Key Points
-
Ankle arthritis usually results from posttraumatic arthritis.
-
Patients with ankle arthritis are usually younger than those individuals with hip and knee osteoarthritis (OA) but are equally disabled.
-
Common traumatic injuries to the ankle include ankle fractures and sprains.
-
Ankle fractures are common in young and old adult populations and are one of the most common orthopedic injuries.
-
Ankle OA has a specific pathology in cartilage load bearing and injury compared to OA of the knee and hip.
-
Injuries to the ankle may predispose to an altered gait cycle and weight-bearing process in the lower extremity.
-
Treatment for ankle injuries can be nonoperative or operative depending on the severity of trauma, involved soft tissue, and bony anatomy.
-
OA of the ankle can be treated conservatively with anti-inflammatory medications and therapy. Surgical treatments include joint-sparing procedures, joint fusions, or total ankle replacements.
-
Research related to the biomechanics of trauma and ankle OA remains an area of focus.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Ankle Osteoarthritis (OA) arthritis usually results from posttraumatic arthritis.
-
Patients with ankle OA are usually younger than those individuals with hip and knee OA but are equally disabled.
-
Common traumatic injuries to the ankle include ankle fractures and sprains.
-
Ankle fractures are common in young and old adult populations and are one of the most common orthopedic injuries.
-
Ankle OA has a specific pathology in cartilage load bearing and injury compared to OA of the knee and hip.
-
Injuries to the ankle may predispose to an altered gait cycle and weight-bearing process in the lower extremity.
-
Treatment for ankle injuries can be nonoperative or operative depending on the severity of trauma, involved soft tissue, and bony anatomy.
-
OA of the ankle can be treated conservatively with anti-inflammatory medications and therapy. Surgical treatments include joint-sparing procedures, joint fusions, or total ankle replacements.
-
Research related to the biomechanics of trauma and ankle OA remains an area of focus.
Introduction
The ankle joint is one of the major weight-bearing joints in the body. Unlike the common degenerative pathology in hip and knee arthritis related to aging, arthritis in the ankle usually results from posttraumatic causes [1]. Ankle arthritis can affect both young and older populations, resulting in pain, limited mobility, and decreased quality of life [2]. Combination of both bony and ligamentous issues related to trauma and aging may play a role in accelerating the quality and viability of the cartilage, ligaments, and tendons of the ankle [3]. Alterations to the unique biomechanical properties of the ankle which are involved in the gait cycle can create issues with mobility and stability of the lower limbs. There are many different treatment options, both surgical and nonsurgical, which have been developed. Potential treatment options for ankle arthritis continue to be a dedicated focus for clinical research, with an aim to better address the symptoms and pathologies involved in ankle degeneration.
Incidence
The common pathology of arthritis can have many causes including trauma, infection, and inflammatory and systemic disorders. Primary OA has been defined as an idiopathic condition developing in previously undamaged joints in the absence of an obvious causative mechanism [4]. Secondary arthritis can be caused by an underlying condition, such as a joint injury, accumulation of calcium inside the joint, other inflammatory bone and joint conditions (e.g., rheumatoid arthritis (RA)), or a medical condition, such as diabetes. Rheumatoid and psoriatic arthritis, as well as gout, neuromuscular disorders, and infection, can contribute to degeneration of a joint. However, in the ankle, posttraumatic arthritis is the most common cause of OA.
The most common etiological factor in the development of OA of the ankle is posttraumatic following fractures and severe sprains of the ankle [5]. Injuries to the ankle have a bimodal population distribution among young, active, risk-taking individuals and middle-aged individuals with sprains or work-related injuries. Foot and ankle fractures were most common presentations seen at major trauma hospitals in the United States [6], with a majority of the posttraumatic ankle arthritis resulting from rotational ankle fractures. While the reported prevalence of posttraumatic arthritis in the ankle has been variable, an important predictor is the severity of the injury to the articular cartilage [7].
Ankle Anatomy and Osteoarthritis
The ankle joint provides a combination of the ability to serve as a weight-bearing surface with the ability to permit motion and force alterations in a normal gait cycle. In order to address the complex changes which can occur in this joint due to injury and resultant pathology, a basic understanding of the anatomical structure of the ankle is paramount.
The ankle joint is comprised of three bony surfaces: the distal tibia, the distal fibula, and the talus. These three surfaces articulate with each other with each step of the gait cycle. The tibiotalar joint is covered with articular cartilage that reduces the shear and compressive forces transmitted across the ankle with normal weight-bearing. The distal fibula is the central attachment point for the lateral ankle ligaments as well as the syndesmosis of the ankle. The syndesmosis complex is located 2 cm above the ankle joint and contains four ligaments, including the anterior and posterior tibiofibular ligamentous complex which helps to stabilize the mortise of the ankle. The deltoid, a primary robust stabilizer of the ankle, attaches to the medial aspect of the tibia and inserts along the medial column of the foot. Stability of the ankle is dependent on the interaction between the bony articulations of the ankle joint and ligamentous structures for balance. These ligaments ensure that the tibia and fibula, which create the primary constraints of the joint, stay in close contact while weight-bearing, and the joint remains a stable construct in the ankle mortise. Any pathology which may affect the bone [8] and soft tissue complex of the ankle can cause altered biomechanics and acceleration in degenerative changes.
