large fatty meals and high-residue diets.
A recent study showed that even in patients with disease in remission, persistent avoidance of major food groups remains common, with approximately one-third avoiding grains, another one-third avoiding dairy, and 18 % avoiding vegetables entirely [9]. In addition, multiple studies have reported that the majority of IBD patients, regardless of disease activity, intake levels of calcium and vitamin C that are significantly lower than Recommended Daily Allowance (RDA, Table 5.2). In addition, suboptimal intake of folate, thiamine (B1) and pyridoxine (vitamin B6), vitamin K, vitamin E and beta-carotene have also been reported to be prevalent amongst IBD patients [5, 15].
Two other important potential causes of malnutrition are enteric loss of nutrients (i.e., from diarrhea or fistula output) and malabsorption. Chronic diarrhea and fistula output can lead to wasting of zinc, calcium, and potassium [3] while iron deficiency is the most common nutritional deficiency in colitis, due largely to chronic gastrointestinal bleeding [16]. Malabsorption more frequently occurs in CD, due to small bowel inflammation or resection. Specifically, significant terminal ileal disease and/or resections >40–60 cm can lead to vitamin B12 deficiency as well as bile-salt wasting and resultant impaired fat-soluble vitamin absorption [17]. In addition, patients with advanced primary sclerosing cholangitis are also at risk for malabsorption, as biliary strictures especially within the main branches of the biliary tract can lead to bile-salt insufficiency and steatorrhea [17].
Finally, several medications used commonly in IBD can interfere with normal micronutrient absorption. Glucocorticoids potently inhibit calcium, phosphorus, and zinc absorption and may also lead to impaired metabolism of vitamins C and D [4]. Methotrexate is a potent folate antagonist and sulfasalazine interferes with folate absorption [18]. Proton pump inhibitors, antacids, and calcium supplements can inhibit iron absorption , if taken simultaneously as dietary or supplemental iron [16]. Cholestyramine, which may be used as an antidiarrheal adjunct, can interfere with absorption of fat-soluble vitamins [4, 11]. Finally, the use of long-term parenteral nutrition can lead to deficiencies in any micronutrient not added in sufficient quantities, most commonly vitamins A, D, E, zinc, copper, and selenium [19].
Specific Micronutrient Deficiencies in IBD
A wide array of vitamin and mineral deficiencies may occur in IBD patients, particularly those with moderate-to-severe disease activity, small bowel Crohn’s involvement, and history of bowel resection [1–4]. The most well-recognized nutritional deficiencies are those of iron, vitamin D, folate, cobalamin, and zinc [4–6]. Besides being relatively common in IBD cohorts , deficiencies in these micronutrients are associated with well-known clinical manifestations (i.e., anemia with iron or folate deficiency, and osteoporosis with vitamin D).
For many of the other micronutrients, the literature is sparse and the results of existing studies are often difficult to interpret, as there is significant variation with regard to the definitions of deficiency (i.e., inadequate dietary intake vs. serum levels vs. suspected clinical syndrome) and the type of IBD cohort studied (pediatric vs. adult, active disease vs. remission).
In this section, we will review the data available on the major essential micronutrients and the risk of deficiency for each in IBD . Specifically, we will focus on the prevalence, risk factors, clinical manifestations, diagnostic testing, and treatment with both diet and supplementation (summarized also in Tables 5.2, 5.3, and 5.4).
Major B Vitamins
Folate (Vitamin B9)
Folic acid plays an important role in erythrocyte metabolism, serving as a cofactor in DNA synthesis and erythrocyte division [11, 18]. Consequently, folate deficiency is classically associated with a macrocytic megaloblastic anemia . In addition, because folate is an important cofactor in the conversion of homocysteine to methionine, folate deficiency can lead to accumulation of homocysteine levels in the blood. Hyperhomocysteinemia is a known risk factor for arterial and potentially venous thromboembolism [28, 29]. In patients with IBD there is an increased prevalence of hyperhomocysteinemia (defined as fasting plasma level >15 ng/mL), with reported frequency between 11 and 52 %, compared with 3.3–5 % in the control population [30–33], which may at least partially account for the increased risk of thromboembolic disease in IBD patients.
A controversial association between folate deficiency and increased colorectal cancer risk in IBD has also been reported. Folate may play an important role in colonic inflammation and carcinogenesis , since it participates in biological methylation and nucleotide synthesis. In animal models , deficiencies have been associated with reduced levels of p53 mRNA, increased DNA strand breaks, and DNA hypomethylation in the colon [33, 34]. In human epidemiologic studies, low dietary folate intake has been associated with sporadic colorectal cancer [35–38]. Within the IBD population, there have been two case-control studies and a retrospective analysis that have shown decreased serum folate levels in patients with premalignant lesions or cancer in the colon, compared with colitis patients without neoplasms [39–41].
Folate deficiency can occur rather rapidly without regular daily intake, since total body stores only averages ~500–20,000 μg in healthy individuals and may be much lower in patients with acute illness or with malabsorptive disease [18]. Recommended Daily Allowance (RDA) for folic acid is 400 μg for healthy adults and 500–600 μg during pregnancy and lactation [11]. Daily intake up to 1000 μg might be required for individuals at higher risk for deficiency, including those on folate antagonist drugs such as methotrexate or sulfasalazine and those who consume significant and regular alcohol. Foods naturally rich in folic acid include dark leafy greens (spinach, collard, and turnip greens), asparagus, broccoli, citrus fruits, avocado, beets, and lentils (refer to Table 5.2). In the United States and Canada, nearly all cereals and enriched grain products are enriched with folate, due to national mandated programs launched in the 1980s to decrease rates of neural tube birth defects [42].
In spite of these folate fortification programs , IBD patients may be at increased risk of folic acid deficiency compared with the general population. While more recent studies demonstrate that folate deficiency is less prevalent than was previously reported in historical IBD cohort studies (51–80 %) [3, 4, 18], folate deficiency still appears to be relatively common, particularly in CD. In a recent retrospective case-control study performed in 2010, abnormal serum folate levels (<3 ng/mL) were found in 28.8 % of the CD patients, 8.8 % of ulcerative colitis (UC) patients, and 3 % of controls [43]. Three studies performed in CD —one of which only included patients with disease in remission—reported similar rates (20–26 %) of subnormal folate levels [24, 43, 44]. It should be noted that all of the above studies used serum folate level, although red blood cell (RBC) folate levels is a superior test as it averages folate levels over the preceding 3 months. There have been two studies utilizing RBC folate levels in IBD patients, showing much lower rates of deficiency seen (0–7 %) [45].
Potential mechanisms of folate deficiency in IBD include inadequate dietary intake, malabsorption, and medication interactions. Inadequate intake is likely a major contributor, as supported by two studies in which prospective food records of outpatient IBD showed inadequate folate intake in 40–78 % [5, 45]. Active Crohn’s ileitis and history of small bowel resection have been demonstrated to be risk factors for folate deficiency, supporting malabsorptive mechanisms [24, 43]. Finally, sulfasalazine and methotrexate both can cause folate deficiency, as both are inhibitors of dihydrofolate reductase and cellular uptake of folate [46].
Currently, there are no clear guidelines on screening for folate deficiency in IBD patients, especially in patients with disease in remission and who report no major restrictions in their diet. However, measuring folate levels (RBC levels preferred over serum) is definitely indicated in all anemic IBD patients, particularly those with CD. In addition, if patients display other clinical symptoms of folate deficiency, such as glossitis, angular stomatitis, or depression, checking folate status is warranted [11]. If RBC folate level is normal, but suspicion for folate deficiency is high, homocysteine levels can also be assessed. Elevated serum homocysteine is potentially more sensitive, although less specific for folate deficiency, since hyperhomocysteinemia can also occurs with deficiencies of vitamin B6 and B12 [18].
Once folate deficiency is diagnosed, folate supplementation of 1 mg/day is usually sufficient to replenish deficient folate stores within 2–3 weeks [47]. Following repletion of folate stores, folate intake at the DRI levels of 400–600 μg should be sufficient in the long term. The exception to this is patients who are on folate antagonist drugs (methotrexate or sulfasalazine) , pregnant IBD patients, and those on long-term TPN [48]. These higher-risk patients should receive at least 1 mg/day of folate indefinitely or for as long as their risk factor is present (i.e., until they are taken off folate antagonist/TPN or give birth).
