Abstract
Objectives
Vertical root fractures (VRFs) are a common cause of tooth loss. Little evidence exists though, relating the incidence of VRFs to the type of endodontic retreatment. This retrospective study aimed at evaluating the impact of conventional versus surgical endodontics on root canal-filled teeth with VRFs.
Materials and methods
Over a period of 13 years, 200 endodontically retreated teeth from 192 patients with VRFs were extracted and further examined. VRFs were assessed in relation to age, gender, tooth group, clinical signs, extension on the root surface, patency, as well as type of endodontic retreatment and restoration. Statistical analysis was conducted using a Cox PH Model, Chi-squared, Wilcoxon rank-sum, and Log rank tests at a significance level of 5 %.
Results
The majority of teeth with VRFs (62.31 %) had undergone the combination of conventional root canal retreatment and apical surgery. Women (64.06 %) presented VRFs more frequently than men (35.94 %) at the mean age of 51.1 and 55.1 years, respectively. Maxillary first (17.5 %) and second (16.5 %) premolars, restored by a resin-based material without a post (56.28 %) were more susceptible to VRFs. Apically initiated (84.1 %) VRFs could be diagnosed more easily on radiographs.
Conclusions
The type of endodontic treatment strongly correlated with VRFs. The prevalence of VRFs in teeth having undergone both conventional and surgical endodontic retreatment could be attributed, among others, to additive dentin damage related to the aforementioned endodontic procedures.
Clinical relevance
The possible involvement of endodontic retreatment in the multifactorial etiology of VRFs needs to be taken into consideration in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Novel NiTi retreatment systems and root canal obturation techniques allow for minimized dentin loss of root canals during endodontic procedures and thus, for fracture resistance of root canal-treated teeth in the long term [1]. However, these vast improvements in modern endodontics are still accompanied by the unexpected occurrence of vertical root fractures (VRFs) in root canal-treated teeth. According to the American Association of Endodontists, vertically fractured teeth are characterized by a crack that begins in the root at any level and extends toward the occlusal surface, usually in the bucco-lingual direction [2].
The diagnosis of VRFs, usually years after the final crown restoration of the root canal-treated teeth, may be confusing because of the existence of nonspecific radiographic and clinical signs that imitate endodontic treatment failure or periodontal disease [3, 4]. Representative clinical features of VRFs usually include a deep, thread-thin, isolated periodontal pocket, and multiple sinus tracts, sometimes situated coronally on both the buccal and lingual gingiva [5]. Furthermore, an angular resorption pattern (“halo” lesion) which incorporates a periapical along with a lateral radiolucency extending apically has been shown as a typical radiographic feature of VRFs on conventional X-rays [6]. High-resolution visualization techniques with image accuracy and low radiation doses such as local CT, tuned-aperture computed tomography, and optical coherence tomography have been also successfully employed for monitoring VRFs [7, 8]. Nevertheless, when the diagnosis of a VRF is still inconclusive, exploratory surgical procedures are usually applied to verify its occurrence [6].
Clinical management has to be undertaken as soon as possible to prevent additional bone loss, which might pose difficulties for the further reconstruction of the region later on. Vertically fractured teeth inevitably lead to extraction in most of the cases. Alternative treatment procedures involve extraction only of the fractured root in multirooted teeth [9, 10]. Some authors suggest also removing the fractured tooth and rebonding the fractured parts extraorally followed by the reimplantation of the tooth [11, 12]. The introduction of cone-beam computed tomography in dentistry facilitated the three-dimensional high-resolution visualization of VRFs [13, 14].
The higher incidence of VRFs in root canal-treated teeth is mainly attributed to factors relating to conventional root-canal treatment such as excessive biomechanical preparation and extreme lateral-vertical forces during compaction of root canal filling materials [15–17]. The use of irrigants (NaOCl, EDTA) and intracanal medicaments (Ca(OH)2) for more than 30 days can also induce VRFs [18]. Additionally, tooth structural loss is mainly due to dehydration of dentine and microbe-induced degradation or modification of collagen constitutes risk factors for fracture predisposition in root canal-treated teeth [19]. Various restorative parameters such as insufficient ferrule effect, extreme widening of the root canal for posttreatment, and inappropriate postdesign may all contribute to VRF formation [20, 21].