The ankle–foot mechanism is a critical component of gait. The gait cycle is a complex of interdependent physiological interactions between the bony and soft tissue components of the foot and ankle, and the surrounding environment. The gait cycle has two phases – the stance phase and the swing phase. During the stance phase, bony articulations of the foot and ankle lock together to provide a platform for weight-bearing, whereas in the swing phase, the bony and soft tissue articulations unlock to allow for push-off of the foot to follow with an additional step, which creates the cycle again. The joints that comprise the ankle and the foot allow for full weight-bearing through the stance phase while at the same time dynamically adjusting to any alterations in terrain. The ability of the foot to adjust and respond to terrain variability optimizes people’s ability to mobilize. Unfortunately, it also increases the risk of trauma to the ankle/foot mechanism [9].
Pathogenesis
The process of cartilage degeneration can vary among different joints in the body. Primary and progressive OA is not common in the ankle compared to other joints, such as the hip and knee [10]. Cartilage in the ankle, with its terminal weight-bearing properties and smaller joint surface area compared to the knee and hip, has unique features to allow these functions. Basic science research has dedicated a focus to determining specific biochemical and mechanical properties following traumatic injuries which may explain this phenomenon. Although the exact mechanisms underlying the pathogenesis of posttraumatic OA have not yet been fully established, inflammatory responses within the joint, direct impact of the articular cartilage, and early changes in subchondral bone have all been implicated as potentially deleterious processes predisposing to OA development over the long term [11]. Nakasa et al. [12] studied these differences between the ankle and other joints and concluded a strong relationship between the subchondral bone plate and cartilage degeneration in the progression of OA in the ankle. Cartilage in the ankle joint differs from other joints of the body due to the unique properties with weight-bearing and gait. Interestingly, the articular cartilage of the ankle is one of the thinnest of the weight-bearing joints and ranges from 1 to 1.7 mm [13]. In addition, ankle cartilage shows a higher compressive stiffness and proteoglycan density, lower matrix degradation, and decreased response to catabolic stimulations [14].
Compared to other smaller joints in the body, such as the elbow and wrist, the ankle joint maintains a flexible range of motion (ROM). However, in the ankle as a weight-bearing joint, the osteoarthritic process of degeneration and biomechanics are strongly linked: altered loading patterns, micro-ligamentous instability, increased intra-articular and periarticular mechanical forces, and changed biomechanics are substantial contributing factors in the initiation and progression of ankle OA [15]. This is illustrated in the fact that 1 mm of lateral displacement of the fibula post fracture can result in significantly diminished joint contact area and increased joint reactive forces on the talus that result in accelerated abnormal wear patterns [16].
Structural/Biomechanical Alterations
During normal walking, forces up to five times the body weight are transferred through the ankle, and this increases with running and other strenuous exercise [17]. The cartilage of the ankle joint possesses unique physical and biomechanics characteristics which allow adaption to weight-bearing stressors. The cartilage in the ankle is stiffer and more resistant to deformation than other weight-bearing joints, allowing it to support these increased loads [18]. In the setting of OA, the cartilage of the ankle joint degenerates, which may negatively impact the weight-bearing properties and mobility of the ankle during the gait cycle.
Changes in gait patterns are common complaints in patients with ankle OA. Quality and quantity of distance walking ability, usually diminish as the disease progresses. Patients with restricted ankle function due to OA generally walk slower than normal [19], which has been shown to mediate joint load reduction [20].
In addition to changes in gait, other factors may predispose individuals with previous ankle trauma to an accelerated process of cartilage and joint degeneration. The circumstances and timeline surrounding acute treatment of ankle injuries have been shown to be a critical factor in increased risk of developing OA. The more severe the fracture, the more likely a patient develops degenerative joint disease [21]. Several conditions have been associated with an increased risk of developing radiographic ankle OA or end-stage OA following a malleolar fracture. These include increasing age, female gender, fracture severity, location and extent of cartilage lesions (especially of the medial malleolus), quality of fracture reduction, and presence of a fracture dislocation [22]. Goals of acute operative fracture treatment, include, anatomic restoration of the joint; adequate reduction is critical, with reduction of the lateral malleolus to restore normal length, and produce correct alignment of the talus within the mortise being most important [23]. A mere 1 mm of lateral displacement of the talus, the combination of decreased surface area and increased contact pressures across the ankle joint articular cartilage, if left unaddressed, results in cartilage wear and arthritis [24].
There are other factors that can increase the likelihood of complications and predispose one to the development of ankle OA. Patients with a body mass index (BMI) greater than 25 have a 1.5 times higher risk for the diagnosis of foot and ankle OA [25], with the risk increasing in people with rising BMI and in patients over 30 years of age at the time of injury and with increasing length of time since surgery. The probability of developing posttraumatic ankle OA among patients having three or more risk factors was 60–70 % in an 18-year follow-up study [22]. In general, a higher risk for ankle fractures in overweight and obese persons has been suggested [26]. Additionally, overweight and obese subjects seem to sustain more severe types of ankle fractures [27].
