Abstract
Purpose of Review
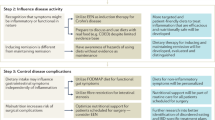
Diet and nutrition have emerged as key factors in the development and course of inflammatory bowel disease (IBD), including the approach to therapy. We present an overview of evidence-based recommendations and recent research in dietary therapy and nutrition management for patients with IBD.
Recent Findings
Patients with IBD should undergo a comprehensive nutrition assessment with the assistance of a registered dietitian (RD), including screening for micronutrient deficiencies. Multiple specialized whole foods and liquid formula diets have been evaluated as part of induction and maintenance therapy for IBD. Nutritional status should ideally be optimized in the perioperative setting as well.
Summary
Nutritional issues are prevalent among IBD patients and should be addressed by a multidisciplinary team, tailored to each patient’s disease type, severity and course, including response to medical therapy and need for surgical management, as well as relevant psychosocial considerations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The management of inflammatory bowel disease (IBD) has increasingly become multifaceted, involving medical, surgical and nutritional expertise in the approach to patient care. Diet has been recognized as a potential risk factor for IBD development, as well as a modifiable effector for patients with IBD. Diet can result in disruption of the gut microbiome and dysregulation of intestinal immune responses, which may, in turn, contribute to chronic inflammation of the gastrointestinal (GI) tract [1]. The Western diet, in particular, has evolved to include more processed foods and additives that may promote pro-inflammatory cytokine and endotoxin production, leading to IBD [2]. As a result, increasing research of nutrient-dense whole foods diets, with or without additional modifications, is being performed to evaluate whether dietary modification may improve symptoms, dysbiosis, inflammation and the long-term clinical course for patients with IBD. Data on this complex interplay is still emerging. Utilizing data from recently published studies, as well as recommendations for dietary management in IBD, we present a practical clinical approach to the assessment and management of diet and nutrition in patients with IBD.
While diet refers to food and liquid intake, nutrition refers to the ability to utilize food for growth, metabolism and tissue repair. According to the World Health Organization (WHO), malnutrition may be defined as “deficiencies, excesses or imbalances in a person’s intake of energy and/or nutrients,” and includes both undernutrition (i.e., poor growth, underweight status, micronutrient deficiencies) and overnutrition (i.e., overweight status, obesity, diet-related noncommunicable diseases, such as diabetes, heart disease, etc.) [3]. While rates of undernutrition among adults with IBD have declined in recent decades, the associated morbidity remains of significant concern, especially in the Crohn’s disease (CD) population, given that small intestinal disease may put these patients at higher risk of malabsorption [4••]. On the other hand, obesity affects about 15–40% of the IBD population, which can impact nutritional status, drug clearance, response to therapy and perioperative risk [5]. Screening tools, such as the Malnutrition Universal Screening Tool (MUST), Subjective Global Assessment (SGA) and Saskatchewan Inflammatory Bowel Disease Nutrition Risk questionnaire (SaskIBD-NR), may be utilized to identify patients who are at risk for malnutrition [4••]. However, these tools are better at identifying undernutrition, carry variable sensitivity in the IBD population and may not be routinely utilized in clinical practice.
In general, IBD patients with highly restricted diets, difficulty maintaining oral intake, unintentional weight loss or moderate-to-severe symptoms should be referred to a GI-specific registered dietitian (RD) for further evaluation and management. Baseline evaluation with a GI RD may be helpful for most patients with IBD, to facilitate comprehensive dietary assessments and evaluate nutritional status. Eating patterns should be carefully reviewed, including screening for disordered eating behaviors, eating disorders (i.e., anorexia nervosa, bulimia) and avoidant restrictive food intake disorder (ARFID), as well as other comorbid psychiatric conditions, such as anxiety and depression, which may impact eating behaviors, treatment plan adherence and IBD disease course [6, 7]. Moreover, additional psychosocial influences on eating patterns, including cultural and religious background and food insecurity, should be considered. In addition to routine physical examination and calculation of body mass index (BMI), GI RDs may also perform point-of-care analyses measuring waist or arm circumference or dynamometer measurements of muscle group strength, since myopenia (lean muscle mass depletion) and sarcopenia (muscle wasting with associated functional loss) may be more clinically relevant parameters with prognostic significance in the IBD population [8,9,10]. To this end, GI RDs may advise clinicians to consider obtaining specialized imaging, including ultrasound, CT, MRI and/or dual energy X-ray absorptiometry (DEXA), to help assess muscle mass, bone density and fat content [11].