Nowadays, the widespread conduction of endodontic surgery is considered an alternative approach with good prognosis in cases where an orthograde attempt at retreatment is not indicated [22]. Despite that modern microtechniques coupled with the appropriate surgical magnification have been introduced, VRFs relating to apical surgery may still occur. The removal of the apical part of the root, the use of specially designed ultrasonic tips as well as the retrograde MTA filling are treatment parameters that may be associated with VRFs in the framework of their multifactorial etiology.
The purpose of the present retrospective study was to evaluate potential etiological, clinical, and radiographic features of 200 root canal-treated teeth referred for extraction after a clinical diagnosis of VRF. All teeth had received an endodontic retreatment previously, either by a conventional root-canal retreatment, root-end resection or the combination of both techniques.
Materials and methods
Inclusion and exclusion criteria
The cross-sectional study was conducted over a period of 13 years in a total of 192 patients with 200 root canal-retreated teeth with a diagnosis of VRF. The vertically fractured teeth that were selected for this study had received endodontic treatment by general practitioners. It could be assumed that the prevailing quality guidelines for endodontic treatment at that time were followed to eliminate procedural complications [23]. However, if the quality of the root canal retreatment controlled by another endodontist prior to the study was questionable, the teeth were excluded from the study. Based on the type of endodontic retreatment they had received, the teeth were divided into three groups. In the first group, a conventional retreatment had been conducted; the second group had undergone apical surgery and the third group had been treated by both methods. Endodontic retreatment of all teeth had been completed at least 2 years earlier. In all cases, retreatment was conducted after the initial root canal treatment had been considered a failure.
Teeth with VRF were finally excluded from the amount of teeth studied if patient records lacked sufficient information about dental history of the fractured tooth or if the extraction was associated with dental trauma as well as other types of tooth fractures. Teeth with insufficient coronal restorations, with direct exposure of the root canal filling material to the oral cavity or with obturation material that did not reach within 2 mm of the radiographic apex were also excluded from the study.
Clinical procedure
When the inclusion criteria were fulfilled, the following clinical parameters were further evaluated by an endodontist: gender and age of the patient, endodontic history, tooth type (incisor, premolar, or molar in upper/lower jaw), clinical signs (depth and extent of periodontal pockets and presence of sinus tract and pus), type of endodontic retreatment (conventional retreatment, root-end resection, and combined use of both methods), and type of definite restoration (composite, post, and crown). Radiographic alterations were detected with the aid of a view-box with background illumination and magnification; loss of attachment was demonstrated as a deep, narrow, isolated periodontal pocket; and distinct separation of the cracked tooth fragments was diagnosed on X-rays. Exploratory surgery was additionally conducted to confirm an uncertain diagnosis. The use of magnifying loops (Carl Zeiss, Oberkochen, Germany) and staining with methylene blue solution along fractures enabled the operator not only to visualize the fracture lines but also to identify the extension of the fracture on the root surface (apical, central) and patency of fractures depending on separation of root fragments (complete, incomplete). All vertically fractured teeth were finally extracted by two oral surgeons, collected and stored in a 0.9 % saline solution at 4 °C until use.
Statistical analysis
Frequency tables and cross tables were used for the statistical evaluation of the data. To evaluate associations between categorical variables, the Chi-squared test was used. The Wilcoxon rank sum test was applied to detect significant differences in age between gender groups.
The analysis for evaluating differences between treatment groups was performed with a Cox PH model and corresponding Kaplan–Meier curves were presented. The log rank test was used to examine the difference between patients with different endodontic treatment. All statistical tests were done at the significance level of 5 % and were performed using the statistical software SAS 9.1.2.
