Abstract
The purpose of this study was to evaluate the distribution rate of etiologies leading to ankle arthritis and to quantify and compare the important clinical and radiologic variables among these etiologic groups. We evaluated data from 390 patients (406 ankles) who consulted our center because of painful end-stage ankle osteoarthritis (OA) by using medical history, physical examination, and radiography. Posttraumatic ankle OA was seen in 78% of the cases (n = 318), secondary arthritis in 13% (n = 52), and primary OA in 9% (n = 36). The average American Orthopaedic Foot and Ankle Society (AOFAS) hindfoot score was 38 points (range, 0–74 points), range of motion was 22° (range, 0°−65°), and visual analog scale for pain was 6.8 (range, 2–10). Patients with posttraumatic end-stage ankle OA were younger than patients with primary OA. The average tibiotalar alignment was 88° (range, 51°–116°) and did not differ between the etiologic groups. Our study showed trauma is the main cause of ankle OA and primary OA is rare. In the majority of patients with ankle OA the average tibiotalar alignment is varus regardless of the underlying etiology.
Level of Evidence: Level IV, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 15% of the world’s adult population is affected by joint pain and disability resulting from OA [7], and approximately 1% have OA of the ankle [29]. Substantial clinical and basic research related to hip and knee OA has been performed; however, research related to ankle OA is sparse.
The knowledge of the underlying etiology is important for selecting the appropriate treatment for end-stage ankle OA (arthrodesis, total ankle arthroplasty). Although hip and knee OA are mostly of primary origin [9], clinical treatment studies of ankle OA have shown the most common type is of posttraumatic origin [25, 36, 39, 40]. Traumatic ankle injuries that may result in OA include fractures of the malleoli, tibial plafond, talus, isolated osteochondral damage of the talar dome, and ankle ligament injury [6, 20, 39]. In an epidemiologic study, the etiology distribution in a large group of patients with ankle OA was determined [33]; however, the specific clinical and radiologic characteristics of etiology subgroups in a large cohort of patients with ankle OA have not been described. This may be of importance, because for the definition of treatment algorithms for a specific ankle OA subgroup, it is not the distribution rate that is so important, but rather the knowledge of the typical clinical and radiologic characteristics of the subgroups. Therefore, the large cohort in our study provides the distribution rate of etiology and clinical and radiologic data for the etiologic subgroups.
We hypothesized that (1) trauma would be the main etiology of ankle OA; (2) there would be a difference in the clinical variables among the etiology groups; and (3) varus alignment would predominate. Consequently, the three main purposes of this etiologic cohort investigation were to determine the distribution rate among the three main etiology subgroups (ie, posttraumatic ankle OA, secondary arthritis, and primary OA), to quantify and compare the important clinical variables such as age, pain score, range of motion (ROM), and AOFAS score among the three etiologic subgroups, and finally, to similarly quantify and compare the important radiologic variables such as OA grade and radiologic alignment among the three main etiology subgroups.
Materials and Methods
Our study cohort included patients with symptomatic end-stage OA of the ankle who consulted our tertiary university orthopaedic foot and ankle center. In one decade, 390 patients (191 women; 199 men; 406 cases) met the inclusion criteria of symptomatic end-stage ankle OA (radiologic ankle OA grade greater than 2) (Table 1). Exclusion criteria were patients with low-symptomatic ankle OA (radiologic grade less than 1), patients with symptomatic ankle fusion, and patients with failed total ankle arthroplasty. The mean age of the cohort was 58 years (range, 22–90 years). There was no difference (p = 0.75) between the ages of the men (mean, 58 years; range, 22–83 years) and women (mean, 59 years; range, 27–90 years). The study was approved by the Medical Sciences Institutional Ethical Review Board of the authors’ university, and all subjects gave informed consent to participate. The study was performed in accordance with the World Medical Association Declaration of Helsinki.
