Abstract
Ankle osteoarthritis is a growing problem in health care, with 1 % of the world’s adult population being affected. Previous trauma is the most common origin of ankle osteoarthritis. In the current literature, there is no evidence whether sport activities accelerate or prevent the development of ankle degenerative changes. Different surgical approaches have been described for the treatment of ankle osteoarthritis based on osteoarthritis stage. The treatment options range from joint preserving procedures (e.g. open or arthroscopic debridement, joint distraction arthroplasty, and supramalleolar osteotomies) to joint sacrificing procedures (e.g. total ankle replacement and ankle arthrodesis). While numerous studies have addressed clinical and radiographic outcomes in patients who underwent surgery for ankle osteoarthritis, there is scant literature addressing the role of sports participation of patients with ankle osteoarthritis before and after surgical treatment. In general, low impact sports can be recommended postoperatively. However, further prospective clinical studies are needed to identify whether sport activities can be identified as risk factors for treatment failure or for poorer postoperative results.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Ankle
- Ankle osteoarthritis
- Sport
- Sport activities
- Ankle osteoarthritis etiology
- Joint-preserving procedure
- Joint sacrificing procedures
- Supramalleolar osteotomy
- Total ankle replacement
- Ankle arthrodesis
Etiology of Ankle Osteoarthritis
Ankle osteoarthritis (OA) is a constantly growing problem in world health care and should not be underestimated [1]. More than 1 % of the entire world’s adult population is affected by ankle OA [2]. The mental and physical disability in patients suffering from end-stage ankle OA is at least as severe as that associated with end-stage hip OA [2].
In the current literature there are clinical and epidemiologic studies which address the etiology of ankle OA [1, 3]. Valderrabano et al. [4] evaluated the distribution of etiologies in 390 consecutive patients (406 ankles) with end-stage ankle OA. Posttraumatic ankle OA was observed in the majority (78 %) of patients. Malleolar fractures (type AO 44) were the most common injuries (39 %), followed by ankle ligament lesions (16 %), and tibial plafond fractures (type AO 43, 14 %). Secondary, atraumatic OA was observed in 13 % of patients including patients with rheumatoid arthritis, hemochromatosis, hemophilia, clubfoot etc. Primary OA was the rarest etiology, with 9 % of patients affected. Patients with posttraumatic ankle OA were significantly younger than patients with other ankle OA etiologies [4]. Similar findings were found in another epidemiologic study by Saltzman et al. [5]. In this study, 639 consecutive patients with Kellgren grade 3 or 4 ankle OA who presented to the University of Iowa Orthopaedic Foot and Ankle Surgery service between 1991 and 2004 were included. The majority of patients (70 %) had posttraumatic ankle OA, with rotational ankle fractures and recurrent instability being the most common causes, at 37 % and 15 %, respectively. Primary and secondary OA was diagnosed in 22 % and 8 %, respectively [5]. Wang et al. [6] analyzed radiographic hindfoot alignment in 226 consecutive patients with end-stage ankle OA who underwent total ankle replacement (TAR) or ankle arthrodesis. The most common etiology in this cohort was posttraumatic, with 71.2 % of patients reporting previous fractures or recurrent ligament injuries. Primary ankle OA was diagnosed in 5.6 % of patients. Secondary ankle OA was seen in 23.2 %, including OA due to pes planovalgus deformity, rheumatoid arthritis, clubfoot or other congenital foot deformity, postinfectious arthritis, Charcot-Marie-Tooth disease, and haemophilic arthritis [6].
Sport as Risk Factor for the Development of Ankle Osteoarthritis
In the current literature, there is a controversial discussion whether sport activities play a positive or negative role in the development of ankle OA. Based on the available literature, a causal link between pediatric sports injuries and ankle OA development is possible [7].
In the 1970s, Vincelette et al. [8] compared degenerative changes of the foot and ankle between professional soccer players and controls. Fifty-nine professional football players, with an average age of 23 years (19–27 years), with an average football experience of 9.5 years (2–15 years) were included. The group evaluated 367 radiographs of soccer players and 377 radiographs of control patients. Radiographs were classified as abnormal if they showed signs of OA, periarticular ossifications, dorsal exostosis of the talus, or distal interosseous ligament calcification. Among soccer players, mild findings were found in 10 % and severe findings were found in 90 % of radiographs. In the control group, 22 % had mild findings and 4 % had severe findings regarding radiographic degenerative changes [8].
In 1979, Adams [9] examined 56 soccer players and six coaches (who were former professional players) clinically and radiographically at one football club. All 62 patients showed some signs of ankle pathology. However, the overall incidence of radiographic OA was only 1.6 % [9].
Hellmann et al. [10] performed radiographic analysis of six amateur athletes who had severe atypical degenerative joint disease. One of the patients presented with right ankle pain. The 20-year-old male participated in cross-country motorcycling for several years. Radiographs and computed tomography showed degenerative changes of the subtalar joint in this patient, most likely resulting from extensive sport activities [10].
Kujala et al. [11] investigated the cumulative 21 year incidence of admission to a hospital for OA of the hip, knee, and ankle in former elite athletes and control subjects. In total, 2,049 male athletes who had represented Finland in international events from 1920 to 1965 and 1403 controls were included into this national population based study. The cumulative incidence of admission to a hospital among the former athletes was 3.3 % (95 % CI 2.6–4.1 %), 2.4 % (95 % CI 1.8–3.2 %), and 0.4 % (95 % CI 0.2–0.8 %) for hip, knee, and ankle, respectively. These values were substantially higher than values observed in controls: 1.4 % (0.9–2.2 %), 1.3 % (95 % CI 0.8–2.0 %), and 0 % for hip, knee, and ankle, respectively [11].
The potential influence of long-term, high-intensity physical training on early ankle OA has been investigated in a retrospective study by Knobloch et al. [12]. Twenty-seven track and field long-distance runners and orienteers and nine bobsledders with a mean age of 42 years were compared with a control group of 23 healthy men with a mean age of 35 years. The long-distance runners had a higher prevalence of early ankle OA, however, the multivariate analysis demonstrated that not the sport itself, but rather age and ankle instability were significantly correlated with the development of ankle OA [12].
In their comparative study, Gross and Marti [13] addressed the influence of long-term, professional volleyball playing on the development of early ankle OA. A group of 22 former elite volleyball players with a mean age of 34 ± 6 years who had played for at least three years in the highest league in Switzerland was compared to 19 healthy controls with a mean age of 35 ± 6 years. The majority of players (20 of 22) had lateral ligament lesions, and eight of these required surgery. Radiographic evidence of ankle OA was found in 19 of 22 volleyball players, but only in two of 19 controls. The multiple regression analysis revealed that positive anterior drawer test and subjective instability were statistically significant and independent risk factors for radiographic OA [13].
Zinder et al. [14] evaluated the prevalence of ankle OA following ankle sprains in a cohort of retired professional football players. In total, 2,552 retired professional football players completed a general health questionnaire. Of them, 448 (17.69 %) reported at least one severe ankle sprain in the past. Forty patients developed significant ankle OA. Compared to players without a history of sprains, the injured cohort had a 2.3 times higher prevalence of ankle OA [14].
Kuijt et al. [15] performed a systematic review of the recent literature to investigate the prevalence of knee and/or ankle OA in former elite soccer players. Only four studies were included in the final analysis. The prevalence of degenerative joint disease was found to be between 40 and 80 % for the knee and between 12 and 17 % for the ankle. The prevalence of knee and ankle OA in the former players was substantially higher compared to the general population. However, only the prevalence of OA was measured in this study. Therefore, the authors mentioned the need of further studies based on a health surveillance program to be able to identify players at risk for OA [15].
Recently, Gouttebarge et al. [16] published a systematic review to explore the OA prevalence in former elite athletes from team and individual sports. In total, 15 studies were included in the review. Prevalence of ankle OA was reported only in one study [17]. In this study, by Schmitt et al. [17], which included 40 former elite high jumpers, ankle OA was found in 2.5 %, with a mean age of 41.8 years at time of diagnosis.
In 2015, Iosifidis et al. [18] investigated the prevalence of lower extremity clinical and radiographic OA in a comparative study. The study compared 218 former elite male athletes from various sports (soccer, volleyball, martial arts, track and field, basketball, and skiing) with 181 controls. The prevalence of clinical OA was similar in both groups, with 15.6 % prevalence for former elite athletes and 14.4 % for controls. However, the prevalence of radiographic OA was significantly higher in the former athletes (36.6 %) compared to the controls. Therefore, the radiographic signs of OA may precede the clinical onset of OA. In both groups, several risk factors for OA development were identified: age, body mass index, and occupation [18].
Ankle Instability as Risk Factor for the Development of Ankle Osteoarthritis
Lateral ankle sprain (LAS) is one of the most common sports injuries in the world. LAS accounts for up to 30 % of all athletic injuries and up to 60 % of injuries in certain sports [19, 20]. It is one of the most common injuries in basketball [21–28], soccer [29–41], football [42–47], and tennis [48–51]. One LAS occurs per 10,000 person-days, and an estimated 2 million acute LAS injuries occur each year in the United States [52]. LAS injuries occur most commonly between 15 and 19 years of age [52], and there is no statistically significant difference in LAS incidence between males and females [52–55]. Ankle injuries, including LAS, are among the most common injuries in children and youth sports, accounting for up to one fourth of all injuries sustained by high-school athletes during the 2005–2006 school year [7, 56]. Swenson et al. [57] analyzed the sports injury data for the 2005 through 2008 academic years from a nationally representative sample of 100 United States high schools. The injuries most often involved the ankle (19 %), knee (14.5 %) and head/face (10.7 %). Notably, the ankle was the most frequently diagnosed site of recurrent injuries at 28.3 % [57].
Up to 40 % of all patients with LAS develop chronic ankle instability (CAI) [58–60]. Different intrinsic and extrinsic factors have been identified as risk factors for development of CAI after LAS: high body mass index, high height, and severity of initial ankle sprain [61, 62]. As mentioned above, CAI from repetitive ankle sprains is an important etiology of ankle OA – up to 20 % of all ankle OA cases and up to 30 % of all patients with posttraumatic ankle OA [4, 5, 63]. Different arthroscopic studies demonstrated a high number of chondral injuries in patients with a prolonged history of ankle instability [64–67].
Several studies have investigated the pathomechanism of ankle instability leading to ankle OA [68–71]. McKinley et al. [71] used an ankle cadaveric model to measure incongruity and instability-associated changes in contact stress directional gradients in the tibiotalar joint. An increase of up to 100 % was observed in unstable specimens [71].
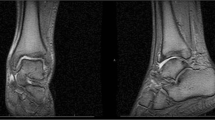
Caputo et al. [69] used magnetic resonance imaging (MRI) and orthogonal fluoroscopy to perform kinematic measurements in nine patients with lateral ankle instability and, in particular, insufficient anterior talofibular ligaments. Several significant changes were observed as compared with the intact contralateral ankles: increase in anterior translation of 0.9 ± 0.5 mm, increase in internal rotation of 5.7° ± 3.6°, and increase in superior translation of 0.2 ± 0.2 mm. These findings [69] may explain the degenerative changes often observed on the medial talus in patients with lateral CAI [65, 72, 73].