Stufkens et al. [28] performed a long-term follow-up study of a prospective cohort of 288 ankle fractures that were treated operatively between 1993 and 1997. In the initial study, arthroscopy was performed in all cases to assess the extent and location of intra-articular cartilage damage. In a follow-up study, a total of 109 patients were available for clinical and radiographic assessment. Deep cartilage lesions on the anterior and lateral aspect of the talus and on the medial malleolus with odds ratios of 12.3, 5.4, and 5.2, respectively, were identified as independent predictors of the development of posttraumatic ankle OA [29]. Traumatic injuries to the ankle joint can accelerate the process of OA. Although this may not occur as an acute process in all individuals with ankle injuries, it may accelerate osteoarthritic symptoms and cartilage quality of the ankle joint. Traumatic ankle injuries that may result in OA, include, fractures of the malleoli, tibial plafond, talus, isolated osteochondral damage of the talar dome secondary to ankle sprain, and ankle ligament injury. The fact that primary injuries are more likely to be sustained by younger individuals indicates that posttraumatic OA develops earlier than other forms of OA, with a recent study finding that individuals with ankle and knee posttraumatic OA were approximately 14 and 10.4 years younger, respectively, than their counterparts with other forms of OA [30].
Clinical Presentation/Risk Factors
Clinical history is of uttermost importance in patients presenting with ankle OA. Due to the nature of causes of OA in the ankle, commonly being a result of injury, information about the timeline since injury, method of treatment, and location of symptoms can assist with clinical decision making. Gathering information regarding duration and specificity of symptoms, in conjunction with complete physical exam of the ankle, including, gait analysis, can help to identify issues of concern specific to each patient.
Patients with ankle OA usually present with gait abnormalities and decreased ROM of the affected ankle. These abnormalities may affect simple daily functions of living, such as, walking upstairs, and tolerating inclines and uneven surfaces. Clinical examination should include, observation of gait, and stance of the lower extremities. In general, gait analyses in patients with ankle OA revealed a lower walking speed, cadence, step length, and stride length compared to healthy people of a similar age [19]. Individuals may be able to specify the exact location of their discomfort with a related activity, whereas others may complain of overall ankle pain. It is common for patients with ankle OA to have small to moderate joint effusions and crepitus of the affected ankle. Patients may complain of symptoms related to impingement, secondary to osteophyte and degenerative bony changes, and hypertrophied soft tissues with stair climbing, with walking on uneven surfaces, or with prolonged activity. Specifying the location and distinguishing features of ankle-related pain can help direct clinical testing and radiographic investigations.
Identification of the position of the ankle, hind foot, and forefoot during weight-bearing and phases of the gait cycle can help identify primary or secondary structural abnormalities. Altered positions of the ankle and foot may reflect underlying soft tissue pathologies such as tenosynovitis, tendon dysfunction, incompetent ligaments, neurological abnormalities, or associated degenerative joints of the ankle and foot. These structural differences may be unilateral or bilateral and should be explored as possible contributors to the patients’ spectrum, dysfunction, and presentation of ankle OA.
Tendons and ligaments of the affected ankle and foot should be examined for excursion, strength, and fatigue. Specific structures to examine on the lateral side of the ankle include, the peroneus longus and brevis, the lateral ankle ligamentous complex, and the syndesmosis. On the medial side, specific attention should be directed to the deltoid ligament, the tibialis posterior tendon, and the spring ligament. It is important to determine whether the interplay of ligament or tendon pathology is functional or mechanical in nature. Quality of the ligaments and tendons as well as ROM of the affected side should be compared to the contralateral side.
A complete neurological as well as a vascular exam should accompany any physical exam of the lower extremities. Patients with underlying systemic conditions, such as, diabetes mellitus or vascular insufficiency may be at an increased risk for complications such as, infection, nonunion, and wound healing issues. Identifying these potential risk factors may guide decision making for specific treatments in joint-preserving versus joint-sacrificing procedures within the ankle.
Although it is not always feasible, reviewing previous imaging and identification of possible complications and treatments to date can guide ongoing treatment decisions. Review of imaging with evolving symptoms and complaints is important to determine which structures of the ankle joint may be involved or becoming progressively involved.
Diagnosis
There are many facets to the clinical diagnosis of OA: clinical exam, patient complaints, and history can help point to the diagnosis. With the adjuncts of radiographic imaging and application to research-based ankle OA scales, treatment-specific goals can help address the underlying stage of OA of the ankle.
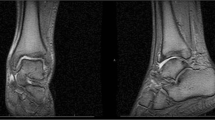
Radiographic evaluation should begin with weight-bearing anteroposterior, lateral, and mortise (oblique) views of the ankle (Fig. 5.1a–c). Weight-bearing radiographs of the ankle are essential to observe the natural joint reference contact relationships of the ankle and supporting hind and midfoot joints. The Saltzman hind foot alignment view is helpful for the evaluation of hind foot deformity. Standing AP hip to ankle views (4 ft standing) can also be helpful in assessing generalized limb alignment. Additional imaging studies, such as, computed tomography (CT) scans are helpful for assessing bone morphology and for the preoperative mapping of size, shape, and quantity of osteophytes or loose bodies. Magnetic resonance imaging (MRI) can define surrounding soft tissue structures, including tendons and ligaments. MRIs can also help determine cartilage quantity of the ankle joint, including the presence of osteochondral defects.