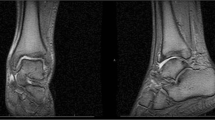
The included patients were analyzed clinically and radiologically. All data were collected by two individuals (VV, MH). When they disagreed in judgments, they discussed the data until consent was achieved. For determination of the underlying etiology (fractures, ligament lesions, rheumatoid arthritis, and others), medical history and all radiographs were studied carefully and additional information was obtained from the patients during the visit in which the indication for total ankle arthroplasty or ankle fusion was made. The indication for surgery was made by one author (BH) not involved in data collection. If no etiology was documented in the history or no cause could be elucidated at examination, the case was classified as primary ankle OA. The pain level was quantified using a visual analog scale with 0 representing no pain and 10 representing maximal pain. The AOFAS ankle score [17], which includes pain, function, and hindfoot alignment evaluations, was used to assess clinical-functional level (minimum score of 0 points; maximum score of 100 points). ROM was measured with a goniometer (degrees) for plantar flexion, dorsiflexion, and inversion/eversion as a percentage of either the uninvolved contralateral leg or of a healthy population as is required for the AOFAS ankle score. Body mass index (BMI) was calculated for all patients. The patients were examined radiologically using standard weightbearing radiographs in two planes (anteroposterior [AP] and lateral). The radiologic ankle arthritis grade was quantified based on the classification of Morrey and Wiedeman [27] (minimum score of 0 points; maximum score of 3 points). Ankle alignment was measured radiologically and digitally on the AP radiographs (radiologic ankle alignment; angular value between long tibial axis and talus surface on AP radiographs [18]) and defined as: normal alignment, 90° to 99°; varus alignment, less than 90°; and valgus alignment, 100° or greater.
Statistical analysis of the data was performed by an independent biostatistics expert using SPSS® software (Version 12.0; SPSS Inc, Chicago, IL). One-way ANOVA was performed to determine whether there was any overall group effect on the analyzed variables. For the variables with significant group effect (p < 0.05), a post hoc test (Student-Newman-Keul’s test) was performed to locate the differences within groups. For association between categorical variables, the chi square test was used. The significance level was set at p < 0.05.
Results
The underlying etiology in this cohort was posttraumatic ankle OA in 78% of the cases (318 ankles), secondary arthritis in 13% of the cases (52 cases), and primary OA in 9% of the cases (36 ankles) (Table 1). Patients in the posttraumatic ankle OA group had malleolar ankle fractures (AO fracture type 44; 39%), ankle ligament lesions (16%), pilon tibial fractures (AO fracture type 43, 14%), tibial shaft fractures (AO fracture type 42; 5%), talus fractures (2%), and severe combined fractures (2%). Patients in the secondary OA group had rheumatoid arthritis (5%), hemochromatosis (3%), hemophilia (1%), clubfoot deformity (1%), avascular necrosis of the talus (1%), osteochondritis dissecans (1%), and postinfectious arthritis (1%).
Clinical variables differed among the three etiologic groups. There was an age difference (p = 0.006) among patients in the main three etiology groups (Table 2). Patients in the primary OA group were older than patients in the posttraumatic OA group (p = 0.02) and in the secondary OA group (p = 0.01). Patients in the posttraumatic OA group did not differ (p = 0.6) in age from patients in the secondary OA group. There was a difference in pain (p = 0.04) among patients in the three etiology groups (Table 2). The overall mean pain score in this cohort was 6.8 points (range, 2–10 points). Patients in the primary OA group experienced less pain than patients in the posttraumatic OA group (p = 0.035) and the secondary OA group (p = 0.036). Between the posttraumatic OA and secondary OA groups, there was no difference (p = 0.6) in the pain level. Similarly, there was a difference (p = 0.03) in ROM among patients in the three etiology groups (Table 2). The overall mean ROM for dorsiflexion and plantar flexion was 22° (range, 0°–65°). Patients in the primary OA group had greater ROM than patients in the posttraumatic OA group (p = 0.02) and the secondary OA group (p = 0.04). There was no difference (p = 0.4) observed in ROM between patients in the posttraumatic OA and secondary OA groups. The AOFAS ankle score, representing a widely accepted clinical-functional evaluation of the patients, showed an overall mean of 38 points (range, 0–74 points). There was an AOFAS score difference (p = 0.04) among patients in the three etiology groups (Table 2). The score of patients in the posttraumatic OA was higher (p = 0.01) than that of patients in the secondary OA group. The other combinations were not different from each other: posttraumatic OA versus primary OA (p = 0.9) and secondary OA versus primary OA (p = 0.1). The average BMI was 26.7 kg/m2 (range, 18.2–44.3 26.7 kg/m2) with no statistically significant differences among the three groups (posttraumatic OA versus secondary arthritis, p = 0.12; posttraumatic OA versus primary OA, p = 0.78; secondary arthritis versus primary OA, p = 0.28).