Nutritional Evaluation
Even in the absence of a GI RD, the clinician can assess diet and nutritional status of IBD patients. The initial evaluation of patients with IBD should include evaluation of symptoms (especially as they relate to or affect oral intake), IBD history, current disease activity, anatomy and/or IBD-related complications, such as strictures and fistulas. Dietary intake, utilization of specialized diets, individual intolerances and psychosocial factors can be obtained through the history. Physical examination, BMI, recent changes in weight or oral intake and serum albumin levels can help evaluate nutritional status, though it is important to interpret these measures in the context of other parameters, including IBD activity, course and medical history.
Micronutrients
As part of the assessment of nutritional status, IBD patients should be routinely screened for micronutrient deficiencies, with the understanding that levels may fluctuate based on underlying inflammation, as they can be positive or negative acute phase reactants. Baseline evaluation should include iron studies (iron panel and ferritin, in addition to complete blood count), vitamin D, vitamin B12 and zinc levels, with consideration of other potential deficiencies based on concurrent conditions, medication use and surgical history (Table 1). Micronutrient levels should also be monitored closely in patients who undertake elimination diets, discussed below [12••]. Vitamin D and iron often require dedicated supplementation beyond a daily multivitamin. Vitamin D has been associated with immune regulation and is recommended in conjunction with calcium to help prevent low bone density, especially in patients who are treated with steroids. With respect to anemia, the Crohn’s & Colitis Foundation published the Anemia Care Pathway in 2017 for evaluation and management of anemia in patients with IBD [13••]. Iron can be provided orally or intravenously to help replenish stores and normalize hemoglobin when ferritin is less than 100 ng/mL or transferrin saturation is less than 20%. IV iron should be utilized in the setting of active disease and if there is inadequate response to or intolerance of oral iron supplementation (i.e., hemoglobin does not increase by at least 2 g/dL after one month of oral therapy) [13••]. In CD patients who have had greater than 20 cm of distal ileum resected, B12 monitoring is recommended and supplementation is indicated. Similarly, patients with ostomies and fistulas may lose zinc through the GI tract or ineffectively absorb it in the setting of active inflammation and should increase dietary intake and consider zinc supplementation. Correction of zinc deficiency has been associated with improved clinical outcomes in IBD patients [4••]. Folic acid supplementation is generally indicated in women of child-bearing age, as well as patients treated with methotrexate and sulfasalazine, which may affect folate absorption. Nutritional status should be monitored closely in patients who may become pregnant, are pregnant or are breastfeeding [14••].
General Recommendations for Diet in Patients with IBD
While there is no consensus on any one specific diet best suited for patients with IBD, based on the best available data, the International Organization for the Study of Inflammatory Bowel Diseases (IOIBD) recommends a diet generally rich in omega-3 fatty acids, fruits and vegetables for patients with both CD and ulcerative colitis (UC) [16••]. In contrast, processed foods and artificial sweeteners should generally be avoided, as they may contribute to increased inflammation and GI symptoms. Based on the IOIBD guidelines and a recent Cochrane review of several different dietary therapies for IBD, there is insufficient data to recommend any one specialized diet, including specifically restricting wheat, gluten or dairy if otherwise tolerated [17]. Alcohol should be consumed in moderation [16••]. According to the European Society for Clinical Nutrition and Metabolism (ESPEN), macronutrient and general energy requirements in patients with IBD are comparable to their healthy counterparts. Energy needs can be individualized based on BMI, inflammation and activity level. Optimal protein intake is approximately 1 g/kg/d. Daily protein should be increased to 1.2–1.5 g/kg/d during flares because of the catabolic response with subsequent proteolysis during such periods [4••, 18••]. Weight management counseling and resources should be provided to obese patients, especially during periods of remission [12••]. For prevention of IBD, ESPEN also advocates breastfeeding, as well as a diet rich in fruits, vegetables and n-3 fatty acids and low in n-6 fatty acids [18••].