Another potential indication for folate supplementation in IBD patients is the prevention of colitis-associated colorectal cancer (CRC) , although this is more controversial. There have been several small studies that have suggested folate may potentially have chemopreventative effects, at least on the molecular level. In one small prospective, placebo-controlled study of patients with sporadic adenomas , it was found that daily supplementation with 5 mg of folate was associated with an increase in genomic DNA methylation and a decrease in the extent of p53 strand breaks, after 6 and 12 months [33]. In UC patients, supplementation with folate at doses of 15 mg/day resulted in reduced cell proliferation/kinetics in the rectal mucosa [49]. Despite these preclinical studies, the findings of several meta-analyses cannot convincingly demonstrate a clear chemopreventative effect for folate [50, 51]. However, given the safety and low cost of folate, additional folate supplementation of at least 1 mg/day (or at least counseling about adequate dietary intake) should be considered in patients with multiple years of pancolitis or other risk factors for CRC.
Cyanocobalamin (Vitamin B12)
Vitamin B12, also known as cyanocobalamin, is an essential nutrient which serves as an important cofactor in normal energy metabolism as well as amino acid and fatty acid metabolism . Additionally, B12 is vital in a myriad of other vital physiological processes such as neuron function, blood formation, bone marrow health, and DNA synthesis/regulation.
Although probably less common than folate deficiency in the general population, vitamin B12 deficiency is an especially important consideration in patients with Crohn’s disease and in all elderly IBD patients. Similar to folate, deficiency in vitamin B12 is associated with a megaloblastic anemia and hyperhomocysteinemia [17, 30]. In addition to these hematological abnormalities, other clinical manifestations of B12 deficiency include neurologic and skeletal changes . Vitamin B12 deficiency appears to be associated with an increased risk of osteoporosis [52] and hip and spine fractures [53], possibly due to suppression of osteoblast activity [54]. In patients with neuropsychiatric manifestations, deficiency in vitamin B12 likely impacts neuronal myelin formation , leading to a syndrome marked by dementia, paresthesias, ataxia, weakness, and spasticity [11, 55].
Dietary sources of B12 principally come from animal products, particularly red meats, and marine sources such as mackerel, salmon, and sardine. Other sources of vitamin B12 are listed in Table 5.2. Gastrointestinal absorption of vitamin B12 occurs by a fairly complex process. Dietary cobalamin is cleaved from R factor by pancreatic proteases and binds to intrinsic factor, which is produced in the stomach. The IF-cobalamin compound then travels to the ileum where it binds to a specific receptor, cobalamin, and then is absorbed through the distal ileal mucosa. Since CD frequently affects the ileum, with 25–35 % of patients with isolated ileal inflammation and another 30–40 % with ileocolonic involvement [1], long-term inflammation can lead to impaired absorption of vitamin B12. Therefore, patients with CD are thought to be at significant risk for developing vitamin B12 deficiency [43].
In IBD cohorts, there have been few recent studies evaluating vitamin B12 status. In patients with CD, deficiency was reported in 11–22 % [17, 43, 56]. In the largest of these studies, Headstrom et al. [56] found in a retrospective multivariate analysis of 200 CD patients that the greatest risk factors for B12 deficiency were prior ileal resection (odds ratio [OR] 7.22; 95 % confidence interval [CI], 1.97–26.5) or ileocolonic resection (OR 5.81; 95 % CI, 2.09–10.12). Neither disease location nor duration was independently associated with risk of B12 deficiency. In contrast, UC is always confined to inflammation within the colon, and thus rates of B12 deficiency have generally been found to be comparable to that of the general population [43, 44]. However, there have been several reports of B12 deficiency in UC patients who have undergone proctocolectomy with ileoanal pouch anastomosis , although it is unclear if this may be related to the small amount of ileum resected during this anastomotic reconstruction (≈20–40 cm) or small bowel overgrowth of the pouch [57].
Diagnosis of vitamin B12 deficiency has traditionally been based on serum vitamin B12 levels, usually defined as less than 200 pg/mL (150 pmol/L), along with clinical evidence of disease. However, in many individuals, particularly elderly patients, irreversible neuropsychiatric manifestations can begin to occur, even in the absence of hematological manifestations of B12 deficiency [55]. Therefore, it is advocated that if serum B12 levels are normal in at-risk populations (Crohn’s disease patients with ileal disease, elderly IBD patients), that methylmalonic acid and homocysteine levels —metabolites of vitamin B12—be assessed next, as these appear to be more sensitive [55, 56].
Assessing for vitamin B12 status is definitively indicated in all IBD patients with anemia . In addition, any patient with new onset of depression, memory difficulties, motor dysfunction, severe fatigue, or personality changes should also be tested for B12 deficiency. In addition, periodic screening should be considered in all CD patients, especially those with active ileal CD or history of ileal resection, although the recommended intervals for screening have not been established. Previous studies have demonstrated that patients with terminal ileal resections of >60 cm will need lifelong B12 replacement, while up to 48 % of patients with shorter resection lengths of 20–40 cm are at risk of eventually developing B12 deficiency [58, 59].
In CD patients with intact ileum and whose disease is in remission, either oral or sublingual vitamin B12 supplementation can be considered. In patients with ileal resection or those with severe ileal inflammation, the optimal method for supplementation is less clear. Traditionally, the preferred approach has been monthly parenteral injections, as this route is inexpensive and is effective in quickly correcting B12 deficiency [47]. A recent Cochrane meta-analysis suggested that high-dose oral cobalamin of 1000–2000 μg (initially daily, then weekly, then monthly) was as effective as intramuscular injections in patients with B12 deficiency, although the studies did not include patients with CD [60]. However, it seems reasonable to assume that patients with IBD, especially active small bowel disease, may have impaired absorption of oral cobalamin. Therefore, at the current time further studies need to be performed before oral supplements can be widely recommended to IBD patients with B12 deficiency.
Pyridoxine (Vitamin B6)
Vitamin B6 (pyridoxine) is a water-soluble B vitamin that comes in several forms, including pyridoxine, pyridoxal, and pyridoxamine, as well as 5′ phosphates. Pyridoxal-5-phosphate (PLP), the biologically active form of vitamin B6, is a cofactor for over 140 biochemical reactions, including those involved in carbohydrate and protein metabolism, neuronal function, and RBC production. In addition, vitamin B6 may also play a role in inflammation, as Plasma PLP concentrations are inversely related to markers of inflammation such as C-reactive protein [61].
Since vitamin B6 is absorbed by passive diffusion in both jejunum and ileum, deficiency is less common than other B vitamins and rarely occurs in isolation. Although severe vitamin B6 deficiency is rare in the general population, mild inadequacy [plasma pyridoxal 5′-phosphate (PLP) <20 nmol/L] is observed in 19–27 % of the US population [62]. In IBD patients, only two studies to date have looked at vitamin B6 status. From these small studies, it appears that rates of vitamin B6 deficiency were 10–13 %, with one study demonstrating a greater risk in patients (27 % vs. 2.9 %, p < 0.01) with active disease compared with those with quiescent disease [63, 64]. Similar to earlier observations in rheumatoid arthritis, it has been suggested that inflammation can deplete plasma vitamin B6. Lastly, certain drugs, including corticosteroids and isoniazid, may interfere with B6 metabolism [46].
The RDA for vitamin B6 is 1.3–1.7 mg/day (Table 5.2) and sources can be found in both plant and animal sources, including grains, nuts, vegetable such as spinach and cabbage, and meats such as tuna, turkey, and beef. Food preparation and processing—particularly overcooking—can significantly reduce vitamin B6 availability up to 50 % [62].
Classic manifestations of vitamin B6 deficiency include a seborrheic dermatitis-like rash, atrophic glossitis, and neurological symptoms including neuropathy. Vitamin B6 status can be assessed by measuring PLP level (deficiency defined as <10 ng/mL). In certain IBD patients with suggestive symptoms, erythrocyte transaminase activity, with and without PLP added, can also used as a functional test of pyridoxine status, and may be a more accurate reflection of vitamin B6 status in critically ill patients [61, 62]. Vitamin B6 deficiency can be treated with 50–100 mg/day of pyridoxine daily [11].
Other B Vitamins
Thiamine (Vitamin B1)
Thiamine is a water-soluble vitamin that is important in the catabolism of sugars and amino acids, and in which severe deficiencies are associated with peripheral neuropathy and cardiomyopathy (beri-beri) [11]. Thiamine is found in multiple dietary sources (eggs, meats, bread, nuts), and high temperature cooking and baking as well as pasteurization can destroy thiamine. Similar to vitamin B6, thiamine absorption mainly occurs in the jejunum by varying degrees of active and passive transport, depending on body stores and luminal concentrations of thiamine.
There have been two small studies demonstrating that thiamine deficiency may be more common in CD patients compared with controls [5, 63]. The more recent of these studies was performed within the last decade on 54 CD patients whose disease was in remission. Even in this group, dietary thiamine intake was significantly lower than controls and low serum vitamin B1 was found in 32 % of patients [5]. The rate of thiamine deficiency in either active CD or in patients with UC is not known. In another study, IBD patients with fatigue attribute to mild intracellular thiamine deficiency were treated with oral or parenteral thiamine with reported improved in symptom [65]. The RDA for thiamine is 1.2–1.4 mg/day for the general population [11] and at least this amount should be recommended for patients with IBD. If patients are unable to meet these requirements through dietary sources, most B-complex multivitamins will provide sufficient amounts of thiamine.