There were no major differences seen in radiologic data among the three subgroups. The mean radiologic ankle OA grade in the entire cohort was 2.7 (range, 2–3). No differences (p = 0.2) were observed among the three etiology groups for OA grade, because end-stage ankle OA was an inclusion criterion. The mean radiologic ankle alignment in the entire cohort was 88.0° (range, 51°–116°). In the entire cohort, 55% of the patients (225 ankles) had varus alignment, 37% (148 ankles) had normal alignment, and 8% (33 ankles) had valgus alignment (Table 3). Similar alignment distribution (p = 0.8) was seen among the three etiology groups (Table 3).
Discussion
This study quantified the etiology of ankle OA in a large patient series and quantified clinical and radiologic characteristics for the specific etiologic groups. The major results of this study were (1) posttraumatic ankle OA was the most common etiology; (2) major differences exist in clinical variables among the three major etiology groups; and (3) varus alignment was the most common hindfoot alignment in ankle OA.
Our study has some limitations. First, the chosen cohort study with retrospective design does not allow a conclusion on the true prevalence rate of OA of the ankle. A prospective analysis of all possible etiologies (eg, malleolar fractures, ankle sprains, rheumatoid arthritis) scientifically would be more correct. However, knowing the long latency time of posttraumatic ankle OA, such a prospective study would have to be conducted for several decades or two physicians’ generations. In this context, to get substantial numbers of patients with primary ankle OA, a large population also would have to be observed prospectively for years. Second, our study did not address the exact pathomechanism of each of the etiology subgroups (Table 1), eg, specific patterns of the different fracture subgroups or ligament injuries. Thus, future studies should evaluate the exact underlying injury mechanisms of each of these subgroups in detail.
Compared with results reported for knee (67%) and hip (58%) OA [9], our results showed a substantially lower rate of primary ankle OA (9%). This phenomenon is thought to be caused by the unique anatomic, biomechanical, and cartilage characteristics of the ankle, which differ from those of other joints of the lower extremity [5, 12]. Specifically, it has been reported the ankle has a substantially smaller contact area than the hip or knee (at 500-N load: ankle, 350 mm2; hip, 1100 mm2; knee, 1120 mm2 [2, 13, 16]). Consequently, the ankle experiences more force per square centimeter than the knee or hip [37]. Functionally, the ankle acts mainly as a rolling joint with high congruency [41]. The knee, however, deals with higher shear forces by acting more as a rolling, sliding, and rotating joint during motion [41]. This difference may be one of the main reasons for increased cartilage degeneration and the high rate of primary OA in the knee [9, 41]. Although the ankle cartilage is thinner compared with knee or hip cartilage (ankle, 1.0–1.62 mm; knee, 1.69–2.55 mm; hip, 1.35–2.0 mm) [35], the ankle cartilage shows a higher compressive stiffness and proteoglycan density [41], lower matrix degradation [1], and less response to catabolic stimulations (as interleukin 1, fibronectin fragments) [5, 15]. This fact of relative higher cartilage resistance might protect the ankle from degenerative changes leading to primary OA.
Our study showed that in 78% of our patient cohort with ankle OA, a trauma event was responsible. This result is in the same order of magnitude as the results of the epidemiology study by Saltzman et al., who reported a posttraumatic ankle OA rate of 70% [33]. Of the 78% of cases of ankle OA in our study, 62% were attributable to fracture events (Table 1). The most common fracture type was the malleolar fracture (AO fracture type 44; 39%). This reflects the notion that fracture of the malleoli is the most severe risk factor for development of ankle OA [40]. Tibial plafond fractures, the second most frequent fracture type in our study, are known to be associated with a high rate of posttraumatic OA [4, 42]. This is believed to be caused by a combination of articular damage, avascular necrosis of fracture fragments, and/or difficulty in obtaining a satisfactory and accurate reduction [40]. Our results also support the notion that fracture of the talus may end in posttraumatic OA of the ankle.