Positive imaging findings should correlate with clinical findings. Common radiographic signs associated with OA, include, formation of osteophytes, associated bone cysts, subchondral sclerosis, and joint space narrowing (JSN). Painful impingement at the ankle joint on dorsiflexion can be caused by osteophytes at the anterior joint margin. These spurs may be related to OA but can also be seen in athletes, especially those involved in kicking sports [31].
There have been many scales and tools developed to quantify the degree of OA of the ankle. Although many of the scales have been applied and revised, a current scale to determine the stages of ankle OA and appropriate treatments has been developed by the Canadian Foot and Ankle Society (COFAS). This tool was designed to be a simple and reliable tool to be used for arthritis stratification and outcome comparison in research, being a representation of the local anatomic conditions that may affect outcome and surgical decisions, not applicable to patients who are not eligible for a joint replacement [32]. Although it does not take into account patient factors, it is a valuable and useful tool for surgeons to utilize as a platform for decision making for nonsurgical and surgical treatment options for the patient with ankle OA (Table 5.1).
Nonsurgical Treatment/Foot and Ankle Care
First-line treatment in many orthopedic conditions is nonsurgical treatment. Due to the pathologies involved in the development of ankle OA, different populations may require different nonoperative treatment options; they should be offered for a minimum of 6 months for all older patients. However, early discussions among young and active patients with mild, moderate, and occasionally even advanced asymmetric ankle OA should occur more expediently, as certain joint-preserving treatment may help delay the progression of joint degeneration [33].
Successful conservative care is dependent on the stage of the ankle OA and the patients’ age and motivation. When choosing between conservative and joint-sparing/joint-sacrificing treatment, the extent of subchondral bone exposed and the time over which the OA has advanced are factors that should be considered. Patients with only little exposure of subchondral bone and slow OA progression will likely respond better to conservative treatment.
There are several modes of nonoperative and conservative treatment. Some options have research examined benefits, while others are newer therapies that lack concrete evidence of the benefits. Therapies include activity modification, shoe wear modification, weight loss, the use of anti-inflammatories, bracing, and physical therapy. These nonoperative treatments immobilize or off-load the joint to improve symptoms. Newer modalities include intra-articular injections, such as, hyaluronate viscosupplementation to help reduce joint inflammation and pain and assist in lubrication.
These newer modalities remain popular in the orthopedic literature as a clear determination of efficacy remains undefined. Clinically, a benefit of chondroitin or glucosamine for ankle OA has not yet been proven. In ankle OA, viscosupplementation demonstrated evidence for significant improvement after 1 and 6 months of five weekly injections in a prospective randomized double-blind trial [34]. A randomized control trial (RCT) was done by Witteveen et al. [35] of 70 patients who received HA injection into the joint under fluoroscopy versus distraction in patients with severe OA. There is no significant difference between the two injection methods regarding any of our formulated outcome measures. Considering the substantial amount of possible extra-articular injections prior to fluoroscopic control with both techniques, the use of contrast-aided fluoroscopy for injecting the ankle with severe OA, anterolateral or anteromedial osteophytes, is advisable.
There is no evidence of the efficacy of protein-rich plasma for ankle OA in the literature. Furthermore, the efficacy of intra-articular corticosteroid injections in the osteoarthritic ankle has not been studied; most clinical studies have involved knee OA.
Additional oral conservative treatment for OA includes the use of nonsteroidal anti-inflammatory medications or drugs (NSAIDs) [36]. They can be used as a temporary measure for control of intermittent pain, inflammation, and symptoms. However, many older individuals may have other medical conditions, such as, cardiac and respiratory disorders, that may interact with these medications and preclude their use.
Physical therapy and activity modification can be effective in addressing the loss of mobility in ankle OA; muscle strength during dorsiflexion and plantar flexion in individuals with ankle arthritis has been found to be decreased [37]. Therapy programs for the nonoperative management of ankle arthritis should have a focus on lower extremity strengthening, proprioception, and gait training.
Orthoses and shoe modifications can provide effective pain alleviation, improve quality of life, and postpone total ankle replacement or ankle arthrodesis in patients affected by advanced ankle arthritis with or without deformity [38]. The Ankle Foot Orthosis (AFO) is used to address pathology at the level of the ankle joint during the stance phase of gait [39].
Surgical Treatments
Conservative treatment should be the first-line treatment in ankle OA. However, many individuals fail to alleviate their symptoms of pain and limited mobility despite their best efforts. Although conservative treatment should be attempted, there may be a limit to its efficacy, and surgical management of ankle OA may be considered.
The goals of surgical management remain directed toward a pain-free ankle joint. Although in many of the surgical options, joint motion may be sacrificed to achieve this goal; joint-sparing procedures may provide options for sufficient pain relief while allowing ankle motion to remain. Treatment, joint-sparing versus joint-sacrificing, depends on many factors including patient age, patient preference, cartilage quality and quantity, and other systemic conditions.