Bischof et al. [68] used three-dimensional MRI models and biplanar fluoroscopy to evaluate in vivo cartilage contact strains in patients with isolated lateral ankle instability. In total, seven patients were included in this study. The contralateral healthy side was used as a control to measure the magnitude and location of peak cartilage strain. The unstable ankles demonstrated significantly increased peak strain with 29 ± 8 % vs. 21 ± 5 %. Furthermore, the location of peak strain in the unstable ankles was translated anteriorly by 15.5 ± 7.1 mm and medially by 12.9 ± 4.3 mm. The authors found a correlation between the translation of peak strain and the location of clinically observed degenerative changes of the tibiotalar joint [68].
Recently, Golditz et al. [70] investigated the impact of functional ankle instability on the development of early cartilage damage using quantitative T2-mapping MRI. In total, 36 patients were included, and they were classified into one of three groups: functional ankle instability, ankle sprain “copers” (persons with initial sprains, but without residual instability), and controls (persons without a history of ankle injuries). The authors performed zonal region-of-interest T2-mapping of the deep and superficial layers of the talar and tibial cartilage. Significant to highly significant differences in T2-values in 11 of 12 regions were observed, demonstrating that functional instability causes substantially unbalanced loading in the tibiotalar joint. This, in turn, may result in early degenerative changes of the joint cartilage [70].
Valderrabano et al. [63] investigated the data from 30 patients (33 ankles) with ligamentous end-stage ankle OA. There were 23 male and seven female patients with a mean age of 58.6 years (33–78 years). Ligamentous lesions suffered during sports activities were the most frequent cause for ankle OA (55 %), followed by ankle sprains that occurred during normal daily activities (36 %), and sprains suffered at work (9 %). In 33 % of patients, the ankle injury occurred while playing soccer. In 28 ankles, the initial injury was a lateral ligament injury, in four ankles the medial ligaments were initially injured, and in one ankle a combined medial-lateral ligament injury was diagnosed. The overall mean latency time between the initial injury and development of ligamentous posttraumatic ankle OA was 34.3 years, with a range between 6 and 57 years. The survivorship rate for single ankle sprains was statistically worse than that for chronic recurrent sprains, with the average latency time of 25.7 and 38.0 years, respectively. Also, the survivorship rate for medial sprains was statistically worse than for lateral sprains with 27.5 and 35.0 years until the development of OA, respectively [63].
Treatment Options for Ankle Osteoarthritis
In the current literature, numerous treatment options have been described for ankle OA. In general, surgical treatments can be divided into joint-preserving and joint-sacrificing procedures (Fig. 33.1). The surgical indications and the choice of treatment for patients with various stages of ankle OA is complex and requires adequate experience in foot and ankle surgery.
Corrective Osteotomies
As mentioned above, the most common etiology for ankle OA is posttraumatic. Therefore, degenerative changes often develop asymmetrically with a concomitant varus or valgus deformity of the hindfoot [1, 6, 74, 75]. In patients with asymmetric ankle OA, a part of the tibiotalar joint remains preserved and free of degenerative changes. Thus, joint-sacrificing procedures like TAR or ankle arthrodesis may not be the most appropriate treatment options in this patient cohort [76]. In recent decades, realignment surgeries including supramalleolar osteotomies have evolved into valuable treatment options in patients with asymmetric ankle OA [77, 78]. The main indication for supramalleolar osteotomies is asymmetric ankle OA, with concomitant valgus or varus deformity, and a partially (at least 50 %) preserved tibiotalar joint surface [77–81] (Fig. 33.2). Recent literature demonstrates that the short- and mid-term results following realignment surgery are promising, with substantial pain relief and functional improvement observed postoperatively in the majority of patients [77, 78]. However, there is limited literature addressing the effect of corrective osteotomies on patients` ability to participate in sports activities.
Supramalleolar realignment surgery. (a, b) An osteochondroma was diagnosed and resected in a 15 year-old female patient by pediatric orthopaedic surgeons. (c) Three years later, the patient developed a painful supramalleolar valgus deformity with a medial distal tibial angle [180] of 96°, substantial shortening of the fibula according to Weber´s criteria [221], and valgus position of the heel on the Saltzman hindfoot alignment view [222]. The patient complained of 7/10 pain on a visual analog scale and restriction of sports and daily activities. (d) A supramalleolar closing-wedge tibial osteotomy and a corrective lengthening osteotomy of the fibula were performed. At 6-months follow-up, the patient reported substantial pain relief (1–2 on a visual analogue scale)
Takakura et al. [82] performed valgus opening wedge supramalleolar osteotomies in nine patients with a mean age of 35 years (12–61 years) with posttraumatic varus deformity of the ankle. Osseous union occurred within two months in eight patients and after six months in one patient. At the mean follow-up of 7.3 years, the range of motion of the ankle decreased in six patients and remained the same in three patients. However, none of the patients reported any limitation in daily activities. Moreover, four adolescent patients were able to participate in sports activities at school [82].
Harstall et al. [83] performed supramalleolar lateral closing wedge osteotomies in nine patients between the ages of 21–59 years, with varus ankle OA. The etiology of disease was posttraumatic in eight and childhood osteomyelitis in one. At the mean follow-up of 4.7 years, significant pain relief (American Orthopaedic Foot and Ankle Society (AOFAS) pain subscore change from 16 ± 8.8 preoperatively to 30 ± 7.1 postoperatively) and significant functional improvement (AOFAS hindfoot score change from 48 ± 16.0 preoperatively to 74 ± 11.7 postoperatively) was observed. However, only three patients were able to perform sports activities as desired [83].
Pagenstert et al. [84] analyzed a prospective case series of 35 consecutive patients with a mean age of 43 years (26–68 years) who underwent realignment surgery due to varus or valgus ankle OA. Significant pain relief (visual analog scale (VAS) change from 7 ± 1.6 preoperatively to 2.7 ± 1.6 postoperatively) and significant functional improvement (AOFAS hindfoot score change from 38.5 ± 17.2 preoperatively to 85.4 ± 12.4 postoperatively) were observed at the final follow-up of a mean of five years. The authors demonstrated that realignment surgery may increase sports activity (Sports Activity Level change from 1.3 ± 1.4 preoperatively to 1.8 ± 1.2 postoperatively, p = 0.02, and Ankle Activity Scale change from 25.7 ± 15 preoperatively to 68.1 ± 21 postoperatively, p = 0.0001). The types of sports activities that patients performed after realignment surgery were mostly low impact activities, like hiking, biking, swimming or golfing. However, jumping and running were reported as well. The rate of sports inactivity decreased from 43 % before surgery to 20 % at final follow-up. Actually, sports frequency in hours per week showed a weak and statistically insignificant correlation (r = 0.34, p = 0.054) with the symptom-related Ankle Activity Scale [84].
Hintermann et al. [85] performed a prospective study to analyze the outcome of 48 malunited pronation-external rotation ankle fractures treated by corrective supramalleolar osteotomy. At the mean follow-up of 7.1 years (2–15 years), patients reported significant pain relief (87.2 % of all patients were pain free and 12.8 % reported moderate pain with a mean VAS of 2.1 points) and significant functional improvement (AOFAS hindfoot score from 48 points [36–66] preoperatively to 86 points [64–100] postoperatively). However, the preoperative and postoperative range of motion of the ankle was comparable at 41.2° (30°–50°) and 40.1° (30°–50°), respectively. In total, 43 patients (89.6 %) returned to their former professional activity, and 34 (70.8 %) returned to their former sport activities. However, 11 patients did not participate in sport prior to their initial injury [85].
Mann et al. [86] published a retrospective study describing the results of opening medial tibial wedge osteotomy (plafond-plasty) as a novel surgical option for treatment of intra-articular varus ankle OA. Nineteen consecutive patients were assessed clinically and radiographically at a mean follow-up of 4.9 years. In total, the varus ankle deformity significantly decreased from 18° preoperatively to 10° postoperatively. The AOFAS hindfoot score improved significantly from 46 points preoperatively to 78 points postoperatively. During the follow-up, four of 19 patients underwent revision surgery: two ankle arthrodeses at seven and 36 months after the index surgery, and two TARs at 30 and 48 months. At the latest follow-up, 12 patients reported participation in moderate sporting activities like biking, golfing, gym exercising, and skiing. Five of 19 patients, were active and were able to walk up to five miles daily. Two patients did not report any activities; both had procedure failure requiring ankle arthrodesis or TAR [86].
Conclusion
In conclusion, promising short- and midterm results have been reported in patients who underwent supramalleolar realignment surgery. However, there is only one clinical study prospectively comparing the sport activity level in this patient group preoperatively and postoperatively [84]. It still remains unclear whether postoperative functional improvement positively correlates with sport activity level. Further clinical studies are needed to identify the positive and negative predictors for being active in sports and recreational activities.
Total Ankle Replacement
While total hip replacement and total knee replacement have evolved to well-established treatment options in patients with end-stage degenerative changes, the indication for TAR remains controversial. TAR using current 3rd-generation prosthesis designs provides substantial postoperative pain relief and good functional outcome, including preserved range of motion [87–91]. However, the overall survivorship can be expected to be approximately 90 % at 5 years after initial implantation [92]. The failure rate of TAR is still substantially higher than that of total hip or knee replacement. Labek et al. [93] performed a systematic review, including national registries and clinical studies, demonstrating that the revision rate after TAR was 3.29 per 100 observed component years. This is significantly higher than after total knee replacement (1.26 revisions), medial unicompartmental replacement (1.53 revisions), or total hip replacement (1.29 revisions). The most common reasons for revision surgery after TAR were aseptic loosening (38 %), persisting pain syndrome (12 %), and septic loosening (9.8 %) [94].
Based on our experience with TAR [87, 88, 95–127], the ideal candidate for TAR is middle-aged or older, is reasonably mobile, has no significant comorbidities, participates in low impact physical activities (e.g. hiking, swimming, biking, golfing), is not obese or overweight, has good bone stock, and has no concomitant instabilities/deformities [88, 105] (Fig. 33.3). In our clinic, we still consider the need for high impact physical activities (e.g. contact sports, jumping) as a contraindication for TAR [88, 105]. However, there is limited evidence whether (1) the patients who underwent TAR are able to return to sport activities postoperatively and (2) postoperative sport activities can be identified as risk factors for TAR failure.
The clinical study by Pipino and Calderale [128] is the first clinical study mentioning sport activities in patients who underwent TAR. In this study from the year 1983, the 1st generation PC ankle prosthesis was used in 15 patients. The authors stated that one of 15 patients had started practicing sports after TAR [128].
The study by Valderrabano et al. [126] was the first study specifically analyzing participation in sports after TAR. In total, 147 patients (152 TARs) with a mean age of 59.6 years (28–86 years) were included in this prospective study. At the mean follow-up of 2.8 years (2–4 years) a significant functional improvement was observed in AOFAS hindfoot score (from 36 preoperatively to 84 postoperatively) and range of motion (from 21° (0°–45°) preoperatively to 35° (10°–55°) postoperatively). A special sports frequency score was developed to assess sports activity (Table 33.1). TAR resulted in significant increase of sports participation (36 % preoperatively to 56 % postoperatively). Sports-active patients had a significantly higher AOFAS hindfoot score than patients who did not participate in sports. The most commonly reported sports activities were hiking, biking, swimming, aerobics, downhill skiing, and golfing [126].
