Abstract
Vertical root fracture in an endodontically treated tooth originates from the root at any level and is considered a frustrating and vexing complication in endodontic therapy. Many times, it is difficult to achieve an accurate diagnosis and to differentiate the fracture from other clinical entities. However, usually combination of cervicaly located sinus tract combined with a narrow deep periodontal defect present is highly suggestive of a vertical root fracture. When the diagnosis of a vertical root fracture is made, usually years after all endodontic and restorative procedures have been completed, extraction of the tooth or root should be done in a timely manner to minimize the bone loss in the surrounding bone. This bone loss may compromise subsequent implant placement in the area. This chapter will emphasize the importance of achieving an accurate and timely vertical root fracture diagnosis and will describe the more typical signs, symptoms, and radiographic features that are suggestive for vertical root fracture diagnosis in the susceptible teeth and roots.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The vertical root fracture (VRF) is not uncommon [1]. This is a frustrating complication of endodontically treated teeth and is often difficult to identify [2]. The treatment plan is straightforward, that is, extraction of a single-rooted tooth or at least root removal in a molar. So the definitive and accurate diagnosis is important; the clinician does not wish to remove a nonfractured root. A further complication is that the VRF is frequently problematic to diagnose; these root fractures usually mimic other conditions. Signs and symptoms, for example, dull pain or pain on mastication, mobility, presence of a sinus tract, deep probing defects, a periodontal-type abscess, and periapical radiolucencies, are often similar to those found in failing root canal treatment or in periodontal disease [3–7]. A mistake in identification would lead to other inappropriate management. An example would be periodontal treatment or root canal retreatment; the VRF has damaged the periodontium to the point that it is mistaken for another entity. Complications in diagnosis of teeth scheduled for endodontic surgery may occur because of other causes such as a periodontal condition, VRF, and misdiagnosis of nonendodontic pathosis mimicking inflammatory periapical lesions [8]. An error in diagnosis is devastating and may have serious consequences. Therefore the need for a cautious and rigorous approach to identification of a suspected VRF.
How can the clinician make a definitive diagnosis and identification of a VRF? Are there any absolute signs, symptoms, tests, radiographic characteristics, or combinations that are “classic” for VRF? It is commonly believed that certain findings, for example, two narrow probing defects or two sinus tracts (one on the buccal and one on the lingual), indicate a VRF. If that is the finding, is this tooth to be extracted? The answer is probably yes, but this alone is not pathognomonic. In fact, with the evidence available, there are no noninvasive tests that are definitive for VRF.
A problem in recounting available information is always to locate and report on sound, evidence-based research. This is largely lacking on this topic. An article [9] systematically reviewed the subject of diagnosis of VRF in endodontically treated teeth. The conclusion was that there are not substantive evidence-based data concerning the diagnostic accuracy as to the effectiveness of clinical and radiographic evaluation. However, it is difficult to design randomized trials with controls (high levels of evidence of 1 and 2) on this type of complication because treatment is required. To date, most published information is lower levels of evidence [3–5] represented by case reports, case series, or case report studies.
Therefore, much of what is included in this chapter is based on the information that is currently available. Careful application, in fact, will usually result in accurate identification and diagnosis and ultimately the proper treatment.
Pathogenesis
This is reviewed in more detail in “Pathogenesis” (Chap. 6). The pathogenesis is an important consideration in designing a diagnostic approach because of the nature of the injury and the outcome. The histology of the VRF on extracted, fractured roots was examined by Walton et al. [10]. The findings were that the irritants from the fracture line generate an inflammatory lesion that results in irreversible linear devastation to the soft tissues and bone of the periodontium. This mimics other entities such as a periodontal-like defect or failed root canal treatment. The fracture may be complete apical to coronal/facial to lingual or incomplete. This further confuses the diagnosis [1]. Thus, the objective is differential diagnosis.
Diagnosis
A diagnostic process is based on the combination of the patient’s subjective complaints and objective clinical and radiographic evaluation. In the case of VRF diagnosis, there is no known single pathognomonic sign, symptom, or radiographic feature to make the diagnosis definitive [11].
Importantly, most means of examination at the clinician’s disposal must be employed when trying to achieve accurate and timely diagnosis of VRF. Omission of a step may result in an error. The sequence is the following: (1) Subjective evaluation, (2) Objective tests, (3) Radiographic findings, (4) History of the tooth, (5) Flap reflection when indicated. Usually, there are no specific combinations of noninvasive, classic tests or signs and symptoms that would predictable identify a VRF. There are findings—clinical and radiographic ones [12]—that strongly suggested a VRF, but usually flap reflection is necessary. The factors that point in the direction of fracture are reviewed below.