Severe ankle OA treatments are usually joint sacrificing in nature, including total ankle arthroplasty and ankle arthrodesis. Mild to moderate OA in a younger patient may be treated by joint-preserving surgery, such as arthroscopic debridement, osteochondral repair, ligament and tendon reconstruction, and osteotomies.
Arthroscopic Debridement/Osteophyte Resection
With any injury, the cartilage of the ankle joint may be affected. Radiographic investigations, such as, MRIs can help to provide information about the cartilage of the ankle joint. Despite the emerging role of three-dimensional imaging studies, ankle arthroscopy is considered the gold standard in determining the true extent of cartilage damage in the ankle joint [40].
Diagnostic arthroscopy also has a role in the prognostication of OA development as a result of trauma [41]. Glazebrook [42] and colleagues performed a systematic review of the benefits of ankle arthroscopy treatment in ankle injuries and posttraumatic arthritis. This systematic review found a general trend of improved postoperative outcomes in these case series in patients with soft tissue impingement compared with bony impingement and increasingly poor results with increasing degree of ankle OA. Although evidence is limited, arthroscopic debridement has shown benefits in the treatment of arthritic disorders that primarily involve synovium of the ankle joint including RA, localized pigmented villonodular synovitis, and hemophilic arthropathy [41]. It is, however, important to assess alignment prior to arthroscopy, as this may need to be additionally addressed so that the mechanical forces for creating osteophytes may be altered.
Indications for ankle arthroscopy for ankle OA include diagnostic arthroscopy and loose body removal, anterior ankle impingement, and early stage ankle OA with intact joint space.
With any surgical procedure, there are postoperative risks and complications. Review of ankle arthroscopy complications by Deng et al. [43] revealed that the most common complication was cutaneous nerve injury, which involved nine cases (3.46 %), and localized superficial infection, which involved eight cases (3.08 %). Injury to the superficial peroneal nerve accounted for five of the cutaneous nerve injuries.
Allograft Resurfacing
Osteochondral lesions can be seen as a local degeneration of the ankle joint, can be the result of injury to the tibiotalar joint from direct trauma, or can be seen as a secondary injury due to a severe ankle sprain. Within the foot and ankle, the talar dome is the most common location for development of an osteochondral lesion [44], termed an osteochondral lesion of the talus, and can be degenerative or posttraumatic. Surgical treatment techniques can be categorized into non-tissue transplantation and tissue transplantation methods. Potential options for repair or reconstruction, include, procedures such as arthroscopic debridement combined with microfracture and/or drilling, autologous chondrocyte implantation, and the osteochondral autograft transplant system (OATS)/mosaicplasty. However, each of these has limitations in the treatment of large lesions for which the success rates are poor and tissue available for harvest and implantation is limited by risk of harvest-site morbidity [44].
Treatment of osteochondral lesions may be a temporary measure to prevent further joint degeneration, although most studies demonstrate little long-term success. Despite the fact that in theory, this procedure is a potentially desirable option for a young patient with advanced ankle arthritis, it has a high level of technical difficulty and complications with the reported results showing a high failure rate [44].
Supramalleolar Osteotomy
In younger patients with mild to moderate ankle OA, goals of treatment include preserving the joint while addressing altered joint mechanics as a result of injury. Supramalleolar osteotomy (SMO), reported to be an effective realignment surgery in patients with varus ankle OA, is performed to restore orientation and axial alignment of the ankle. It has been shown to reduce pain and improve function and radiological signs of arthritis, as well as postpone fusion and replacement surgery in these patients [45].
The main indication for SMOs is asymmetric ankle OA with concomitant valgus or varus deformities and a partially (at least 50 %) preserved tibiotalar joint surface [46].
SMO is an option for some surgeons to consider but is based on surgeon experience. In patients with supramalleolar valgus or varus deformities, the surgeon can choose from four surgical options: medial closing wedge osteotomy (anti-valgus osteotomy), medial opening wedge osteotomy, lateral closing wedge osteotomy (anti-varus osteotomy), and dome osteotomy. Rotational and translational osteotomies can also be performed where necessary. In some cases where there is a sagittal (anterior–posterior) deformity, various osteotomies can be performed to correct the deformity at the center of rotation and angulation [47].
The clinical effectiveness of SMOs can vary from patient to patient. A study by Egloof et al. demonstrated a decrease in tibial and talar subchondral bone plate density distribution after supramalleolar medial closing wedge osteotomy in patients with valgus ankle OA; our patients reported a decrease in pain and most of them were satisfied with the procedure. SMO should be considered a surgical treatment option for ankle OA in certain patients with remaining joint space.
Total Ankle Arthroplasty
Total ankle arthroplasty was designed as an alternative to arthrodesis of the ankle joint in the treatment of OA. The design of this prosthetic joint implant has continued to develop since its inception in the early 1970s, with several generations of prosthetic templates continuing to evolve (Fig. 5.1d, e).
Total ankle arthroplasty was developed to reduce pain and retain motion of the ankle joint in patients with OA, much like its total hip and knee counterparts. Total knee and hip arthroplasties remain one of the most common surgical procedures in the modern orthopedic theater. While arthrodesis is still considered the “gold standard” for treatment of end-stage ankle arthritis, progression of adjacent joint arthrosis and diminished gait efficiency has led to a resurgence of interest in ankle arthroplasty. Long-term outcome studies for total ankle replacement found excellent or good results in 82 % of patients who received a newer generation ankle device compared with 72 % if undergoing ankle fusion [48].