Considerations During Flares or in Symptomatic Patients with Quiescent IBD
During IBD flares, food consistency can be modified to help with symptom control. Apart from those with chronic stricturing disease, patients in remission should not necessarily restrict fiber intake; however, decreasing insoluble fiber and/or modifying the texture of fiber may be more tolerable during periods of active disease. Cooking, chopping, blending or pureeing higher fiber foods, like fresh fruits and vegetables, can decrease food particle size and may be helpful to optimize digestion. Adding a soluble fiber supplement, like psyllium husk, can help in cases of high-volume stool output during significant flares or in patients with J pouches or ostomies. Increasing nutrient dense liquid intake by adding high calorie ingredients, like nut butters, avocado and olive oil, may also be beneficial to help maintain caloric needs. Avoiding lactose and fermentable oligo-, di-, monosaccharides and polyols (FODMAPs) may provide symptomatic relief as well, especially for patients with quiescent disease, by reducing abdominal pain, bloating and diarrhea not related to underlying inflammation [19]. Bile acid sequestrants can be a very helpful adjunct in patients with a history of ileal resection or extensive small bowel disease. There is limited data to support the use of pre- and probiotics and antioxidants for induction or maintenance of remission in IBD. However, therapy with multistrain probiotics may be considered for patients with mild-to-moderate UC or pouchitis unresponsive to antibiotics and for primary and secondary prophylaxis against pouchitis [20].
Specialized Whole Foods Diets
Multiple specialized diets have been studied in the context of IBD treatment induction and maintenance therapy. Prior to recommending or initiating a particular therapeutic diet, various factors should be considered, including patients’ overall clinical status and degree of malnutrition, if present, history of or current eating disorder, patients’ ability to adhere to the diet based on their level of commitment and feasibility of the diet itself, with regard to access and other potential constraints. We will review a few of these specialized diets here (Table 2).
The Mediterranean diet is largely plant-based and includes poultry, dairy products and alcohol in moderation, while limiting red meat and sweets. It may be beneficial in patients affected by various inflammatory diseases, including IBD, psoriasis and rheumatoid arthritis, and can be utilized as part of induction and maintenance therapy in IBD, given its multiple other health benefits. In 2020, the results of the DINE-CD randomized controlled trial (RCT) were published, comparing the efficacy of the Mediterranean diet with the specific carbohydrate diet (SCD) in adults with active CD (short Crohn’s disease activity index or sCDAI of 176–399). The SCD focuses on elimination of highly processed foods, grains, starchy vegetables, dairy and refined sugars, as well as preservatives and artificial ingredients. Foods included in the SCD are fruits and vegetables, most nuts/nut flours/nut butters, fish, unprocessed meat, poultry, homemade yogurt (fermented for 24 hours) and some hard cheeses. The DINE-CD RCT found no significant difference in rates of symptomatic remission or inflammatory markers in adults with mild-to-moderate CD [21]. At week 6 (primary outcome), there was no significant difference in rates of symptomatic remission, even when stratified by baseline inflammation. However, at both weeks 6 and 12, 40–50% of patients in both arms achieved symptomatic or clinical remission and 30–35% of patients had an improvement in fecal calprotectin. No significant changes were noted in C-reactive protein (CRP). In this study, patients remained on stable doses of medications, with 50–60% on biologics at the time of study entry. This suggests that dietary modification, with the Mediterranean diet being less restrictive, may improve symptoms and inflammation in patients with IBD, including as an adjunct to existing IBD therapy. A more recent study of IBD patients with active disease or in remission found the Mediterranean diet improved nutritional status, IBD activity, CRP, fecal calprotectin and quality of life over six months [26], lending further support to the original IOIBD recommendations.