Results
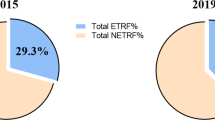
Type of endodontic treatment
Orthograde endodontic retreatment had been performed in 31.16 % of the teeth, whereas root-end resection had been conducted in only 6.5 % of the root-filled teeth. The majority of the vertically fractured teeth (62.31 %) had undergone the combination of conventional root canal retreatment and apical surgery. Moreover, after a maximum period of 4.4 years following only apical surgery all teeth were diagnosed with VRFs, whereas teeth which had been treated by both nonsurgical endodontic retreatment and root-end resection were diagnosed after a longer maximum period of 20 years. Box plots illustrating the time periods between the different types of endodontic treatment and detection of VRFs are shown in Fig. 1.
Box plots demonstrating the detection times of vertically fractured teeth in relation to different types of endodontic retreatment. The central line is the median; whiskers indicate minimum and maximum. After a maximum period of 4.4 years following only root-end resection (RER) all fractured root-filled teeth were diagnosed with VRFs, whereas all teeth which had been treated by both root canal retreatment and root-end resection (RCT + RER) were diagnosed after a longer maximum period of 20 years
Gender and age
The percentages of female and male patients demonstrating VRFs were 64.06 and 35.94 %, respectively. The mean age of patients presenting VRFs was 52.6 (±13.5; range, 22 to 79) years. The mean age of female and male patients with VRFs was 55.1 (±13.1; range, 22 to 78) years and 51.1 (±13.5; range, 22 to 79) years, respectively. This difference in age between gender was significant (p value = 0.02, Wilcoxon rank-sum test).
Tooth group
The most commonly extracted teeth were the maxillary first premolars (n = 35, 17.5 %), maxillary second premolars (n = 33, 16.5 %), maxillary central and lateral incisors (n = 24, 12 %), mandibular first molars (n = 23, 11.5 %), mandibular second premolars (n = 23, 11.5 %), and maxillary canines (n = 23, 11.5 %). There were very few extracted mandibular and maxillary second molars as well as mandibular incisors (n = 3, 1.5 %).
Clinical signs
The presence of deep periodontal pockets (23.9 %) was revealed along with the presence of a sinus tract without pus (28.93 %), sinus tract with pus (3.31 %) and combination of periodontal pocket and fistula (43.8 %).
Extension of VRF on the root surface
After the extraction of the vertically fractured teeth the extension of VRFs on the root surface was assessed macroscopically using magnifying loops (Carl Zeiss, Oberkochen, Germany). If the localization of the fracture line was difficult (especially by incomplete VRFs) staining with methylene blue solution along fractures enabled the inspection and categorization of VRFs (coronal, central, and apical) according to their extension on the root surface (Fig. 2). The extension point of VRFs was located apically in 56.77 % of the teeth which were macroscopically examined, whereas 43.23 % of the fractures reached the middle of the root surface. The mean distance measured between the extension point of VRFs and the cement–enamel junction was 5.8 (±3.5; range, 1 to 15) mm.
A vertically fractured mandibular first molar (46) with a fracture line reaching the middle third of the root surface. According to their extension point on the root surface (coronal third, middle third, and apical third), vertical root fractures (VRFs) were characterized as coronal, central, and apical, respectively. CEJ cement–enamel junction
Partial/complete VRFs
Based on separation of root fragments, 57.39 % of the VRFs were incomplete, whereas 42.61 % were complete. The inspection of the VRFs was conducted both radiographically (mainly complete VRFs) and visually (partial VRFs) with magnifying loops after the extraction of the vertically fractured teeth. Teeth with VRFs that could not be extracted under atraumatic conditions were excluded from the study in order to avoid the risk of turning an incomplete VRF into a complete one.
Radiographic diagnosis
Almost only half of the total amount of VRFs (56.5 %) was radiographically recognizable. There was a statistically significant association between radiographically recognizable VRFs and their location on the root. It was found that apically initiated VRFs were more easily observed on the radiographs (84.1 %) compared with the centrally located fractures (p < 0.001, Chi-square test).