In a prospective study of malleolar fractures, it was shown that the true prevalence of posttraumatic ankle OA after ankle fractures was 14% [20]. In articular ankle fractures, it was concluded the severity of articular cartilage damage and subtle joint instability (eg, mortise instability) might be determinants of posttraumatic ankle OA [22]. However, the influence of an anatomic reduction on the prevalence of posttraumatic OA is questionable. One study showed a positive correlation between reduction and functional outcome [32], whereas others have disclaimed this correlation [4, 42]. Although there is broad advocacy that the best fracture outcome is associated with minimal articular damage, anatomic reduction, early mobilization, and a lack of complications [22, 40], more basic and clinical research is needed to understand the development of posttraumatic OA after fractures and to identify optimal methods to prevent it.
In our cohort, 16% of the patients had an underlying ankle ligament lesion, ie, ligamentous posttraumatic ankle OA. This is consistent with a retrospective study in which 37 patients (13%) with chronic ankle instability had OA [21]. Another study reported an even higher ligamentous posttraumatic osteoarthritis rate of 78% (particularly varus OA) in 36 patients with chronic lateral ankle instability [10]. The underlying pathomechanisms causing secondary OA in ankle sprains might be twofold: either an acute osteochondral lesion [38], as in single severe ankle sprains, or chronic change in ankle mechanics leading to repetitive cartilage degeneration [11, 28], as in recurrent or chronic instable ankles.
Rheumatoid arthritis is a systemic disease often affecting the foot and ankle. Approximately 20% to 42% of patients with rheumatoid arthritis have foot and ankle symptoms [14]. In our study, rheumatoid arthritis was the major diagnosis of patients in the etiology group with nonposttraumatic secondary ankle OA, with a rate of 5% (Table 1). This rate was less than the 12% rate reported by Saltzman et al. [33], which could be explained by a different regional incidence of rheumatoid arthritis between their study patients and ours. Other systemic diseases such as hemochromatosis or hemophilia might be present in patients with secondary ankle OA, however, in a lower percentage than in patients with rheumatoid arthritis (Table 1).
Older age is considered a risk factor for development of OA [8, 26, 30]. In vitro studies showed the synthetic activity of chondrocytes in articular cartilage declines with age [23]. Furthermore, the rehabilitation potential or neuromuscular protective mechanisms in OA are known to be reduced in elderly patients owing to such factors as sarcopenia, reduced proprioception, and increased physical disability [19, 24]. Based on these aging aspects of tissues and the known relatively large latency time for development of ankle OA [3, 27, 43], the mean age and age distribution of our cohort (Fig. 1) might be explainable. Our study showed patients with primary OA presented at an older age than patients with posttraumatic or secondary OA (Table 2).
Impairment of functional ability, as represented by the clinical-functional AOFAS ankle score, was substantial in this cohort with ankle OA (Table 2), but comparable to reported rates [25, 36]. The documented ROM in the primary OA group was higher than in the posttraumatic or secondary OA group, as was the pain score. This might be explained by the less scarred and inflamed soft tissues in the primary OA group as compared with the other two groups and might allow a better long-term outcome.
Our alignment analysis showed dominance of varus alignment throughout the entire cohort (55%, n = 225) (Table 2; Fig. 2) and the three etiology groups (Table 3). Correlation between varus alignment and degeneration of the ankle has been reported, however, in a small sample [31]. A varus deformity of the ankle secondary to a fracture of the distal tibial epiphysis or the distal third of the tibial shaft can lead to OA and functional impairment of the ankle [34, 39]. This supports our finding that distal tibial shaft fracture (AO fracture type 42; Table 1) may end in posttraumatic ankle OA. Also, malleolar fractures may result in a varus alignment [39]. Varus alignment also might be a common finding in chronic ankle instability [10], and there might be a biomechanical explanation for this. In a kinematic gait analysis, it was found that ankles that have sustained an injury to the lateral ligaments abnormally pronate and rotate externally at the time of heel strike and abnormally supinate (ie, varization of the heel) and rotate internally during the acceleration phase [11]. These changes in ankle mechanics, together with a potential peroneal muscle dysfunction, may lead to repetitive cartilage damage of the medial ankle by increased rotatory shear forces and may support the development of varus-malaligned ankle OA.
Our study showed in most of the cases, ankle OA developed secondary to trauma, mostly malleolar fractures, ankle ligament lesions, and tibial plafond fractures. Primary OA, ie, OA with no history of trauma or any kind of secondary or infectious OA, in the ankle is rare. Patients with posttraumatic ankle OA or secondary OA are preferentially younger than patients with primary OA. Also, patients with ankle OA predominantly have varus alignment. Because trauma is the dominant etiology of ankle OA, more research is needed to determine contributing factors of OA and prevent development of posttraumatic ankle OA.