Riboflavin (Vitamin B2)
Vitamin B2 (riboflavin) is a water-soluble vitamin that acts as an oxidant in several important reactions, including fatty acid oxidation, reduction of glutathione, and pyruvate decarboxylation. Dietary sources of vitamin B2 include meats, fish, eggs and milk, green vegetables, yeast, and certain enriched foods. Absorption occurs in the jejunum by sodium-dependent active transport. Deficiency can manifest with oral (angular cheilitis, cracked lips) and ocular (photophobia) symptoms. Riboflavin deficiency does not appear to be common in IBD , with only one study performed in 1983 documenting a modestly elevated incidence in CD patients compared with controls [63].
Niacin (Vitamin B3)
Niacin or nicotinic acid is another water-soluble member of the B complex family. It is a precursor to NAD+/NADH and NADP+/NADPH, and also is involved in both DNA repair and production of adrenal steroid hormones. Absorption of niacin occurs mainly in the jejunum, and dietary sources include chicken, beef, fish, cereal, nuts, dairy, and eggs. Severe deficiency can cause pellagra (diarrhea, dermatitis, and dementia), although dermatological and psychiatric symptoms are common in even mild deficiency [66].
A recent study found plasma vitamin B3 levels to be low in 77 % of CD patients with disease in remission [5]. However, these results need to be carefully interpreted, given that niacin status should be assessed via urinary biomarkers, as these are more reliable than plasma levels. Nevertheless, this study does suggest that niacin deficiency may be fairly prevalent in the CD population (prevalence in UC patients is not known). The recommended daily allowance of niacin is 14 mg/day for women, 16 mg/day for men, and 18 mg/day for pregnant or breast-feeding women [11]. If patients cannot meet these requirements, oral vitamin B3 at doses commonly found in standard multivitamin preparations should be encouraged.
Biotin (Vitamin B7)
Vitamin B7 (biotin) is a coenzyme in the metabolism of fatty acids and leucine, and it plays a role in gluconeogenesis. Like the other B vitamins, its absorption occurs primarily in the jejunum. Deficiency in biotin is rare and tends to present with mild symptoms. There has only been one study of biotin status in IBD patients, in which serum levels did not differ from that of healthy controls [63].
Fat-Soluble Vitamins
Vitamin A
Vitamin A actually refers to a group of related compounds which includes retinol/retinal (so-called preformed active forms of vitamin A that can only be found from animal sources, such as beef and eggs), retinoic acid (converted from retinal by the body), and the carotenoids (provitamin A compounds which are synthesized by plants and can be converted by humans into retinol). The most important of the carotenoids is β-carotene , which is found in carrots, greens, spinach, orange juice, sweet potatoes, and cantaloupe [11].
The vitamin A compound group plays an important role in vision and wound healing . Retinal is a vital structural component of the visual pigments of retinal rod and cone cells [20]. Retinoic acid plays an important role in wound healing, by augmenting the presence of macrophage and monocyte at the wound site and stimulating fibroblasts’ production of collagen [20, 67]. Vitamin A also plays an important role in reproduction as well as serving as a hormone-like growth factor for epithelial cells, participating in cellular differentiation and gene regulation [20].
Following ingestion of dietary retinol and carotenoids , these compounds are solubilized by bile salts, absorbed by enterocytes throughout the small bowel, incorporated in chylomicrons, and shuttled between the liver (main storage site, 50–80 % of stores) and to tissues such as the retina and skin. The amount of vitamin A available from dietary carotenoids depends on the efficiency of absorption (can vary between 5 and 50 %, depending on the type and source of carotenoid), the digestibility of the associated protein complex, and the level of dietary fat accompanying carotenoid intake [11, 20]. Normal vitamin A metabolism is dependent on zinc, as this mineral is necessary for the synthesis of retinol binding protein (RBP) , which transports retinol through the circulation and also is required for enzymatic reactions that activate retinol.
There have been several small studies in which mean vitamin A and β-carotene levels were found to be significantly lower in IBD patients [14, 21, 22]. These studies need to be interpreted carefully, as assessing vitamin A status can be quite complicated and serum testing does not accurately reflect body stores, as discussed further below. However, there have been also several cohort studies which suggest that the majority of IBD patients—between 36 and 90 %—have inadequate vitamin A intake with significantly lower dietary levels than the RDA (700 μg in women, 900 μg in men) [5, 6, 45].
Vitamin A deficiency remains more of a clinical diagnosis, as serum testing can be quite inaccurate and confusing. The tests available include serum retinol levels, serum retinal-binding protein, and serum carotene levels. Because most vitamin A is stored in the liver, serum retinol testing can underestimate deficiency, since retinol can be released by liver until very late stages of vitamin A deficiency. Conversely, serum retinol tests can be artificially low in the setting of severe protein-energy malnutrition (i.e., IBD patient who is cachectic or losing weight), partially because production of the retinol’s binding protein (RBP) is decreased. Serum carotene levels can vary tremendously based on recent intake of dietary vitamin A.
Despite these limitations , serum retinol levels (levels less than 20 μg/dL or a ratio of retinol:RBP (a molar ratio <0.8)) are suggestive of vitamin A deficiency [20]. However, in high-risk patients who do not meet these laboratory criteria, one should keep a high suspicion and observe for earlier clinical signs of vitamin A deficiency. This includes dry eyes (xerophthalmia) and impaired night vision (nyctalopia) from the loss of visual pigments—both can actually occur quite quickly in the setting of vitamin A deficiency. In addition, vitamin A deficiency is also associated with skin texture changes involving follicular hyperkeratosis (phrynoderma), impaired wound healing, unexplained anemia, and impaired immunocompetence (reduced numbers and mitogenic responsiveness of T lymphocytes) [20].
Vitamin A supplementation in IBD patients has not been well studied, so currently it is suggested that, in the absence of suspected deficiency, vitamin A should not be routinely recommended because of the risk of toxicity. For patients with deficiency, particularly those with visual changes, short courses of higher-dose vitamin A is usually recommended. For example, to treat xerophthalmia , ultra-high doses of 100,000 IU (20,000 μg) have been used, but these doses should only be done in conjunction with an ophthalmologists. In general, to replete deficient IBD patients, doses should be aimed at the DRI’s Tolerable Upper Limit Intake Levels (UL) of 10,000–15,000 IU (2000–3000 μg of retinol or 3000–4500 μg of carotenoid form) per day for a 1–2 week period. Once patients are started on therapy, signs of vitamin A toxicity (headache, bone pain, liver toxicity, hemorrhage) should be closely monitored [11].
In addition, another potential indication for vitamin A supplementation may be in the perioperative period after bowel surgery and/or for patients with refractory fistulas . To enhance wound healing in the acute setting, several expert groups have recommended 10,000 IU–15,000 IU/day orally or intramuscularly for 10 days [20, 68]. This may be especially beneficial for patients who are on corticosteroids or have concomitant protein malnutrition.
Vitamin D
Vitamin D is a fat-soluble vitamin that is essential for skeletal bone health and may have an important role in regulating the adaptive immune system. Several reports have demonstrated that IBD patients are at higher risk for hypovitaminosis D, with rates between 22 and 70 % for CD patients and up to 45 % in UC [68, 69]. A more detailed discussion of the vitamin D deficiency will be covered in a separate chapter.
Vitamin E
Vitamin E refers to a group of fat-soluble vitamins which play a fundamental role in protecting the body against the damaging effects of reactive oxygen species. When located in the lipid portion of cell membranes, vitamin E protects the unsaturated membrane phospholipids from oxidative degradation from highly reactive oxygen free radicals. Vitamin E includes two classes of biologically active substances: (1) the tocopherols and (2) the related but less biologically active compounds, the tocotrienols. Amongst the tocopherols, γ-tocopherol is the most common in the North American diet, found in corn oil, soybean oil, margarine, and dressings. Alpha (α-) tocopherol, the most biologically active form of vitamin E and the second most common dietary form of vitamin E, is found in sunflower and safflower oils. Vitamin E is absorbed in the duodenum via micelle-dependent diffusion. Similar to other fat-soluble vitamins, its use depends on the presence of dietary fat and sufficient biliary and pancreatic function. Vitamin E in the form of supplements is usually found in esterified forms (which can be more stable) but is absorbed only after hydrolysis by duodenal esterases [70].