Subjective Evaluation
Interestingly (and importantly), symptoms tend to be minimal, that is, none to mild pain [7, 12]. Seldom are the pain levels moderate or severe. So the VRF does not elicit symptoms that bring the patient to the dentist. Often, the patient detects some mobility, but usually the tooth is stable. Symptoms from the periapical region, that is, pain on mastication, is common but mild. Many of these vertical root fractures may resemble periodontal lesions; the patient may report some localized swelling or a bad taste from drainage of a periodontal-type abscess. They may also report a “gum boil” (draining sinus tract) [1, 3, 4].
Objective Pulpal and Periapical Tests
-
Pulpal: Because the tooth has had root canal treatment, these are not useful.
-
Periapical: These are not particularly useful either. Percussion and palpation usually generate a mild response, which is not diagnostic for VRF.
Clinical Examination Findings
A common finding is a sinus tract or a gingival swelling (Fig. 4.1a). Again, these may mimic either a periodontal or an endodontic lesion.
Common findings: (a) A highly located sinus tract in a mandibular molar. (b) A highly located sinus tract and deep probing in midbuccal area of another mandibular molar. The periapical radiograph (c) shows a combined bony lesion in the bifurcation area and along the lateral aspect of the mesial root which is typical for VRF in mandibular molars. The combination of the clinical signs in the endodonyically treated tooth is considered pathognomonic for VRFs
Probing Patterns
These are more diagnostic although not absolute. There is a common assumption that VRFs produce narrow and deep defects on the facial and/or lingual surfaces representing the periodontal breakdown and inflammatory process facing the fracture [10, 13, 14]. Although this may occur, patterns are not predictable. Significantly, some teeth with vertical root fractures have normal probing depths. In a recent clinical prevalence study [15], in less than 24 % of the VRF cases was a deep probing defect found. However, most do show significant deep defects with narrow or rectangular patterns (Figs. 4.1b, c and 4.2). These also are often indicative of endodontic-type lesions. When present, these deep defects are not necessarily on both the facial and lingual aspects. When they are deep on the facial and lingual, VRF is strongly suspected, but if this is the only clinical sign, it is not pathognomonic. In summary, probing patterns are not in themselves totally diagnostic. However, these deep defects in association with other findings strongly suggest the presence of a fracture. In 2008 [16], the Guidelines of the American Association of Endodontists stated that when there is a combination of a probing defect coupled with a sinus tract in an endodontically treated tooth (with or without a post), this is often pathognomonic for a VRF (Figs.4.1b, c and 4.3).
Deep probing defects may occur on different surfaces but mostly in the buccal aspect as the buccal cortical plate is much thinner than the lingual and the palatal ones. (a) Mesiobuccal probing defect in a maxillary lateral incisor. (b) Periapical radiograph of a maxillary molar, showing the large bone loss along the MB root causing deep probing defects in the buccal as well as in the palatal. (c) A sinus tract can be seen as well on the attached gingivae at the palatal aspect
A “pathognomonic combination” for VRF. A deep probing defect on the mesiobuccal aspect of the tooth and gutta-percha tracing cone through a highly located sinus tract (a) is directing to a “halo” radiolucency surrounding endodontically treated and restored mandibular premolar (b) (Courtesy Dr. S. Taschieri)
Often, this “pathognomonic combination” does not exist, resulting in a high percentage of misdiagnoses [4].
Radiographic Findings
Radiographs show a very wide variation of patterns of bone resorption [7, 12]. These resorptive lesions are adjacent rather than within the tooth itself. Very rarely can a tiny hair-like radiolucent fracture line be demonstrated in a root.
There are no specific radiographic pathognomonic findings because there is an assortment of patterns that often resemble other entities such as periodontal or endodontic inflammatory resorptive lesions [16]. Importantly, a vertical root fracture may demonstrate no radiographic changes [4, 10]. In a recent publication [15], it was shown that many of the VRF cases did not show any pathological bony changes (Fig. 4.4). The clinician must rely on other suggestive findings to help make a correct and timely diagnosis.
A most frequent radiographic feature of VRF is the “halo” (“J shaped”) (Figs. 4.5 and 4.6) appearance. This is a combined periapical and lateral radiolucency along the side of the root or a lateral radiolucency on one or both sides of the root. It may also present as an angular radiolucency from the crestal bone terminating on the side of the root (Fig. 4.7).