The optimal patient is older (>50 years old), with end-stage ankle arthrosis, nonobese, and with low physical demands [49]. Patients with posttraumatic ankle arthrosis, especially younger patients, seem to have worse outcomes and are more likely to undergo revision than patients with other causes of arthritis [50].
Complications, such as, infection required revision for implant failure with positive radiographical anomalies in 18 AES total ankle arthroplasties. In this study by Rodgiuez et al. [51], the most frequently encountered complication was asymptomatic osteolysis, which was best detected on CT scan compared to conventional X-rays. For now, the osteolysis leads to only a very low frequency revision. It was most frequently seen around the tibial component on X-ray and in the talar body on CT scan. Therefore, it is recommended to repeat CT scans every 6 months to monitor for osteolysis and prosthesis stability.
Symptomatic improvement can vary from patient to patient depending on preoperative symptoms. However, many patients may prefer maintaining some movement of the affected joint choosing arthroplasty versus arthrodesis. The gait patterns of patients following three-component, mobile-bearing total ankle arthroplasty more closely resembled normal gait when compared with the gait patterns of patients following arthrodesis [52].
In conclusion, the intermediate-term clinical outcomes of ankle replacement and arthrodesis in a diverse cohort of patients were comparable, even when patients who required revision ankle replacement were included; however, the rates of additional surgery and major complications were higher after ankle replacement than after arthrodesis [53].
Ankle Arthrodesis
Another treatment option for ankle OA includes ankle arthrodesis. Debilitating posttraumatic arthritis is the most common indication for arthrodesis and is widely considered the gold standard. It is also indicated for pain and deformity secondary to previous infection, osteochondral defects, osteonecrosis of the talus, OA, inflammatory arthropathies, and RA [48].
While ankle arthrodesis, otherwise known as ankle fusion, sacrifices any remaining ankle joint motion, the results are predictable with regard to consistent pain relief once fusion is achieved. Assessment of postoperative fusion is based on clinical and radiographic means, such as, CT.
In most cases, good and excellent intermediate-term results are reported for modern arthrodesis techniques. Long-term reliability, however, is questioned because ankle fusion has been associated with premature arthritis, pain, and dysfunction of the adjacent hind foot joints. Waters and coworkers reported a 16 % decrease in gait velocity, 3 % increase in oxygen consumption, and 10 % decrease in gait efficiency after ankle fusion [54]. In a long-term follow-up study of 23 patients evaluated over an average of 22 years after tibiotalar arthrodesis, Coester and associates [55] demonstrated progressive degenerative changes of ipsilateral subtalar (91 %), talonavicular (57 %), and tarsometatarsal (41 %) joints. The progressive arthritis in these joints led to ipsilateral foot pain and limitations in ambulation and activities of daily living. Pseudoarthrosis rates approach 50 % in some studies, and appropriate position for fusion is often difficult to obtain in cases with bone loss. With the advent of arthroscopic ankle fusion, there are the potential benefits of improved wound and bony healing, due to preservation of the soft tissue envelope and diminished soft tissue stripping, and potential improved outcomes.
Several patient factors can contribute to post-op complications including nonunion. Factors associated with nonunion, included, fracture type, evidence of avascular necrosis, infection, major medical problems, and open injuries. Factors that were not associated with nonunion, included, age, past history of subtalar or triple arthrodesis, and technique [56].
Joint fusion in foot and ankle surgery may allow a high activity level, but degeneration of the neighboring joints occurs in up to 50 % of cases after 7–8 years and up to 100 % of cases after 22 years [57].
The debate continues over which joint-sacrificing procedure – total ankle arthroplasty or ankle arthrodesis – is best to address ankle OA. A recent systematic review was done by Jordon et al. [58] to determine how end-stage ankle OA should be managed. Although half of the reviewed studies report some functional improvement following total ankle replacement, the lack of high quality evidence limits a definitive conclusion being drawn. Insufficient evidence is available to decide whether total ankle replacement or ankle arthrodesis improves functional outcomes and further research in the form of robust RCTs is indicated.
Conclusions
Ankle OA is a common pathology among young adults and older populations. There are many etiologies contributing to the prevalence of this disease, although posttraumatic OA is the primary cause. Recognizing the uniqueness of the properties of the ankle joint, both biology and biomechanics, is important for determination of nonoperative versus operative treatment. Many nonoperative treatments may be applicable to particular populations; however, many still lack evidence for efficacy. Operative therapies should be attempted after a trial of conservative therapy, although conversations with younger patients about joint-sparing procedures should take place early. Joint-preserving and sacrificing procedures may offer symptom relief but are associated with increased risks and complications. Pathogenesis and associated treatments of ankle OA remains a topic of interest in orthopedic research and will continue to provide additional information to address this common disease. Patient-tailored approaches with biologics and mechanical realignment may be the key focus for future research, as it may allow for patient-specific joint-preserving modalities.
References
Saltzman CL SM, Blanchard GM, Huff T, Hayes A, Buckwalter JA, Amendola A. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–6.