Naal et al. [129] analyzed the preoperative and postoperative participation in sports and recreational activities of 101 patients with a mean age of 59.4 years (24–85 years), at a mean of 3.7 years after TAR. The preoperative and postoperative percentage of sports-active patients was 62.4 % and 66.3 %, respectively. The patients were active in 3.0 ± 1.8 different sports and recreational activities preoperatively, and in 3.0 ± 1.6 activities postoperatively. The sports frequency remained the same, with 2.0 ± 1.6 sessions per week before TAR and 2.3 ± 1.7 sessions after TAR. However, 65 % of patients stated that the surgery substantially improved their sports ability. The University of California at Los Angeles activity scale improved significantly from 45.5 ± 16.6 to 84.3 ± 13.3. Neither sports participation nor activity levels were identified as risk factors for development of periprosthetic radiolucencies [129].
Bonnin et al. [130] evaluated function and return to sports after TAR in 140 patients who underwent TAR with the Salto total ankle prosthesis (noncemented, mobile bearing prosthesis) due to OA (100 patients) or rheumatoid arthritis (40 patients). At the mean follow-up of 4.5 years, the Foot Function Index scores were 13.7 ± 17 for “activity limitations”, 31.7 ± 23 for “disability”, and 16.9 ± 19 for “pain”. The Foot and Ankle Ability Measurement scores were 74.9 ± 18 for activities of daily living and 48.9 ± 28 for sports activities. In the OA subgroup, 38 bicycled, 21 performed recreational gymnastics, 58 swam, 50 gardened, 27 danced, and 43 hiked. Seven patients played tennis, nine cross-country ski, 17 downhill skied, and six regularly ran more than 500 m. Most often, patients limited their sports activity for reasons independent of their ankle. Of the patients who had regular or intense sports activity, four mentioned substantial pain in their ankle during sports. In conclusion, the authors demonstrated that TAR may improve quality of life, and that return to recreational activities was generally possible. However, the return to high impact sport was rarely possible [130].
A prospective study has been performed by Barg et al. [99] to evaluate the mid-term outcome in eight haemophilia patients treated with TAR (10 TAR). At the mean follow-up of 5.6 years, significant pain relief and functional improvement was observed. Preoperatively, only one patient was able to participate in sport activities. However, at the latest follow-up, five patients had a normal level of sport activity and one patient had a moderate level [99]. Considering the unique hemophilic etiology of OA in this cohort, the postoperative increase in sport activities may have an especially positive effect, as it has been demonstrated that exercise may help reduce further joint destruction in haemophilia patients [131]. Another prospective study by Barg et al. [112] evaluated the feasibility of TAR in 18 patients with von Willebrand disease. Similar to patients with haemophilia, significant pain relief and functional improvement was observed at the mean follow-up of 7.5 years. Preoperatively, seven patients were moderately active in sports. At the latest follow-up, the postoperative sports activity level was moderate and normal in ten and seven patients, respectively [112]. The same group has evaluated the clinical and radiographic outcome in 16 patients with hereditary hemochromatosis who underwent TAR (21 procedures) [100]. At latest follow-up of 5.3 years in this prospective study, four of 19 patients had a normal level of sport activity and four of 19 patients had a moderate level. For comparison, preoperatively only two of 19 patients had a normal level of sport activity and two of 19 had a moderate level [100]. A similar increase in sport activity was observed in another clinical study addressing the outcome of TAR in 16 patients (19 ankles) with gouty arthritis [107]. Preoperatively, only one patient reported a moderate level of sport activity. Postoperatively, at a mean follow-up of 5.1 years, 13 patients reported participating in a moderate level of sport activity [107].
The outcome in 26 patients with simultaneous bilateral TAR has been analyzed by Barg et al. [102]. Significant pain relief and improvement in functional outcome and quality of life were observed at the mean follow-up of five years in this prospective study. Also, sport activity was assessed preoperatively and postoperatively using Valderrabano’s score [126]. Preoperatively, five patients had a normal level of sport activity and three patients had a moderate level. At latest postoperative follow-up, eight patients had a normal level of sport activity, six patients had a moderate level, and one patient had a high level. One patient in the cohort had a reduced level of sport activity postoperatively (from normal to moderate) [102].
The component stability, weight change, and functional outcome was analyzed in 118 consecutive obese patients in the International Federation of Foot & Ankle Societies 2011 Award paper [104]. Preoperatively, 23 patients (19.5 %) reported a moderate level, 15 patients (12.7 %) a normal level, and one patient (0.8 %) a high level of sport activity. At the mean follow-up of 5.6 years (2.4–10.5 years), 61 patients (22.9 %) reported a moderate level, 29 patients (24.6 %) a normal level, and one patient (0.8 %) a high level of sport activity. A significant weight loss after one and two years of 1.6 ± 3.2 kg, and 2.1 ± 3.6 kg, respectively. Using a 5 % weight loss criterion, 14 patients (11.9 %) lost weight at one-year follow-up. Significant weight loss could be predicted by male gender, but not by age or, surprisingly, postoperative sport activity level [104].
Schuh et al. [132] compared the participation in sports and recreational activities in 21 patients with ankle arthrodesis and 20 patients with TAR. At the mean follow-up of 2.9 years of this prospective study, 86 % and 76 % of all patients were active in sports in the arthrodesis and TAR groups, respectively. Also, clinical and functional outcomes were comparable [132].
Criswell et al. [133] analyzed survival, overall reoperation rate, and functional outcome in 64 patients (65 ankles) who underwent TAR using the Agility prosthesis. Sixteen of the 41 patients (39 %) needed revision of at least one prosthesis component. At the median follow-up of 8 years (0.5–11 years), the average Foot and Ankle Ability Measure subscale scores for sports and daily living activities were 33 and 57 points, respectively. Thirty-three patients reported moderate to extreme difficulty with running, jumping, low impact activities, and the ability to participate in sports [133].
Dalat et al. [134] retrospectively evaluated two continuous series of 59 ankle arthroplasties and 46 ankle arthrodeses performed between 1997 and 2009. The mean follow-up was 4.4 and 4.8 years in TAR and ankle arthrodesis groups, respectively. The mean overall sports level was relatively low in both groups. However, patients who underwent TAR had significantly higher Foot Ankle Ability Measure sports scores with 49.5 ± 24.4 points vs. 29.8 ± 26.2 points. The most common sports in both patient cohorts were non-contact sports including cycling, swimming, and hiking [134].
Nodzo et al. [135] performed a retrospective study including 74 consecutive patients (75 ankles), with a mean age of 60.6 years (41–82 years), who underwent TAR using the Salto prosthesis. At the mean follow-up of 3.6 years, average dorsiflexion and plantarflexion significantly improved from 4.3° ± 3.3° to 8.7° ± 5.6° and from 24° ± 11° to 29° ± 7°, respectively. The subscales of the validated Foot and Ankle Outcome Score for sport activity and activity of daily living also improved significantly from 20 ± 12 to 55 ± 35 and from 50 ± 16 to 83 ± 22, respectively. Positive correlations between high patient satisfaction and the pain, activities of daily living, and quality of life scores were identified [135].
Braito et al. [136] analyzed clinical and radiographic outcomes in 84 patients who underwent HINTEGRA TAR at a mean follow-up of four years. The sports subscale of the Foot and Ankle Outcome Score improved significantly from 17.2 ± 15.4 points preoperatively to 45.8 ± 24.2 points postoperatively [136].
Recently, Kerkhoff et al. [137] analyzed short-term results in 67 patients who underwent primary TAR using the three-component Mobility prosthesis. The percentage of sports active patients was the same before and after surgery at 73 %. Six patients stopped their sports activities after surgery and six patients resumed some sports activities following TAR. The most common sports following TAR were cycling, hiking, and swimming. Although 73 % of all patients were sport active, 91 % were unable to run a short distance [137].
Conclusion
In the last 25 years, TAR has progressed remarkably as a treatment option in patients with end-stage ankle OA [87, 88]. A prospective controlled trial comparing TAR with ankle arthrodesis demonstrated the superiority of TAR in postoperative pain relief and functional outcome [138]. However, the overall survivorship of TAR is still lower than total hip or knee replacement [93], with aseptic loosening being the most common reason for TAR failure [94]. In the current literature, it remains controversial whether patients with TAR have improved ability to participate in sport activities [126, 129, 130]. Also, the question of whether the patients with TAR are more sports-active than demographically comparable patients who underwent ankle arthrodesis cannot be answered definitively by the current literature. There is only one comparative study addressing participation in sports and recreational activities in patients who underwent either ankle arthrodesis or TAR, and it demonstrated no significant differences between groups [132]. However, both groups were small, with only 41 patients in total, and the mean follow-up was relatively short at 2.9 years [132]. Thus, the results of this study must be interpreted with caution.
In the current literature, there are no evidence-based findings that high level sport activity is associated with increased failure rate of TAR. Therefore, such activity should not be considered a contraindication for TAR. However, we recommend against performing TAR in patients with high demands or unrealistic expectations for physical activities [88, 105]. This is the most common recommendation in the literature, as it is supported by numerous studies [139–151]. However, we do not support suggestions that patients with any sports activities should be excluded from TAR, as stated by Giannini et al. [152].
Ankle Arthrodesis
For decades, ankle arthrodesis has been considered the “gold-standard” treatment in patients with end-stage ankle OA, independent of the underlying etiology [153, 154]. Ankle arthrodesis was first described in the nineteenth century [155]. Since then almost 50 different surgical techniques have been described in the literature with good mid-term results: substantial pain relief and acceptable functional outcome [154, 156, 157] (Fig. 33.4). However, many clinical reports have described short-term and long-term problems following ankle arthrodesis in association with daily activities, including climbing stairs, getting out of a chair, walking on uneven surfaces, and running [158–161]. Another major long-term complication following ankle arthrodesis is development of degenerative changes in the adjacent joints, as reported by several authors [157, 160, 162–166]. The development of subsequent OA in adjacent joints may lead to additional fusion surgeries [157, 167]. OA development in adjacent joints can be partially explained by alterations in gait resulting in compensatory motion and overload in the neighboring joints [168]. There are numerous clinical studies investigating gait analysis in patients who underwent ankle arthrodesis. Hahn et al. [169] performed a comparative gait analysis of ankle arthrodesis and TAR. Substantial pain relief and functional improvement was demonstrated one year after both procedures. However, TAR resulted in more natural ankle joint function with increased range of motion [169]. A similar comparative study has been performed by Piriou et al. [170]. Three groups of 12 patients were analyzed: patients with ankle arthrodesis, patients with TAR, and controls. Clinically important differences were demonstrated, but neither TAR nor fusion restored normal movement or walking speed. Patients with ankle arthrodesis showed a faster gait with a longer step length, while patients with TAR had greater ankle range of motion, symmetrical timing of gait, and restored ground reaction force pattern [170]. Recently, Jastifer et al. [171] prospectively compared the performance of TAR and ankle arthrodesis on uneven surfaces, stairs, and inclines. Both groups demonstrated improved performance at one-year follow-up compared to preoperatively. However, TAR patients had higher functional scores than the ankle arthrodesis patients [171].
Ankle arthrodesis. (a) A 29-year old male with ankle osteoarthritis and significant pain due to avascular necrosis of the talus. (b) Magnetic resonance imaging demonstrates avascular necrosis of the talus with more than 50 % involvement. (c) At 1-year follow-up after arthrodesis, the patient had no pain and was able to regain his participation in sport and recreational activities including bowling, cycling, diving, fishing, golf, hiking, ice hockey, and skiing
Regarding the possible development of subsequent OA in adjacent joints and alterations in gait after fusion, it remains unclear whether the patients with ankle arthrodesis are able to regain the ability to participate in sport. Also, there is no data on what effect sport activities may have on long-term outcome.