In mandibular molars, a furcal radiolucency is frequently found (Fig. 4.8) and is often coupled with other periapical/lateral changes [4, 12, 14]. The radiolucency may have other more familiar configurations such as the periapical “hanging-drop” shape (Fig. 4.9), thus resembling a lesion of failed root canal treatment [3].
Separated root segments are seldom visible on radiographs. If there is obvious separation, this is usually accompanied by a large radiolucency including and between the roots; this is inflammatory tissue separating the segments [17]. Obviously, when visible, these are absolutely diagnostic (Fig. 4.10). Segment separation with the large resorptive lesion indicates a long-standing event probably unnoticed by the patient. Lustig et al. [11] found that in most patients with other signs and symptoms (sinus tract, large osseous defect, mobility), or with acute exacerbations, greater interproximal bone loss was recorded than in patients in whom the VRF diagnosis was made at an early stage.
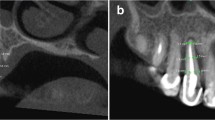
Computed tomography has been examined as a means of identifying vertical fractures of the root [18, 19]. Most studies have been in vitro with artificially generated fractures that really cannot be compared to in vivo situations. These are quite different than the actual fracture in situ; the data from these studies may not be useful in clinical situations. Also, the obturating materials that are always present and posts that are often in place may interfere with the beam and cause scattering. This would mask the presence of the fracture anyway. However, an advantage in cone beam computed tomography may be the ability to identify and study more subtle patterns of bone resorption that are not visible on standard digital or analogue radiographs; this has not been thoroughly examined in clinical trials. There have been publications in recent years claiming to demonstrate the superiority of CBCT scans over periapical radiographs to diagnose VRFs [19–21]. However, there is considerable heterogeneity in the experimental design of these studies resulting in a wide variability in the outcomes. At this point of time, there is insufficient evidence to suggest the superiority of CBCT over conventional radiographs to detect VRFs [22]. In fact, the American Association of Endodontists Colleagues for Excellence - Cone Beam Computed Tomography in Endodontics stated [23], “What may be observed is the resultant vertical bone loss in one or more scans” rather than the fracture itself (Fig. 4.11).
There is the common error of noting a radiolucent line separating the obturating material from the canal wall [7]. This is likely a radiolucent artifact. This artifact is common and is adjacent to gutta-percha or a post or is an incomplete root canal filling. This thin radiolucent line may also represent an overlying bony pattern or another radiographic structure that is easily confused with a fracture.
Therefore, radiographs (including CBCT) can be helpful in identifying a suspected vertical root fracture but are seldom solely diagnostic except in those few instances when the fracture segment separation is readily visible.
Dental History
Identifying and considering past procedures that impact the root is very helpful in diagnosis. Vertical root fractures do not occur spontaneously. There is a defined history of certain treatment modalities. These procedures have generated lateral wedging forces. All fractured roots have experienced root canal treatment and/or root end surgery as well [15]. Many will demonstrate post placement. Different types of obturations are associated although those that generate more destructive forces such as lateral or vertical condensation tend to be major culprits [24, 25]. Certain post designs, particularly custom tapered posts, also generate more wedging forces [26–28]. Canal preparation techniques that remove more tooth structure have more potential to result in fractures [29–31]. These may be as part of root canal treatment or post preparation (See also Chap. 3).
Endodontic and restorative procedures may have been completed years before the fracture manifests itself clinically. Forces that stress the dentin are established early, but the actual fracture may begin and grow later taking considerable time to reach a root surface. It is seldom a sudden catastrophic event.
Root Anatomy
The shape of the root and size of canal in cross section are considered to be predisposing factors. This shape should be determined as it is indicative of what may be a VRF. Those with narrow mesial–distal and deep facial–lingual shapes are the most susceptible [32, 33]. These susceptible teeth and roots are the maxillary and mandibular premolars, mesial roots of mandibular molars, and mandibular anteriors. Therefore, more bulky roots such as maxillary central incisors and lingual roots of maxillary molars seldom fracture (Fig. 4.12) (See also Chap. 3).
Flap Reflection
To summarize the above information, seldom do any combinations of signs, symptoms, tests, or findings predictably identify the vertical root fracture. If this were true, the clinician could confidently extract the tooth or remove the fractured root from a molar. In studies on diagnosis [11, 12], all suspected teeth were subjected to flap reflection to examine bone and root patterns. It was determined that this exposure was the best and most reliable diagnostic approach for fracture confirmation. Vertical root fractures have consistent pathological patterns because of the potency of the irritants and the longitudinal nature of the fracture and accompanying inflammation. The inflammation stimulates bony resorption that is oblong and overlies the root surface. There is a visible “punched-out” bony defect taking the form of a dehiscence or fenestration at various root levels (Figs. 4.13, 4.14 and 4.15). Usually, the defect is cervical to apical but may be more limited. The defect is filled with granulomatous tissue.