Other whole foods diets that have been studied include the plant-based diet, diets low in fat, meat, emulsifiers and sulfur, the paleo autoimmune protocol (AIP), the novel UC exclusion diet (UCED) and food exclusion based on IgG antibodies. The low emulsifier diet involves limiting additives and natural emulsifiers, such as carrageenan, a seaweed extract, and has been studied for both induction and maintenance therapy. Data in vitro and in animals have suggested that emulsifiers can potentially induce colitis, and a cohort of 20 patients with CD experienced symptom reduction and improved quality of life on this diet [27]. The low sulfur diet involves total and sulfur containing protein and additive reduction, with limited evidence of clinically significant efficacy to date [28]. The paleo AIP is perhaps the most restrictive diet during induction, with staged elimination of grains, dairy, legumes, nightshades, alcohol, processed/refined foods and additives, though it focuses on nutrient dense intake, high in meats, and emphasizes other lifestyle factors. A small uncontrolled study of 15 adults with active CD and UC found 73% (11/15) achieved clinical remission (measured by partial Mayo score for UC or Harvey Bradshaw Index for CD), as well as improvements in fecal calprotectin and quality of life, though patients were not followed into reintroduction [22]. The UCED is a two-phase diet used for treatment induction, limiting animal fats and sulfated amino acids, and was associated with 38% improvement in UC activity scores in a prospective, single-arm, open-label study of 24 pediatric patients with mild-to-moderate UC [23]. A more recent trial, CRAFT UC, randomized 51 adult UC patients to UCED with or without fecal microbiota transplantation (FMT) or FMT with a free diet. The UCED alone achieved higher remission (~ 40%) and mucosal healing rates (27%) compared to FMT with or without dietary modification [24]. Finally, with respect to dietary modifications, patients often ask about the value of testing for IgG to identify potential sensitivities. Unlike IgE, which may suggest food allergy, IgG testing does not carry a pathophysiologic basis for demonstrating food allergy, sensitivity or intolerance and is not recommended by guidelines [29].
It is important to recognize that specialized diets, like the SCD or other exclusion diets, often begin with an induction phase (lasting anywhere from 1–6 weeks), followed by a maintenance phase that is self-paced to allow for achievement and/or maintenance of remission. It is suggested that remission be maintained for anywhere from three months to two years before introducing foods initially excluded. Foods can generally be added back into the diet one at a time every few days and gradually thereafter, based on individual tolerance.
Specialized Diets Involving Enteral Nutrition
In certain circumstances, liquid-based nutrition may be indicated for patients with active disease (whether perioperative, active disease, symptoms or complications affecting oral intake and/or as a form of induction therapy) or those in remission with associated malnutrition. In these cases, enteral nutrition (EN), with or without a whole foods diet, can be a helpful approach. Standard formulas of liquid supplementation contain complete nutrition with carbohydrates (little or no fiber), fat and protein (typically polymeric, though can be elemental or semi-elemental). Administration of EN via oral intake is preferred, with polymeric formulas being more palatable and commercially available. However, nasogastric, nasoduodenal or percutaneous gastrostomy/jejunostomy tubes are utilized when oral intake remains insufficient or is not feasible [4••]. EN may be given as exclusive enteral nutrition (EEN, comprising > 90% daily calories), partial enteral nutrition (PEN, comprising ~ 50% daily calories) or as a supplement (with < 50% calories from formula). When given as a supplement, EN is often referred to as oral nutrition supplementation (ONS). EN is preferred over parenteral nutrition (PN), which is administered intravenously, except when EN is contraindicated (i.e., patients with bowel obstruction, short bowel syndrome or those who are intolerant of oral feeds). Of note, those with distal fistulizing CD with low output can generally receive EN, whereas partial parenteral nutrition (PPN) or total parenteral nutrition (TPN) should be used in those with more proximal, high output fistulas and is of primary importance for those who cannot maintain adequate hydration orally. In contrast, PN is generally not recommended in UC except in cases of intestinal failure. Regardless of approach (EN vs. PN), monitoring for refeeding syndrome should be undertaken in the setting of prolonged nutritional deprivation.