In patients with evidence of fat malabsorption and/or those receiving cholestyramine treatment, risk for potential vitamin E deficiency is increased. Currently, the RDA for vitamin E is quantified in terms of α-tocopherol equivalents (α-TEs); 1 mg of α-tocopherol is defined as one α-TE. Typical recommendation for adults (both male/female) is 15 mg/day of α-tocopherol (or 15 α-TE). Clinical manifestations suggestive of vitamin E deficiency can include the neuromuscular, vascular, and reproductive systems, including impaired vibratory and position sensation, changes in balance and coordination, muscle weakness, loss of deep tendon reflexes and visual disturbances [70, 71].
There have been three studies to date looking at vitamin E status in IBD patients. The cohorts used were heterogeneous, with one only including CD patients [63] one with only UC [72] and one study which combined UC and CD patients [22]. Of these three studies, only the study of CD patients found a significantly lower serum vitamin E level, compared with controls, and this difference appeared irrespective of disease activity. Given the very scant data available on vitamin E deficiency in IBD, there are no current recommendations on monitoring and replacement of vitamin E. However, in patients with suggestive symptoms for possible deficiency, particularly CD patients with significant fat malabsorption, low-dose supplementation (15 mg/day) for a limited period may be warranted. Regular interval monitoring of vitamin E level is recommended during supplementation in order to prevent toxicity.
Vitamin K
Vitamin K is a fat-soluble vitamin that exists in two major forms: (1) phylloquinones, which are primarily synthesized by green plants and (2) menaquinones, which are derived mainly from bacteria. Dietary phylloquinones are absorbed by an energy-dependent process in the small intestine while the menaquinones are absorbed in the small intestine and colon by passive diffusion [73]. Like the other fat-soluble vitamins, absorption depends on a minimum amount of dietary fat and on bile salts and pancreatic juices. Good dietary sources of vitamin K include green vegetables (collards, spinach, salad greens, broccoli), brussel sprouts, cabbage, plant oils, and margarine. Because of a lack of data on optimal vitamin K need, the DRI does not provide an RDA but rather than “Adequate Intake” value for vitamin K (an observed mean value of what a group of “healthy persons” was noted to consume—which is 90 μg/day (women) to 120 μg (for men)) [11].
Vitamin K serves an important function in both skeletal bone health and normal blood clotting. Vitamin K is a known cofactor for posttranslational γ-carboxylation of multiple proteins, including blood coagulation factors as well as osteocalcin (OC), a regulator of bone mineral maturation [74, 75]. Osteocalcin is produced by osteoblasts and requires γ-carboxylation in order to bind calcium. Under conditions of vitamin K deficiency, OC remains uncarboxylated and is transferred into the circulation. Serum uncarboxylated osteocalcin (percent or total) reflects vitamin K status in the bone and is often used as an indirect measure of total vitamin K stores. The other method of measuring vitamin K status is serum phylloquinone levels, although levels can be influenced by recent dietary intake and triglyceride levels [75, 76]. The lack of a single reliable and direct method of vitamin K status is a principle limitation in interpretation of studies on this vitamin’s importance in bone health.
There have been several large epidemiological studies, including one that used the Nurses’ Health Study cohort and another the Framingham cohort, which demonstrate that low dietary intake of vitamin K appears to be associated with osteoporotic fracture risk and low BMD [75–77]. However, studies correlating biochemical measures of vitamin K (uncarboxylated osteocalcin level or serum phylloquinone levels) with bone disease have been less consistent, with some studies showing an association while others do not [78–80]. This likely reflects either limitations of current tests of vitamin K status, or a weak association between vitamin K status and bone disease.
In the general population, vitamin K deficiency is rare, but patients with malabsorptive disorders or who have been on chronic or frequent antibiotics may be at increased risk. Within the IBD literature, there have been relatively few studies addressing vitamin K status. The earliest study utilized abnormal prothrombin antigen assay as a surrogate measure of vitamin K status, and found that in an IBD cohort (17 CD/1 UC), 31 % were vitamin K-deficient [73]. There have been two more recent studies that measured serum uncarboxylated osteocalcin levels in CD patients and found levels to be significantly lower compared with controls [81] and with UC patients [82, 83]. Although these studies were too small to perform subgroup analysis, there was a suggestion that vitamin K deficiency was more common in patients with active inflammation and more extensive small bowel involvement, suggesting malabsorption as a potential mechanism. There have been multiple studies showing that dietary intake of vitamin K is also significantly lower in IBD patients, even in patients with disease remission, compared with controls [9, 81].
While in older adults, low intake of vitamin K has been associated with increased incidence of hip fractures, currently there does not appear to be sufficient evidence to support the use of vitamin K supplements in IBD patients as a means to prevent or treat bone disease. While there have been no trials performed in the IBD population, there have been four randomized controlled trials of phylloquinone supplementation in elderly women and healthy controls. None of these showed increased BMD in >1 skeletal site [84–86]. There have been a few positive studies from Japan, in which menaquinone-4 (a different form of vitamin K, naturally present in natto, a fermented soybean product common in Japan) at doses of 45 mg/day appeared to be more effective at improving BMD and decreased fracture risk [87, 88]. However, these studies lacked sufficient sample size and many were not placebo-controlled, so further prospective studies need to be performed.
In summary, there is evidence that inadequate dietary vitamin K may increase risk of bone disease, although this may not be adequately reflected in current measurements of vitamin K. Because of malabsorption and dietary restrictions, IBD patients may be at risk for vitamin K deficiency. There is limited evidence suggesting vitamin K deficiency may contribute to bone disease, especially in those with normal vitamin D status, although currently there is insufficient evidence to recommend oral vitamin K supplements. Rather, since vitamin K is found in large amounts in green leafy vegetables (typically at levels greater than 100 μg/100 g), increased dietary intake should be encouraged in all patients to improve bone health.
Vitamin C
Vitamin C, also known as ascorbic acid or L-ascorbic acid, is an important antioxidant in multiple tissues and also serves as a cofactor in multiple enzymatic reactions, including collagen synthesis. With respect to wound healing, vitamin C is also important, as it supports angiogenesis and regulates neutrophil activity [23].
Vitamin C cannot be synthesized intrinsically due to lack of the enzyme L-gulonolactone oxidase in humans. The RDA for vitamin C intake is 75 mg for women and 90 mg for men. Fruits and vegetables are the best dietary sources of vitamin C, particularly citrus fruits, tomatoes, and potatoes. Vitamin C is absorbed from the diet in the jejunum by active transport and passive diffusion. Once absorbed, vitamin C is concentrated primarily in its oxidized form (dehydroascorbic acid) in many vital organs, including the adrenals, brain, and eye [11].
In the general population, significant vitamin C deficiency is rare. Severe vitamin C deficiencies can result in clinical scurvy, which is characterized by bleeding gums, hemarthroses, and poor wound healing. Less severe deficiency, as measured by subnormal serum vitamin C levels, have been reported to be relatively common in IBD [21, 22]. This is most likely due to low dietary intake, which has been shown in several IBD cohort studies to be quite common [5, 15].
Vitamin C status is typically assessed by measuring plasma vitamin C levels. Other measures, such as leukocyte vitamin C concentration, could be more accurate indicators of tissue vitamin C levels, but are not yet readily available in commercial laboratories [89]. Vitamin C deficiency should also be suspected in patients with easy bruising, gingival bleeding, and enlargement and hyperkeratosis of the hair follicles. In IBD patients with vitamin C deficiency, higher dose of supplementation at 100–200 mg/day may be needed. Higher-dose vitamin C may also be helpful for those with acute wound healing needs, including fistulas or recent surgery [23]. One special consideration should be made for IBD patients who are smokers. Because of the lower concentrations of ascorbic acid in this population, it has been recommended that smokers increase their intake by an additional 35 mg/day.
Macrominerals
Calcium
Calcium is the most abundant mineral in the human body, with average body stores of 1–2 kg, 99 % of which is in the skeleton and teeth. Serum calcium level is maintained within a narrow range of 8.8–10.8 mg/dL, of which the ionized calcium concentrations range from 4.4 to 5.2 mg/dL, since both hypocalcemia and hypercalcemia have significant physiologic effects. Extracellular calcium is normally regulated in a narrow range by the combined actions of calcitonin and parathyroid hormone, which in turn regulates the activity of the vitamin D system, the main inducer of active calcium absorption in the intestine [90].
Intestinal absorption of calcium primarily occurs in the duodenum and proximal jejunum. Calcium absorption occurs by two mechanisms: (1) an unregulated paracellular route, which largely depends on dietary intake and luminal calcium concentration and (2) an active intracellular route via calcium channels, the transcription of which is dependent on vitamin-1,25OH D (1,25-OHD). In addition, calcium is secreted in the distal small bowel (distal jejunum and ileum) as well as in the colon by unclear mechanisms. Intestinal calcium losses are likely aggravated by diarrhea and malabsorption, although the extent has not been well studied [90].