After the granulomatous tissue is removed, the fracture is usually but not always visible on the root (Figs. 4.14 and 4.15). The operating microscope and application of a dye such as methylene blue are useful. If not readily obvious, the fracture may be very small or on a line angle of the root and tucked behind a bony ledge. Transillumination may be helpful as well. If the fracture line is still not visible, it is possible that this represents failed root treatment requiring surgical correction. An aggressive root end resection is then performed and the resected root end carefully examined. If a fracture line is still not identified, the root end surgery may be completed. The prognosis is questionable as the fracture may not extend as far as the level of resection and therefore not visible. If the fracture is an incomplete one on the lingual aspect of a maxillary premolar, it can be missed during endodontic surgery and will cause eventually unsuccessful results [34].
Treatment Choices
The patient is informed prior to flap reflection that there are two alternatives if the fracture is identified. One is that the tooth or the root on a molar (root amputation) [35] (Fig. 4.16) is removed at that time (see also Chap. 6). The other approach is to delay extraction until a future appointment. Biologically, the best approach is immediate extraction as there will be further bone resorption if the fractured root is not removed. The future rehabilitation of the area of extraction will then be much more difficult (see also Chap. 7).
Treatment option on a mandibular molar. (a) “pathognomonic combination” in a mandibular first molar. 9 mm probing in midbuccal area, and a cervicaly located sinus tract (arrow). (b) Periapical radiograph reveals combined bifurcation and “halo” radiolucency around the mesial root. (c) Following crown removal, the mesial root was amputated
Conclusions
Treatment of the vertical root fracture is straightforward most of the times but diagnosis is often challenging and has to be done accurately and in a timely manner. A series of findings is suggestive of a fracture. However, there are no noninvasive findings including subjective, objective, probing, radiographic, or clinical observations that are definitive. Certain combinations are indicative: deep probing defects, localized swelling, a sinus tract, and radiographic changes are very suggestive. Flap reflection has been shown to be the final and most reliable approach. The findings of dehiscences and fenestration bony defects filled with inflammatory tissue as well as the visualized fracture line are pathognomonic. The treatment is then extraction of the tooth if single rooted. As an alternative, if the tooth is multirooted, the fractured root may be removed, thus retaining the remainder of the tooth.
Bibliography
Tamse A. Vertical root fractures in endodontically treated teeth. In: Ingle JI, Backland LK, Baumgartner JC, editors. Ingle’s endodontics. 6th ed. Hamilton: BC Decker Inc; 2008. p. 676–89.
Pitts DL, Natkin E. Diagnosis and treatment of vertical root fractures. J Endod. 1983;9:338–46.
Rivera E, Walton R. Longitudinal tooth fractures: findings that contribute to complex endodontic diagnosis. Endod Top. 2009;16:82–111.
Tamse A, Fuss Z, Lustig J, Kaplavi J. An evaluation of endodontically treated vertically fractured teeth. J Endod. 1999;25:506–8.
Tamse A. Iatrogenic vertical root fractures in endodontically treated teeth. Endod Dent Traumatol. 1988;4:190–6.
Fuss Z, Lustig J, Katz A, Tamse A. An evaluation of endodontically treated vertical root fractured teeth: impact of operative procedures. J Endod. 2001;27:46–8.
Rivera E, Walton R. Longitudinal tooth fractures. In: Torabinejad M, Walton R, Fouad A, editors. Endodontics: principles and practice. 5th ed. St Louis: Elsevier; 2015. p. 121–41.
Vered M, Tamse A, Tsesis I, Rosen E. Zebra Hunt: clinical reasoning and misdiagnoses. In: Tsesis I, editor. Complications in endodontic surgery. Heidelberg: Springer; 2014. p. 7–17.
Tsesis I, Rosen E, Tamse A, Taschieri S, Kfir A. Diagnosis of vertical root fractures in endodontically teated teeth based on clinical and radiographic indices: systematic review. J Endod. 2010;36:1455–8.
Walton R, Michelich R, Smith GN. The histopathogenesis of vertical root fractures. J Endod. 1984;10:48–56.
Lustig J, Tamse A, Fuss Z. Pattern of bone resorption in vertically fractured, endodontically treated teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:224–7.