Glazebrook MP, Daniels T, Younger A, Foote CJ, Penner M, Wing K, Lau J, Leighton R, Dunbar M. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008;90(3):499–505.
Snedeker JG, Wirth SH, Espinosa N. Biomechanics of the normal and arthritic ankle joint. Foot Ankle Clin. 2012;17(4):517–28.
Herrero-Beaumont G, Roman-Blas JA, Castañeda S, Jimenez SA. Primary osteoarthritis no longer primary: three subsets with distinct etiological, clinical, and therapeutic characteristics. Semin Arthritis Rheum. 2009;39(2):71–80.
Zaidi R, Cro S, Gurusamy K, Siva N, Macgregor A, Henricson A, Goldberg A. The outcome of total ankle replacement: a systematic review and meta-analysis. Bone Joint J. 2013;95(11):1500–7.
Shibuya N, Davis M, Jupiter DC. Epidemiology of foot and ankle fractures in the United States: an analysis of the National Trauma Data Bank (2007 to 2011). J Foot Ankle Surg. 2014;53(5):606–8.
Thomas RH, Daniels TR. Ankle arthritis. J Bone Joint Surg Am. 2003;85(5):923–36.
Bartonícek J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat. 2003;25(5–6):379–86.
Dubin A. Gait: the role of the ankle and foot in walking. Med Clin North Am. 2014;98(2):205–11.
Coughlin MJ, Saltzman CL, Roger A. Mann, Mann’s surgery of the foot and ankle. Philadelphia: Elsevier Saunders; 2014.
Riordan E, Little C, Hunter D. Pathogenesis of post-traumatic OA with a view to intervention. Best Pract Res Clin Rheumatol. 2014;28(1):17–30.
Nakasa T, Adachi N, Kato T, Ochi M. Correlation between subchondral bone plate thickness and cartilage degeneration in osteoarthritis of the ankle. Foot Ankle Int. 2014;35(12):1341–9.
Simon TM, Jackson D. Articular cartilage: injury pathways and treatment options. Sports Med Arthrosc. 2006;14(3):146–54.
Eger W, Schumacher B, Mollenhauer J, Kuettner KE, Cole AA. Human knee and ankle cartilage explants: catabolic differences. J Orthop Res. 2002;20(3):526–34.
Egloff C, Hügle T, Valderrabano V. Biomechanics and pathomechanisms of osteoarthritis. Swiss Med Wkly. 2012;19(July):142.
Dattani R, Patnaik S, Kantak A, Srikanth B, Selvan TP. Injuries to the tibiofibular syndesmosis. J Bone Joint Surg Br. 2008;90(4):405–10.
Rodgers MM. Dynamic biomechanics of the normal foot and ankle during walking and running. Phys Ther. 1998;68(12):1822–30.
Ritterman SA, Fellars T, Digiovanni CW. Current thoughts on ankle arthritis. R I Med J. 2013;96(3):30–3.
Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467(7):1800–6.
Mündermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52(9):2835–44.
Broos PL, Bisschop A. Operative treatment of ankle fractures in adults: correlation between types of fracture and final results. Injury. 1991;22:403–6.
Lübbeke A, Salvo D, Stern R, Hoffmeyer P, Holzer N, Assal M. Risk factors for post-traumatic osteoarthritis of the ankle: an eighteen year follow-up study. Int Orthop. 2012;36(7):1403–10.
Yablon I. The key role of the lateral malleolous in displaced fractures of the ankle. J Bone Joint Surg Am. 1977;59(2):69–73.
Mandi D. Ankle fractures. Clin Podiatr Med Surg. 2012;29(2):155–86.
Schmid T. Conservative treatment of asymmetric ankle arthritis. Foot Ankle Clin. 2013;18(3):437–48.
Bergkvist D. Obesity in orthopedic patients. Surg Obes Relat Dis. 2009;5(6):670–2.
Bostman O. Body mass index of patients with elbow and ankle fractures requiring surgical treatment. J Trauma. 1994;37(1):62–5.
Stufkens SA, Knupp MM, Horisberger M, Lampert C, Hintermann B. Cartilage lesions and the development of osteoarthritis after internal fixation of ankle fractures. J Bone Joint Surg Am. 2010;92(2):279–86.
Hintermann MB, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30(3):402–9.
Brown TD, Johnston R, Saltzman CL, Marsh JL, Buckwalter JA. Posttraumatic osteoarthritis: a first estimate of incidence, prevalence, and burden of disease. J Orthop Trauma. 2006;20(10):739–44.
Koulouris MG, Morrison WB. Foot and ankle disorders: radiographic signs. Semin Roentgenol. 2005;40(4):358–79. Elsevier Inc.
Krause FG, Di Silvestro M, Penner MJ, Wing KJ, Glazebrook MA, Daniels TR, Lau JT, Younger AS. The postoperative COFAS end-stage ankle arthritis classification system: interobserver and intraobserver reliability. Foot Ankle Spec. 2012;5(1):31–6.
Van Valburg AA, Van Roermund PM, Marijnissen ACA, Van Melkebeek J, Lammens J, Verbout AJ, Bijlsma JWJ. Joint distraction in treatment of osteoarthritis: a two-year follow-up of the ankle. Osteoarthritis Cartilage. 1999;7(5):474–9.