EEN has been widely studied and proven to be effective for induction or symptomatic relapses in the mild-to-moderate pediatric CD population [30, 31]. It is also considered a safe adjunctive therapy in the pediatric UC population. EEN is typically administered over 6–12 weeks and results in high remission rates of 50–80%. Though it can be effective in adults as well, EEN is generally not tolerated for prolonged periods of time in the adult population, affecting adherence and response rates. The goal of EEN is to supply 100% of nutritional needs in the form of a nutrient-dense liquid supplement, purposefully easing digestive function and allowing for bowel rest. It has been associated with superior mucosal healing (up to 80%) [25, 30]. However, EEN may not need to be used in lieu of medical therapy. A recent meta-analysis of nine studies suggested that EEN may improve response and remission rates for CD patients already on anti-tumor necrosis factor (TNF) therapy, again highlighting the synergistic effects of diet and medical therapy for patients [32].
Consideration for use of EEN as first line nutrition therapy should focus on patients’ ability to maintain compliance, as well as optimizing their quality of life. Given limitations of widespread adoption of EEN, Levine et al. recently conducted an RCT comparing EEN with a Crohn’s Disease exclusion diet (CDED) and PEN in 78 children with recently diagnosed mild-to-moderate CD. CDED excludes dairy, wheat, animal fat, additives, fried foods and processed foods, but in a two-stage manner includes fruits, vegetables, rice, potatoes, lean meats and eggs. During the first six weeks of the study, CDED was given with 50% EN, whereas the other arm was 100% EN. The authors found that both were effective at achieving remission, but CDED plus PEN was better tolerated than EEN. In the second six weeks, CDED was given with 25% EN and the EEN arm was transitioned to 25% EN with a free diet. At week 12, they found CDED plus PEN was superior in sustaining remission and reducing inflammation, as measured by fecal calprotectin [25].
Similar recommendations for specialized diets apply to the use of EN, with staged introduction/induction, maintenance and reintroduction of foods. With EN, the first 4–12 weeks of the diet are used to induce remission, and when combined with a whole foods diet, it is helpful to initially limit insoluble fiber that could cause obstructive issues. During latter stages of induction or maintenance, once patients are feeling better, it may be feasible to gradually add soluble fiber from fruits and vegetables. For patients doing EEN initially, latter stages may also allow for reintroduction of whole foods and shift towards PEN and even ONS. Eventually, during reintroduction, movement should be towards a Mediterranean style diet with minimization of processed foods and refined sugars. It is important to recognize that many specialized diets may involve unique sustained eliminations, particularly as they relate to dairy and gluten, though there is insufficient data to recommend this.
Perioperative Nutritional Management
Perioperative nutritional management should be focused on optimizing nutritional status prior to elective surgery for IBD. Enhance Recovery After Surgery (ERAS) protocols offer perioperative nutrition support most often in the form of higher carbohydrate ONS a few weeks to days leading up to surgery, as well as aggressive nutrition support in the few days following surgery, with the intent to achieve early recovery by minimizing the stress response from surgical intervention [33]. Per ERAS protocols, ONS can be implemented as first line therapy, followed by EN support, if patients are unable to meet metabolic demands with oral supplementation alone. Multiple cohort studies have found that preoperative EN support is associated with decreased complication rates, including related to stoma function and infection, in patients undergoing surgical management of IBD, especially those with CD [34, 35]. A retrospective case-control study of stricturing or penetrating CD patients undergoing planned surgery found that 25% of patients receiving EEN preoperatively were able to avoid surgery [36]. In this study, preoperative EEN (mean duration 6.3 weeks, SD 0.4) was associated with a shorter length of operation and lower rate of postoperative complications [36]. The European Crohn's and Colitis Organisation (ECCO) Current Practice Position statement notes that EEN may improve nutritional status and reduce complications for preoperative CD patients, though optimal duration and route of administration is best defined by a multidisciplinary team [37]. In malnourished patients who require emergency surgery, EN or TPN should be initiated as early as possible, especially if prolonged nil per os (NPO) status is anticipated. In all circumstances, EN is preferred over TPN, which is reserved for cases in which EN is contraindicated (i.e., ileus, obstruction, intestinal ischemia, severe shock). The significant metabolic impact of a surgical intervention is the result of total body protein catabolism and an increased postsurgical stress response, as evidenced by increased cardiac output, hyperglycemia, insulin resistance and mobilization of energy reserves for tissue repair and fuel optimization. In malnourished patients, this response can result in postoperative complications and longer hospitalizations. The primary goals of perioperative nutrition support are to minimize surgical stress, improve physiologic and functional recovery and reduce postoperative complications [18••, 38, 39].