Surprisingly little is known about the extent to which active small bowel inflammation can directly affect calcium absorption and impact risk for osteoporosis. This is difficult to study, given that calcium absorption is interdependent on vitamin D, a micronutrient which is insufficient in a large proportion of IBD patients, as discussed elsewhere. Further, calcium malabsorption is known to be exacerbated by magnesium deficiency (can occur with diarrhea) and glucocorticoids, which causes decreased absorption of calcium from both the intestine and kidney. In addition to malabsorption, several studies have demonstrated that as many as 80–86 % of IBD patients have inadequate daily dietary calcium intake [5, 15]. This is not surprising, since avoidance of milk and other dairy products is quite common in IBD patients, due to rates of concomitant lactose intolerance of 70–90 % [90].
Adequate calcium intake is recommended in most patients with IBD, at doses of 1000–1500 mg/day (1000 mg for women age 25 until menopause and men <65 years old; 1300 mg for women between 18 and 25 years; 1500 mg for postmenopausal women, and men >65 years old). For patients unable to tolerate dairy products, dark green leafy vegetables such as kale, collards, turnip greens, and broccoli as well as almonds, sardines, and canned salmon are recommended. For IBD patients unable to meet dietary calcium goals, calcium supplements are widely available.
There have been relatively few studies evaluating the efficacy of calcium alone or combined with vitamin D supplementation. However, from two observational cohorts, it did appear that calcium at doses of 1000 mg with nontreatment doses of vitamin D may have resulted in a slight improvement in BMD after 1 year, although no change in the incidence of fractures was seen [91]. In general, however, calcium supplementation alone is probably not sufficient to prevent bone loss in IBD patients, especially those with significant glucocorticoid exposure [92, 93], so bisphosphonate medications may be needed for clinically significant bone loss.
Magnesium
Magnesium is the fourth most abundant cation in the body and plays a fundamental role in most cellular reactions, mainly as a cofactor in enzymatic reactions involving ATP. In addition, 50–60 % of the body’s magnesium is incorporated in the hydroxyapatite crystal of bone and may be important in bone cell activity. The efficiency of absorption of magnesium ranges from 35 to 45 %, typically absorbed along the length of the small intestine, particularly in the jejunum. Once in circulation, approximately half the magnesium in plasma is free; approximately one-third is bound to albumin while the rest is complexed with citrate, phosphate, or other anions. Homeostasis of magnesium homeostasis is regulated by intestinal absorption and renal excretion [94].
There have been several epidemiological studies suggesting that dietary magnesium and hypomagnesemia may be weakly associated with osteoporosis [94, 95]. The mechanisms for magnesium deficiency on bone disease are not clear. In cell culture and animal models, magnesium has a mitogenic role on osteoblasts and deficiency of this cation leads to a decrease in osteoblastic activity. Likely more important, however, is the influence that magnesium balance has on calcium homeostasis. Magnesium deficiency is known to induce hypocalcemia, via impaired parathyroid gland function and inappropriately low PTH levels, which leads to lower intestinal calcium absorption [95]. Hypokalemia is also commonly observed in hypomagnesemic patients, occurring in 40–60 % of cases [96]. This is likely due to underlying disorders that cause both magnesium and potassium loss, such as diarrhea or malabsorption.
Magnesium deficiency is a growing problem in the Western world, with 32 % of Americans failing to meet US recommended daily allowance (RDA) [97]. IBD patients appear to be at increased risk of magnesium deficiency, with rates reported in 13–88 % of patients [98, 99]. Deficiency is likely due to a combination of decreased dietary intake [9, 99], losses from chronic diarrhea and fistula output [98], and malabsorption [98]. Clinical manifestation of magnesium deficiency includes neuromuscular hyperexcitability such as tremor and weakness, cardiovascular manifestations including widening of the QRS, and other mineral and hormone imbalance hypocalcemia, hypokalemia, and hypoparathyroidism.
Magnesium status is generally assessed by random serum magnesium levels, although these levels do not accurately reflect total body stores of magnesium as they may remain constant despite a wide range of intake levels. Leukocyte magnesium content is a much more sensitive test of nutritional status. Alternatively, 24-h urinary magnesium is quite accurate in determining total body stores, though burdensome for patients to complete. Magnesium screening and supplementation should be considered in all patients with significant diarrhea (>300 g/day), while diarrheal symptoms are active [97].
For patient with minimal food restriction, good dietary sources include seeds, nuts, legumes, and milled cereal grains, as well as dark green vegetables. For IBD patient requiring supplementation, most oral magnesium formulations can exacerbate diarrhea, although magnesium heptogluconate (Magnesium-Rougier) or magnesium pyroglutamate (Mag 2) may be better tolerated, especially if mixed with oral rehydration solution and sipped throughout the day oral magnesium (Magnesium-Rougier) or magnesium pyroglutamate (Mag 2) may be better tolerated, especially if mixed with oral rehydration solution and sipped throughout the day. The total dose of elemental magnesium required to ensure normal serum magnesium varies between 5 and 20 mmol/day [100].
Iron
Iron deficiency is the leading cause of anemia in the IBD population, present in 36–90 % of patients [101, 102]. The clinical significance, diagnosis, and treatment of iron deficiency in IBD cohorts are discussed elsewhere in a separate chapter.
Trace Elements
Zinc
Zinc is an abundant trace mineral widely distributed in different organs, with high concentrations in the kidney, liver, muscle, bone, pancreas, hair, and skin. Zinc is an essential mineral, required for catalytic activity of ≈100 enzymes, including metalloproteinases, and is also important in immune function, protein and collagen synthesis, and wound healing. Zinc is absorbed along the length of the small intestine by a poorly characterized transport mechanism [103]. Typically, good dietary sources of zinc can be found in meats, poultry, and milk. In addition, since many breads and cereal-based products are currently fortified with zinc, zinc deficiency is not common in the general population.
Zinc deficiency is thought to be relatively common in patients with chronic diarrhea, malabsorption, and hypermetabolic states. In IBD patients, a number of studies have reported low plasma zinc levels in IBD patients [5, 15]. These results are difficult to interpret, given that very little zinc is present in the serum, so this is likely a poor measure of zinc status. There have been several historical studies reporting that clinical symptoms of zinc deficiency (acrodermatitis, poor taste acuity) were not uncommon especially in CD [2], although more recent assessments of the incidence of subclinical zinc deficiency among IBD cohorts are not well characterized. Clinicians should also observe for other signs of possible zinc deficiency—including mild anemia, hair and skin changes, hypogeusia, and poor wound healing [103].
The current RDA recommendation for zinc intake is 11 mg/day for men and 8 mg/day for women. It has been suggested that for patients with significant diarrhea (>300 g of stool/day), additional zinc supplementation is reasonable with 25–50 mg of elemental zinc [103]. Unless patients have severe ongoing diarrhea, such doses should not be given for longer than 2–3 weeks as excess zinc can interfere with iron and copper absorption and can lead to deficiency of these important minerals.
To enhance wound healing, zinc supplementation of 40 mg of elemental zinc (176 mg zinc sulfate) for 10 days has been suggested [23, 103]. Zinc comes in two major forms: zinc sulfate (contains 23 % elemental zinc, so that 220 mg zinc sulfate contains 50 mg elemental zinc) and zinc gluconate (contains 14.3 % elemental zinc; 10 mg zinc gluconate contains 1.43 mg elemental zinc). One must also be careful to monitor calcium and folic acid consumption with zinc, since high intake calcium or folic acid can reduce zinc absorption. Conversely, high doses of zinc can impair absorption of iron from ferrous sulfate if a patient is also concomitantly being treated for iron deficiency anemia.
Selenium
Selenium is a necessary component of vital enzymes with antioxidant function, including glutathione peroxidase and thioredoxin reductase. In animal models, selenium has been associated with reduced risk of cancer, including colorectal cancer [104, 105], although human epidemiological data are mixed [106].
A narrow dietary intake range exists for selenium; current RDA is 55 μg/day for both men and women. Seafoods and organ meats are the richest food sources of selenium. Other sources include muscle meats, cereals and other grains, and dairy products. With prolonged low intake of selenium, symptoms associated with deficiency can manifest in form of joint pain in mild disease, and cardiomyopathy when severe. Minimal dietary intake of approximately 40 μg of selenium per day seems to be necessary to maintain glutathione peroxidase (GSH-Px), an enzyme containing selenium [105].
Absorption of selenium is poorly understood, but is believed to occur most avidly in the ileum, followed by the jejunum and large intestine. There have been five studies to date, in which selenium levels were found to be significantly lower in both UC and CD patients, compared with controls [25–27]. This observation was seen irrespective of disease activity and/or location. The exact prevalence of true selenium deficiency was not obtainable from these studies, as most only reported mean selenium levels, which can vary widely without accurately reflecting true body selenium storage.