Type of restoration
One hundred twelve teeth (56.28 %) had been previously coronally restored by resin-based composite without a post, 25 teeth (12.56 %) had been restored by a composite material with a post, 15 teeth (7.54 %) with posts were crowned, and 47 teeth (23.62 %) were only crowned.
An overview of the major findings of this study relating different clinical and radiographic parameters to VRFs after conventional root-canal retreatment, root-end resection or the combination of both techniques is presented in Table 1.
Discussion
The susceptibility of root canal-filled teeth to VRFs is highlighted in some recent reports [24–26]. The innovation of the present study is that it relates the type of endodontic retreatment with the incidence of VRFs. Specifically, orthograde endodontic retreatment had been previously performed in 31.16 % of the teeth, whereas 62.31 % of the vertically fractured teeth had undergone the combination of root canal retreatment and root-end resection. 6.5 % of the teeth had been retreated only with root-end resection. Procedures associated to the initial endodontic treatment such as the use of irrigants, medicaments, and root canal fillings can pave the way for the occurrence of VRFs [17, 18, 27]. The additional influence of the low moisture content and the reduced structural tooth integrity after access cavity preparation are also common VRF-predisposing side effects of the conventional root canal therapy [19]. However, a more profound damage is made to dentin during retreatment procedures. The additional mechanical widening of the canal system for the efficient removal of the old root canal filling, the use of various dissolving agents to soften gutta-percha as well as the removal of separated instruments and posts can cumulatively promote the defect progression in dentin [28–30].
Topical anomalies or more extensive pre-existing flaws located in the canal wall can induce subcritical cracks resulting in catastrophic root fractures after cyclic loading or immense occlusal stress [31]. Given also the fact that circumferential and radial stresses on root dentin are doubled by the presence of a root canal itself, the excessive removal of the apical part of roots, the application of ultrasonic instruments and retrograde filling materials as well as the mechanical stress during surgical endodontic procedures could further trigger comprehensive stress at the root surface and hence crack initiation [32]. The anisotropic mechanical properties of dentin because of the orientation of the tubules still challenges further research in this field [33]. Nevertheless, the effects of additional potentially harmful procedures during apical surgery are reflected in the higher incidence of VRFs (62.31 %) among teeth having undergone the combination of root canal retreatment and root-end resection. Excluding the cases where the conventional root canal therapy or retreatment failed because of pre-existing VRFs, it seems that the cumulative dentine damage associated with the initial endodontic treatment, retreatment and apical surgery could be possibly responsible for the outstanding presence of VRFs in teeth having undergone both conventional and surgical retreatment.
The multifactorial origin of VRFs in root canal-treated teeth has been well studied, so far. The influence of chemical agents (irrigants, intracanal medicaments), obturation biomaterials (gutta-percha, sealer), instrumentation and compaction techniques as well as restorative parameters (posts, crowns) in VRF predilection in teeth after initial endodontic treatment has been highlighted in previous studies [17–19, 27–29]. Nonetheless, endodontic retreatment procedures are not similar and thus, not comparable to the initial endodontic therapy. Root canals undergoing endodontic retreatment are subjected to additional preparation for the removal of the old obturation material, the use of different irrigants, ultrasonication, and the retrieval of posts and separated files. Given the different treatment protocols followed during retreatment cases resulting in additional stress of root canal walls, the comparison to primary cases was not considered meaningful in this report.
The fact that the root-canal treatments were conducted by general practicioners was one of the limitations of this study. Nevertheless, teeth were excluded from the study if the quality of the root canal retreatment was questionable. Under-/overinstrumented and insufficiently filled root canals were therefore rejected as they would compromise the results of this study.