Conclusion
Patients with IBD face several concerns regarding risk of malnutrition, micronutrient deficiency and change in dietary patterns during periods of remission and active disease. Malnutrition remains a common complication of IBD, both as a direct consequence of the disease itself and secondary factors, including decreased oral intake, disordered eating, malabsorption, increased nutrient losses and food insecurity. Patients should undergo appropriate risk stratification with close monitoring of their nutritional status as part of routine IBD care and perioperative nutrition management under the guidance of an IBD specialized RD. The approach to each patient should be individualized based on disease subtype, extent of involvement/clinical severity, medical and surgical history and psychosocial determinants of disease. In most studies presented, dietary interventions were performed in patients on stable medical therapy, rather than in lieu of therapy, suggesting that diet can be utilized alongside medical and/or surgical therapy to improve response rates and quality of life. Research is ongoing, and indeed we may find that a subset of patients may only need dietary manipulation for management of IBD. Larger, evidence-based studies are needed to further guide treatment decisions to help promote optimization of nutritional status and dietary approach.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Chang J. Pathophysiology of inflammatory bowel diseases. N Engl J Med. 2020;383(27):2652–64. https://doi.org/10.1056/NEJMra2002697.
Lewis JD, Abreu M. Diet as a trigger or therapy for inflammatory bowel diseases. Gastroenterology. 2017;152(2):398-414.e6. https://doi.org/10.1053/j.gastro.2016.10.019.
Who.int. 2022. Fact sheets - Malnutrition. [online] Available at: https://www.who.int/news-room/fact-sheets/detail/malnutrition. Accessed 19 Sept 2022.
•• Fitzpatrick JA, Melton S, Yao C, et al. Dietary management of adults with IBD — the emerging role of dietary therapy. Nat Rev Gastroenterol Hepatol 2022:1–18. https://doi.org/10.1038/s41575-022-00619-5. Recent comprehensive review of approach to nutritional assessment and management in IBD patients.
Singh S, Dulai PS, Zarrinpar A, et al. Obesity in IBD: epidemiology, pathogenesis, disease course and treatment outcomes. Nat Rev Gastroenterol Hepatol 2017:14(2):110–21. https://doi.org/10.1038/nrgastro.2016.181.
Ludvigsson JF, Olén O, Larrson H, et al. Association between inflammatory bowel disease and psychiatric morbidity and suicide: a Swedish nationwide population-based cohort study with sibling comparisons. J Crohns Colitis 2021:15:1824–36. https://doi.org/10.1093/ecco-jcc/jjab039.
Ilzarbe L, Fàbrega M, Quintero J, et al. Inflammatory bowel disease and eating disorders: a systematized review of comorbidity. J Psychosom Res 2017:102:47–53. https://doi.org/10.1016/j.jpsychores.2017.09.006.
Bryant RV, Schultz CG, Ooi Soong, et al. Obesity in inflammatory bowel disease: gains in adiposity despite high prevalence of myopenia and osteopenia. Nutrients 2018:10:1192. https://doi.org/10.3390/nu10091192.
Fearon K, Evans WJ, Anker SD. Myopenia–a new universal term for muscle wasting. J. Cachexia Sarcopenia Muscle 2011:2:1–3. https://doi.org/10.1007/s13539-011-0025-7.
Bryant RV, Ooi S, Schultz CG, et al. Low muscle mass and sarcopenia: common and predictive of osteopenia in inflammatory bowel disease. Aliment Pharmacol Ther. 2015;41:895–906. https://doi.org/10.1111/apt.13156.
Wood J, Ward L, Sparrow M, et al. Utility of bioimpedance methods for the assessment of fat-free mass in adult outpatients with inflammatory bowel disease. Nutrition. 2020;77:110833. https://doi.org/10.1016/j.nut.2020.110833.
•• Ananthakrishnan A, Kaplan G, Bernstein CN, et al. Lifestyle, behaviour, and environmental modification for the management of patients with inflammatory bowel diseases: an international organization for study of inflammatory bowel diseases consensus. Lancet Gastroenterol Hepatol 2022:7(7):666–678. https://doi.org/10.1016/S2468-1253(22)00021-8. Recent overview of lifestyle, including dietary modifications, as part of IBD therapy.