References
Aurich M, Squires GR, Reiner A, Mollenhauer JA, Kuettner KE, Poole AR, Cole AA. Differential matrix degradation and turnover in early cartilage lesions of human knee and ankle joints. Arthritis Rheum. 2005;52:112–119.
Brown TD, Shaw DT. In vitro contact stress distributions in the natural human hip. J Biomech. 1983;16:373–384.
Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83:219–228.
DeCoster TA, Willis MC, Marsh JL, Williams TM, Nepola JV, Dirschl DR, Hurwitz SR. Rank order analysis of tibial plafond fractures: does injury or reduction predict outcome? Foot Ankle Int. 1999;20:44–49.
Eger W, Schumacher BL, Mollenhauer J, Kuettner KE, Cole AA. Human knee and ankle cartilage explants: catabolic differences. J Orthop Res. 2002;20:526–534.
Elgafy H, Ebraheim NA, Tile M, Stephen D, Kase J. Fractures of the talus: experience of two level 1 trauma centers. Foot Ankle Int. 2000;21:1023–1029.
Felson DT. The epidemiology of osteoarthritis: prevalence and risk factors. In: Kuettner KE, Goldberg VM, eds. Osteoarthritis Disorders. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1995:13–24.
Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Joint injury in young adults and risk for subsequent knee and hip osteoarthritis. Ann Intern Med. 2000;133:321–328.
Gunther KP, Sturmer T, Sauerland S, Zeissig I, Sun Y, Kessler S, Scharf HP, Brenner H, Puhl W. Prevalence of generalised osteoarthritis in patients with advanced hip and knee osteoarthritis: the Ulm Osteoarthritis Study. Ann Rheum Dis. 1998;57:717–723.
Harrington KD. Degenerative arthritis of the ankle secondary to long-standing lateral ligament instability. J Bone Joint Surg Am. 1979;61:354–361.
Hashimoto T, Inokuchi S. A kinematic study of ankle joint instability due to rupture of the lateral ligaments. Foot Ankle Int. 1997;18:729–734.
Huch K, Kuettner KE, Dieppe P. Osteoarthritis in ankle and knee joints. Semin Arthritis Rheum. 1997;26:667–674.
Ihn JC, Kim SJ, Park IH. In vitro study of contact area and pressure distribution in the human knee after partial and total meniscectomy. Int Orthop. 1993;17:214–218.
Jaakkola JI, Mann RA. A review of rheumatoid arthritis affecting the foot and ankle. Foot Ankle Int. 2004;25:866–874.
Kang Y, Koepp H, Cole AA, Kuettner KE, Homandberg GA. Cultured human ankle and knee cartilage differ in susceptibility to damage mediated by fibronectin fragments. J Orthop Res. 1998;16:551–556.
Kimizuka M, Kurosawa H, Fukubayashi T. Load-bearing pattern of the ankle joint: contact area and pressure distribution. Arch Orthop Trauma Surg. 1980;96:45–49.
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–353.
Knupp M, Ledermann H, Magerkurth O, Hinterman B. The surgical tibiotalar angle: a radiologic study. Foot Ankle Int. 2005;26:713–716.
Koralewicz LM, Engh GA. Comparison of proprioception in arthritic and age-matched normal knees. J Bone Joint Surg Am. 2000;82:1582–1588.
Lindsjö U. Operative treatment of ankle fracture-dislocations: a follow-up study of 306/321 consecutive cases. Clin Orthop Relat Res. 1985;199:28–38.
Lofvenberg R, Karrholm J, Lund B. The outcome of nonoperated patients with chronic lateral instability of the ankle: a 20-year follow-up study. Foot Ankle Int. 1994;15:165–169.
Marsh JL, Buckwalter J, Gelberman R, Dirschl D, Olson S, Brown T, Llinias A. Articular fractures: does an anatomic reduction really change the result? J Bone Joint Surg Am. 2002;84:1259–1271.
Martin JA, Ellerbroek SM, Buckwalter JA. Age-related decline in chondrocyte response to insulin-like growth factor: I. The role of growth factor binding proteins. J Orthop Res. 1997;15:491–498.