More recently, it has been suggested that selenium status may be better assessed by measuring selenium or GSH-Px in serum, platelets, and erythrocytes and/or in whole blood. Erythrocyte selenium measurement is an indicator of long-term intake. Since no studies have yet to assess these new biomarkers, currently there is no evidence to support checking for or repleting selenium deficiency in IBD patients. The exception to this is in patients on long-term total parenteral nutrition (TPN). Selenium is now routinely added to TPN, often in premixed commercial trace element concentrates (often also including zinc, copper, manganese, and chromium). Updated guidelines from the American Society of Parenteral or Enteral Nutrition (A.S.P.E.N.) recommend that 20–60 μg daily be supplemented in TPN.
Copper
Copper is a trace element that has diverse roles in biological electron transport and oxygen transportation. Because of large stores of copper in the liver, muscle, and bone, deficiency is relatively rare. Copper absorption is tightly controlled, with absorption occurring in the small intestine. Entry at the mucosal surface is by facilitated diffusion, and exit across the basolateral membrane is primarily by active transport [26].
There have been several small studies that have addressed copper status in IBD patients, with equivocal results. While a recent study of CD patients in remission reported that serum copper was found to be low in up to 84 % of patients [5], two other studies have failed to show this. In several studies of UC patients, serum copper was found to be similar to controls in one study, and elevated in UC patients in two studies [27]. However, one must be careful in interpreting these results. Since copper does not exist as a free ion in the body, 90 % of the copper in serum is incorporated into ceruloplasmin, a functional enzyme at the erythrocyte-forming cells of the bone marrow. The remaining 10 % of copper is bound loosely to albumin. This highlights the limitation of serum copper and ceruloplasmin in determining body copper stores, as both may also be acute phase reactants. Serum copper may also be falsely decreased with certain renal diseases, with prolonged inflammation, and due to increased iron or zinc intake [106].
An RDA of 900 μg/day of copper is recommended for adults of both genders. Copper is widely available in animal products, including organ and muscle meats, chocolate, nuts, and cereal grains. Fruits and vegetables contain little copper. Currently , there are no recommended screening or supplementation guidelines for copper, other than in TPN. Guidelines from A.S.P.E.N. recommend that 0.3–0.5 mg daily be supplemented in TPN. Copper is normally excreted in bile, so lower doses should be utilized in patients with cholestasis (i.e., PSC with elevated bilirubin).
Chromium
Chromium is a trace mineral with function including potentiation of insulin action and regulation of lipid and protein metabolism. Chromium potentiates insulin action and influences carbohydrate, lipid, and protein metabolism. Chromium can exist in several valency states, with trivalent chromium being the only biologically active form and an important regulator of insulin action. As with other minerals, organic and inorganic forms of chromium are absorbed differently. Less than 2 % of the trivalent chromium consumed is absorbed [11]. In animal studies, chromium absorption was shown to be increased by oxalate intake and is higher in iron-deficient animals than in animals with adequate iron, suggesting that it shares some similarities with the iron absorption pathway.
Chromium deficiency is rare and has been reported mainly in patients on long-term TPN who presented with glucose intolerance and neuropathy, both of which were reversed with addition of chromium to TPN. Currently, A.S.P.E.N. recommends 10–15 g of chromium is added daily to TPN.
Manganese
Manganese is an essential trace element required as a catalytic cofactor for multiple enzymatic reactions. Manganese is absorbed throughout the small intestine, with iron competing for common binding sites for absorption. Good food sources include whole grains, legumes, nuts, and tea [11].
There have been virtually no cases of clinically significant manganese deficiency reported in the literature, so assessing manganese status is not necessary for IBD patients. The only exception to this is in patients on long-term TPN, in which manganese toxicity is an increasingly important problem. This is especially problematic in patients with chronic liver disease and/or cholestasis, as manganese is primarily excreted in bile. Manganese toxicity is associated with liver injury as well as neurotoxicity. The 2004 guidelines put forth by A.S.P.E.N. recommended lower doses of manganese (0.04–0.1 mg) than previous guidelines. However, there have been several studies demonstrating that even at these lower doses, whole-blood manganese levels was elevated in 82–93 % of long-term TPN patients. This may be due to the fact that most TPN formulas contain high levels of manganese contaminants and commercial trace element mixtures contain excessive manganese.
Conclusions
IBD has classically been associated with malnutrition and weight loss, although this has become less common with advances in treatment and greater proportions of patients attaining clinical remission. However, micronutrient deficiencies are still relatively common, particularly in CD patients with active small bowel disease and/or multiple resections.
Micronutrient deficiencies are associated with several important extraintestinal complications of IBD. Anemia is the most common of these complications, and can be due to iron, vitamin B12, folate, zinc, or vitamin A deficiencies. Abnormal bone metabolism, manifesting as osteopenia or osteoporosis, can be due to inadequate intake of calcium, vitamin D, magnesium, and possibly vitamin K and vitamin B12. IBD patients have an increased incidence of venous thromboembolism, which may be due at least partly to hyperhomocysteinemic states induced by folate, vitamin B12, or pyridoxine deficiencies.
The goal of advancing nutritional therapy in IBD is to recognize and treat these complications earlier, so as to decrease morbidity and prevent long-term sequelae. Unfortunately, there are no guidelines about the timing and frequency we should be assessing micronutrient status in IBD patients. Clearly, in the presence of clinical symptoms , evaluating micronutrient status and treating deficiencies is indicated (Tables 5.4 and 5.5).
In certain high-risk populations, it may make sense to empirically supplement for a specific time period, as there is some evidence that doing so can improve outcomes or prevent complications.
Some of the more common situations are listed below (Table 5.6):
Finally, in lower-risk patients (mild disease, in remission), recommendations for nutritional screening is even less clear. However, based on the current literature it does appear that certain micronutrients may still be commonly deficient in patients in remission , we generally recommend (Table 5.7).
While nutrition is one of the most common concerns of patients with IBD, the literature remains inadequate with respect to clear guidelines for micronutrient monitoring and supplementation. The above recommendations are based on currently available data. These will likely change over time based on ongoing studies, but currently can serve as a useful tool for clinicians to apply in their practice.
References
Mekhjian HS, Switz DM, Melnyk CS, et al. Clinical features and natural history of Crohn’s disease. Gastroenterology. 1979;77(4):898–906.
Harries AD, Heatley RV. Nutritional disturbances in Crohn’s disease. Postgrad Med J. 1983;59:690–7.
Dawson AM. Nutritional disturbances in Crohn’s disease. Br J Surg. 1972;59:817–9.
Dawson AM. Nutritional disturbances in Crohn’s disease. Proc R Soc Med. 1971;64:166–70.
Filippi J, Al-Jaouni R, Wiroth JB, et al. Nutritional deficiencies in patients with Crohn’s disease in remission. Inflamm Bowel Dis. 2006;12:185–91.
Aghdassi E, Wendland BE, Stapleton M, et al. Adequacy of nutritional intake in a Canadian population of patients with Crohn’s disease. J Am Diet Assoc. 2007;107:1575–80.
Jahnsen J, Falch JA, Mowinckel P, et al. Body composition in patients with inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2003;98:1556–62.
Valentini L, Schaper L, Buning C, et al. Malnutrition and impaired muscle strength in patients with Crohn’s disease and ulcerative colitis in remission. Nutrition. 2008;24:694–702.
Sousa Guerreiro C, Cravo M, Costa AR, et al. A comprehensive approach to evaluate nutritional status in Crohn’s patients in the era of biologic therapy: a case-control study. Am J Gastroenterol. 2007;102:2551–6.
Hass DJ, Brensinger CM, Lewis JD, et al. The impact of increased body mass index on the clinical course of Crohn’s disease. Clin Gastroenterol Hepatol. 2006;4:482–8.
Institute of Medicine of the National Academy of Sciences, Food and Nutrition Board. Dietary reference intakes: the essential guide to nutrient requirements. Washington, DC: National Academies Press; 2006. p. 542.
Institute of Medicine of the National Academy of Sciences, Food and Nutrition Board. Dietary reference intakes for calcium and vitamin D. Washington, DC: National Academies Press; 2006. p. 1116.
Wallace TC, McBurney M, Fulgoni III VL. Multivitamin/mineral supplement contribution to micronutrient intakes in the United States, 2007–2010. J Am Coll Nutr. 2014;33(2):94–102.
Braegger CP, MacDonald TT. Immune mechanisms in chronic inflammatory bowel disease. Ann Allergy. 1994;72(2):135–41.
Vagianos K, Bernstein CN. Homocysteinemia and B vitamin status among adult patients with inflammatory bowel disease: a one-year prospective follow-up study. Inflamm Bowel Dis. 2012;18(4):718–24.
Weiss G, Gasche C. Pathogenesis and treatment of anemia in inflammatory bowel disease. Haematologica. 2010;95:175–8.