As far as the detection time of VRF in the vertically fractured teeth is concerned, all surgically retreated teeth without conventional retreatment were diagnosed after 4.4 years. All nonsurgically retreated teeth following apical surgery were diagnosed with VRF after a longer period of 20 years. The delayed VRF diagnosis and thus, tooth removal in these cases can be attributed to the time-consuming treatment sessions as well as long inter-appointment, observation and recall periods in the framework of orthograde endodontic retreatment. Secondly, given their great desire to retain the tooth, patients having received nonsurgical retreatment probably seeked for dental procedures as conservative as possible in order to postpone or even avoid the extraction of the fractured teeth. Finally, the role of the dentist should also be taken into account. Specialized endodontists conducting conventional retreatment usually possess dental operating microscopes allowing for better discrimination of anatomic variations, control of instruments and prevention of intraoperative complications prior to surgery [34].
The gender distribution manifests a higher incidence of VRFs in women, a finding that contradicts with the results of other studies, where they are equally divided [35, 36]. The assumption that bleaching usually preferred by female patients attributes to dentin dehydration and thus to crack initiation seems a plausible explanation for this phenomenon [37]. Although it is difficult to ascertain why women have a higher degree of VRFs, it is much easier to surmise why older patients are prone to VRFs. Teeth of older patients that are longer in everyday use are more likely to receive root canal therapy over the years. The propensity of VRFs in older population is also related to low moisture content in dentine, closure of dentin tubules followed by an increased mineral concentration in dentin, as well as decrease in fracture toughness and fatigue crack growth resistance with advancing patient age [32, 38–40].
Maxillary first premolars (n = 35, 17.5 %) and maxillary second premolars (n = 33, 16.5 %) were found to have more VRFs than any other tooth, a fact which is consistent with other studies [41, 42]. The combination of all the maxillary and mandibular premolars constituted about 56 % of all the teeth seen with VRFs.
Despite that deep, narrow, osseous periodontal defects were present in many cases of VRFs (23.9 %), the simultaneous occurrence of sinus tracts showed significantly higher rates (43.8 %) invertically fractured teeth. However, the absence of the aforementioned clinical signs was verified in more than half of the VRFs examined, a fact that highlights the lack of specific clinical features for the diagnosis of VRFs. A recent report demonstrated a strong correlation between periodontal pockets and VRFs [43].
The radiographic diagnosis of VRFs can be a very challenging task. Although the detection of VRFs on radiographs is theoretically possible, the X-ray beam must be aligned with the fracture to enable its observation. Considering this technical restriction, radiographs have been proved an unreliable method for the diagnosis of VRFs [44]. Their low sensitivity to detect longitudinal fractures can be further attributed to the superimposition of other structures [13]. The development of three-dimensional intraoral radiography systems such as cone-beam computed tomography or digital volume tomography has facilitated a more accurate visualization of vertically fractured teeth and their adjacent structures. [14]. The present study confirmed that only about half of the VRFs (56.5 %) examined were radiographically recognizable. Nonetheless, the detection of apically extended VRFs on X-rays is probably more feasible because of their greater extension on the root surface compared with the centrally extended fractures.
The type of definite restoration plays an essential role in the process of fracturing [26]. Within the limitations of the present cross-sectional study, the use of resin composite as filling material appears to increase the susceptibility of root canal-treated teeth to VRFs. However, the presence of posts combined with composite restorations or with crowns seemed to prevent the appearance of VRFs despite that in some studies they increased fracture risk because of the stress they caused to dentin [40, 45]. It is generally believed that the least intraradicular stress is produced by fiber reinforced composite posts [46]. Nevertheless, posts should be utilized only in cases where there is little remaining tooth structure and hard tissue supports the apical portion of the post [21, 22].