Mazur et al. [160] analyzed functional outcome and gait in 13 patients with ankle arthrodesis. This was a long-term study with a mean follow-up of 8.3 years. All but one patient were sports active at the latest follow-up, reporting activities like hunting, hockey, baseball, golf, swimming, bowling, skiing, and jogging. Ten of 13 patients were able to return to the recreational sports activities they performed before they developed ankle symptoms [160].
Lynch et al. [159] reported their long-term results in 39 patients with a mean age of 50 years who underwent ankle arthrodesis. At the latest follow-up of a mean of seven years, none of the patients were involved in high impact sports, and running activities were difficult for all but four younger patients who could run limited distances. Three of these four patients were able to participate in ice skating and ice hockey without any restrictions [159].
Thermann et al. [172] reported their results of 225 ankle arthrodeses performed between 1975 and 1995 using external fixation (44 patients) or screw fixation (225 patients). In total, 68 % of all patients were able to participate in sports activities (swimming and biking). Younger patients were also active in playing badminton and soccer, climbing (at a low level), and bodybuilding [172].
Vertullo and Nunley [173] used questionnaires sent to members of the American Orthopaedic Foot and Ankle Society and to trainers of professional basketball and American football teams and asked respondents for guidelines for sports participation after an ankle arthrodesis. The most recommended sport activities were golf, skiing, and tennis with 94 %, 77 %, and 38 % of respondents suggesting them. The authors stated that all high-impact sports should be avoided to minimize the development of adjacent joint OA and stress fractures [173].
Goebel et al. [174] performed a short-term prospective study including 29 patients who underwent tibiotalocalcaneal arthrodesis using a retrograde femur nail. At the mean follow-up of 2.1 years, complete osseous union was achieved in 90 % of patients. At the latest follow-up one fourth of all patients were sports active, whereas none of the patients were able to participate in their chosen sports before surgery [174].
Akra et al. [175] reported their results of 25 patients (26 ankles) treated with ankle arthrodesis using a transfibular approach over a five-year period. In this patient cohort, all patients who were involved in recreational sporting activities were able to return to their usual sports. However, the authors did not mention the percentage of sports active patients in their study [175].
Conclusion
Ankle arthrodesis can be used as a safe surgical procedure for numerous indications in patients with end-stage ankle OA [153, 154, 156]. On one hand, it may provide acceptable mid-term results [154]. But, on the other hand, it may be associated with long-term complications including development of painful OA in the adjacent joints [163]. Similar to TAR, there is limited literature addressing patients’ participation in sports postoperatively. In general, younger patients with ankle arthrodesis are able to participate in sports. However, there are no studies revealing positive or negative effects of sport activities on long-term clinical outcome and OA status in the neighboring joints. Nevertheless, in the current literature there is consensus that high impact sport activities should be avoided in patients who underwent ankle arthrodesis.
Sports Activities in Patients Treated for Ankle Osteoarthritis
The most common etiology for end-stage ankle OA is posttraumatic [4, 5]. Therefore, it is not surprising that almost half of all patients with posttraumatic ankle OA present with a concomitant hindfoot deformity [6, 74, 75]. A direct correlation between the degree of hindfoot malalignment and degenerative process in the ankle joint has been described in the literature [176, 177]. Patients with substantial varus or valgus hindfoot deformity may develop asymmetric ankle OA [1]. Patients with posttraumatic asymmetric ankle OA are a challenging patient cohort, as they are often young and active. Furthermore, the complex underlying biomechanics of their concomitant deformities needs to be recognized and addressed [178]. The treatment of asymmetric ankle OA is also challenging because a substantial portion of the tibiotalar joint surface is usually preserved, and so joint-sacrificing procedures like TAR or ankle arthrodesis may not be the most appropriate treatment [77]. In the recently published review articles, realignment hindfoot surgeries have been shown to have promising short-term and mid-term results, with substantial pain relief and functional improvement [77, 78].
What can be said about sports participation in this specific patient group, who underwent hindfoot realignment, TAR, or ankle arthrodesis surgery? The literature addressing this specific topic is rare, indeed. As such, our recommendations are based on our experience with these surgical procedures over the last two decades [76–78, 80, 81, 84, 85, 178–193] (Table 33.2).
The next discussion point is represented by patients with complete end-stage ankle OA. Due to improved designs and overall survivorship of newer generation TAR systems, ankle arthrodesis should not be considered as the only “gold-standard” treatment option in patients with end-stage ankle OA. However, ankle arthrodesis still remains a proven procedure with good mid-term results, including substantial pain relief [153, 154, 156, 194–196] and acceptable functional outcome [166, 197]. Considering the survivorship of TAR, which is still lower than knee or hip replacement [93], young patients with end-stage ankle OA are better treated by ankle arthrodesis. In a previous study, we analyzed TAR survivorship in 684 patients and determined that age ≤70 years is a statistically significant and independent risk factor for TAR failure with an odds ratio of 3.85 (95 % CI 1.47–10.00) [111]. Literature addressing outcomes following TAR n younger patients is rare. Kofoed and Lundberg-Jensen [145] compared survivorship and functional outcome of TAR between two groups consisting of 30 patients younger than 50 years and 70 patients aged 70 years or older. The postoperative results were comparable in both groups. However, the mean follow-up in both groups was six years with a wide range between one and 15 years [145]. The results of studies with short follow-up should be interpreted carefully. For example, several studies demonstrated encouraging results following TAR using the STAR prosthesis. These studies showed high prosthesis survivorship: 95 % at six years [198], 93.9 % at five years [199], and 96.0 % at five years [200]. However, a long-term TAR study by Brunner et al. [113] with a mean follow-up of 12.4 years (10.8–14.9 years) revealed the probability of implant survival was 70.7 % and 45.6 % at 10 and 14 years, respectively. The recent systematic literature reviews by Gougoulias et al. [92] and Zaidi et al. [91] demonstrated a five-year survivorship of 90 % and 10-year survivorship of 89 %, respectively. Based on results reported in the current literature, a 30 year old patient treated by TAR will most likely have revision surgery due to failure. A salvage procedure of failed TAR – conversion to ankle arthrodesis [201–205] or revision TAR [115, 120, 206, 207] – is a technically demanding procedure and may have worse results than the comparable primary procedure.
Biomechanical cadaver studies demonstrated that TAR may change the natural ankle joint kinematics and biomechanics. However, these changes are less than those observed in fused ankles [208–210]. Still, as mentioned before, patients with high to elite sports activities or unrealistic expectations should not be considered for TAR. Why might excessive sport activities have a negative influence on TAR? First, excessive sport activities and consecutive overload may dramatically change the joint contact pressures. Espinosa et al. [211] analyzed the influence of misalignment of total ankle components on joint contact pressures using finite element models. Two prosthesis types were compared in this in-vitro study: the highly congruent mobile-bearing design of the Mobility TAR and the less congruent two-component Agility TAR. It has been demonstrated, that the congruent mobile-bearing design resulted in more evenly distributed and lower-magnitude joint contact pressure. However, both designs were highly vulnerable to increased contact pressure induced by malalignment of prosthesis components [211]. It can be speculated that excessive sport activities may substantially worsen this problem. Another problem which may occur in excessively sports-active patients may be related to increased polyethylene insert wear or failure. It has been demonstrated that TAR generates wear particles similar to knee prostheses [212]. Increased polyethylene wear may cause periprosthetic osteolysis as a foreign-body reaction resulting in TAR failure, similar to failures observed in total hip replacement. Harris et al. [213] published a case report describing large wear debris cysts in a 65-year-old man who underwent TAR, and required revision surgery. Another complication is fracture of the mobile bearing, which may occur in up to 14 % of patients who undergo TAR using a three-component prosthesis design [87, 113, 214]. Sport activities at high level may increase the rate of this type of complication, although this is only speculation. Finally, periprosthetic fractures may be a specific problem in sports-active patients who undergo TAR. In the current literature, there are only few reports on this complication. The literature consists primarily of case reports [215–217] or short annotations within large TAR studies [218]. Recently, Manegold et al. [219] established a concise classification system of periprosthetic fractures in TAR and described their treatment algorithm based on data from 503 ankle replacements. In total, 21 patients (4.2 %) were identified with a periprosthetic fracture. Eleven and ten patients had intraoperative and postoperative fractures, respectively. The postoperative fractures included two traumatic cases and eight stress fractures. The authors did not mention how traumatic periprosthetic fractures occurred. However, high-energy sports, including contact sports, may be responsible for this difficult to treat complication [219].
Can all these problems be easily avoided by choosing ankle arthrodesis as a treatment option for end-stage ankle OA? Problems unique to TAR, like component loosening or failure of polyethylene inserts will not occur in patients who undergo ankle arthrodesis. However, other long-term problems in this patient cohort can occur. In a cadaveric study by Jung et al. [220] it was demonstrated that the tibiotalar joint arthrodesis significantly affected joint pressure distribution in the adjacent tarsal joints. This may explain the high incidence of OA in the adjacent joints following ankle arthrodesis [163, 165]. Further clinical studies need to be performed whether sports activities may accelerate the degenerative changes of the adjacent joints in patients who underwent ankle arthrodesis.
Based on our experience in foot and ankle surgery, we developed guidelines regarding sport activities in patients who underwent surgical treatments due to ankle OA (Table 33.2). We do believe that sports activities are part of an appropriate postoperative rehabilitation process in these patients. We encourage the patients to stay sports active or to regain their previous recreational activities. However, as Paracelsus stated in the sixteenth century, Dosis sola facit venenum. “The dose makes the poison”: that means that even healthy sporting activities can be harmful it taken to excess. Every patient should keep in mind that he or she had ankle surgery in the past which may substantially lower the limits of their personal physical capacity. These limits should be respected, and not exceeded, in order to ensure good long-term results.
Evidence
-
Bonnin MP, Laurent JR, Casillas M. Ankle function and sports activity after total ankle arthroplasty. Foot Ankle Int 2009;30:933–44. Level of Evidence: III, Retrospective Case Control Study. This study included 140 patients who underwent Salto total ankle replacement. Surgery improved their quality of life and return to recreational activities was generally possible, but return to impact sport was rarely possible [130].
-
Iosifidis MI, Tsarouhas A, Fylaktou A. Lower limb clinical and radiographic osteoarthritis in former elite male athletes. Knee Surg Sports Traumatol Arthrosc 2015;23:2528–35. Level of Evidence: III, Case–control Prognostic Study. This case–control study included 218 former elite male athletes and 181 male controls. It showed that former elite athletes may not be at increased risk of developing clinical osteoarthritis. However, radiographic osteoarthritis signs had a significantly higher incidence in the athletes group [18].
-
Naal FD, Impellizzeri FM, Loibl M, Huber M, Rippstein PF. Habitual physical activity and sports participation after total ankle arthroplasty. Am J Sports Med 2009; 37:95–102. Level of Evidence: IV, Case Series. The preoperative and postoperative percentage of sports-active patients was constant with two-thirds of the 101 patients included in this study. No association between sports participation, increased physical activity, or the appearance of periprosthetic radiolucencies was found at a mean follow-up of 3.7 years after TAR [129].