Melton LJ III, Khosla S, Crowson CS, O’Connor MK, O’Fallon WM, Riggs BL. Epidemiology of sarcopenia. J Am Geriatr Soc. 2000;48:625–630.
Monroe MT, Beals TC, Manoli A. Clinical outcome of arthrodesis of the ankle using rigid internal fixation with cancellous screws. Foot Ankle Int. 1999;20:227–231.
Mont MA, Sedlin ED, Weiner LS, Miller AR. Postoperative radiographs as predictors of clinical outcome in unstable ankle fractures. J Orthop Trauma. 1992;6:352–357.
Morrey BF, Wiedeman GP Jr. Complications and long-term results of ankle arthrodeses following trauma. J Bone Joint Surg Am. 1980;62:777–784.
Okuda R, Kinoshita M, Morikawa J, Yasuda T, Abe M. Arthroscopic findings in chronic lateral ankle instability: do focal chondral lesions influence the results of ligament reconstruction? Am J Sports Med. 2005;33:35–42.
Peyron JG. The epidemiology of osteoarthritis. In: Moskowitz RW, Howell DS, Goldberg VM, Mankin HJ, eds. Osteoarthritis. Diagnosis and Treatment. Philadelphia, PA: WB Saunders; 1984:9–27.
Phillips WA, Schwartz HS, Keller CS, Woodward HR, Rudd WS, Spiegel PG, Laros GS. A prospective, randomized study of the management of severe ankle fractures. J Bone Joint Surg Am. 1985;67:67–78.
Puno RM, Vaughan JJ, Stetten ML, Johnson JR. Long-term effects of tibial angular malunion on the knee and ankle joints. J Orthop Trauma. 1991;5:247–254.
Ruedi T. Fractures of the lower end of the tibia into the ankle joint: results 9 years after open reduction and internal fixation. Injury. 1973;5:130–134.
Saltzman CL, Salamon ML, Blanchard GM, Huff T, Hayes A, Buckwalter JA, Amendola A. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–46.
Seitz WH, Andrews DL, Shelton ML, Feldman F. Triplane fractures of the adolescent ankle: a report of three cases. Injury. 1985;16:547–553.
Shepherd DE, Seedhom BB. Thickness of human articular cartilage in joints of the lower limb. Ann Rheum Dis. 1999;58:27–34.
Stamatis ED, Cooper PS, Myerson MS. Supramalleolar osteotomy for the treatment of distal tibial angular deformities and arthritis of the ankle joint. Foot Ankle Int. 2003;24:754–764.
Stauffer RN, Chao EY, Brewster RC. Force and motion analysis of the normal, diseased, and prosthetic ankle joint. Clin Orthop Relat Res. 1977;127:189–196.
Taga I, Shino K, Inoue M, Nakata K, Maeda A. Articular cartilage lesions in ankles with lateral ligament injury: an arthroscopic study. Am J Sports Med. 1993;21:120–126.
Takakura Y, Takaoka T, Tanaka Y, Yajima H, Tamai S. Results of opening-wedge osteotomy for the treatment of a post-traumatic varus deformity of the ankle. J Bone Joint Surg Am. 1998;80:213–218.
Thomas RH, Daniels TR. Current concepts review: ankle arthritis. J Bone Joint Surg Am. 2003;85:923–936.
Treppo S, Koepp H, Quan EC, Cole AA, Kuettner KE, Grodzinsky AJ. Comparison of biomechanical and biochemical properties of cartilage from human knee and ankle pairs. J Orthop Res. 2000;18:739–748.
Wyrsch B, McFerran MA, McAndrew M, Limbird TJ, Harper MC, Johnson KD, Schwartz HS. Operative treatment of fractures of the tibial plafond: a randomized, prospective study. J Bone Joint Surg Am. 1996;78:1646–1657.
Wyss C, Zollinger H. The causes of subsequent arthrodesis of the ankle joint. Acta Orthop Belg. 1991;57(suppl 1):22–27.
Acknowledgments
We thank Dr Tak S. Fung, Statistics/University of Calgary, for verifying the statistical treatment of the data.
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors (VV) has received funding from the Swiss National Research Foundation (SNF Number PBZHB-106269).
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Valderrabano, V., Horisberger, M., Russell, I. et al. Etiology of Ankle Osteoarthritis. Clin Orthop Relat Res 467, 1800–1806 (2009). https://doi.org/10.1007/s11999-008-0543-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-008-0543-6