References
Tang W, Wu Y, Smales RJ (2010) Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod 36:609–617
Fuss Z, Lustig J, Tamse A (1999) Prevalence of vertical root fractures in extracted endodontically treated teeth. Int Endod J 32:283–286
Fuss Z, Lustig J, Katz A, Tamse A (2001) An evaluation of endodontically treated vertical root fractured teeth: impact of operative procedures. J Endod 27:46–48
Tamse A, Kaffe I, Lustig J, Ganor Y, Fuss Z (2006) Radiographic features of vertically fractured endodontically treated mesial roots of mandibular molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:797–802
Tamse A, Fuss Z, Lustig J, Kaplavi J (1999) An evaluation of endodontically treated vertically fractured teeth. J Endod 25:506–508
Tamse A, Fuss Z, Lustig J, Ganor Y, Kaffe I (1999) Radiographic features of vertically fractured, endodontically treated maxillary premolars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 88:348–352
Shemesh H, van Soest G, Wu MK, Wesselink PR (2008) Diagnosis of vertical root fractures with optical coherence tomography. J Endod 34:739–742
Ozer SY (2010) Detection of vertical root fractures of different thicknesses in endodontically enlarged teeth by cone beam computed tomography versus digital radiography. J Endod 36:1245–1249
Lin CC, Tsai YL, Li UM, Chang YC, Lin CP, Jeng JH (2008) Horizontal/oblique root fractures in the palatal root of maxillary molars with associated periodontal destruction: case reports. Int Endod J 41:442–447
Floratos SG, Kratchman SI (2012) Surgical management of vertical root fractures for posterior teeth: report of four cases. J Endod 38:550–555
Hayashi M, Kinomoto Y, Miura M, Sato I, Takeshige F, Ebisu S (2002) Short-term evaluation of intentional reimplantation of vertically fractured roots reconstructed with dentin-bonded resin. J Endod 28:120–124
Kawai K, Masaka N (2002) Vertical root fracture treated by bonding fragments and rotational replantation. Dent Traumatol 18:42–45
Khedmat S, Rouhi N, Drage N, Shokouhinejad N, Nekoofar MH (2012) Evaluation of three imaging techniques for the detection of vertical root fractures in the absence and presence of gutta-percha root fillings. Int Endod J 45:1004–1009
Metska ME, Aartman IH, Wesselink PR, Özok AR (2012) Detection of vertical root fractures in vivo in endodontically treated teeth by cone-beam computed tomography scans. J Endod 38:1344–1347
Joyce AP, Loushine RJ, West LA, Runyan DA, Cameron SM (1998) Photoelastic comparison of stress induced by using stainless-steel versus nickel-titanium spreaders in vitro. J Endod 24:714–715
Gharai SR, Thorpe JR, Strother JM, McClanahan SB (2005) Comparison of generated forces and apical microleakage using nickel–titanium and stainless steel finger spreaders in curved canals. J Endod 31:198–200
Hammad M, Qualtrough A, Silikas N (2007) Effect of new obturating materials on vertical root fracture resistance of endodontically treated teeth. J Endod 33:732–736
Doyon GE, Dumsha T, von Fraunhofer JA (2005) Fracture resistance of human root dentin exposed to intracanal calcium hydroxide. J Endod 31:895–897
Kishen A (2006) Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod Topics 13:57–83
Schmitter M, Huy C, Ohlmann B, Gabbert O, Gilde H, Rammelsberg P (2006) Fracture resistance of upper and lower incisors restored with glass fiber reinforced posts. J Endod 32:328–330
Naumann M, Preuss A, Frankenberger R (2007) Reinforcement effect of adhesively luted fiber reinforced composite versus titanium posts. Dent Mater 23:138–144
Pop I (2013) Oral surgery: part 2. Endodontic surgery. Br Dent J 215:279–286
European Society of Endodontology (1994) Consensus report of the European Society of Endodontology on quality guidelines for endodontic treatment. Int Endod J 27:115–124
Santos AF, Tanaka CB, Lima RG, Espósito CO, Ballester RY, Braga RR, Meira JB (2009) Vertical root fracture in upper premolars with endodontic posts: finite elementanalysis. J Endod 35:117–120
Touré B, Faye B, Kane AW, Lo CM, Niang B, Boucher Y (2011) Analysis of reasons for extraction of endodontically treated teeth: a prospective study. J Endod 37:1512–1515