-
Pagenstert G, Leumann A, Hintermann B, Valderrabano V. Sports and recreation activity of varus and valgus ankle osteoarthritis before and after realignment surgery. Foot Ankle Int 2008;29:985–93. Level of Evidence: II, Prospective Comparative Study. This study demonstrated that hindfoot realignment surgery in patients with varus or valgus deformity substantially increased sports activity postoperatively. Improved ankle pain and function correlated with ability to perform activity without symptoms [84].
-
Saltzman CL, Mann RA, Ahrens JE, Amendola A, Anderson AB, Berlet GC, Brodsky JW, Chou LB, Clanton TO, Deland JT, DeOrio JK, Horton GA, Lee TH, Mann JA, Nunley JA, Thordarson DB, Walling AK, Wapner KL, Coughlin MJ. Prospective controlled trial of STAR total ankle replacement versus ankle fusion: Initial results. Foot Ankle Int 2002; 23:68–74. Level of Evidence: II, Prospective Controlled Comparative Surgical Trial. The only available prospective controlled trial addressing the safety and efficacy of total ankle replacement versus ankle fusion to treat end-stage ankle osteoarthritis. At 2-years follow-up, patients treated with total ankle replacement had better function and equivalent pain relief as patients treated with fusion [138].
-
Schuh R, Hofstaetter J, Krismer M, Bevoni R, Windhager R, Trnka HJ. Total ankle arthroplasty versus ankle arthrodesis. Comparison of sports, recreational activities and functional outcome. Int Orthop 2012; 36:1207–14. Level of Evidence: II, Prospective Comparative Study. This study included 21 patients with ankle arthrodesis and 20 patients with total ankle replacement. It revealed no significant difference between groups concerning activity levels, participation in sports activities, or functional scores [132].
-
Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Relat Res 2009; 467:1800–6. Level of Evidence: IV, Prognostic Study. In this study, the distribution of etiologies leading to ankle arthritis in 406 ankles was analyzed. Ankle osteoarthritis developed secondary to trauma in 79 %. The traumas were mostly malleolar fractures, ligament lesions, and tibial plafond fractures [4].
-
Valderrabano V, Pagenstert G, Horisberger M, Knupp M, Hintermann B. Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. Am J Sports Med 2006; 34:993–9. Level of Evidence: IV, Case Series. This is the first clinical study addressing participation in sports after total ankle replacement. There was a significant increase in sports activity after total ankle replacement, with sports-active patients having better functional outcome than patients who did not participate in sports activities [126].
Summary
-
Ankle OA is a debilitating disease and a growing problem in health care worldwide.
-
Unlike the hip and knee, the ankle is most commonly affected by posttraumatic OA following fractures or ligament injuries.
-
In the current literature, there is a controversial discussion whether sport activities play a positive or negative role in the development of ankle OA.
-
In patients with ankle OA, numerous treatment options have been described, including joint-preserving and joint-sacrificing procedures.
-
There is limited literature addressing participation in sports in patients who underwent surgical procedures due to ankle OA. In general, low impact sports can be recommended postoperatively. Further clinical studies are needed to define the role of sport in postoperative rehabilitation and to determine whether excessive sports activity is a risk factor for failure or worse outcomes.
References
Barg A, Pagenstert GI, Hugle T, Gloyer M, Wiewiorski M, Henninger HB, et al. Ankle osteoarthritis: etiology, diagnostics, and classification. Foot Ankle Clin. 2013;18(3):411–26.
Glazebrook M, Daniels T, Younger A, Foote CJ, Penner M, Wing K, et al. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008;90(3):499–505.
Egloff C, Gloyer M, Barg K, Hugle T, Pagenstert G, Valderrabano V, et al. Ankle osteoarthritis – etiology and biomechanics. Fuss Sprungg. 2013;11(4):179–85.
Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467(7):1800–6.
Saltzman CL, Salamon ML, Blanchard GM, Huff T, Hayes A, Buckwalter JA, et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25(1):44–6.
Wang B, Saltzman CL, Chalayon O, Barg A. Does the subtalar joint compensate for ankle malalignment in end-stage ankle arthritis? Clin Orthop Relat Res. 2015;473(1):318–25.
Caine DJ, Golightly YM. Osteoarthritis as an outcome of paediatric sport: an epidemiological perspective. Br J Sports Med. 2011;45(4):298–303.
Vincelette P, Laurin CA, Levesque HP. The footballer's ankle and foot. Can Med Assoc J. 1972;107(9):872–4.
Adams ID. Osteoarthrosis and sport. J R Soc Med. 1979;72(3):185–7.
Hellmann DB, Helms CA, Genant HK. Chronic repetitive trauma: a cause of atypical degenerative joint disease. Skeletal Radiol. 1983;10(4):236–42.
Kujala UM, Kaprio J, Sarna S. Osteoarthritis of weight bearing joints of lower limbs in former elite male athletes. BMJ (Clin Res ed). 1994;308(6923):231–4.
Knobloch M, Marti B, Biedert R, Howald H. Risk of arthrosis of the upper ankle joint in long distance runners: controlled follow-up of former elite athletes. Sportverletzung Sportschaden. 1990;4(4):175–9.
Gross P, Marti B. Risk of degenerative ankle joint disease in volleyball players: study of former elite athletes. Int J Sports Med. 1999;20(1):58–63.
Zinder SM, Guskiewicz KM, Marshall SW. Prevalence of ankle osteoarthritis following a history of ankle sprain in retired professional football players. Med Sci Sports Exerc. 2010;42(5):608.
Kuijt MT, Inklaar H, Gouttebarge V, Frings-Dresen MH. Knee and ankle osteoarthritis in former elite soccer players: a systematic review of the recent literature. J Sci Med Sport. 2012;15(6):480–7.
Gouttebarge V, Inklaar H, Backx F, Kerkhoffs G. Prevalence of osteoarthritis in former elite athletes: a systematic overview of the recent literature. Rheumatol Int. 2015;35(3):405–18.
Schmitt H, Lemke JM, Brocai DR, Parsch D. Degenerative changes in the ankle in former elite high jumpers. Clin J Sport Med. 2003;13(1):6–10.
Iosifidis MI, Tsarouhas A, Fylaktou A. Lower limb clinical and radiographic osteoarthritis in former elite male athletes. Knee Surg Sports Traumatol Arthrosc. 2015;23(9):2528–35.
Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37(1):73–94.
Kobayashi T, Gamada K. Lateral ankle sprain and chronic ankle instability: a critical review. Foot Ankle Spec. 2014;7(4):298–326.
Agel J, Olson DE, Dick R, Arendt EA, Marshall SW, Sikka RS. Descriptive epidemiology of collegiate women's basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):202–10.
Borowski LA, Yard EE, Fields SK, Comstock RD. The epidemiology of US high school basketball injuries, 2005–2007. Am J Sports Med. 2008;36(12):2328–35.
Deitch JR, Starkey C, Walters SL, Moseley JB. Injury risk in professional basketball players: a comparison of Women's National Basketball Association and National Basketball Association athletes. Am J Sports Med. 2006;34(7):1077–83.
Dick R, Hertel J, Agel J, Grossman J, Marshall SW. Descriptive epidemiology of collegiate men's basketball injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007;42(2):194–201.
McCarthy MM, Voos JE, Nguyen JT, Callahan L, Hannafin JA. Injury profile in elite female basketball athletes at the Women's National Basketball Association combine. Am J Sports Med. 2013;41(3):645–51.
McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35(2):103–8.
Meeuwisse WH, Sellmer R, Hagel BE. Rates and risks of injury during intercollegiate basketball. Am J Sports Med. 2003;31(3):379–85.
Starkey C. Injuries and illnesses in the national basketball association: a 10-year perspective. J Athl Train. 2000;35(2):161–7.
Agel J, Evans TA, Dick R, Putukian M, Marshall SW. Descriptive epidemiology of collegiate men's soccer injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2002–2003. J Athl Train. 2007;42(2):270–7.
Dick R, Putukian M, Agel J, Evans TA, Marshall SW. Descriptive epidemiology of collegiate women's soccer injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2002–2003. J Athl Train. 2007;42(2):278–85.
Dvorak J, Junge A, Derman W, Schwellnus M. Injuries and illnesses of football players during the 2010 FIFA World Cup. Br J Sports Med. 2011;45(8):626–30.
Faude O, Junge A, Kindermann W, Dvorak J. Injuries in female soccer players: a prospective study in the German national league. Am J Sports Med. 2005;33(11):1694–700.
Gaulrapp H, Becker A, Walther M, Hess H. Injuries in women's soccer: a 1-year all players prospective field study of the women's Bundesliga (German premier league). Clin J Sport Med. 2010;20(4):264–71.
Herrero H, Salinero JJ, Del Coso J. Injuries among Spanish male amateur soccer players: a retrospective population study. Am J Sports Med. 2014;42(1):78–85.
Le Gall F, Carling C, Reilly T. Injuries in young elite female soccer players: an 8-season prospective study. Am J Sports Med. 2008;36(2):276–84.
Leininger RE, Knox CL, Comstock RD. Epidemiology of 1.6 million pediatric soccer-related injuries presenting to US emergency departments from 1990 to 2003. Am J Sports Med. 2007;35(2):288–93.
Smith RW, Reischl SF. Treatment of ankle sprains in young athletes. Am J Sports Med. 1986;14(6):465–71.
Tegnander A, Olsen OE, Moholdt TT, Engebretsen L, Bahr R. Injuries in Norwegian female elite soccer: a prospective one-season cohort study. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):194–8.
Valderrabano V, Barg A, Paul J, Pagenstert G, Wiewiorski M. Foot and ankle injuries in professional soccer players. Sport Orthop Traumatol. 2014;30(2):98–105.
Walden M, Hagglund M, Ekstrand J. Time-trends and circumstances surrounding ankle injuries in men's professional football: an 11-year follow-up of the UEFA Champions League injury study. Br J Sports Med. 2013;47(12):748–53.
Wong P, Hong Y. Soccer injury in the lower extremities. Br J Sports Med. 2005;39(8):473–82.
Darrow CJ, Collins CL, Yard EE, Comstock RD. Epidemiology of severe injuries among United States high school athletes: 2005–2007. Am J Sports Med. 2009;37(9):1798–805.
Iacovelli JN, Yang J, Thomas G, Wu H, Schiltz T, Foster DT. The effect of field condition and shoe type on lower extremity injuries in American Football. Br J Sports Med. 2013;47(12):789–93.
Kaplan LD, Jost PW, Honkamp N, Norwig J, West R, Bradley JP. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop (Belle Mead, NJ). 2011;40(1):40–4.
Meyers MC. Incidence, mechanisms, and severity of game-related college football injuries on FieldTurf versus natural grass: a 3-year prospective study. Am J Sports Med. 2010;38(4):687–97.
Olson D, Sikka RS, Labounty A, Christensen T. Injuries in professional football: current concepts. Curr Sports Med Rep. 2013;12(6):381–90.
Osbahr DC, Drakos MC, O'Loughlin PF, Lyman S, Barnes RP, Kennedy JG, et al. Syndesmosis and lateral ankle sprains in the National Football League. Orthopedics. 2013;36(11):e1378–84.
Abrams GD, Renstrom PA, Safran MR. Epidemiology of musculoskeletal injury in the tennis player. Br J Sports Med. 2012;46(7):492–8.
Bylak J, Hutchinson MR. Common sports injuries in young tennis players. Sports Med. 1998;26(2):119–32.
Hjelm N, Werner S, Renstrom P. Injury profile in junior tennis players: a prospective two year study. Knee Surg Sports Traumatol Arthrosc. 2010;18(6):845–50.