•• Hou JK, Gasche C, Drazin NZ, et al. Assessment of gaps in care and the development of a care pathway for anemia in patients with inflammatory bowel diseases. Inflamm Bowel Dis 2017:23(1):35–43. https://doi.org/10.1097/MIB.0000000000000953. Crohn’s and Colitis Foundation Anemia Care Pathway.
•• Mahadevan U, Robinson C, Bernasko N, et al. Inflammatory bowel disease in pregnancy clinical care pathway: a report from the american gastroenterological association IBD parenthood project working group. Inflamm Bowel Dis 2019:25(4):627–41. https://doi.org/10.1053/j.gastro.2018.12.022. Multisociety guideline for management of fertility, pregnancy and lactation in IBD.
Hwang C, Ross V, Mahadevan U. Inflamm Bowel Dis. 2012;18(10):1961–81. https://doi.org/10.1002/ibd.22906.
•• Levine A, Rhodes JM, Lindsay JO, et al. Dietary guidance from the international organization for the study of inflammatory bowel diseases. Clin Gastroenterol Hepatol 2020:18(6):1381–92. https://doi.org/10.1016/j.cgh.2020.01.046. IOIBD dietary guidelines for IBD.
Limketkai BN, Iheozor-Ejiofor Z, Gjuladin‐Hellon T, et al. Dietary interventions for induction and maintenance of remission in inflammatory bowel disease. Cochrane Database Syst Rev 2019(2). Art. No.: CD012839. https://doi.org/10.1002/14651858.CD012839.pub2.
•• Bischoff SC, Escher J, Hébuterne X, et al. ESPEN practical guideline: clinical nutrition in inflammatory bowel disease. Clin Nutr 2020:39:632–53. https://doi.org/10.1016/j.clnu.2019.11.002. Evidence-based nutrition guidelines for IBD from the European Society for Clinical Nutrition and Metabolism.
Cox S, Lindsay J, Fromentin S, et al. Effects of Low FODMAP Diet on symptoms, fecal microbiome, and markers of inflammation in patients with quiescent inflammatory bowel disease in a randomized trial. Gastroenterology 2020:158(1):176–188. https://doi.org/10.1053/j.gastro.2019.09.024.
Fujiya M, Ueno N, Kohgo Y. Probiotic treatments for induction and maintenance of remission in inflammatory bowel diseases: a meta-analysis of randomized controlled trials. Clin J Gastroenterol 2014:7(1)e13. https://doi.org/10.1007/s12328-013-0440-8.
Lewis JD, Sandler RS, Brotherton C, et al. A randomized trial comparing the specific carbohydrate diet to a Mediterranean diet in adults with Crohn’s disease. Gastroenterology 2021:161:837–52.e9. https://doi.org/10.1053/j.gastro.2021.05.047.
Konijeti GG, Kim N, Groven S, et al. Efficacy of the autoimmune protocol diet for inflammatory bowel disease. Inflamm Bowel Dis 2017:23:2054–60. https://doi.org/10.1097/MIB.0000000000001221.
Sarbagili-Shabat C, Albenberg L, Van Limbergen J, et al. A novel UC exclusion diet and antibiotics for treatment of mild to moderate pediatric ulcerative colitis: a prospective open-label pilot study. Nutrients 2021:13:3736. https://doi.org/10.3390/nu13113736.
Levine A, Scaldaferri F, Sarbagili Shabat C, et al. OP01 Comparison of fecal transplantation, fecal transplantation with the novel UC diet or the UC diet alone for Refractory Mild to Moderate Active Ulcerative Colitis: The CRAFT UC randomized controlled trial. J Crohn’s Colitis. 2021;15(Supplement 1):001. https://doi.org/10.1093/ecco-jcc/jjab165.
Levine A, Wine E, Assa A, et al. Crohn’s disease exclusion diet plus partial enteral nutrition induces sustained remission in a randomized controlled trial. Gastroenterology 2019:157:440–50.e8. https://doi.org/10.1053/j.gastro.2019.04.021.