Duerksen DR, Fallows G, Bernstein CN. Vitamin B12 malabsorption in patients with limited ileal resection. Nutrition. 2006;22:1210–3.
Hoffbrand AV, Stewart JS, Booth CC, et al. Folate deficiency in Crohn’s disease: incidence, pathogenesis, and treatment. Br Med J. 1968;2:71–5.
Van Gossum A, Cabre E, Hebuterne X, et al. ESPEN guidelines on parenteral nutrition: gastroenterology. Clin Nutr. 2009;28:415–27.
D’Ambrosio DN, Clugston RD, Blaner WS. Vitamin A metabolism: an update. Nutrients. 2011;3(1):63–103.
D’Odorico A, Bortolan S, Cardin R, et al. Reduced plasma antioxidant concentrations and increased oxidative DNA damage in inflammatory bowel disease. Scand J Gastroenterol. 2001;36:1289–94.
Hengstermann S, Valentini L, Schaper L, et al. Altered status of anti-oxidant vitamins and fatty acids in patients with inactive inflammatory bowel disease. Clin Nutr. 2008;27:571–8.
Sinno S, Lee DS, Khachemoune A. Vitamins and cutaneous wound healing. J Wound Care. 2011;20:287–93.
Hodges P, Gee M, Grace M, et al. Vitamin and iron intake in patients with Crohn’s disease. J Am Diet Assoc. 1984;84:52–8.
Sturniolo GC, Mestriner C, Lecis PE, et al. Altered plasma and mucosal concentrations of trace elements and antioxidants in active ulcerative colitis. Scand J Gastroenterol. 1998;33:644–9.
Ringstad J, Kildebo S, Thomassen Y. Serum selenium, copper, and zinc concentrations in Crohn’s disease and ulcerative colitis. Scand J Gastroenterol. 1993;28:605–8.
Fernandez-Banares F, Mingorance MD, Esteve M, et al. Serum zinc, copper, and selenium levels in inflammatory bowel disease: effect of total enteral nutrition on trace element status. Am J Gastroenterol. 1990;85:1584–9.
den Heijer M, Rosendaal FR, Blom HJ, et al. Hyperhomocysteinemia and venous thrombosis: a meta-analysis. Thromb Haemost. 1998;80:874–7.
Cleophas TJ, Hornstra N, van Hoogstraten B, et al. Homocysteine, a risk factor for coronary artery disease or not? A meta-analysis. Am J Cardiol. 2000;86:1005–9.
Cattaneo M, Vecchi M, Zighetti ML, et al. High prevalence of hyperchomocysteinemia in patients with inflammatory bowel disease: a pathogenic link with thromboembolic complications? Thromb Haemost. 1998;80:542–5.
Mahmood A, Needham J, Prosser J, et al. Prevalence of hyperhomocysteinaemia, activated protein C resistance and prothrombin gene mutation in inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2005;17:739–44.
Papa A, De Stefano V, Danese S, et al. Hyperhomocysteinemia and prevalence of polymorphisms of homocysteine metabolism-related enzymes in patients with inflammatory bowel disease. Am J Gastroenterol. 2001;96:2677–82.
Romagnuolo J, Fedorak RN, Dias VC, et al. Hyperhomocysteinemia and inflammatory bowel disease: prevalence and predictors in a cross-sectional study. Am J Gastroenterol. 2001;96:2143–9.
Biasco G, Zannoni U, Paganelli GM, et al. Folic acid supplementation and cell kinetics of rectal mucosa in patients with ulcerative colitis. Cancer Epidemiol Biomarkers Prev. 1997;6(6):469–71.
Giovannucci E, Rimm EB, Ascherio A, et al. Alcohol, low-methionine–low-folate diets, and risk of colon cancer in men. J Natl Cancer Inst. 1995;87:265–73.
Konings EJ, Goldbohm RA, Brants HA, et al. Intake of dietary folate vitamins and risk of colorectal carcinoma: results from the Netherlands cohort study. Cancer. 2002;95:1421–33.
Meyer F, White E. Alcohol and nutrients in relation to colon cancer in middle-aged adults. Am J Epidemiol. 1993;138:225–36.
Su LJ, Arab L. Nutritional status of folate and colon cancer risk: evidence from NHANES I epidemiologic follow-up study. Ann Epidemiol. 2001;11:65–72.
Lashner BA. Red blood cell folate is associated with the development of dysplasia and cancer in ulcerative colitis. J Cancer Res Clin Oncol. 1993;119:549–54.
Lashner BA, Heidenreich PA, Su GL, et al. Effect of folate supplementation on the incidence of dysplasia and cancer in chronic ulcerative colitis. A case-control study. Gastroenterology. 1989;97:255–9.
Lashner BA, Provencher KS, Seidner DL, et al. The effect of folic acid supplementation on the risk for cancer or dysplasia in ulcerative colitis. Gastroenterology. 1997;112:29–32.
Honein MA, Paulozzi LJ, Mathews TJ, et al. Impact of folic acid fortification of the US food supply on the occurrence of neural tube defects. JAMA. 2001;285:2981–6.
Yakut M, Ustun Y, Kabacam G, et al. Serum vitamin B12 and folate status in patients with inflammatory bowel diseases. Eur J Intern Med. 2010;21:320–3.
Fernandez-Banares F, Abad-Lacruz A, Xiol X, et al. Vitamin status in patients with inflammatory bowel disease. Am J Gastroenterol. 1989;84:744–8.
Vagianos K, Bector S, McConnell J, et al. Nutrition assessment of patients with inflammatory bowel disease. JPEN J Parenter Enteral Nutr. 2007;31:311–9.
Lindenbaum J. Drugs and vitamin B12 and folate metabolism. Curr Concepts Nutr. 1983;12:73–87.
McNulty H, Scott JM. Intake and status of folate and related B-vitamins: considerations and challenges in achieving optimal status. Br J Nutr. 2008;99 Suppl 3:S48–54.
Tominaga M, Iida M, Aoyagi K, Kohrogi N, Matsui T, Fujishima M. Red cell folate concentrations in patients with Crohn’s disease on parenteral nutrition. Postgrad Med J. 1989;65(769):818–20.
Schernhammer ES, Ogino S, Fuchs CS. Folate and vitamin B6 intake and risk of colon cancer in relation to p53 expression. Gastroenterology. 2008;135:770–80.
Baars JE, Looman CW, Steyerberg EW, et al. The risk of inflammatory bowel disease-related colorectal carcinoma is limited: results from a nationwide nested case-control study. Am J Gastroenterol. 2011;106(2):319–28.
Subramanian V, Logan RF. Chemoprevention of colorectal cancer in inflammatory bowel disease. Best Pract Res Clin Gastroenterol. 2011;25(4–5):593–606.
Dhonukshe-Rutten RA, Lips M, de Jong N, Chin A, Paw MJ. Vitamin B-12 status is associated with bone mineral content and bone mineral density in frail elderly women but not in men. J Nutr. 2003;133(3):801–7.
Merriman NA, Putt ME, Metz DC, Yang YX. Hip fracture risk in patients with a diagnosis of pernicious anemia. Gastroenterology. 2010;138(4):1330–7.
Carmel R, Lau KH, Baylink DJ, Saxena S, Singer FR. Cobalamin and osteoblast-specific proteins. N Engl J Med. 1988;319(2):70–5.
Carmel R. Subtle and atypical cobalamin deficiency states. Am J Hematol. 1990;34:108–14.
Headstrom PD, Rulyak SJ, Lee SD. Prevalence of and risk factors for vitamin B12 deficiency in patients with Crohn’s disease. Inflamm Bowel Dis. 2008;14:217–23.
Coull DB, Tait RC, Anderson JH, et al. Vitamin B12 deficiency following restorative proctocolectomy. Colorectal Dis. 2007;9:562–6.
Lenz K. The effect of the site of lesion and extent of resection on duodenal bile acid concentration and vitamin B12 absorption in Crohn’s disease. Scand J Gastroenterol. 1975;10:241–8.
Thompson WG, Wrathell E. The relation between ileal resection and vitamin B12 absorption. Can J Surg. 1977;20:461–4.
Vidal-Alaball J, Butler CC, Cannings-John R, et al. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency. Cochrane Database Syst Rev. 2005;(3):CD004655.
Friso S, Jacques PF, Wilson PW, Rosenberg IH, Selhub J. Low circulating vitamin B(6) is associated with elevation of the inflammation marker C-reactive protein independently of plasma homocysteine levels. Circulation. 2001;103(23):2788–91.
Morris MS, Picciano MF, Jacques PF, Selhub J. Plasma pyridoxal 5′-phosphate in the US population: the National Health and Nutrition Examination Survey, 2003–2004. Am J Clin Nutr. 2008;87(5):1446–54.