Hutchinson MR, Laprade RF, Burnett 2nd QM, Moss R, Terpstra J. Injury surveillance at the USTA Boys' Tennis Championships: a 6-yr study. Med Sci Sports Exerc. 1995;27(6):826–30.
Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont Jr PJ. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92(13):2279–84.
Beynnon BD, Murphy DF, Alosa DM. Predictive factors for lateral ankle sprains: a literature review. J Athl Train. 2002;37(4):376–80.
Beynnon BD, Vacek PM, Murphy D, Alosa D, Paller D. First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med. 2005;33(10):1485–91.
Murphy DF, Connolly DA, Beynnon BD. Risk factors for lower extremity injury: a review of the literature. Br J Sports Med. 2003;37(1):13–29.
Caine D, Caine C, Maffulli N. Incidence and distribution of pediatric sport-related injuries. Clin J Sport Med. 2006;16(6):500–13.
Swenson DM, Yard EE, Fields SK, Comstock RD. Patterns of recurrent injuries among US high school athletes, 2005–2008. Am J Sports Med. 2009;37(8):1586–93.
Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bull NYU Hosp Jt Dis. 2011;69(1):17–26.
de Vries JS, Krips R, Sierevelt IN, Blankevoort L, van Dijk CN. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011(8):CD004124.
van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121(4):324–31.
Hershkovich O, Tenenbaum S, Gordon B, Bruck N, Thein R, Derazne E, et al. A large-scale study on epidemiology and risk factors for chronic ankle instability in young adults. J Foot Ankle Surg. 2015;54(2):183–7.
Pourkazemi F, Hiller CE, Raymond J, Nightingale EJ, Refshauge KM. Predictors of chronic ankle instability after an index lateral ankle sprain: a systematic review. J Sci Med Sport/Sports Med Aust. 2014;17(6):568–73.
Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34(4):612–20.
Cha SD, Kim HS, Chung ST, Yoo JH, Park JH, Kim JH, et al. Intra-articular lesions in chronic lateral ankle instability: comparison of arthroscopy with magnetic resonance imaging findings. Clin Orthop Surg. 2012;4(4):293–9.
Hintermann B, Boss A, Schafer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30(3):402–9.
Lee J, Hamilton G, Ford L. Associated intra-articular ankle pathologies in patients with chronic lateral ankle instability: arthroscopic findings at the time of lateral ankle reconstruction. Foot Ankle Spec. 2011;4(5):284–9.
Sugimoto K, Takakura Y, Okahashi K, Samoto N, Kawate K, Iwai M. Chondral injuries of the ankle with recurrent lateral instability: an arthroscopic study. J Bone Joint Surg Am. 2009;91(1):99–106.
Bischof JE, Spritzer CE, Caputo AM, Easley ME, DeOrio JK, Nunley 2nd JA, et al. In vivo cartilage contact strains in patients with lateral ankle instability. J Biomech. 2010;43(13):2561–6.
Caputo AM, Lee JY, Spritzer CE, Easley ME, DeOrio JK, Nunley 2nd JA, et al. In vivo kinematics of the tibiotalar joint after lateral ankle instability. Am J Sports Med. 2009;37(11):2241–8.
Golditz T, Steib S, Pfeifer K, Uder M, Gelse K, Janka R, et al. Functional ankle instability as a risk factor for osteoarthritis: using T2-mapping to analyze early cartilage degeneration in the ankle joint of young athletes. Osteoarthritis Cartilage. 2014;22(10):1377–85.
McKinley TO, Tochigi Y, Rudert MJ, Brown TD. The effect of incongruity and instability on contact stress directional gradients in human cadaveric ankles. Osteoarthritis Cartilage. 2008;16(11):1363–9.
Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61(3):354–61.
Taga I, Shino K, Inoue M, Nakata K, Maeda A. Articular cartilage lesions in ankles with lateral ligament injury. An arthroscopic study. Am J Sports Med. 1993;21(1):120–6; discussion 6–7.
Horisberger M, Hintermann B, Valderrabano V. Alterations of plantar pressure distribution in posttraumatic end-stage ankle osteoarthritis. Clin Biomech (Bristol, Avon). 2009;24(3):303–7.
Horisberger M, Valderrabano V, Hintermann B. Posttraumatic ankle osteoarthritis after ankle-related fractures. J Orthop Trauma. 2009;23(1):60–7.
Barg A, Paul J, Pagenstert GI, Leumann A, Horisberger M, Henninger HB, et al. Supramalleolar osteotomies for ankle osteoarthritis. Tech Foot Ankle. 2013;12(2):138–46.
Barg A, Pagenstert GI, Horisberger M, Paul J, Gloyer M, Henninger HB, et al. Supramalleolar osteotomies for degenerative joint disease of the ankle joint: indication, technique and results. Int Orthop. 2013;37(9):1683–95.
Barg A, Saltzman CL. Single-stage supramalleolar osteotomy for coronal plane deformity. Curr Rev Musculoskelet Med. 2014;7(4):277–91.
Colin F, Gaudot F, Odri G, Judet T. Supramalleolar osteotomy: techniques, indications and outcomes in a series of 83 cases. Orthop Traumatol Surg Res. 2014;100(4):413–8.
Knupp M, Stufkens SA, Bolliger L, Barg A, Hintermann B. Classification and treatment of supramalleolar deformities. Foot Ankle Int. 2011;32(11):1023–31.
Pagenstert G, Knupp M, Valderrabano V, Hintermann B. Realignment surgery for valgus ankle osteoarthritis. Oper Orthop Traumatol. 2009;21(1):77–87.
Takakura Y, Takaoka T, Tanaka Y, Yajima H, Tamai S. Results of opening-wedge osteotomy for the treatment of a post-traumatic varus deformity of the ankle. J Bone Joint Surg Am. 1998;80(2):213–8.
Harstall R, Lehmann O, Krause F, Weber M. Supramalleolar lateral closing wedge osteotomy for the treatment of varus ankle arthrosis. Foot Ankle Int. 2007;28(5):542–8.
Pagenstert G, Leumann A, Hintermann B, Valderrabano V. Sports and recreation activity of varus and valgus ankle osteoarthritis before and after realignment surgery. Foot Ankle Int. 2008;29(10):985–93.
Hintermann B, Barg A, Knupp M. Corrective supramalleolar osteotomy for malunited pronation-external rotation fractures of the ankle. J Bone Joint Surg. 2011;93(10):1367–72.
Mann HA, Filippi J, Myerson MS. Intra-articular opening medial tibial wedge osteotomy (plafond-plasty) for the treatment of intra-articular varus ankle arthritis and instability. Foot Ankle Int. 2012;33(4):255–61.
Barg A, Saltzman CL. Ankle replacement. In: Coughlin MJ, Saltzman CL, Anderson RB, editors. Mann's Surgery of the foot and ankle. Philadelphia: Elsevier Saunders; 2014. p. 1078–162.
Barg A, Wimmer MD, Wiewiorski M, Wirtz DC, Pagenstert GI, Valderrabano V. Total ankle replacement – indications, implant designs, and results. Dtsch Arztebl Int. 2015;112(11):177–84.
Gougoulias NE, Agathangelidis FG, Parsons SW. Arthroscopic ankle arthrodesis. Foot Ankle Int. 2007;28(6):695–706.
Bonasia DE, Dettoni F, Femino JE, Phisitkul P, Germano M, Amendola A. Total ankle replacement: why, when and how? Iowa Orthop J. 2010;30(1):119–30.
Zaidi R, Cro S, Gurusamy K, Siva N, Macgregor A, Henricson A, et al. The outcome of total ankle replacement: a systematic review and meta-analysis. Bone Joint J. 2013;95-B(11):1500–7.
Gougoulias N, Khanna A, Maffulli N. How successful are current ankle replacements?: a systematic review of the literature. Clin Orthop Relat Res. 2010;468(1):199–208.
Labek G, Thaler M, Janda W, Agreiter M, Stockl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg. 2011;93(3):293–7.
Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Bohler N, Labek G. Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty. 2013;28(8):1329–32.
Barg A, Barg K, Schneider SW, Pagenstert G, Gloyer M, Henninger HB, et al. Thrombembolic complications after total ankle replacement. Curr Rev Musculoskelet Med. 2014;6(4):328–35.
Barg A, Barg K, Wiewiorski M, Schneider SW, Wimmer MD, Wirtz DC, et al. Total ankle replacement in patients with bleeding disorders. Orthopade. 2015;44(8):623–8.
Barg A, Elsner A, Anderson AE, Hintermann B. The effect of three-component total ankle replacement malalignment on clinical outcome: pain relief and functional outcome in 317 consecutive patients. J Bone Joint Surg Am. 2011;93(21):1969–78.
Barg A, Elsner A, Chuckpaiwong B, Hintermann B. Insert position in three-component total ankle replacement. Foot Ankle Int. 2010;31(9):754–9.
Barg A, Elsner A, Hefti D, Hintermann B. Haemophilic arthropathy of the ankle treated by total ankle replacement: a case series. Haemophilia. 2010;16(4):647–55.
Barg A, Elsner A, Hefti D, Hintermann B. Total ankle arthroplasty in patients with hereditary hemochromatosis. Clin Orthop Relat Res. 2011;469(5):1427–35.
Barg A, Henninger HB, Hintermann B. Risk factors for symptomatic deep-vein thrombosis in patients after total ankle replacement who received routine chemical thromboprophylaxis. J Bone Joint Surg. 2011;93(7):921–7.
Barg A, Henninger HB, Knupp M, Hintermann B. Simultaneous bilateral total ankle replacement using a 3-component prosthesis: outcome in 26 patients followed for 2–10 years. Acta Orthop. 2011;82(6):704–10.
Barg A, Hintermann B. Takedown of painful ankle fusion and total ankle replacement using a 3-component ankle prosthesis. Tech Foot Ankle. 2010;9(4):190–8.
Barg A, Knupp M, Anderson AE, Hintermann B. Total ankle replacement in obese patients: component stability, weight change, and functional outcome in 118 consecutive patients. Foot Ankle Int. 2011;32(10):925–32.
Barg A, Knupp M, Henninger HB, Zwicky L, Hintermann B. Total ankle replacement using HINTEGRA, an unconstrained, three-component system: surgical technique and pitfalls. Foot Ankle Clin. 2012;17(4):607–35.
Barg A, Knupp M, Hintermann B. Simultaneous bilateral versus unilateral total ankle replacement: a patient-based comparison of pain relief, quality of life and functional outcome. J Bone Joint Surg. 2010;92(12):1659–63.
Barg A, Knupp M, Kapron AL, Hintermann B. Total ankle replacement in patients with gouty arthritis. J Bone Joint Surg Am. 2011;93(4):357–66.
Barg A, Pagenstert GI, Leumann AG, Muller AM, Henninger HB, Valderrabano V. Treatment of the arthritic valgus ankle. Foot Ankle Clin. 2012;17(4):647–63.
Barg A, Schneider SW, Pagenstert G, Hintermann B, Valderrabano V. Thromboembolic complications following ankle prosthesis implantation. Orthopade. 2013;42(11):948–56.
Barg A, Suter T, Zwicky L, Knupp M, Hintermann B. Medial pain syndrome in patients with total ankle replacement. Orthopade. 2011;40(11):991–2. 4–9.
Barg A, Zwicky L, Knupp M, Henninger HB, Hintermann B. HINTEGRA total ankle replacement: survivorship analysis in 684 patients. J Bone Joint Surg Am. 2013;95(13):1175–83.