Seo DG, Yi YA, Shin SJ, Park JW (2012) Analysis of factors associated with cracked teeth. J Endod 38:288–292
Grigoratos D, Knowles J, Ng YL, Gulabivala K (2001) Effect of exposing dentine tosodium hypochlorite and calcium hydroxide on its flexural strength and elastic modulus. Int Endod J 34:113–119
Erdemir A, Eldeniz AU, Belli S (2004) Effect of the gutta-percha solvents on the microhardness and the roughness of human root dentine. J Oral Rehabil 31:1145–1148
Shemesh H, Bier CA, Wu MK, Tanomaru-Filho M, Wesselink PR (2009) The effects of canal preparation and filling on the incidence of dentinal defects. Int Endod J 42:208–213
Shemesh H, Roeleveld AC, Wesselink PR, Wu MK (2011) Damage to root dentin during retreatment procedures. J Endod 37:63–66
Lertchirakarn V, Palamara JE, Messer HH (2003) Patterns of vertical root fracture: factors affecting stress distribution in the root canal. J Endod 29:523–528
Winter W, Karl M (2012) Dehydration-induced shrinkage of dentin as a potential cause of vertical root fractures. J Mech Behav Biomed Mater 14:1–6
Lertchirakarn V, Palamara JE, Messer HH (2001) Anisotropy of tensile strength of root dentin. J Dent Res 80:453–456
Torabinejad M, Corr R, Handysides R, Shabahang S (2009) Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod 35:930–937
Chan CP, Lin CP, Tseng SC, Jeng JH (1999) Vertical root fracture in endodontically versus nonendodontically treated teeth: a survey of 315 cases in Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87:504–507
Cohen S, Berman LH, Blanco L, Bakland L, Kim JS (2006) A demographic analysis of vertical root fractures. J Endod 32:1160–1163
Betke H, Kahler E, Reitz A, Hartmann G, Lennon A, Attin T (2006) Influence of bleaching agents and desensitizing varnishes on the water content of dentin. Oper Dent 31:536–542
Bajaj D, Sundaram N, Nazari A, Arola D (2006) Age, dehydration and fatigue crack growth in dentin. Biomaterials 27:2507–2517
Soares CJ, Santana FR, Silva NR, Preira JC, Pereira CA (2007) Influence of the endodontic treatment on mechanical properties of root dentin. J Endod 33:603–606
Mireku AS, Romberg E, Fouad AF, Arola D (2010) Vertical fracture of root filled teeth restored with posts: the effects of patient age and dentine thickness. Int Endod J 43:218–225
Llena-Puy MC, Forner-Navarro L, Barbero-Navarro I (2001) Vertical root fracture in endodontically treated teeth: a review of 25 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 92:553–555
Kahler B, Heithersay GS (2008) An evidence-based appraisal of splinting luxated, avulsed and root-fractured teeth. Dent Traumatol 24:2–10
Takeuchi N, Yamamoto T, Tomofuji T, Murakami C (2009) A retrospective study on the prognosis of teeth with root fracture in patients during the maintenance phase of periodontal therapy. Dent Traumatol 25:332–337
Özer SY, Ünlü G, Değer Y (2011) Diagnosis and treatment of endodontically treated teeth with vertical root fracture: three case reports with 2-year follow-up. J Endod 37:97–102
Meira JB, Quitero MF, Braga RR, Placido E, Rodrigues FP, Lima RG, Ballester RY (2008) The suitability of different FEA models for studying root fractures caused by wedge effect. J Biomed Mater Res A 84:442–446
Hayashi M, Sugeta A, Takahashi Y, Imazato S, Ebisu S (2008) Static and fatigue fracture resistances of pulpless teeth restored with post-cores. Dent Mater 24:1178–1186
Acknowledgments
The authors express their gratitude to Dr. Fadil Elamin, Jonathan Bass, and Dr. Dougal Laird for their valuable scientific and linguistic contribution to this report.
Conflict of interest
We declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere. We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome. The manuscript has been read and approved by all named authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karygianni, L., Krengel, M., Winter, M. et al. Comparative assessment of the incidence of vertical root fractures between conventional versus surgical endodontic retreatment. Clin Oral Invest 18, 2015–2021 (2014). https://doi.org/10.1007/s00784-013-1182-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-013-1182-1