Chicco F, Magrì S, Cingolani A, et al. Multidimensional impact of mediterranean diet on IBD patients. Inflamm Bowel Dis. 2020;27(1):1–9. https://doi.org/10.1093/ibd/izaa097.
Sandall AM, Cox SR, Lindsay JO, et al. Emulsifiers impact colonic length in mice and emulsifier restriction is feasible in people with Crohn’s disease. Nutrients 2020:12:2827. https://doi.org/10.3390/nu12092827.
Yao C, Muir J, Gibson P. Review article: insights into colonic protein fermentation, its modulation and potential health implications. Aliment Pharmacol Ther. 2015;43(2):181–96. https://doi.org/10.1111/apt.13456.
Bock S. AAAAI support of the EAACI Position Paper on IgG4. J Allergy Clin Immunol. 2010;125(6):1410. https://doi.org/10.1016/j.jaci.2010.03.013.
Ruemmele FM, Veres G, Kolho KL, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohn’s Colitis 2014:8:1179–1207. https://doi.org/10.1016/j.crohns.2014.04.005.
van Rheenen PF, Aloi M, Assa A, et al. The medical management of Paediatric Crohn’s Disease: an ECCO-ESPGHAN Guideline Update. J Crohn’s Colitis 2021:15(2):171–94. https://doi.org/10.1093/ecco-jcc/jjaa161.
Hirai F, Takeda T, Takada Y, et al. Efficacy of enteral nutrition in patients with Crohn’s disease on maintenance anti-TNF-alpha antibody therapy: a meta-analysis. J Gastroenterol 2020:55(2):133–41. https://doi.org/10.1007/s00535-019-01634-1.
Lee GC, Hodin RA. Applying enhanced recovery pathways to unique patient populations. Clin Colon Rectal Surg. 2019;32(2):134–137. https://doi.org/10.1055/s-0038-1676479.
Abdalla S, Benoist S, Maggiori L, et al. Impact of preoperative enteral nutritional support on postoperative outcome in patients with Crohn’s disease complicated by malnutrition. Colorectal Dis 2021:23:1451–62. https://doi.org/10.1111/codi.15600.
Meade S, Patel KV, Luber RP, et al. A retrospective cohort study: Pre-operative oral enteral nutritional optimisation for Crohn’s disease in a UK tertiary IBD Centre. Aliment Pharmacol Ther 2022:56:646–63. https://doi.org/10.1111/apt.17055.
Heerasing N, Thompson B, Hendy P, et al. Exclusive enteral nutrition provides an effective bridge to safer interval elective surgery for adults with Crohn’s disease. Aliment Pharmacol Ther 2017:45:660–69. https://doi.org/10.1111/apt.13934.
Adamina M, Bonovas S, Raine T, et al. European Crohn’s and Colitis Organisation [ECCO], ECCO guidelines on therapeutics in Crohn’s Disease: surgical treatment. J Crohn’s Colitis 2020:14(2):155–68. https://doi.org/10.1093/ecco-jcc/jjz187.
Feldman LS, Delaney CP, Ljungqvist O, et al. The SAGES / ERAS Society Manual of Enhanced Recovery Programs for Gastrointestinal Surgery. Cham: Springer International Publishing; 2015.
Fiorindi C, Cuffaro F, Piemonte G, et al. Effect of long-lasting nutritional prehabilitation on postoperative outcome in elective surgery for IBD. Clin Nutr. 2021;40(3):928–35. https://doi.org/10.1016/j.clnu.2020.06.020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Pooja R. Magavi declares no potential conflict of interest.
Lori A. Beeken declares no potential conflict of interest.
Rebecca Matro is on the speakers bureau for AbbVie.
Mazer Ally is on the speakers bureau for AbbVie.
Melissa J. Ferrari declares no potential conflict of interest.
Gauree G. Konijeti is on the advisory board for Pfizer & ProciseDx and the speakers bureau for Takeda.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Inflammatory Bowel Disease
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Magavi, P.R., Beeken, L.A., Matro, R. et al. Incorporating Nutrition-Based Strategies into IBD Treatment. Curr Gastroenterol Rep 24, 183–190 (2022). https://doi.org/10.1007/s11894-022-00851-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11894-022-00851-8