Barg K, Wiewiorski M, Anderson AE, Schneider SW, Wimmer MD, Wirtz DC, et al. Total ankle replacement in patients with von Willebrand disease: mid-term results of 18 procedures. Haemophilia. 2015;21(5):e389–401.
Brunner S, Barg A, Knupp M, Zwicky L, Kapron AL, Valderrabano V, et al. The Scandinavian total ankle replacement: long-term, eleven to fifteen-year, survivorship analysis of the prosthesis in seventy-two consecutive patients. J Bone Joint Surg Am. 2013;95(8):711–8.
Hintermann B, Barg A. Total ankle replacement in patients with osteoarthritis. Arthroskopie. 2011;24(4):274–82.
Hintermann B, Barg A, Knupp M. Revision arthroplasty of the ankle joint. Orthopade. 2011;40(11):1000–7.
Hintermann B, Barg A, Knupp M, Valderrabano V. Conversion of painful ankle arthrodesis to total ankle arthroplasty. J Bone Joint Surg Am. 2009;91(4):850–8.
Hintermann B, Barg A, Knupp M, Valderrabano V. Conversion of painful ankle arthrodesis to total ankle arthroplasty. Surgical technique. J Bone Joint Surg Am. 2010;92(Suppl 1 Pt 1):55–66.
Hintermann B, Valderrabano V. Total ankle replacement. Foot Ankle Clin. 2003;8(2):375–405.
Hintermann B, Valderrabano V, Dereymaeker G, Dick W. The HINTEGRA ankle: rationale and short-term results of 122 consecutive ankles. Clin Orthop Relat Res. 2004;424:57–68.
Hintermann B, Zwicky L, Knupp M, Henninger HB, Barg A. HINTEGRA revision arthroplasty for failed total ankle prostheses. J Bone Joint Surg Am. 2013;95(13):1166–74.
Paul J, Barg A, Kretzschmar M, Pagenstert G, Studler U, Hugle T, et al. Increased osseous 99mTc-DPD uptake in end-stage ankle osteoarthritis: correlation between SPECT-CT imaging and histologic findings. Foot Ankle Int. 2015;36(12):1438–47.
Valderrabano V, Frigg A, Leumann A, Horisberger M. Total ankle arthroplasty in valgus ankle osteoarthritis. Orthopade. 2011;40(11):971–4. 6–7.
Valderrabano V, Hintermann B, Dick W. Scandinavian total ankle replacement: a 3.7-year average followup of 65 patients. Clin Orthop Related Res. 2004;424(1):47–56.
Valderrabano V, Nigg BM, von Tscharner V, Frank CB, Hintermann B. J. Leonard Goldner Award 2006. Total ankle replacement in ankle osteoarthritis: an analysis of muscle rehabilitation. Foot Ankle Int. 2007;28(2):281–91.
Valderrabano V, Nigg BM, von Tscharner V, Stefanyshyn DJ, Goepfert B, Hintermann B. Gait analysis in ankle osteoarthritis and total ankle replacement. Clin Biomech (Bristol, Avon). 2007;22(8):894–904.
Valderrabano V, Pagenstert G, Horisberger M, Knupp M, Hintermann B. Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. Am J Sports Med. 2006;34(6):993–9.
Valderrabano V, Pagenstert GI, Muller AM, Paul J, Henninger HB, Barg A. Mobile- and fixed-bearing total ankle prostheses: is there really a difference? Foot Ankle Clin. 2012;17(4):565–85.
Pipino F, Calderale PM. PC ankle prosthesis. Five year follow-up. Acta Orthop Belg. 1983;49(6):725–35.
Naal FD, Impellizzeri FM, Loibl M, Huber M, Rippstein PF. Habitual physical activity and sports participation after total ankle arthroplasty. Am J Sports Med. 2009;37(1):95–102.
Bonnin MP, Laurent JR, Casillas M. Ankle function and sports activity after total ankle arthroplasty. Foot Ankle Int. 2009;30(10):933–44.
Harris S, Boggio LN. Exercise may decrease further destruction in the adult haemophilic joint. Haemophilia. 2006;12(3):237–40.
Schuh R, Hofstaetter J, Krismer M, Bevoni R, Windhager R, Trnka HJ. Total ankle arthroplasty versus ankle arthrodesis. Comparison of sports, recreational activities and functional outcome. Int Orthop. 2012;36(6):1207–14.
Criswell BJ, Douglas K, Naik R, Thomson AB. High revision and reoperation rates using the Agility Total Ankle System. Clin Orthop Relat Res. 2012;470(7):1980–6.
Dalat F, Trouillet F, Fessy MH, Bourdin M, Besse JL. Comparison of quality of life following total ankle arthroplasty and ankle arthrodesis: retrospective study of 54 cases. Orthop Traumatol Surg Res. 2014;100(7):761–6.
Nodzo SR, Miladore MP, Kaplan NB, Ritter CA. Short to midterm clinical and radiographic outcomes of the Salto total ankle prosthesis. Foot Ankle Int. 2014;35(1):22–9.
Braito M, Dammerer D, Reinthaler A, Kaufmann G, Huber D, Biedermann R. Effect of coronal and sagittal alignment on outcome after mobile-bearing total ankle replacement. Foot Ankle Int. 2015;36(9):1029–37.
Kerkhoff YRA, Kosse NM, Louwerens JW. Short term results of the Mobility Total Ankle System: Clinical and radiographic outcome. Foot Ankle Surg. 2016;22(3):152–7.
Saltzman CL, Mann RA, Ahrens JE, Amendola A, Anderson RB, Berlet GC, et al. Prospective controlled trial of STAR total ankle replacement versus ankle fusion: initial results. Foot Ankle Int. 2009;30(7):579–96.
Colombier JA, Judet T, Bonnin M, Gaudot F. Techniques and pitfalls with the Salto prosthesis: our experience of the first 15 years. Foot Ankle Clin. 2012;17(4):587–605.
Daniels TR, Younger AS, Penner M, Wing K, Dryden PJ, Wong H, et al. Intermediate-term results of total ankle replacement and ankle arthrodesis: a COFAS multicenter study. J Bone Joint Surg Am. 2014;96(2):135–42.
Ellis SJ, Moril-Penalver L, Deland JT. The Schandinavian Total Ankle Replacement (STAR) system. Semin Arthro. 2010;21(2):275–81.
Frigg A, Nigg B, Hinz L, Valderrabano V, Russell I. Clinical relevance of hindfoot alignment view in total ankle replacement. Foot Ankle Int. 2010;31(10):871–9.
Kofoed H. The evolution of ankle arthroplasty. Orthopade. 1999;28(9):804–11.
Kofoed H. Schandinavian total ankle replacement: the surgical technique. Tech Foot Ankle. 2005;4(2):55–61.
Kofoed H, Lundberg-Jensen A. Ankle arthroplasty in patients younger and older than 50 years: a prospective series with long-term follow-up. Foot Ankle Int. 1999;20(8):501–6.
Krause FG, Schmid T. Ankle arthrodesis versus total ankle replacement: how do I decide? Foot Ankle Clin. 2012;17(4):529–43.
Lieske S, Schenk K, Neumann HW, John M. Implantation of a Salto 2 total ankle prosthesis. Oper Orthop Traumatol. 2014;26(4):401–11.
Mittlmeier T. Arthrodesis versus total joint replacement of the ankle. Unfallchirurg. 2013;116(6):537–50; quiz 51–2.
Rippstein PF, Naal FD. Total ankle replacement in rheumatoid arthritis. Orthopade. 2011;40(11):984–6. 8–90.
Rzesacz EH, Gosse F. Management of posttraumatic osteoarthritis of the upper ankle joint by implantation of the S.T.A.R. ankle prosthesis. Oper Orthop Traumatol. 2007;19(5–6):527–46.
Thermann H, Saltzman CL. Prosthetic replacement of the upper ankle joint. Unfallchirurg. 2002;105(6):496–510.
Giannini S, Romagnoli M, O'Connor JJ, Malerba F, Leardini A. Total ankle replacement compatible with ligament function produces mobility, good clinical scores, and low complication rates: an early clinical assessment. Clin Orthop Relat Res. 2010;468(10):2746–53.
Ahmad J, Raikin SM. Ankle arthrodesis: the simple and the complex. Foot Ankle Clin. 2008;13(3):381–400.
Nihal A, Gellman RE, Embil JM, Trepman E. Ankle arthrodesis. Foot Ankle Surg. 2008;14(1):1–10.
Albert E. Einige Falle kunstlicher Ankylosen: Bildung an paralytischen Gliedmassen. Wien Med Press. 1882;23(5):726–8.
Chalayon O, Wang B, Blankenhorn B, Jackson 3rd JB, Beals T, Nickisch F, et al. Factors affecting the outcomes of uncomplicated primary open ankle arthrodesis. Foot Ankle Int. 2015;36(10):1170–9.
Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83(2):219–28.
Lance EM, Paval A, Fries I, Larsen I, Patterson Jr RL. Arthrodesis of the ankle joint: a follow-up study. Clin Orthop Related Res. 1979;142(1):146–58.
Lynch AF, Bourne RB, Rorabeck CH. The long-term results of ankle arthrodesis. J Bone Joint Surg. 1988;70(1):113–6.
Mazur JM, Schwartz E, Simon SR. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Joint Surg Am. 1979;61(7):964–75.
Morgan CD, Henke JA, Bailey RW, Kaufer H. Long-term results of tibiotalar arthrodesis. J Bone Joint Surg Am. 1985;67(4):546–50.
Ebalard M, Le Henaff G, Sigonney G, Lopes R, Kerhousse G, Brilhault J, et al. Risk of osteoarthritis secondary to partial or total arthrodesis of the subtalar and midtarsal joints after a minimum follow-up of 10 years. Orthop Traumatol Surg Res. 2014;100(4 Suppl):S231–7.
Fuchs S, Sandmann C, Skwara A, Chylarecki C. Quality of life 20 years after arthrodesis of the ankle. A study of adjacent joints. J Bone Joint Surg. 2003;85(7):994–8.
Ling JS, Smyth NA, Fraser EJ, Hogan MV, Seaworth CM, Ross KA, et al. Investigating the relationship between ankle arthrodesis and adjacent-joint arthritis in the hindfoot: a systematic review. J Bone Joint Surg Am. 2015;97(6):513–20.
Suckel A, Burger A, Wulker N, Wunschel M. Ankle arthrodesis – clinical, radiological and biomechanical aspects with special regard to the adjacent joints. Z Orthop Unfall. 2012;150(6):588–93.
van der Plaat LW, van Engelen SJ, Wajer QE, Hendrickx RP, Doets KH, Houdijk H, et al. Hind- and midfoot motion after ankle arthrodesis. Foot Ankle Int. 2015;36(12):1430–7.
Hendrickx RP, Stufkens SA, de Bruijn EE, Sierevelt IN, van Dijk CN, Kerkhoffs GM. Medium- to long-term outcome of ankle arthrodesis. Foot Ankle Int. 2011;32(10):940–7.
Fuentes-Sanz A, Moya-Angeler J, Lopez-Oliva F, Forriol F. Clinical outcome and gait analysis of ankle arthrodesis. Foot Ankle Int. 2012;33(10):819–27.