Salk RS, Chang TJ, D’Costa WF, Soomekh DJ, Grogan KA. Sodium hyaluronate in the treatment of osteoarthritis of the ankle: a controlled, randomized, double-blind pilot study. J Bone Joint Surg Am. 2006;88(2):295–302.
Witteveen AG, Sierevelt IN, Blankevoort L, Kerkhoffs GM, van Dijk CN. Intra-articular sodium hyaluronate injections in the osteoarthritic ankle joint: effects, safety and dose dependency. Foot Ankle Surg. 2010;16(4):159–63.
Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis: an update with relevance for clinical practice. Lancet. 2011;377(9783):2115–26.
Shih LY, Wu JJ, Lo WH. Changes in gait and maximum ankle torque in patients with ankle arthritis. Foot Ankle Int. 1993;14(2):97–103.
John S, Bongiovanni F. Brace management for ankle arthritis. Clin Podiatr Med Surg. 2009;26(2):93–7.
Lin RS, Gage JR. The neurological control system for normal gait. J Prosthetics Orthot. 1989;2(1):1–13.
Sugimoto K, Takakura Y, Okahashi K, Samoto N, Kawate K, Iwai M. Chondral injuries of the ankle with recurrent lateral instability: an arthroscopic study. J Bone Joint Surg Am. 2009;91(1):99–106.
Phisitkul P, Tennant JN, Amendola A. Is there any value to arthroscopic debridement of ankle osteoarthritis and impingement? Foot Ankle Clin. 2013;18(3):449–58.
Glazebrook MA, Ganapathy V, Bridge MA, Stone JW, Allard JP. Evidence-based indications for ankle arthroscopy. Arthroscopy. 2009;25(12):1478–90.
Deng DF, Hamilton GA, Lee M, Rush S, Ford LA, Patel S. Complications associated with foot and ankle arthroscopy. J Foot Ankle Surg. 2012;51(3):281–4.
Winters BS, Raikin SM. The use of allograft in joint-preserving surgery for ankle osteochondral lesions and osteoarthritis. Foot Ankle Clin. 2013;18(3):529–42.
Kim YS, Youn HK, Kim BS, Choi YJ, Koh YG. Arthroscopic evaluation of persistent pain following supramalleolar osteotomy for varus ankle osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2014;1(8).
Barg A, Pagenstert GI, Horisberger M, Paul J, Gloyer M, Henninger HB, Valderrabano V. Supramalleolar osteotomies for degenerative joint disease of the ankle joint: indication, technique and results. Int Orthop. 2013;37(9):1683–95.
Wukich DK, Belczyk RJ. An introduction to the Taylor spatial frame for foot and ankle applications. Oper Tech Orthop. 2006;16(1):2–9.
John JY, Sheskier S. Total ankle replacement. Bull Hosp Joint Dis. 2014;72(1):120–8.
Saltzman C. Total ankle replacement – State of art. Instr Course Lect. 1999;49:263–8.
Easley ME, Vertullo CJ, Urban WC, Nunley JA. Total ankle arthroplasty. J Am Acad Orthop Surg. 2002;10(3):157–67.
Rodriguez D, Bevernage BD, Maldague P, Deleu PA, Tribak K, Leemrijse T. Medium term follow-up of the AES ankle prosthesis: high rate of asymptomatic osteolysis. Foot Ankle Surg. 2010;16(2):54–60.
Singer S, Klejman S, Pinsker E, Houck J, Daniels T. Ankle arthroplasty and ankle arthrodesis: gait analysis compared with normal controls. J Bone Joint Surg Am. 2013;95(24):e191–1.
Daniels TR, Younger AS, Penner M, Wing K, Dryden PJ, Wong H, Glazebrook M. Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg Am. 2014;96(2):135–42.
Waters RL, Barnes G, Husserl T, Silver L, Liss R. Comparable energy expenditure after arthrodesis of the hip and ankle. J Bone Joint Surg Am. 1998;70(7):1032–7.
Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83(2):219.
Frey C, Halikus NM, Vu-Rose T, Ebramzadeh E. A review of ankle arthrodesis: predisposing factors to nonunion. Foot Ankle Int. 1994;15(11):581–4.
Takakura Y, Tanaka Y, Sugimoto K, Akiyama K, Tamai S. Long term results of arthrodesis for osteoarthritis of the ankle. Clin Orthop Relat Res. 1999;361:178–85.
Jordan RW, Chahal GS, Chapman A, Jordan RW, Chahal GS, Chapman A. Is end-stage ankle arthrosis best managed with total ankle replacement or arthrodesis? a systematic review. Advances in orthopedics. 2014.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Lau, J., Veljkovic, A.N., Farrugia, P. (2015). Ankle Osteoarthritis. In: Kapoor, M., Mahomed, N. (eds) Osteoarthritis. Adis, Cham. https://doi.org/10.1007/978-3-319-19560-5_5
Download citation
DOI: https://doi.org/10.1007/978-3-319-19560-5_5
Publisher Name: Adis, Cham
Print ISBN: 978-3-319-19559-9
Online ISBN: 978-3-319-19560-5
eBook Packages: MedicineMedicine (R0)