Kuroki F, Iida M, Tominaga M, et al. Multiple vitamin status in Crohn’s disease. Correlation with disease activity. Dig Dis Sci. 1993;38:1614–8.
Saibeni S, Cattaneo M, Vecchi M, et al. Low vitamin B6 plasma levels, a risk factor for thrombosis, in inflammatory bowel disease: role of inflammation and correlation with acute phase reactants. Am J Gastroenterol. 2003;98:112–7.
Costantini AI, Pala MI. Thiamine and fatigue in inflammatory bowel diseases: an open-label pilot study. J Altern Complement Med. 2013;19(8):704–8.
Crook MA. The importance of recognizing pellagra (niacin deficiency) as it still occurs. Nutrition. 2014;30(6):729–30.
Anstead GM. Steroids, retinoids, and wound healing. Adv Wound Care. 1998;11:277–85.
Sentongo TA, Semaeo EJ, Stettler N, et al. Vitamin D status in children, adolescents, and young adults with Crohn disease. Am J Clin Nutr. 2002;76:1077–81.
Leslie WD, Miller N, Rogala L, et al. Vitamin D status and bone density in recently diagnosed inflammatory bowel disease: the Manitoba IBD cohort study. Am J Gastroenterol. 2008;103:1451–9.
Herrera E, Barbas CJ. Vitamin E: action, metabolism and perspectives. Physiol Biochem. 2001;57(1):43–56.
Sokol RJ. Antioxidant defenses in metal-induced liver damage. Semin Liver Dis. 1996;16(1):39–47.
Ramakrishna BS, Varghese R, Jayakumar S, et al. Circulating antioxidants in ulcerative colitis and their relationship to disease severity and activity. J Gastroenterol Hepatol. 1997;12:490–4.
Krasinski SD, Russell RM, Furie BC, et al. The prevalence of vitamin K deficiency in chronic gastrointestinal disorders. Am J Clin Nutr. 1985;41:639–43.
Booth SL, Broe KE, Gagnon DR, Tucker KL, Hannan MT, McLean RR, et al. Vitamin K intake and bone mineral density in women and men. Am J Clin Nutr. 2003;77:512–6.
Macdonald HM, McGuigan FE, Lanham-New SA, Fraser WD, Ralston SH, Reid DM. Vitamin K1 intake is associated with higher bone mineral density and reduced bone resorption in early postmenopausal Scottish women: no evidence of gene-nutrient interaction with apolipoprotein E polymorphisms. Am J Clin Nutr. 2008;87:1513–20.
Booth SL, Broe KE, Peterson JW, Cheng DM, Dawson-Hughes B, Gundberg CM, et al. Associations between vitamin K biochemical measures and bone mineral density in men and women. J Clin Endocrinol Metab. 2004;89:4904–9.
Feskanich D, Weber P, Willett WC, Rockett H, Booth SL, Colditz GA. Vitamin K intake and hip fractures in women: a prospective study. Am J Clin Nutr. 1999;69:74–9.
Luukinen H, Kakonen SM, Pettersson K, et al. Strong prediction of fractures among older adults by the ratio of carboxylated to total serum osteocalcin. J Bone Miner Res. 2000;15:2473–8.
Szulc P, Arlot M, Chapuy MC, et al. Serum undercarboxylated osteocalcin correlates with hip bone mineral density in elderly women. J Bone Miner Res. 1994;9:1591–5.
Kawana K, Takahashi M, Hoshino H, et al. Circulating levels of vitamin K1, menaquinone-4, and menaquinone-7 in healthy elderly Japanese women and patients with vertebral fractures and patients with hip fractures. Endocr Res. 2001;27:337–43.
Duggan P, O’Brien M, Kiely M, et al. Vitamin K status in patients with Crohn’s disease and relationship to bone turnover. Am J Gastroenterol. 2004;99:2178–85.
Kuwabara A, Tanaka K, Tsugawa N, et al. High prevalence of vitamin K and D deficiency and decreased BMD in inflammatory bowel disease. Osteoporos Int. 2009;20:935–9342.
Nakajima S, Iijima H, Egawa S, et al. Association of vitamin K deficiency with bone metabolism and clinical disease activity in inflammatory bowel disease. Nutrition. 2011;27:1023–8.
Fang Y, Hu C, Tao X, et al. Effect of vitamin K on bone mineral density: a meta-analysis of randomized controlled trials. J Bone Miner Metab. 2011;30:60–8.
Braam LA, Knapen MH, Geusens P, et al. Vitamin K1 supplementation retards bone loss in postmenopausal women between 50 and 60 years of age. Calcif Tissue Int. 2003;73:21–6.
Bolton-Smith C, McMurdo ME, Paterson CR, et al. Two-year randomized controlled trial of vitamin K1 (phylloquinone) and vitamin D3 plus calcium on the bone health of older women. J Bone Miner Res. 2007;22:509–19.
Shiraki M, Shiraki Y, Aoki C, et al. Vitamin K2 (menatetrenone) effectively prevents fractures and sustains lumbar bone mineral density in osteoporosis. J Bone Miner Res. 2000;15:515–21.
Iwamoto J, Matsumoto H, Takeda T. Efficacy of menatetrenone (vitamin K2) against non-vertebral and hip fractures in patients with neurological diseases: meta-analysis of three randomized, controlled trials. Clin Drug Investig. 2009;29:471–9.
Jacob RA, Sotoudeh G. Vitamin C function and status in chronic disease. Nutr Clin Care. 2002;5(2):66–74.
Bronner F. Mechanisms of intestinal calcium absorption. J Cell Biochem. 2003;88:387–93.
Shea B, Wells G, Cranney A, et al. Meta-analyses of therapies for postmenopausal osteoporosis. VII. Meta-analysis of calcium supplementation for the prevention of postmenopausal osteoporosis. Endocr Rev. 2002;23:552–9.
Bernstein CN, Seeger LL, Anton PA, et al. A randomized, placebo-controlled trial of calcium supplementation for decreased bone density in corticosteroid-using patients with inflammatory bowel disease: a pilot study. Aliment Pharmacol Ther. 1996;10:777–86.
von Tirpitz C, Klaus J, Steinkamp M, et al. Therapy of osteoporosis in patients with Crohn’s disease: a randomized study comparing sodium fluoride and ibandronate. Aliment Pharmacol Ther. 2003;17:807–16.
Reginster JY, Strause L, Deroisy R, et al. Preliminary report of decreased serum magnesium in postmenopausal osteoporosis. Magnesium. 1989;8:106–9.
Rude RK, Gruber HE. Magnesium deficiency and osteoporosis: animal and human observations. J Nutr Biochem. 2004;15:710–6.
Whang R, Ryder KW. Frequency of hypomagnesemia and hypermagnesemia. Requested vs routine. JAMA. 1990;263(22):3063–4.
Krebs-Smith SM, Cleveland LE, Ballard-Barbash R, et al. Characterizing food intake patterns of American adults. Am J Clin Nutr. 1997;65(4 Suppl):1264S–8.
Hessov I. Magnesium deficiency in Crohn’s disease. Clin Nutr. 1990;9:297–8.
Galland L. Magnesium and inflammatory bowel disease. Magnesium. 1988;7:78–83.
Jeejeebhoy KN. Clinical nutrition: management of nutritional problems of patients with Crohn’s disease. CMAJ. 2002;166:913–8.
Gasche C, Lomer MC, Cavill I, et al. Iron, anaemia, and inflammatory bowel diseases. Gut. 2004;53:1190–7.
Kulnigg S, Gasche C. Systematic review: managing anaemia in Crohn’s disease. Aliment Pharmacol Ther. 2006;24:1507–23.
Lansdown AB, Mirastschijski U, Stubbs N, et al. Zinc in wound healing: theoretical, experimental, and clinical aspects. Wound Repair Regen. 2007;15:2–16.
Finley JW, Davis CD, Feng Y. Selenium from high selenium broccoli protects rats from colon cancer. J Nutr. 2000;130:2384–9.
Lane HW, Medina D, Wolfe LG. Proposed mechanisms for selenium-inhibition of mammary tumorigenesis (review). In Vivo. 1989;3:151–60.
Geerling BJ, Badart-Smook A, Stockbrugger RW, et al. Comprehensive nutritional status in recently diagnosed patients with inflammatory bowel disease compared with population controls. Eur J Clin Nutr. 2000;54:514–21.
Jackson RD, LaCroix AZ, Gass M, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354:669–83.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Hwang, C., Hong, K. (2016). Other Micronutrient Deficiencies in Inflammatory Bowel Disease: From A to Zinc. In: Ananthakrishnan, A. (eds) Nutritional Management of Inflammatory Bowel Diseases. Springer, Cham. https://doi.org/10.1007/978-3-319-26890-3_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-26890-3_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-26888-0
Online ISBN: 978-3-319-26890-3
eBook Packages: MedicineMedicine (R0)