Hahn ME, Wright ES, Segal AD, Orendurff MS, Ledoux WR, Sangeorzan BJ. Comparative gait analysis of ankle arthrodesis and arthroplasty: initial findings of a prospective study. Foot Ankle Int. 2012;33(4):282–9.
Piriou P, Culpan P, Mullins M, Cardon JN, Pozzi D, Judet T. Ankle replacement versus arthrodesis: a comparative gait analysis study. Foot Ankle Int. 2008;29(1):3–9.
Jastifer J, Coughlin MJ, Hirose C. Performance of total ankle arthroplasty and ankle arthrodesis on uneven surfaces, stairs, and inclines: a prospective study. Foot Ankle Int. 2015;36(1):11–7.
Thermann H, Huefner T, Schratt HE, von Glinski S, Roehler A, Tscherne H. Schrew fixation for ankle arthrodesis. Foot Ankle Surg. 1999;5(3):131–42.
Vertullo CJ, Nunley JA. Participation in sports after arthrodesis of the foot or ankle. Foot Ankle Int. 2002;23(7):625–8.
Goebel M, Gerdesmeyer L, Muckley T, Schmitt-Sody M, Diehl P, Stienstra J, et al. Retrograde intramedullary nailing in tibiotalocalcaneal arthrodesis: a short-term, prospective study. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg. 2006;45(2):98–106.
Akra GA, Middleton A, Adedapo AO, Port A, Finn P. Outcome of ankle arthrodesis using a transfibular approach. J Foot Ankle Surg. 2010;49(6):508–12.
Puno RM, Vaughan JJ, Stetten ML, Johnson JR. Long-term effects of tibial angular malunion on the knee and ankle joints. J Orthop Trauma. 1991;5(3):247–54.
Puno RM, Vaughan JJ, von Fraunhofer JA, Stetten ML, Johnson JR. A method of determining the angular malalignments of the knee and ankle joints resulting from a tibial malunion. Clin Orthop Relat Res. 1987;223(3):213–9.
Valderrabano V. Joint-preserving surgery of ankle osteoarthritis. Foot Ankle Clin. 2013;18(3):xii–v.
Barg A, Amendola RL, Henninger HB, Kapron AL, Saltzman CL, Anderson AE. Measurement of supramalleolar alignment on the anteroposterior and hindfoot alignment views: Influence of ankle position and radiographic projection angle. Foot Ankle Int. 2015;36(11):1352–61.
Barg A, Harris MD, Henninger HB, Amendola RL, Saltzman CL, Hintermann B, et al. Medial distal tibial angle: comparison between weightbearing mortise view and hindfoot alignment view. Foot Ankle Int. 2012;33(8):655–61.
Egloff C, Paul J, Pagenstert G, Vavken P, Hintermann B, Valderrabano V, et al. Changes of density distribution of the subchondral bone plate after supramalleolar osteotomy for valgus ankle osteoarthritis. J Orthop Res. 2014;32(10):1356–61.
Gloyer M, Barg A, Horisberger M, Paul J, Pagenstert G, Valderrabano V. Joint preserving surgery in patients with valgus- and varus osteoarthritis. Fuss Sprungg. 2013;11(4):186–95.
Hintermann B, Knupp M, Barg A. Joint-preserving surgery of asymmetric ankle osteoarthritis with peritalar instability. Foot Ankle Clin. 2013;18(3):503–16.
Hintermann B, Knupp M, Barg A. Joint preserving surgery in patients with peritalar instability. Fuss Sprungg. 2013;11(4):196–206.
Hintermann B, Knupp M, Barg A. Supramalleolar osteotomies for ankle arthritis. J Am Acad Orthop Surg. 2016;24(7):424–32.
Knupp M, Barg A, Bolliger L, Hintermann B. Reconstructive surgery for overcorrected clubfoot in adults. J Bone Joint Surg Am. 2012;94(15):e1101–7.
Knupp M, Pagenstert G, Valderrabano V, Hintermann B. Osteotomies in varus malalignment of the ankle. Oper Orthop Traumatol. 2008;20(3):262–73.
Nuesch C, Barg A, Pagenstert GI, Valderrabano V. Biomechanics of asymmetric ankle osteoarthritis and its joint-preserving surgery. Foot Ankle Clin. 2013;18(3):427–36.
Nuesch C, Huber C, Paul J, Henninger HB, Pagenstert G, Valderrabano V, et al. Mid- to long-term clinical outcome and gait biomechanics after realignment surgery in asymmetric ankle osteoarthritis. Foot Ankle Int. 2015;36(8):908–18.
Nuesch C, Valderrabano V, Huber C, Pagenstert G. Effects of supramalleolar osteotomies for ankle osteoarthritis on foot kinematics and lower leg muscle activation during walking. Clin Biomech (Bristol, Avon). 2014;29(3):257–64.
Nuesch C, Valderrabano V, Huber C, von Tscharner V, Pagenstert G. Gait patterns of asymmetric ankle osteoarthritis patients. Clin Biomech (Bristol, Avon). 2012;27(6):613–8.
Pagenstert GI, Hintermann B, Barg A, Leumann A, Valderrabano V. Realignment surgery as alternative treatment of varus and valgus ankle osteoarthritis. Clin Orthop Relat Res. 2007;462(1):156–68.
Valderrabano V, Paul J, Monika H, Pagenstert GI, Henninger HB, Barg A. Joint-preserving surgery of valgus ankle osteoarthritis. Foot Ankle Clin. 2013;18(3):481–502.
DeHeer PA, Catoire SM, Taulman J, Borer B. Ankle arthrodesis: a literature review. Clin Podiatr Med Surg. 2012;29(4):509–27.
Muir DC, Amendola A, Saltzman CL. Long-term outcome of ankle arthrodesis. Foot Ankle Clin. 2002;7(4):703–8.
Stone JW. Arthroscopic ankle arthrodesis. Foot Ankle Clin. 2006;11(2):361–8.
Sealey RJ, Myerson MS, Molloy A, Gamba C, Jeng C, Kalesan B. Sagittal plane motion of the hindfoot following ankle arthrodesis: a prospective analysis. Foot Ankle Int. 2009;30(3):187–96.
Wood PL, Sutton C, Mishra V, Suneja R. A randomised, controlled trial of two mobile-bearing total ankle replacements. J Bone Joint Surg. 2009;91(1):69–74.
Nunley JA, Caputo AM, Easley ME, Cook C. Intermediate to long-term outcomes of the STAR Total Ankle Replacement: the patient perspective. J Bone Joint Surg Am. 2012;94(1):43–8.
Mann JA, Mann RA, Horton E. STAR ankle: long-term results. Foot Ankle Int. 2011;32(5):S473–84.
Culpan P, Le Strat V, Piriou P, Judet T. Arthrodesis after failed total ankle replacement. J Bone Joint Surg. 2007;89(9):1178–83.
Hopgood P, Kumar R, Wood PL. Ankle arthrodesis for failed total ankle replacement. J Bone Joint Surg. 2006;88(8):1032–8.
Kotnis R, Pasapula C, Anwar F, Cooke PH, Sharp RJ. The management of failed ankle replacement. J Bone Joint Surg. 2006;88(8):1039–47.
Rahm S, Klammer G, Benninger E, Gerber F, Farshad M, Espinosa N. Inferior results of salvage arthrodesis after failed ankle replacement compared to primary arthrodesis. Foot Ankle Int. 2015;36(4):349–59.
Sagherian BH, Claridge RJ. Salvage of failed total ankle replacement using tantalum trabecular metal: case series. Foot Ankle Int. 2015;36(3):318–24.
Hsu AR, Haddad SL, Myerson MS. Evaluation and management of the painful total ankle arthroplasty. J Am Acad Orthop Surg. 2015;23(5):272–82.
Williams JR, Wegner NJ, Sangeorzan BJ, Brage ME. Intraoperative and perioperative complications during revision arthroplasty for salvage of a failed total ankle arthroplasty. Foot Ankle Int. 2015;36(2):135–42.
Valderrabano V, Hintermann B, Nigg BM, Stefanyshyn D, Stergiou P. Kinematic changes after fusion and total replacement of the ankle: part 3: talar movement. Foot Ankle Int. 2003;24(12):897–900.
Valderrabano V, Hintermann B, Nigg BM, Stefanyshyn D, Stergiou P. Kinematic changes after fusion and total replacement of the ankle: part 2: movement transfer. Foot Ankle Int. 2003;24(12):888–96.
Valderrabano V, Hintermann B, Nigg BM, Stefanyshyn D, Stergiou P. Kinematic changes after fusion and total replacement of the ankle: part 1: range of motion. Foot Ankle Int. 2003;24(12):881–7.
Espinosa N, Walti M, Favre P, Snedeker JG. Misalignment of total ankle components can induce high joint contact pressures. J Bone Joint Surg Am. 2010;92(5):1179–87.
Kobayashi A, Minoda Y, Kadoya Y, Ohashi H, Takaoka K, Saltzman CL. Ankle arthroplasties generate wear particles similar to knee arthroplasties. Clin Orthop Relat Res. 2004;424 (1):69–72.
Harris NJ, Brooke BT, Sturdee S. A wear debris cyst following S.T.A.R. Total Ankle Replacement–surgical management. Foot Ankle Surg. 2009;15(1):43–5.
Scott AT, Nunley JA. Polyethylene fracture following STAR ankle arthroplasty: a report of three cases. Foot Ankle Int. 2009;30(4):375–9.
Haendlmayer KT, Fazly FM, Harris NJ. Periprosthetic fracture after total ankle replacement: surgical technique. Foot Ankle Int. 2009;30(12):1233–4.
McGarvey WC, Clanton TO, Lunz D. Malleolar fracture after total ankle arthroplasty: a comparison of two designs. Clin Orthop Relat Res. 2004;424:104–10.
Yang JH, Kim HJ, Yoon JR, Yoon YC. Minimally invasive plate osteosynthesis (MIPO) for periprosthetic fracture after total ankle arthroplasty: a case report. Foot Ankle Int. 2011;32(2):200–4.
Barg A, Hintermann B, Manegold S. Periprosthetic fractures in specific anatomical locations: ankle. In: Schuetz M, Perka C, editors. Periprosthetic fracture management. Davos: AO Trauma Thieme; 2014. p. 181–9.
Manegold S, Haas NP, Tsitsilonis S, Springer A, Mardian S, Schaser KD. Periprosthetic fractures in total ankle replacement: classification system and treatment algorithm. J Bone Joint Surg Am. 2013;95(9):815–20.
Jung HG, Parks BG, Nguyen A, Schon LC. Effect of tibiotalar joint arthrodesis on adjacent tarsal joint pressure in a cadaver model. Foot Ankle Int. 2007;28(1):103–8.
Weber BG, Simpson LA. Corrective lengthening osteotomy of the fibula. Clin Orthop Relat Res. 1985;199:61–7.
Saltzman CL, el-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995;16(9):572–6.
Acknowledgements
The authors thank Katharina Nikitina from the University of Freiburg, Germany, for her thorough literature review and her preparation of figures.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Barg, A., Gaffney, C.J., Valderrabano, V. (2016). Ankle Osteoarthritis. In: Valderrabano, V., Easley, M. (eds) Foot and Ankle Sports Orthopaedics. Springer, Cham. https://doi.org/10.1007/978-3-319-15735-1_33
Download citation
DOI: https://doi.org/10.1007/978-3-319-15735-1_33
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-15734-4
Online ISBN: 978-3-319-15735-1
eBook Packages: MedicineMedicine (R0)