Tamse A, Kaffe I, Lustig J, et al. Radiographic features of vertically fractured endodontically treated mesial roots of mandibular molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:797–802.
Harrington G. The perio-endo question: differential diagnosis. Dent Clin North Am. 1979;23:673–90.
Nicopoulou-Karayianni K, Bragger U, Lang N. Patterns of periodontal destruction associated with incomplete root fractures. Dentomaxillofac Radiol. 1997;26:321–6.
Karygianni L, Krengel M, Winter M, Stampf S, Wrbas KT. Comparative assessment of the incidence of vertical root fractures between conventional versus surgical endodontic retreatment. Clin Oral Investig. 2014;18:2015–21.
Colleagues for Excellence. Cracking the cracked tooth code: detection and treatment of various longitudinal tooth fractures. Chicago: American Association of Endodontists; 2008.
Moule A, Kahler B. Diagnosis and management of teeth with vertical root fractures. Aust Dent J. 1999;44:75–87.
Mora M, Mol A, Tnydall D, Rivera E. In vitro assessment of local computed tomography for the detection of longitudinal tooth fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:825–9.
Metska M, Aartman I, Wesselink P, Ozok A. Detection of vertical root fractures in vivo in endodontically treated teeth by cone-beam computed tomography scans. J Endod. 2012;38:1344–7.
Bernardes RA, Moraes IG, Duarte MAH, Azevedo BC, Azevedo JR, Bramante CM. Cone-beam volumetric tomography in diagnosis of root fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:270–7.
Edlund M, Nair M, Nair U. Detection of vertical root fracture with cone-beam tomography. J Endod. 2011;37:768–72.
Corbella S, Del Fabbro M, Tamse A, Rosen E, Tsesis I, Taschieri S. Cone beam computed tomography for the diagnosis of vertical root fractures: a systematic review of the literature and meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118(5):593–602.
Colleagues for Excellence. Cone beam-computed tomography in endodontics. Chicago: American Association of Endodontists; 2011.
Dang D, Walton R. Vertical root fracture and root distortion: effect of spreader design. J Endod. 1989;15:294–301.
Murgel C, Walton R. Vertical root fracture and dentin deformation in curved roots: the influence of spreader design. Endod Dent Traumatol. 1990;6:273–8.
Obermayr G, Walton R, Leary J, Krell K. Vertical root fracture and relative deformation during obturation and post cementation. J Prosthet Dent. 1991;66:181–7.
Ross R, Nicholls J, Harrington G. A comparison of strains generated during placement of five endodontic posts. J Endod. 1991;17:450–6.
Al-Omari M, Rayyan M, Abu-Hammad O. Stress analysis of endodontically treated teeth restored with post-retained crowns: a finite element analysis study. J Am Dent Assoc. 2011;142:289–300.
Ricks-Williamson LJ, Fotos PG, Goel VK, Spivey JV, Rivera EM, Khera AC. A three-dimensional finite-element stress analysis of an endodontically prepared maxillary central incisor. J Endod. 1995;21:362–7.
Wilcox L, Roskelley C, Sutton T. The relationship of root canal enlargement to finger-spreader induced vertical root fracture. J Endod. 1997;23:533–4.
Lam P, Palamara J, Messer H. Fracture strength of tooth roots following canal preparation by hand and rotary instrumentation. J Endod. 2005;31:529–32.
Lertchirakarn V, Palamara J, Messer H. Patterns of vertical root fracture: factors affecting stress distribution in the root canal. J Endod. 2003;29:523–8.
Gutmann JL. The dentin-root complex: Anatomic and biologic considerations in restoring endodontically treated teeth. J Prosthet Dent. 1992;67:458–67.
Vered M, Tamse A, Tsesis I, Rosen E. Zebra Hunt: clinical reasoning and misdiagnosis. In: Tsesis I, editor. Complications in endodontic surgery prevention, identification and management. Heidelberg: Springer; 2014.
Floratos SG, Krachman SI. Surgical management of vertical root fractures for posterior teeth. Report of four cases. J Endod. 2012;38:550–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Walton, R.E., Tamse, A. (2015). Diagnosis of Vertical Root Fractures. In: Tamse, A., Tsesis, I., Rosen, E. (eds) Vertical Root Fractures in Dentistry. Springer, Cham. https://doi.org/10.1007/978-3-319-16847-0_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-16847-0_4
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16846-3
Online ISBN: 978-3-319-16847-0
eBook Packages: MedicineMedicine (R0)